Abstract
Objectives
The objective of this study was to investigate the in vitro particle size growth of combination drug and excipient submicrometer aerosols generated from a series of formulations and two aerosol delivery devices.
Methods
Submicrometer combination drug and excipient particles were generated experimentally using both the capillary aerosol generator and the Respimat inhaler. Budesonide and albuterol sulfate were used as model drugs and were formulated with sodium chloride, citric acid, and mannitol as excipients in various ratios. Aerosol growth was evaluated in vitro in a coiled tube geometry designed to provide residence times and thermodynamic conditions consistent with the airways.
Key Findings
Submicrometer combination drug:excipient aerosols when exposed to simulated respiratory conditions increased to micrometer size suitable for pulmonary deposition. It was possible to control the aerosol growth ratio by altering: (1) the hygroscopic excipient, (2) the drug:excipient ratio and (3) the drug. The applicability of this approach was demonstrated using the capillary aerosol generator and the Respimat inhaler.
Conclusions
The enhanced excipient growth (EEG) approach may enable the delivery of submicrometer aerosol particles that increase in size within the airways and result in high percentages of pulmonary deposition.
Keywords: Respiratory drug delivery, enhanced excipient growth (EEG), nanoaerosols, hygroscopic growth, combination particles
INTRODUCTION
Metered dose inhalers (MDI) and dry powder inhalers (DPI) have been shown to be inefficient at delivering pharmaceutical aerosols to the lungs. This is mainly due to depositional loss of drug in the mouth-throat (MT) region during inhalation. Deposition of drug in this region varies between 25–60 % of the dose for HFA MDIs (1–5) and from 50–70% for DPIs (3, 6, 7). Drug deposited in the MT region has no therapeutic effect, may cause side effects (8) and contributes to the observed large intersubject variability in lung doses for inhaled drugs (9). The goal for the next generation of inhalation drug delivery formulations and devices is to significantly improve lung deposition efficiency compared to the current generation of inhalers.
An effective way of increasing the lung delivery of pharmaceutical aerosols is by reducing the aerodynamic size of the particles. Submicrometer aerosol particles have been shown to efficiently penetration the MT region in contrast to conventional pharmaceutical aerosols, which are often 2 μm or greater (10). However, due to their size, deposition and retention of submicrometer particles in the lungs is low and a significant fraction of the aerosol is exhaled (11). Longest and Hindle have proposed using a method of controlled aerosol growth to improve the lung deposition of submicrometer aerosols (12, 13). With this method, submicrometer aerosols are inhaled via the mouth or nose with minimal deposition in these regions. The size of the aerosol increases as it enters the airways and once it is inside the lungs, which ensures deposition and full lung retention. Aerosol growth can be achieved using two methods known as enhanced condensational growth (ECG) and excipient enhanced growth (EEG). For ECG, the submicrometer aerosol is inhaled with a stream of saturated or supersaturated air that is above body temperature. Cooling of the saturated air in the respiratory tract results in water vapor condensation onto the droplets, growth, and enhanced lung deposition (12, 14, 15). For EEG, a formulation approach is used where submicrometer aerosol particles composed of a drug and hygroscopic excipient are inhaled and aerosol growth occurs due to the inherent relative humidity of the lungs (13). This method is suitable for drugs that are inherently hygroscopic or hydrophobic due to the presence of the hygroscopic excipient. Longest and Hindle investigated the size increase of submicrometer aerosols composed of drug and hygroscopic excipient combinations using the EEG approach (13, 16). Longest and Hindle (13) implemented a whole-lung model of aerosol transport to develop correlations of aerosol size increase, whereas Longest and Hindle (16) explored aerosol size increase with EEG by developing a validated computational fluid dynamics (CFD) model. Under typical respiratory exposure conditions, large diameter growth ratios were observed (2.1 – 4.6) for hygroscopic and non-hygroscopic drugs and a range of excipients.
The hygroscopic behavior of aerosols has been studied widely, perhaps most extensively by atmospheric physicists and industrial hygienists who examined the behavior of pollutants following inhalation (17, 18). They recognized that inhaled hygroscopic substances will absorb water vapor which is present in the lung airways and that resulting changes in the aerosol particle size and density may alter their deposition site within the lungs. Similarly, Gonda and Byron recognized that the aerosol particle size of inhaled hygroscopic pharmaceuticals will be affected by the relative humidity within the lungs (19). Hickey and Martonen reviewed the theoretical and experimental hygroscopic growth of a series of commonly used inhaled drugs (20). They described the potential to formulate aerosols of specific size and to target deposition of these particles within specific regions of the lung using the known specific growth kinetics of the aerosol particles during inhalation (20). However, such studies have employed excipients, such as glycerol and fatty acids (lauric acid and capric acid) to reduce the hygroscopicity of the aerosol and prevent an increase in size of initially micrometer aerosols (21). For these studies, aerosol particle hygroscopic growth was minimized in order to avoid excessive upper airways aerosol deposition and to increase deposition in the lower airways. In contrast, the EEG approach initially starts with a submicrometer aerosol to minimize mouth-throat deposition and seeks to foster aerosol particle size increase in order to cause pulmonary deposition and to potentially target the site of aerosol delivery within the airways.
This study seeks to investigate a novel aerosol drug delivery approach using combination drug–excipient submicrometer particles which may offer high drug deposition efficiency in the lungs and minimal losses in the mouth-throat region. Its objective is to investigate the effects of EEG formulation variables (excipient type, drug excipient ratio, drug type and aerosol generation device) on the aerosol hygroscopic growth characteristics of combination drug and excipient submicrometer aerosols using in vitro particle sizing experiments. A non-hygroscopic drug was selected, budesonide, in order to ensure that the observed growth arises entirely from the inclusion of the hygroscopic excipient. To investigate the effects of drug hygroscopicity, albuterol sulfate, was also tested for select formulations. Three hygroscopic excipients were considered, which were a representative salt (sodium chloride; NaCl), a weak acid (citric acid; CA), and a sugar (mannitol; MN), all of which have been employed previously in inhaled drug products. Submicrometer combination drug and excipient particles were generated from solution formulations using both the benchtop capillary aerosol generator (CAG) (12, 22) and the commercially available handheld Respimat inhaler (23, 24). The Respimat is a soft mist inhaler that generates a slow moving aerosol cloud for inhalation. Growth was evaluated in a coiled tube EEG geometry with wet walls designed to provide a residence time consistent with a typical inhalation cycle (approximately 2 s) during which the aerosol was exposed to airway thermodynamic conditions.
