SUMMARY
SETTING
The role of the private sector in tuberculosis treatment in developing countries in sub-Saharan Africa is largely unknown. In recent years, many fee-for-service clinics have opened up in Kampala, Uganda. Little is known about the tuberculosis caseload seen in private clinics or the standard of care provided to the patients.
OBJECTIVE
To compare the appropriateness of tuberculosis care in private and public clinics, and the extent of the tuberculosis burden handled in the private sector.
DESIGN
Cross-sectional survey in private and public clinics treating tuberculosis patients in Kampala, Uganda, during June to August 1999.
MEASUREMENTS
Clinics were evaluated for appropriateness of care. This was defined as provision of proper diagnosis (sputum smear microscopy as the primary means of diagnosis), treatment (short-course chemotherapy, with or without directly observed therapy), outcome evaluation (smear microscopy at 6 or 7 months) and case notification in accordance with the Uganda National Tuberculosis and Leprosy Programme.
RESULTS
A total of 114 clinics (104 private, 10 public) were surveyed. Forty-one per cent of the private clinics saw three or more new tuberculosis patients each month. None of the public or private clinics met all standards for appropriate tuberculosis care. Only 24% of all clinics adhered to WHO-recommended treatment guidelines. Public clinics, younger practitioners and practitioners with advanced degrees were most likely to provide appropriate care for tuberculosis.
CONCLUSION
The private sector cares for many tuberculosis cases in Kampala; however, a new programme that offers continuing medical education is needed to improve tuberculosis care and to increase awareness of national guidelines for tuberculosis care.
Keywords: tuberculosis, quality of care, diagnosis, treatment, private provider
DEVELOPING COUNTRIES, especially countries in sub-Saharan Africa, have recently seen sharp increases in tuberculosis cases. In 1997 the World Health Organization (WHO) estimated that about 3.52 million cases of tuberculosis occurred worldwide; nine out of 10 countries with the highest tuberculosis incidence rates were in Africa.1 The sister epidemic, the human immunodeficiency virus type-1 (HIV), has exacerbated the problem of tuberculosis: there are an estimated 9.4 million persons co-infected with HIV and tuberculosis globally, two-thirds of whom live in sub-Saharan Africa. In 1997, 32% of all tuberculosis cases in sub-Saharan Africa occurred in HIV-infected individuals.1
As in the rest of sub-Saharan Africa, the dual epidemics of HIV and tuberculosis continue to pose serious challenges to health care delivery in Uganda.2 From 1990 through 1996, the annual notification rate of tuberculosis cases in Uganda increased by over 40%, from 14 740 to 27 196 cases per year.3 In 1999, 29 294 tuberculosis cases were reported to the National Tuberculosis and Leprosy Control Programme (NTLP), almost 60% of whom presented with acid-fast bacilli (AFB) on sputum microscopy. Based on cross-sectional HIV seroprevalence surveys among tuberculosis patients, up to 65% of cases in Uganda are HIV seropositive,4 thereby indicating the tremendous burden from this dual epidemic.
The Uganda NTLP is a semi-vertical programme of the Ministry of Health that provides basic diagnostic and curative services for tuberculosis based on recommendations from the WHO. Management, planning and supervision components of the program are vertical, whereas its implementation is integrated into the national health delivery system at the district level.3
The private health sector is growing rapidly in Uganda, and is gradually becoming the main provider of health care services to the general population.5 This growth in service is especially true for private for-profit health clinics. In Kampala City, the number of private medical clinics has more than doubled in the past 2 years.4 Many patients choose private fee-for-service clinics in the private sector rather than government health services, where cost-sharing has been used.5 Cost-sharing is when the patient pays a small fee for the use of the government health facility; these fees are usually $0.30–0.60, and help to defray the costs of running the health facility. Cost-sharing revenue from the public health facilities accounted for 12% of total district health financing in 1999.6
These changes in health care services will impact the NTLP in several ways as patients with tuberculosis seek care in the private sector. First, if the private sector does not provide proper treatment for tuberculosis, there is the potential of creating a reservoir of drug-resistant cases. Second, if the private sector fails to report cases properly to the national tuberculosis control programme, the national statistics will be derived only from cases reported from the public health facilities, so under-reporting will occur. Under-reporting of tuberculosis cases may have important implications in public health policy for the allocation of resources to tuberculosis control and the assessment of key outcomes of tuberculosis control strategies in the country. For these reasons, it is important to assess the quality of tuberculosis care in private clinics, the scope of care and capacity for the tuberculosis cases handled, the emergence of multidrug resistance, and the effectiveness of tuberculosis control, and to compare them with the government clinics.