MATERIALS AND METHODS
Aerosol Formulations
Budesonide and albuterol sulfate (Spectrum Chemicals, New Brunswick, NJ) were used as model drugs. Ethanol (absolute 200% proof) was obtained from Sigma-Aldrich Corp. (St. Louis, MO). The excipients evaluated for hygroscopic growth were sodium chloride (NaCl), citric acid (CA) and mannitol (MN), (Sigma-Aldrich Corp., St Louis, MO). For the CAG aerosol, aerosols were produced from solution formulations of drug and excipient in a 50%v/v water and 50% v/v ethanol vehicle. For Respimat aerosol generation, aerosols were produced from solution formulations of drug and excipient in a 10%v/v water and 90% v/v ethanol formulation.
Aerosol Generation Methods
The capillary aerosol generation system is described and considered in detail by the previous studies of Hindle et al. (22) and Longest et al. (25). A submicrometer aerosol was generated into a 900 ml drying chamber (length: 220 mm x diameter: 76 mm) from the CAG using a solution mass flow rate of 10 mg/s actuated for 2 seconds. For Respimat aerosol generation, the solution formulation was loaded into an empty formulation canister and the Respimat inhaler was primed to waste. A submicrometer aerosol was generated into a 900 ml drying chamber from a single actuation of the Respimat inhaler.
Initial Particle Size Determination
The initial particle size distributions of the aerosols as they exited the 900 ml drying chamber were determined using the Andersen cascade impactor (ACI; Graseby-Andersen Inc, Smyrna, GA) with airflow conditions identical to those that would be used during the EEG growth experiment. A dual flow mouthpiece, previously introduced by Hindle and Longest (2), was connected to the outlet of the 900 ml drying chamber. Aerosols were sampled directly from the dual flow mouthpiece into the ACI operated at 28 ± 2 L/min and maintained at 25°C by placing it in a temperature and humidity controlled environmental chamber (Espec, Hudsonville, MI). The stage cut-off diameters at 28.3 L/min were 9.0, 5.8, 4.7, 3.3, 2.1, 1.1, 0.65, and 0.4 μm. For the CAG experiment, the aerosol was sampled at 1 L/min from the drying chamber via the aerosol inlet of the dual flow mouthpiece. Additional air (45–55% RH and 25°C) at 27 L/min was delivered to the impactor via the humidified air inlet of the mouthpiece. Similarly for the Respimat experiment, aerosol was sampled at 14 L/min from the drying chamber via the aerosol inlet of the dual flow mouthpiece. Additional air (>90% RH and 25°C, Espec Environmental Chamber, Hudsonville, MI) at 14 L/min was delivered to the impactor via the humidified air inlet of the mouthpiece.
Following aerosol generation, washings using appropriate volumes (5–25 ml) were collected from the impaction plates to determine the drug deposition. A 1:1 admixture of methanol and deionized water was used, and the solutions were then assayed using validated HPLC-UV methods for budesonide and albuterol sulfate, respectively. Volumes were selected to produce final drug concentrations between 1 – 10 ug/ml which were suitable for HPLC analysis and differed between plates. The filter was washed with 25 ml and the solution clarified with a 0.45 μm Millex syringe filter (Fisher Scientific, Pittsburg, PA) prior to HPLC analysis. The mass of drug on each impaction plate was determined and used to calculate both the aerodynamic particle size distributions of the drug aerosol. Aerosol particle size distributions were reported as mass distribution recovered from the impactor. The mass median aerodynamic diameter (MMAD) was defined as the particle size at the 50th percentile on a cumulative percent mass undersize distribution (D50) using linear interpolation. The geometric standard deviation (GSD) was defined as the ratio of the particle size at the 84th percentile on a cumulative percent mass undersize distribution (D84) and the particle size at the 50th percentile on a cumulative percent mass undersize distribution (D50) determined using linear interpolation. At least four replicates of each experiment were performed.
EEG Growth Experimental Setup
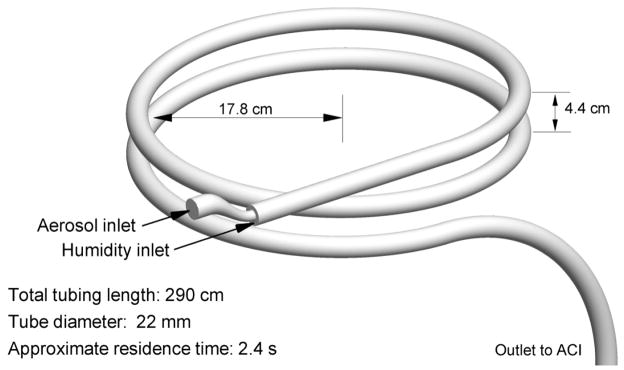
The EEG exposure geometry is illustrated in Figure 1 and is composed of ventilator tubing with an internal diameter of 22 mm wrapped around a 35.6 cm (14 inch) support structure. A coiled tube configuration was selected in order to provide the required residence time in a compact design that could be enclosed in an environmental chamber to control the temperature and humidity. A large diameter of tubing was selected to minimize deposition of the droplets as the aerosol passed through the geometry prior to entering the cascade impactor for sizing. Preliminary CFD simulations were conducted based on the methods described in Longest and Hindle (14) to ensure that aerosol deposition in the model geometry accounted for less than 10% of the delivered drug dose. The EEG exposure geometry was placed in the controlled temperature chamber and supplied with humidified air through the dual flow mouthpiece at 37°C and 99% RH to maintain simulated respiratory thermodynamic conditions. Walls of the growth section were pre-wetted to simulate the wet walled conditions of the respiratory tract, which fosters aerosol growth.
Figure 1.
Coiled tube geometry for evaluating the growth of combination drug-excipient submicrometer particles over a residence time of approximately 2.4 s. The walls of the geometry were wetted before the experiment and supplemental humidified air was supplied to maintain saturation conditions within the model.
In practice, the EEG approach relies on the natural humidity in the lungs to foster aerosol size increase. However, a source of external relative humidity was included in this study to maintain constant thermodynamic conditions within the passive EEG geometry over the time course of the experiments. In these experiments, separate aerosol and humidity streams entered the growth tube inlet through a dual flow mouthpiece, previously introduced by Hindle and Longest (2). Generated aerosols are introduced into the EEG exposure geometry via the aerosol inlet of the dual flow mouthpiece that is connected to the aerosol spacer. For CAG aerosol generation, the aerosol was then sampled into the EEG exposure geometry via the aerosol inlet of the dual flow mouthpiece at 1 L/min. Heated humidified air (37 °C and 99% RH) was supplied to the dual flow mouthpiece humidity entrance at a flow rate of 27 L/min, producing a total flow of 28 L/min in the EEG exposure geometry. This humidified airstream was supplied from a modified compressed air-driven humidifier system (Vapotherm 2000i, Stevensville, MD) which was able to control temperature within ± 0.08 °C at 37.6 °C. Aerosol was sampled into the EEG exposure geometry over a period of approximately 2 minutes. For the Respimat aerosol generation, the aerosol was sampled into the EEG exposure geometry via the aerosol inlet of the dual flow mouthpiece at 14 L/min. Heated humidified air (37 °C and 99% RH) was supplied to the dual flow mouthpiece humidity entrance at a flow rate of 14 L/min (Vapotherm 2000i, Stevensville, MD), producing a total flow of 28 L/min in the EEG exposure geometry. To better approximate bolus aerosol delivery with the Respimat inhaler, the aerosol stream from the drying chamber was pulled into the EEG geometry at a flow rate of 14 L/min over a period of approximately 5 s.
The outlet of the EEG geometry was connected to the inlet of the ACI, which was also in the environmental chamber at 37 °C and operated at a flow rate of 28 L/min, to determine the size distribution of the droplets following exposure to EEG conditions. Drug particle size distributions were obtained as described above for the initial particle sizing.
The temperature and humidity of the humidified air and the temperature of the aerosol mixture stream at the inlet to the EEG test geometry were measured in separate experiments. These measurements were performed using the Humicap Handheld Meter (HMP75B, Vaisala, Helsinki, Finland) positioned at the mid-plane of the tubing and a sheathed Type K thermocouple (Omega Engineering Corp., Stamford, CT) positioned at the mid-plane of the tubing. The Humicap Handheld Meter has a stated temperature accuracy of ±0.2 °C (at 20 °C) and ±0.25 °C (at 40 °C). It has a RH accuracy of ±1.7% (at 20 °C) and ±1.8% (at 40 °C) between 90 – 100 % RH. The probe was factory calibrated using traceable standards and supplied with a NIST calibration certificate. The probe was housed in a plastic filter and incorporated a sensor preheater which was employed to prevent condensation during equilibration prior to measurement.
Effect of Excipient
Budesonide, a non-hygroscopic drug, was selected to investigate the effect of excipient on aerosol growth in the EEG geometry using the CAG as the method of aerosol generation. The excipients evaluated were sodium chloride (NaCl), citric acid (CA) and mannitol (MN). Aerosols were generated with drug:excipient ratios of either 100:0 %w/w (drug only) or 50:50 %w/w from four test formulations containing (i) 0.8 % w/v budesonide, (ii) 0.4 % w/v budesonide and 0.4% w/v NaCl, (iii) 0.4 % w/v budesonide and 0.4% w/v CA (iv) 0.4 % w/v budesonide and 0.4% w/v MN, respectively, in a 50%v/v water and 50% v/v ethanol vehicle.
Effect of Drug:Excipient Ratio
Sodium chloride and citric acid were selected to evaluate effects of the drug:excipient ratio on aerosol growth during the EEG process using budesonide as the model drug with the CAG aerosol generation method. Aerosols were generated with drug:excipient ratios of 25:75, 50:50 and 75:25 %w/w, from the following formulations for NaCl: (i) 0.2 % w/v budesonide and 0.6%w/v NaCl, (ii) 0.4 % w/v budesonide and 0.4% w/v NaCl, (iii) 0.6 % w/v budesonide and 0.2%w/v NaCl, respectively, in a 50%v/v water and 50%v/v ethanol vehicle. Similarly, four aerosols were generated with the same drug:excipient ratios for CA using the following formulations: (i) 0.2 % w/v budesonide and 0.6% w/v CA, (ii) 0.4 % w/v budesonide and 0.4% w/v CA, (iii) 0.6 % w/v budesonide and 0.2% w/v CA, respectively, in a 50%v/v water and 50%v/v ethanol vehicle.
Effect of Drug
EEG aerosol growth was compared for formulations containing budesonide, a non-hygroscopic drug, and albuterol sulfate, a hygroscopic drug, with NaCl as the EEG excipient. CAG aerosols with a drug:excipient ratio of 50:50 %w/w were generated from formulations containing (i) 0.4 % w/v budesonide and 0.4% w/v NaCl and (ii) 0.4 % w/v albuterol sulfate and 0.4% w/v NaCl, in a 50%v/v water and 50%v/v ethanol vehicle.
Effect of Aerosol Generation Method
EEG aerosol growth was evaluated for EEG formulations generated from the soft mist Respimat inhaler and compared with results obtained using the CAG for the same drug and excipient combinations. The formulations employed with the Respimat to generated aerosols with drug:excipient ratios of either 100:0 %w/w (drug only) or 50:50 %w/w were (i) 0.8 % w/v budesonide (ii) 0.4 % w/v budesonide and 0.4%w/v NaCl, (iii) 0.4 %w/v budesonide and 0.4%w/v CA, respectively, in a 10%v/v water and 90%v/v ethanol vehicle.
Statistical Analysis
An aerosol growth ratio was used to evaluate changes in aerosol particle size. The growth ratio was defined as the ratio of the growth MMAD to the mean initial MMAD for the same formulation. Initial MMADs and growth MMADs were compared using a t-test (JMP 9, Cary NC). The effect of excipient type (no excipient (drug only), mannitol, citric acid, and sodium chloride) on the following variables (i) initial MMAD, (ii) growth MMAD and (iii) growth ratio, respectively, was tested using a one-way ANOVA (JMP 9, Cary, NC) for aerosols generated using the CAG with a 50:50 %w/w drug:excipient ratio. A two-way ANOVA (JMP 9, Cary, NC) was used to evaluate the effects of excipient type (sodium chloride and citric acid) and drug:excipient ratio (75:25, 50:50 and 25:75 %w/w) on (i) initial MMAD, (ii) growth MMAD and (iii) growth ratio, respectively, for CAG aerosols. One-way t-test was used to test the effect of drug type (budesonide vs albuterol sulfate) on the growth ratio for aerosols generated using the CAG with a 50:50 %w/w budesonide:NaCl ratio. The effect of excipient type (no excipient (drug only), citric acid, and sodium chloride) on the following variables (i) initial MMAD, (ii) growth MMAD and (iii) growth ratio, respectively, was tested using a one-way ANOVA (JMP 9, Cary, NC) for aerosols generated using the Respimat with a 50:50 %w/w drug:excipient ratio. A two-way ANOVA (JMP 9, Cary, NC) was then used to evaluate the effects of aerosol generator (CAG and Respimat) and excipient (no excipient (drug only), CA and NaCl) on growth ratio for aerosols generated with a 50:50 w/w drug excipient ratio. In all cases, post-hoc comparisons of the means of individual groups were performed using Tukey’s Honestly Significant Difference (HSD) test. A significance level of P < 0.05 denoted significance in all cases. The number of replicate experiments was ≥4 for all experiments.