METHODS
A cross-sectional study of all public clinics and a stratified random sample of private clinics was conducted in Kampala, Uganda, during June to August 1999. The study was conducted in Kampala District in the capital city of Uganda, an urban area with a population of 774 241.7 Approximately 46% of the people live in severe poverty.8 A clinic was eligible for study participation if it was located in Kampala District, if the owner of the clinic was a doctor or medical assistant, and if the owner consented to participate in the study. Clinics were excluded if the owner could not be traced, refused to participate, was a nurse/midwife, or if the clinic did not treat patients with tuberculosis.
To obtain the study sample, we generated a computerised set of random numbers that was used to assign a number to each of 91 parishes within each of five divisions of Kampala. Parishes were then randomly sampled for the study. Once a parish was chosen interviewers went to the trading centre of the assigned parish and walked along the main road, identifying consecutive clinics and collecting information to determine eligibility for the study. Ineligible clinics were replaced by further consecutive sampling from their respective parishes until a minimum of three clinics in that parish were enrolled. All 10 public health clinics in Kampala District were included in the sample.
If a clinic met the eligibility criteria, a standardised questionnaire was administered to the clinic owner by one of four trained interviewers. All interviewers underwent an orientation that involved familiarisation with NTLP policies and tuberculosis diagnosis and treatment. One health practitioner was interviewed at each clinic. The health worker in charge of the public health clinic was approached in a similar manner. Verbal informed consent from the operator of the clinic was obtained before study participation. The study protocol was reviewed and approved by the Uganda National AIDS Research Sub-committee and the institutional review board at Case Western Reserve University.
Information about the clinics, their operating practices and the qualification of the clinic directors was collected using a structured interview and questionnaire. Knowledge and perceptions about the NTLP were also sought. Interviewers were social science students trained to conduct provider interviews. They were chosen over medical students and other practitioners because they had been found to be less threatening to the private providers in earlier studies in India (M Uplekar, personal communication).
Definitions of appropriate care
A panel of three experts in tuberculosis or scale development developed a weighted scale for appropriate care for tuberculosis (Table 1). The scale included four components: diagnosis, treatment, follow-up and reporting. Diagnosis was considered appropriate if AFB smear microscopy was performed whenever a diagnostic specimen was available. In children, diagnosis was considered appropriate if tuberculin skin testing or chest X-ray was used in addition to clinical data. Treatment was considered appropriate if the regimen was recommended by either the WHO or the Ugandan NTLP. Additional points were given if directly observed therapy was used. Follow-up was considered appropriate if sputum microscopy was performed after 2 and 5 months of treatment to assess response to therapy, and if cure was ascertained by microscopy at the end of treatment. Record keeping and reporting was considered appropriate if the clinic kept medical records and if the NTLP was routinely notified of all smear-positive cases. In this scale, diagnosis and treatment were assigned the greatest weights.
Table 1.
Scale used for measuring appropriateness of tuberculosis care
| Component | Points |
|---|---|
| Diagnosis | 4 |
| Sputum microscopy for AFB | 2 |
| Tuberculin skin test or chest X-ray in children | 2 |
| Treatment | 6 |
| WHO or NTLP regimen | 4 |
| Carries out DOT | 2 |
| Outcome evaluation | 2 |
| Sputum microscopy repeated after 2 and 5 months | 1 |
| Ascertains cure by negative sputum | 1 |
| Record keeping and reporting | 2 |
| Keeps medical records | 1 |
| Reports cases to the NTLP | 1 |
| Total score | 14 |
AFB = acid-fast bacilli; WHO = World Health Organization; NTLP = National Tuberculosis and Leprosy Control Programme; DOT = directly observed therapy.
The definition of what constituted a high volume of tuberculosis cases was based on the number of new tuberculosis cases seen each month by the clinics surveyed in the study. Using the mean volume of tuberculosis patients as a cut-off level, clinics that saw more than two new cases of tuberculosis each month on average were said to have high case loads, and those who treated two or fewer new cases monthly had by definition a low case load. The number of professional degrees attained was used as a measure of qualification of the health care provider. Practitioners with at least two degrees were considered more qualified than practitioners with one or fewer degrees. The cost charged to patients was ascertained by asking the health practitioner the amount of money spent by a tuberculosis patient on his/her drugs and investigations.
During the initial interviews, the study interviewers identified 11 providers who were willing to be interviewed a second time to validate the questionnaire. The time interval between the two interviews in the validation sample was 2 months. Inter-rater reliability was assessed in 11 (10%) of the clinics by comparing the responses for each of the four elements of appropriate care on interviews repeated by different interviewers with the kappa statistic. The kappa statistic was 1.0 for diagnosis, 0.84 for treatment, 0.79 for evaluation of treatment outcomes and 0.7 for record keeping. Information collected during the interview was validated against the medical records in 14 (12%) of the clinics. Agreement between self-report and medical records ranged from 24% to 67%.
Analysis
The characteristics of the public and private clinics were compared using the Student’s t-test or χ2 test, where appropriate. Variables were then univariately tested for association with appropriateness of care. This was followed by multivariate analysis with both linear and logistic regression. The results of the two models were compared. All data were entered using Epi-Info version 5.01 (CDC, Atlanta, GA, USA) and analysed using SPSS 8.0 (SPSS Inc, Chicago IL, USA).
RESULTS
Clinic characteristics and practices
A total of 230 clinics were approached in the study area. One hundred and fourteen clinics met all of the eligibility criteria and comprised the study sample. Clinics were not enrolled in the study if they were closed at the time the interviewer arrived, the owner could not be traced or refused to participate (n = 81), they were owned by either a nurse or midwife (n = 20), and they did not treat tuberculosis patients (n = 9). Two clinics were diagnostic centres only, and one clinic was excluded due to incomplete information on the intake assessment. Private clinics were more likely to be run by a male doctor, whereas public clinics were more likely to be run by a female medical assistant.
The public clinics had a higher daily volume of patient visits than the private clinics. The public clinics also evaluated and treated more tuberculosis cases per month than private clinics (Table 2). The median cost for tuberculosis diagnosis and treatment charged to the patient in the private clinics was $190 US dollars, whereas service was most often free of charge in public clinics (Table 2). Nearly all of the private clinics claimed they had referred tuberculosis patients to the NTLP (Table 2). Over half of the tuberculosis cases presenting to the public clinics had already received anti-tuberculosis treatment, compared to only one-third in private clinics.
Table 2.
Baseline characteristics of clinics and respondents
| Characteristic | Private clinics (n = 104) |
Public clinics (n = 10) |
||
|---|---|---|---|---|
| Mean (SD) | Median | Mean (SD) | Median | |
| Age of respondent | 36.5 (10.3) | 34.0 | 34.7 (5.6) | 34.5 |
| Total patients seen/day* | 16.4 (16.5) | 10.0 | 32.2 (19.6) | 30.0 |
| New TB cases/week* | 1.70 (5.2) | 0.0 | 14.6 (25.8) | 3.0 |
| New TB cases/month* | 6.80 (19.2) | 2.0 | 46.4 (97.3) | 13.5 |
| Per cent of patients with prior treatment for TB | 32.6 (37.1) | 12.0 | 52.4 (33.7) | 50.0 |
| Cost charged to patient for TB medications (US$) | 317 (366) | 190 | 58.6 (114) | 0.0 |
| n (%) | n (%) | |||
| Prescribed WHO regimen | 24 (23.1) | 3 (30) | ||
| Directly observed therapy | 66 (63.5) | 7 (70) | ||
| Referred to NTLP | 99 (95.2) | 0 | ||
P < 0.05 when public and private clinics are compared.
SD = standard deviation; WHO = World Health Organization; NTLP = National Tuberculosis and Leprosy Control Programme.