RESULTS AND DISCUSSION
The EEG concept seeks to combine the high mouth-throat penetration efficiency of submicrometer aerosol particles with the deposition efficiency of micrometer sized particles by utilizing hygroscopic growth during the inhalation cycle of the aerosol particles containing drug and excipient. The first step of the process is the production of submicrometer combination particles containing drug and excipient. In this study, submicrometer combination particles were generated as on-demand spray aerosols from the CAG and Respimat, respectively. The aerosols were generated into a 900 ml spacer which acted as a drying chamber from which the particles were then sampled into the EEG exposure geometry. Due to the heating involved in the CAG process, it was possible to generate submicrometer combination aerosol particles using a vehicle containing 50%v/v water and 50% v/v ethanol. In contrast, for the Respimat, in which the aerosols are formed by impinging spray jets, the vehicle used contained 10%v/v water and 90% v/v ethanol to produce submicrometer combination aerosol particles (26). In both cases, based on analytical estimates, there was sufficient mass transfer potential in the spacer to allow for complete drying of the aerosol spray to produce dry combination particles. However, it should be recognized that the presence of some remaining water in the particles would serve to lower the hygroscopic growth potential of these droplets.
In these studies, aerosol particle size was measured by cascade impaction, two possible sources of error in the sizing process include aerosol evaporation or condensational growth during passage through the impactor, which may affect the initial and growth MMAD measurements. Both phenomena have been associated with thermal changes experienced when aerosols enter the impactor. During these studies, the aerosol and the impactor were maintained at the same temperature in the environmental chamber to minimize any temperature variations. In addition, as described above, previous studies indicated that particles entering the impactor during the initial size measurement were dry and stable and therefore unlikely to be subject to additional size change by evaporation (13). Continued condensational growth during passage through the impactor may cause an over-estimation of the aerosol growth, however the impactor transit time was short compared to the exposure in the EEG growth geometry and constant for each of the EEG growth studies.
Nominal drug doses of 40, 80 and 120 μg were delivered to the drying chamber for the formulations with drug:excipient ratios of 75:25, 50:50 and 25:75 %w/w, respectively. Similarly, the nominal dose delivered from the Respimat with the 50:50 %w/w drug:excipient ratio formulations was 60 μg. These doses may be suitable for delivery of conventional respiratory therapeutics (beta agonists and corticosteroids) due to the expected lower mouth-throat losses of these submicrometer aerosols improving lung deposition efficiency. Impactor recovery was > 75% of the dryer emitted dose in all cases.
Effect of Excipient
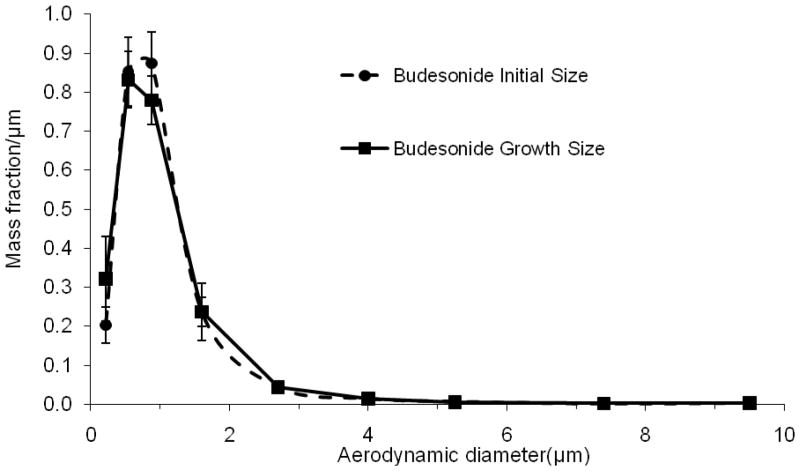
Figure 2 shows the initial aerodynamic particle size distribution for the 0.8 %w/v budesonide (drug only) aerosol generated using the CAG. It was observed to have a mean (SD) initial MMAD of 0.88 (0.07) μm. Table 1 shows that submicrometer combination aerosol particles were produced using the CAG for each of the EEG excipients used in this study when added to the formulation in a 50:50 %w/w mass ratio. There was a significant effect of excipient type on initial MMAD at the p<0.05 level for the formulations [F(3,13) =15.89, p <0.0001]. Post hoc comparisons (Tukey HSD) revealed that there was a significant decrease in the initial MMAD of the aerosols generated with the addition of CA (mean= 0.59, SD =0.1) compared to budesonide alone (mean= 0.88, SD =0.07), perhaps reflecting a change in the CAG aerosol formation process in the presence of this excipient. Geometric standard deviations for the budesonide alone aerosol, budesonide:MN, budesonide:CA and budesonide:NaCl aerosols were 2.06, 2.20, 2.25 and 1.93, respectively.
Figure 2.
Mean (error bars are SD) initial and growth aerodynamic size distributions generated from a 0.8 % w/w budesonide (drug only) formulation in a 50%v/v water and 50% v/v ethanol vehicle using the CAG.
Table 1.
Effect of excipient on the mean (SD) initial aerosol particle size and growth characteristics of submicrometer budesonide particles aerosolized using the capillary aerosol generator (CAG). Formulations were dissolved in water:ethanol (50:50 %v/v) solutions and the drug:excipient ratio was 50:50 %w/w in each study (n≥4 replicates).
| Formulation | Initial MMAD* μm | Growth MMAD* μm | Growth Ratio* |
|---|---|---|---|
| Budesonide | 0.88 (0.07) | 0.91 (0.06) | 1.04 (0.07) |
| Budesonide:Mannitol | 0.90 (0.08) | 2.10 (0.10)** | 2.30 (0.11)** |
| Budesonide:Citric Acid | 0.59 (0.10)** | 1.60 (0.23)** | 2.74 (0.39)** |
| Budesonide:Sodium Chloride | 0.75(0.03) | 2.51 (0.22)** | 3.35 (0.29)** |
P<0.05 Significant effect of excipient on initial MMAD, growth MMAD and growth ratio (One-way ANOVA).