Public clinics were more likely than private clinics to carry out sputum microscopy as the diagnostic test for tuberculosis (80% vs. 69%, P > 0.05). Practitioners in the private clinics relied equally on sputum smear examination and chest X-rays to make a diagnosis of tuberculosis in adults, whereas practitioners in public clinics relied more on sputum examination. Private practitioners more often considered chest X-ray, instead of sputum microscopy, as the best follow-up test for tuberculosis than public practitioners (80% vs. 10%, respectively; P = 0.05). Private and public practitioners used sputum culture equally as a means of diagnosis (30% vs. 28% respectively, P = 0.58).
Of the 10 public clinics, three (33.3%) used a treatment regimen recommended by the WHO (Table 2). Among the 104 private clinics, 24 (23.1%) prescribed the WHO-recommended regimen to their patients. None of the clinics—public or private—treated smear-positive tuberculosis patients using regimens recommended by the NTLP. In fact, 19 different regimens were being used to treat new smear-positive tuberculosis cases. The proportion of practitioners who stated they used directly observed therapy was similar for private and public clinics (63.5 vs. 70%, Table 2). Less than half of the private clinics (46%) stocked all of the standard first-line anti-tuberculosis drugs (isoniazid, rifampicin, pyrazinamide, streptomycin and ethambutol), so most private clinics were not prepared to provide the initial treatment to tuberculosis patients.
There was a widespread lack of knowledge concerning the management of tuberculosis in HIV-infected patients by practitioners in both public and private clinics. Practitioners at only one of the 10 public clinics (10%) were able to answer basic questions related to treatment of HIV patients co-infected with tuberculosis, as compared to 61 (55%) of those interviewed in the private clinics. Of the private providers who answered these questions, 10 (9%) thought treatment of HIV-infected patients with tuberculosis was longer than for non-HIV-infected patients, and 15 (13.3%) thought treatment was shorter. Twenty-one per cent thought that treatment of TB in HIV-infected individuals required different drugs.
Sixty-three per cent of the private health clinics did not attempt to contact patients who failed to keep follow-up appointments for tuberculosis treatment compared to only 30% of the public clinics (P = 0.043). Of the practitioners who did not directly supervise treatment, keeping scheduled appointments and improvement of tuberculosis symptoms were the measures most commonly used to assess compliance.
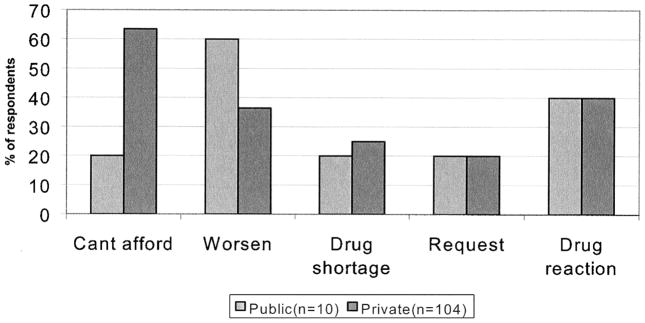
The most common reason for patient referral from the private to the public sector was the cost of treatment and management of tuberculosis (Figure 1). In contrast, the most common reason for public clinics to refer to government hospitals was worsening medical condition or suspected drug reaction (Figure 1). Both private and public clinics referred to the NTLP when drug shortages occurred, upon patient request, and for suspected drug reaction.
Figure 1.
Reasons for referral among public and private practitioners.
The majority of private practitioners knew about the existence of the NTLP, but only half of them knew that it issued national guidelines for diagnosis and treatment of tuberculosis and leprosy. Forty-one per cent of private practitioners wanted an update on information about tuberculosis treatment. Forty-one per cent of the private providers also requested that their clinics be supplied with subsidised anti-tuberculosis medications and laboratory supplies. Almost all (99%) wanted feedback about their performance relative to other practitioners. Preferred avenues for disseminating this information were workshops conducted by the NTLP (70%), brochures and magazines (44%), and newspapers (39%).
Appropriateness of care
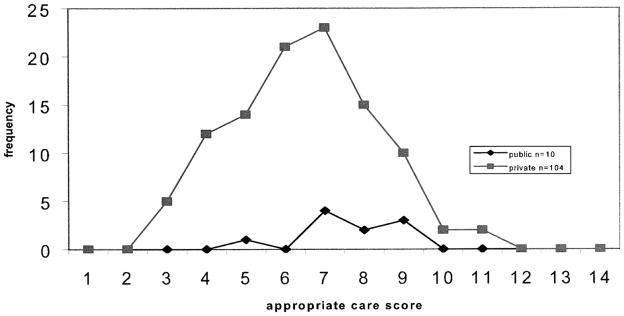
The distribution of scores for appropriateness of care was normally distributed, with a median of 7 and a range of 3 to 11 (Figure 2). None of the clinics scored 14, the hallmark of appropriate care. The median score for private clinics was lower than for public clinics (6.5 vs. 7.5, not significant; Table 3). Approximately one-third of the private clinics had a score greater than 7; thus, a score of 7 was chosen as the cut-off for appropriate care in further analyses. The median scores for diagnosis, outcome evaluation and reporting were the same for each clinic setting (Table 3). The public clinics, however, scored higher in the treatment area, as they provided a WHO-recommended short-course regimen more often (Table 3).
Figure 2.
Appropriate care score distribution.
Table 3.
Mean and median scores for scale measuring appropriateness of care according to private and public clinics
| Appropriate care scale | Private clinics (n = 104) |
Public clinics (n = 10) |
||
|---|---|---|---|---|
| Mean (SD) | Median | Mean (SD) | Median | |
| Diagnosis | 3.0 (0.97) | 3.0 | 3.3 (0.67) | 3.0 |
| Treatment | 1.4 (1.88) | 0.0 | 2.0 (2.11) | 2.0 |
| Outcome evaluation | 0.8 (0.52) | 1.0 | 1.2 (0.63) | 1.0 |
| Record keeping and reporting | 1.8 (0.37) | 2.0 | 1.7 (0.48) | 2.0 |
| Total appropriate care score | 6.5 (1.82) | 6.5 | 7.6 (1.26) | 7.5 |
SD = standard deviation.
In a linear regression analysis, younger age and provider qualifications were independently associated with the score for appropriateness of care. Younger practitioners with medical degrees or certificates were more likely to have higher scores, thereby indicating more appropriate care. When using a score of 7 as a minimal value for appropriate care on the derived scale, the same factors were associated with proper care (Table 4). In this analysis, private clinics were less likely to provide appropriate care when compared with public clinics (odds ratio 0.17); similarly, practitioners aged 35 years or more were less likely to provide appropriate care when compared with the younger practitioners (odds ratio 0.92). More qualified practitioners, as measured by two or more degrees, were more likely to provide appropriate care (odds ratio 4.8).
Table 4.
Logistic regression analysis of the relation between appropriate care and variables related to clinic practice. Dependent variable is appropriateness of care or a dichotomous variable (<7 or ≥7)
| Variable | OR | 95%CI |
|---|---|---|
| Setting | ||
| Public | 1.00 | 0.03–0.8 |
| Private | 0.17 | |
| Age | ||
| <35 years | 1.00 | 0.86–0.98 |
| ≥35 years | 0.92 | |
| Qualification | ||
| <2 degrees | 1.00 | 1.97–10.2 |
| ≥2 degrees | 4.48 | |
OR = odds ratio; CI = confidence interval.
DISCUSSION
Overall, tuberculosis care is in need of improvement in Kampala. Although the diagnosis, outcome evaluation and record keeping appear to be appropriate among health care practitioners, proper choice of anti-tuberculosis treatment regimen is lacking. The use of regimens recommended by the WHO or the Ugandan NTLP was infrequent: only 24% of the private practitioners prescribed a WHO-recommended tuberculosis treatment regimen. Our findings are comparable to a study from Bolivia, where only 21% of the private physicians followed national guidelines,9 but differ from a study in India, where 59% of practitioners used recommended regimens.10 A study in Botswana evaluating the adherence of physicians to national treatment control guidelines concluded that recommended diagnostic procedures for tuberculosis were not being followed by a substantial percentage of physicians.11
One striking finding was that no clinic, either public or private, prescribed the NTLP-recommended regimen.12 This regimen may not be popular in Uganda because of the increased risk of adverse cutaneous drug reactions due to thiacetazone in HIV-infected patients, the longer duration of treatment compared to rifampicin-based short-course regimens, and the use of streptomycin, which requires daily injections during the first 2 months of treatment. Our findings indicate that regimens recommended by the WHO and NTLP are not often used in either the private or public setting. Indeed, a wide variety of regimens are now prescribed with inconsistent use of rifampicin. These findings suggest that the practitioners were not aware of the published recommendations for tuberculosis care.