P<0.05 Significant effect of individual excipient on initial MMAD, growth MMAD and growth ratio compared to budesonide alone (Post hoc Tukey HSD).
In order to evaluate the hygroscopic growth of budesonide alone, this aerosol was delivered to the EEG exposure geometry and exposed to 99% RH and 37 °C for the approximately 2 s exposure time occurring between the inlet and exit of the EEG geometry. Figure 2 shows the aerodynamic particle size distribution of the budesonide aerosol following passage through the EEG exposure geometry. There was no difference in the growth MMAD (0.91 (0.06) μm) compared to the initial MMAD (0.88 (0.07) μm) when assessed using a t-test (p=0.63). The non-hygroscopic characteristics of budesonide make it ideal to use as a model drug to allow a direct assessment of the hygroscopic effects of the EEG excipients on aerosol growth. In addition, the absence of any change between the growth MMAD and the initial MMAD suggested that the assumption of dried aerosol particles exiting the drying chamber was correct.
The EEG growth of the budesonide:excipient aerosols was investigated following transit though the exposure geometry. There was a significant effect of excipient type on growth MMAD at the p<0.05 level for the formulations [F(3,15) = 63.61, p<0.0001]. Post hoc analysis (Tukey HSD) revealed that the growth MMAD’s were each significantly different from each other and from the budesonide alone formulation (Table 1). The mean growth MMADs ranged from 1.6 – 2.51 μm for the EEG combination particles. Due to differences in the initial size for the formulations, a growth ratio (growth MMAD / mean initial MMAD) was calculated for each of the individual formulations and used to compare the effects of excipients on aerosol growth. For the budesonide aerosol in the absence of EEG excipients, the non-hygroscopic characteristics of budesonide resulted in no hygroscopic growth and a calculated mean (SD) growth ratio of 1.04 (0.07). In contrast, the mean growth ratios for budesonide combination particles were 2.30 (0.11), 2.74 (0.39), and 3.35 (0.29) when mixed with the excipients of mannitol, citric acid, and sodium chloride, respectively. There was a significant effect of excipient type on growth ratio at the p<0.05 level for the formulations [F(3,15) =57.35, p <0.0001]. Post hoc comparisons (Tukey HSD) revealed that there was a significant difference (p < 0.05) in the growth ratio for each of the excipient formulations compared to the drug only formulation compared to budesonide alone (Table 1). The aerosol containing sodium chloride demonstrated the highest growth ratio of 3.35, with the mean MMAD increasing from 0.75 μm to 2.51 μm.
For these studies, because budesonide is non-hygroscopic, the extent of the hygroscopic growth of the combination particles is related to the hygroscopic properties of the excipients. Longest and Hindle previously introduced a hygroscopic parameter to describe the growth potential of each of the excipients alone or in combination with drug(s) (13). Hygroscopic parameters for MN, CA, and NaCl were calculated to be 8.2, 16.5, and 77.7, respectively. A direct relationship is observed between these hygroscopic parameters and the amount of growth achieved by each excipient in combination with budesonide in the current study. Longest and Hindle (13) then combined the hygroscopic parameter with initial volume fractions of the excipient and drug to develop a growth coefficient relationship and correlations for the growth of combination drug and excipient aerosols. For budesonide combined with the excipients considered in this study at drug:excipient mass ratios of 50:50 %w/w and CAG aerosol production, the growth correlations of Longest and Hindle (13) predict MMAD growth ratios of 2.0 to 3.6 for a 2 s exposure period in the respiratory airways (Equations (23) and (27) of Ref. (13)). These estimates are very similar to the experimental results of the current study with a growth ratio range of 2.3 to 3.35 for 50:50 %w/w budesonide:excipient combination particles. This magnitude of size increase would be sufficient to produce aerosol particles that are suitable for deposition within the airways. Furthermore, the excipients selected in this initial study have all previously been employed in commercially available inhalation drug products. Sodium chloride is a simple salt that is known for its hygroscopic properties and has been widely studied. Citric acid is a weak acid and mannitol is a simple sugar.
Effect of Drug:Excipient Ratio
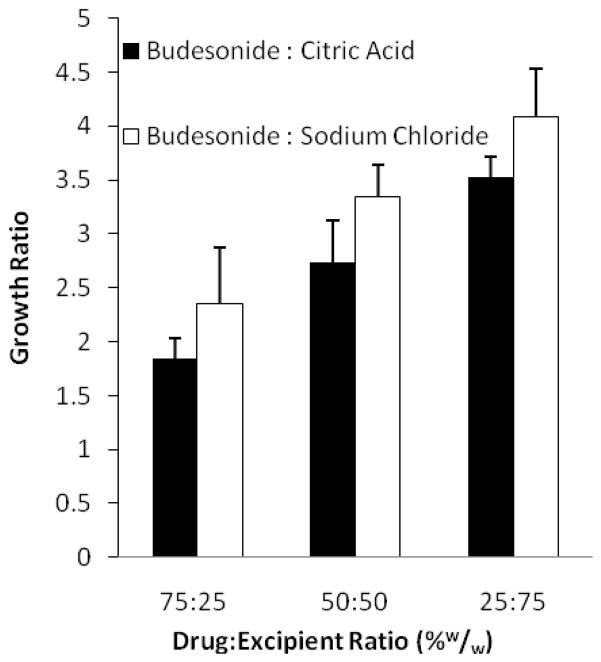
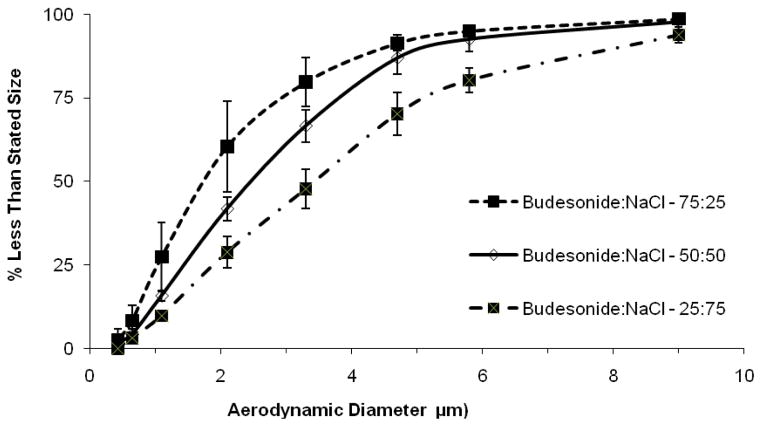
Having established that these hygroscopic excipients are capable of producing significant particle size growth in the EEG exposure geometry, two excipients (CA and NaCl) were selected to examine the effect of changing the drug:excipient ratio on the hygroscopic growth properties of the submicrometer aerosol particles. Table 2 shows the initial MMADs of the aerosols generated from the CAG using formulations containing drug:excipient ratios of 75:25, 50:50 and 25:75 %w/w, respectively, for both CA and NaCl formulations. Two-way ANOVA revealed a significant interaction between excipient type and excipient ratio on the initial MMAD [F(2,21) =11.779, p <0.0004]. For the budesonide:CA combination particle aerosols, there was a significant decrease in initial particle size for the drug:excipient ratio of 25:75 %w/w (mean= 0..40, SD =0.07) compared to the 75:25 %w/w ratio (mean= 0.74, SD =0.12) (Tukey HSD). In contrast, the initial MMADs of the budesonide:NaCl combination aerosol particles were unaffected by changes in the concentration of excipient present. For both excipients, the mean MMADs were indicative of submicrometer aerosols as required for the EEG application in order to efficiently penetrate the mouth-throat region during inhalation. For the budesonide:CA particles, the growth MMADs observed following passage through the EEG exposure geometry ranged from 1.36 μm for the drug:excipient ratio of 75:25 %w/w to 1.6 μm for the 50:50 %w/w ratio and were not statistically different (Tukey HSD). However, considering the growth MMADs for budesonide:NaCl there were significant differences when comparing each of the drug:excipient ratios (Tukey HSD). As described previously, due to differences in the initial size for these combination particles, the growth ratio offers a better comparison of the relative hygroscopic size increase as a function of changing excipient content. The two-factor analysis of variance showed a significant main effect for the excipient type [F(1,20) =14.36, p =0.0011] and for drug:excipient ratio [F(2,20) =44.95, p <0.0001]. There was no significant interaction between excipient and drug:excipient ratio [F(2,20) =0.012, p =0.988]. Table 2 and Figure 3 reveal that the growth ratio increased significantly with increasing excipient content for the budesonide:CA combination particle aerosols (Tukey HSD). Figure 4 shows the cumulative particle size distributions for the budesonide:NaCl combination particle aerosols with drug:excipient ratios of 25:75, 50:50 and 75:25 %w/w, respectively. As with the CA aerosols, there was a significant increase in the growth MMAD with increasing excipient content (Table 2 and Figure 3). For sodium chloride, the most hygroscopic excipient investigated, there was still a large aerosol size increase at the drug:excipient ratio of 75:25 %w/w with a growth ratio of 2.35. Post hoc analysis (Tukey HSD) indicated that the growth ratio was significantly higher for budesonide:NaCl particles compared to budesonide:CA combination particles.
Table 2.
Effect of drug:excipient ratio on the mean (SD) initial aerosol particle size and growth characteristics of submicrometer budesonide particles aerosolized using the CAG. Formulations were dissolved in water:ethanol (50:50 %v/v) solutions (n≥4 replicates).
| Formulation | Drug: Excipient Ratio | Initial MMAD μm* | Growth MMAD μm* | Growth Ratio# |
|---|---|---|---|---|
| Budesonide:Citric Acid | 75:25 | 0.74 (0.12) | 1.36 (0.13) | 1.85 (0.18)*** |
| 50:50 | 0.59 (0.10) | 1.60 (0.23) | 2.74 (0.39)*** | |
| 25:75 | 0.40 (0.07)** | 1.42 (0.07) | 3.53 (0.18)*** | |
| Budesonide:Sodium Chloride | 75:25 | 0.78 (0.12) | 1.83 (0.41)** | 2.35 (0.52)*** |
| 50:50 | 0.75(0.03) | 2.51 (0.22)** | 3.35 (0.29)*** | |
| 25:75 | 0.84 (0.06) | 3.45 (0.37)** | 4.09 (0.44)*** |
P<0.05 Significant interaction between excipient and drug:excipient ratio on the initial MMAD and growth MMAD, respectively (Two-way ANOVA).
P<0.05 Significant main effect of excipient and drug:excipient ratio on growth ratio. No significant interaction (Two-way ANOVA).
P<0.05 Significant effect of drug:excipient for each of the levels on growth MMAD (Post hoc Tukey HSD).
P<0.05 Significant effect of drug:excipient for each of the levels on growth ratio (Post hoc Tukey HSD).
Figure 3.
Effect of drug:excipient ratio on the aerosol growth ratios for combination drug:excipient particles generated from budesonide:CA and budesonide:NaCl EEG formulations aerosolized using the CAG.
Figure 4.
Mean (error bars are SD) cumulative particle size distributions for budesonide:NaCl aerosols generated using the CAG with drug:excipient ratios of 75:25, 50:50 and 25:75 %w/w measured following transit through the EEG exposure geometry.
The effects of changing the drug:excipient ratio on combination particle aerosol growth are important for a number of reasons. Firstly, it may be desirable to maximize the drug payload in the submicrometer combination particle. EEG combination particle formulation will often be required to balance the need for sufficient excipient to produce enhanced particle growth while maintaining sufficient active drug in the particles for the desired therapeutic effect. Even at drug:excipient loadings of 75:25 %w/w, significant growth ratios were observed for CA and NaCl when formulated in combination with the hydrophobic model drug budesonide.
Secondly, one proposed advantage of the EEG approach is the ability to target regional deposition of aerosols within the airways by controlling the hygroscopic growth of the submicrometer combination particles once they have penetrated the mouth-throat region. It may be possible using a combination of selecting the appropriate excipient and formulating at the desired drug:excipient ratio to control the final size of the inhaled aerosol which will determine its regional deposition within the lungs.