Despite the use of non-standard regimens, private practitioners claimed to provide directly observed therapy for nearly two-thirds of patients. This practice in fact seems unlikely, given other responses about monitoring compliance and tracing of defaulters. Nevertheless, it indicates that these practitioners may not fully understand how directly observed therapy should be given. Moreover, private clinics are poorly stocked with anti-tuberculosis drugs, so even if practitioners knew the correct regimen and could provide directly observed therapy, they could not give it to the patient from their stock of medications.
In general, public clinics provided more appropriate care for tuberculosis patients than private clinics. Only one-third of the private clinics practiced a minimal standard of appropriate tuberculosis care. Public clinics are under the supervision of the Uganda NTLP, so their practices are standardised by the use of guidelines. Similar results were reported from a study done in Korea.13
High tuberculosis case volume was not associated with appropriate care, suggesting that experience alone does not lead to expertise in tuberculosis care, but experience with proper training may be the essential ingredient. In addition to the public setting, we found that younger, more qualified practitioners, as measured by the number of degrees, were more likely to provide appropriate care. Each of these favourable characteristics may be linked to training. Public practitioners are usually medical assistants who receive training through the NTLP before working in tuberculosis control. The number of degrees is a measurement of the level of formal education, suggesting that tuberculosis care would be improved with more formal training that awarded certificates or degrees. Younger age may be a surrogate for recent training, through either a degree or work-related programmes.
Several studies have shown a need for periodic updating and continuing education for private physicians. In India, Uplekar and colleagues highlighted the need to educate both private practitioners and their patients with tuberculosis.14 In Vietnam, Viet Cô found that knowledge about tuberculosis diagnosis and treatment was poor among both private and general doctors, and recommended increased training in tuberculosis case management.15 As in the other studies, Ugandan practitioners identify the need for further education in the care and management of tuberculosis. Virtually all private practitioners in Kampala asked to know their performance in tuberculosis care relative to others, indicating an interest in their quality of care.
The referral patterns of tuberculosis cases from the private sector to the NTLP suggest that treatment for tuberculosis is initiated before referral in about half of cases. The most common reason for referral is inability to pay for the health care services or medication. Considering that the annual per capita income in Uganda is US $300,7 the mean cost of $317 charged to patients for tuberculosis diagnosis and treatment is unaffordable for most Ugandans and represents a substantial loss of income to the family.16 This situation is not unique to Uganda, as similar patterns of access to tuberculosis care have been reported in other countries.13,17 This pattern of referral, however, has important implications for tuberculosis care in Kampala. If half of the tuberculosis patients are seen in the private sector and treated with inadequate regimens for varying lengths of time, then the NTLP will see cases at increased risk for treatment failure, relapse and acquired drug resistance. The main reason for referral from the public sector to a hospital was worsening medical condition. This may be because public practitioners are more aware of the complications of tuberculosis because of their training, or because public clinics are often run by medical assistants and registered nurses who may be reluctant to manage complicated cases.
Several limitations must be considered in interpreting our findings. The scale for measuring appropriate care may fail to capture the health care behaviours of practitioners. Future studies of private practitioners should endeavour to link practice behaviours with treatment outcome. Because this study was conducted in Kampala City, an urban area, our results may not be generalisable to the rural areas where there may be considerable differences in practice. Our comparison groups also were not the same size, because the number of public clinics was fixed. It would also have been useful to validate the laboratory practices for TB diagnosis in the clinics. Verification of the private provider information was only possible among those who granted access to their medical records; this may have introduced a reporting bias if practitioners who refused access to their medical records reported inaccurate information.
In Kampala, the practices of private practitioners do not often meet the standards set by the Ugandan National Tuberculosis Programme or the WHO. These practitioners, however, are eager to participate in educational programmes about tuberculosis. Our study opened up a point of contact with private providers in Uganda that did not exist before—one which can be used by the NTLP for further interaction with and education of private practitioners. National tuberculosis training programmes, and other public or private institutions, should consider ways of reaching private practitioners and training them in the proper diagnosis and management of tuberculosis.