Effect of Drug
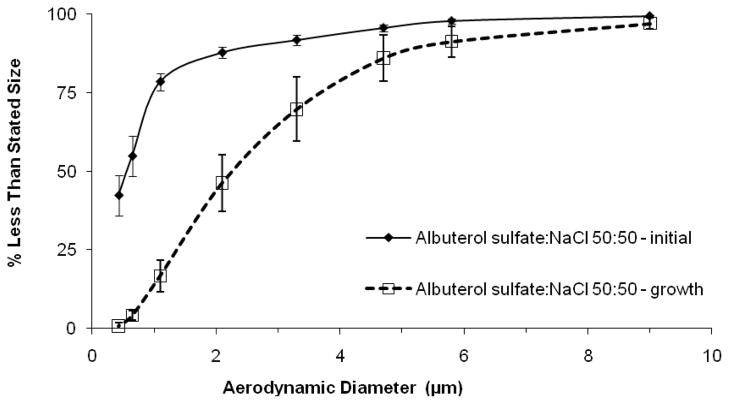
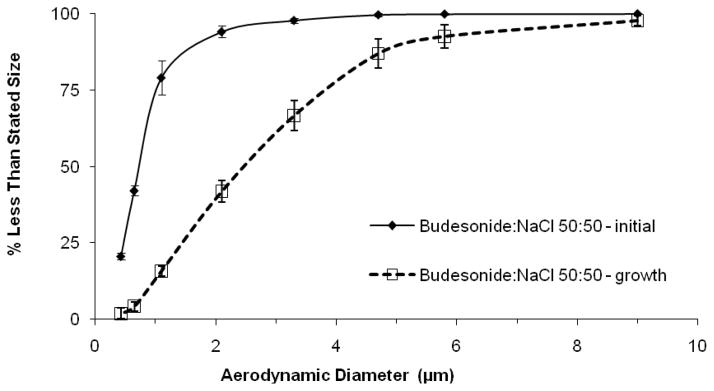
In the previous cases, a non-hygroscopic drug, budesonide, was employed in order to investigate the effects of the excipients in the aerosol formulation and to demonstrate that EEG growth is possible for hydrophobic drugs. Albuterol sulfate was then selected as a model hydrophilic drug and the hygroscopic growth of sodium chloride submicrometer combination aerosol particles was compared with similar budesonide:NaCl particles generated from the CAG. For the albuterol sulfate:NaCl combination particle aerosol with a drug:excipient ratio of 50:50 %w/w, the mean (SD) initial MMAD was 0.57 (0.10) μm. Following RH exposure in the EEG geometry, the growth MMAD was 2.34 (0.47) μm, resulting in a growth ratio of 4.01. The corresponding growth ratio for the budesonide:NaCl formulation with the same drug:excipient ratio was 3.35. A one-way t-test showed a significant increase for the albuterol formulation growth ratio compared to the budesonide formulation (p = 0.026). The significantly larger growth ratio observed for the albuterol sulfate formulation compared to the budesonide formulation is due to the additive hygroscopic effect of the drug in the combination particle. Figures 5 and 6 show the initial and growth cumulative particle size distributions for albuterol sulfate:NaCl and budesonide:NaCl 50:50 %w/w combination particle aerosols, respectively. For the budesonide aerosol, a relatively monodispersed submicrometer combination particle aerosol, with a geometric standard deviation (GSD) of 1.5, underwent hygroscopic growth to produce a more polydispersed micrometer-sized aerosol with a GSD of 2.04. Due to the large submicrometer fraction, the initial size distribution of the albuterol aerosol was relatively polydisperse with a GSD of 3.03; following hygroscopic growth the GSD was 2.1.
Figure 5.
Mean (error bars are SD) initial and growth cumulative particle size distributions for albuterol sulfate:NaCl aerosols (50:50 %w/w) generated using the CAG.
Figure 6.
Mean (error bars are SD) initial and growth cumulative particle size distributions for budesonide:NaCl aerosols (50:50 %w/w) generated using the CAG.
Longest and Hindle reported a hygroscopic parameter of 4.9 for albuterol sulfate (13). Based on these results, the final EEG growth characteristics of the combination particles composing the aerosol are defined by the combined hygroscopic properties of both the drug and excipient.
Effect of Aerosol Generation Method
In order to evaluate the applicability of the EEG approach to other aerosol generation platforms, formulations were developed to produce submicrometer combination particles using the commercially available Respimat inhaler. Zierenberg reported that using an ethanolic solution formulation, the Respimat generated a 1.0 μm aerosol (26). However for the EEG formulations, the selected excipients had limited solubility in ethanol only formulations and therefore 10% v/v water was added to the ethanol formulations for use in the Respimat. As with the CAG studies, the Respimat aerosols were actuated into a 900 ml drying chamber to produce submicrometer combination aerosol particles. Table 3 shows similar initial particle sizes for the aerosols generated using a budesonide only formulation and EEG formulations following the addition of CA and NaCl, respectively. One-way ANOVA revealed no effect of excipient on the initial MMADs of the aerosols generated from the Respimat [F(2,9) =0.32, p =0.733]. Geometric standard deviations for the budesonide alone aerosol, budesonide:CA and budesonide:NaCl aerosols were 1.8, 2.09 and 1.74, respectively. The growth ratio observed for the budesonide formulation was 1.15, which was not significantly different to the value observed with the CAG (1.04) (Tukey HSD). There was a small but significant increase in the particle size of the Respimat-generated budesonide aerosol following transit through the EEG exposure geometry (p=0.024; t-test); the mean (SD) growth MMAD of the budesonide aerosol was 1.01 (0.07) μm. One way ANOVA showed a significant effect of excipient on the growth MMAD of combination particles generated using the Respimat [F(2,9) =45.269, p <=0.0001]. The mean (SD) growth MMADs for the budesonide:CA and budesonide:NaCl aerosols were significantly greater than the growth MMAD for budesonide alone, with values of 2.11 (0.32) μm and 2.60 (0.27) μm, respectively. Two-way analysis of variance again showed a significant main effect for the excipient type [F(2,21) =113.213, p <0.0001], however there was no significant effect for the type of aerosol generation method [F(1,21) =1.7421, p =0.2011]. There was no significant interaction between aerosol generation method and excipient [F(2,21) =1.216, p =0.3164]. The growth ratios for the aerosols generated using the Respimat inhaler with each excipient were not significantly different to those for aerosols generated using the CAG (Table 3), despite the changes in the aerosol formulation vehicle (Tukey HSD). This suggests that the EEG growth is primarily dependent upon the drug and excipient present in the formulation rather than the aerosol generation method and indicates the applicability of this methodology to other aerosol generation devices such as nebulizers, MDIs and DPIs.
Table 3.
Effect of aerosol generator on the mean (SD) initial aerosol particle size and growth characteristics of submicrometer budesonide particles aerosolized using the Respimat inhaler. Formulations were dissolved in water:ethanol (10:90 %v/v) solutions and the drug: excipient ratio was 50:50 %w/w in each study (n≥4 replicates). Also shown for comparison is the growth ratio observed using the CAG for the same drug:excipient combination.
| Formulation | Initial MMAD (μm) | Growth MMAD* μm | Growth Ratio Respimat# | Growth Ratio CAG# |
|---|---|---|---|---|
| Budesonide | 0.88 (0.04) | 1.01 (0.06) | 1.15 | 1.04 |
| Budesonide:Citric Acid | 0.85 (0.09) | 2.11 (0.32)** | 2.48** | 2.74** |
| Budesonide:Sodium Chloride | 0.87 (0.03) | 2.60 (0.27)** | 2.99** | 3.35** |
P<0.05 Significant main effect of inhaler and excipient on growth ratio. No significant interaction (Two-way ANOVA).