Acknowledgments
This work was supported through the AIDS International Training and Research Programme (TW–00011) and the Tuberculosis Research Unit (NO1-AI95383) at Case Western Reserve University. The authors extend their gratitude to the Uganda Ministry of Health, with special thanks to the National Tuberculosis and Leprosy Programme for their support with the study.
References
- 1.Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999;282:677–686. doi: 10.1001/jama.282.7.677. [DOI] [PubMed] [Google Scholar]
- 2.STD/AIDS Control Programme MoH. HIV/AIDS Surveillance Report, June 2000. Kampala, Uganda: MoH; 2000. [Google Scholar]
- 3.Adatu F. National TB/Leprosy Programme: status report 1997. Kampala, Uganda: MoH; 1997. Ministry of Health. [Google Scholar]
- 4.Eriki PP, Okwera A, Aisu T, Morrissey AB, Ellner JJ, Daniel TM. The influence of human immunodeficiency virus infection on tuberculosis in Kampala, Uganda. Am Rev Respir Dis. 1991;143:185–187. doi: 10.1164/ajrccm/143.1.185. [DOI] [PubMed] [Google Scholar]
- 5.Okello D. The growth of the private health sector in Uganda: An appraisal of scope and impact. A research report of the International Health Policy Program (IHPP) project in Uganda. Kampala, Uganda: Uganda National Council of Science and Technology (UNSCT); 1997. [Google Scholar]
- 6.Wilson L. A review by OXFAM, UK. Oxford: Oxfam; 2000. Cost sharing in Uganda. [Google Scholar]
- 7.Statistics Department of Uganda. Population and housing census 1991. Kampala, Uganda: Ministry of Finance PaED; 1991. [Google Scholar]
- 8.Ministry of Finance PaED. Monitoring survey 1995/1996. Kampala, Uganda: Ministry of Finance PaED; 1995. [Google Scholar]
- 9.Olle-Goig JE, Cullity JE, Vargas R. A survey of prescribing patterns for tuberculosis treatment amongst doctors in a Bolivian city. Int J Tuberc Lung Dis. 1999;3:74–78. [PubMed] [Google Scholar]
- 10.Uplekar M, Juvekar S, Morankar S, Rangan S, Nunn P. Tuberculosis patients and practitioners in private clinics in India. IUATLD Int J Tuberc Lung Dis. 1998;2:324–329. [PubMed] [Google Scholar]
- 11.Huebner RE, Moeti TL, Binkin NJ, Rumisha DW. Survey of physician use of radiography and sputum smear microscopy for tuberculosis diagnosis and follow-up in Botswana. Int J Tuberc Lung Dis. 1997;1:333–338. [PubMed] [Google Scholar]
- 12.National Tuberculosis/Leprosy Programme. Manual of the National Tuberculosis/Leprosy Programme in Uganda for the District Tuberculosis/Leprosy supervisors. Kampala, Uganda: MoH; 1992. [Google Scholar]
- 13.Hong YP, Kim SJ, Lee EG, Lew WJ, Bai JY. Treatment of bacillary pulmonary tuberculosis at the chest clinics in the private sector in Korea. Int J Tuberc Lung Dis. 1999;3:695–702. [PubMed] [Google Scholar]
- 14.Uplekar M, Rangan S. Tackling TB: the search for solutions. Bombay, India: The Foundation for Research in Community Health; 1996. [Google Scholar]
- 15.Viet Cô NMHT, Duc Chinh N. Diagnosis and treatment for tuberculosis patients by private doctors and the doctors of the general hospitals in Hanoi and Da Nang of Vietnam. Int J Tuberc Lung Dis. 1998;2(Suppl 2):S259. [Google Scholar]
- 16.Saunderson PR. The Kellensberger memorial lecture 1994. Ethiopian Med J. 1994;32:269–280. [PubMed] [Google Scholar]
- 17.Hurting AK, Pande SB, Baral SC, Porter JDH. Anti-tuberculosis treatment in private pharmacies, Kathmandu Valley, Nepal. Int J Tuberc Lung Dis. 1998;2(Suppl 2):S259. [PubMed] [Google Scholar]