P<0.05 Significant effect of excipient on growth MMAD (One-way ANOVA).
P<0.05 Significant effect of individual excipient on growth ratio compared to budesonide alone (Post hoc Tukey HSD).
CONCLUSIONS
Submicrometer combination drug:hygroscopic excipient aerosols, when exposed to simulated respiratory conditions, increased to micrometer size droplets suitable for pulmonary deposition. Growth MMADs ranging from 1.36 to 3.45 μm were observed for the EEG formulations using a non-hygroscopic model drug. It was possible to control the aerosol growth ratio by altering: (1) the hygroscopic excipient, (2) the drug:excipient ratio and (3) the drug. In addition, the applicability of this approach was demonstrated using the CAG and the Respimat inhaler.
The enhanced excipient growth (EEG) approach may enable the high efficiency delivery submicrometer aerosol particles which will then increase in size within the airways and result in nearly complete pulmonary deposition. Future studies will employ numerical and CFD models together with experimental studies to optimize drug:excipient combinations, together with controlling the initial submicrometer particle size, to achieve the required growth kinetics for targeting either the central airways (for beta agonists) or the lung periphery (for systemic applications). Future studies will also investigate using the EEG approach from dry powder formulations.
Acknowledgments
This study was supported by Award Number R21 HL104319 and R01 HL107333 from the National Heart, Lung, And Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute or the National Institutes of Health.
References
- 1.Longest PW, et al. Developing a better understanding of spray system design using a combination of CFD modeling and experiment. In: Dalby RN, et al., editors. Proceedings of Respiratory Drug Delivery 2008. Illinois: Davis Healthcare International Publishing; 2008. pp. 151–163. [Google Scholar]
- 2.Hindle M, Longest PW. Evaluation of enhanced condensational growth (ECG) for controlled respiratory drug delivery in a mouth-throat and upper tracheobronchial model. Pharmaceutical Research. 2010;27:1800–1811. doi: 10.1007/s11095-010-0165-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang Y, Gilbertson K, Finlay WH. In vivo-in vitro comparison of deposition in three mouth-throat models with Qvar and Turbuhaler inhalers. Journal of Aerosol Medicine. 2007;20(3):227–235. doi: 10.1089/jam.2007.0584. [DOI] [PubMed] [Google Scholar]
- 4.Cheng YS, et al. Respiratory deposition patterns of salbutamol pMDI with CFC. HFA-134a formulations in a human airway replica. Journal of Aerosol Medicine. 2001;14(2):255–266. doi: 10.1089/08942680152484180. [DOI] [PubMed] [Google Scholar]
- 5.Leach CL, Davidson PJ, Bouhuys A. Improved airway targeting with the CFC-free HFA-beclomethasone metered-dose inhaler compared with CFC-beclomethasone. European Respiratory Journal. 1998;12:1346–1353. doi: 10.1183/09031936.98.12061346. [DOI] [PubMed] [Google Scholar]
- 6.Byron PR, et al. Stepping into the trachea with realistic physical models: Uncertainties in regional drug deposition from powder inhalers. Respiratory Drug Delivery 2010. 2010;1:215–224. [Google Scholar]
- 7.Newman SP, Busse WW. Evolution of dry powder inhaler design, formulation, and performance. Respiratory Medicine. 2002;96:293–304. doi: 10.1053/rmed.2001.1276. [DOI] [PubMed] [Google Scholar]
- 8.Kamada AK, et al. Issues in the use of inhaled glucocorticoids. American Journal Of Respiratory and Critical Care Medicine. 1996;153(6):1739–1748. doi: 10.1164/ajrccm.153.6.8665030. [DOI] [PubMed] [Google Scholar]
- 9.Borgstrom L, Olsson B, Thorsson L. Degree of throat deposition can explain the variability in lung deposition of inhaled drugs. Journal of Aerosol Medicine. 2006;19:473–483. doi: 10.1089/jam.2006.19.473. [DOI] [PubMed] [Google Scholar]
- 10.Xi J, Longest PW. Transport and deposition of micro-aerosols in realistic and simplified models of the oral airway. Annals of Biomedical Engineering. 2007;35(4):560–581. doi: 10.1007/s10439-006-9245-y. [DOI] [PubMed] [Google Scholar]
- 11.Jaques PA, Kim CS. Measurement of total lung deposition of inhaled ultrafine particles in healthy men and women. Inhalation toxicology. 2000;12(8):715–731. doi: 10.1080/08958370050085156. [DOI] [PubMed] [Google Scholar]
- 12.Longest PW, McLeskey JT, Hindle M. Characterization of nanoaerosol size change during enhanced condensational growth. Aerosol Science And Technology. 2010;44:473–483. doi: 10.1080/02786821003749525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Longest PW, Hindle M. Numerical model to characterize the size increase of combination drug and hygroscopic excipient nanoparticle aerosols. Aerosol Science And Technology. 2011;45:884–899. doi: 10.1080/02786826.2011.566592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Longest PW, Hindle M. CFD simulations of enhanced condensational growth (ECG) applied to respiratory drug delivery with comparisons to in vitro data. Journal of Aerosol Science. 2010;41:805–820. doi: 10.1016/j.jaerosci.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tian G, et al. Characterization of respiratory drug delivery with enhanced condensational growth (ECG) using an individual path model of the entire tracheobronchial airways. Annals of Biomedical Engineering. 2011;39(3):1136–1153. doi: 10.1007/s10439-010-0223-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Longest P, Hindle M. Condensational Growth of Combination Drug-Excipient Submicrometer Particles for Targeted High Efficiency Pulmonary Delivery: Comparison of CFD Predictions with Experimental Results. Pharmaceutical Research. 2011 doi: 10.1007/s11095-011-0596-1. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thudium J. Water-Uptake and Equilibrium Sizes of Aerosol-Particles at High Relative Humidities - Their Dependence on Composition of Water-Soluble Material. Pure and Applied Geophysics. 1978;116(1):130–148. [Google Scholar]
- 18.Haenel G, Zankl B. Aerosol size and relative humidity: Water uptake by mixtures of salts. Tellus. 1979;31(6):478–486. [Google Scholar]
- 19.Gonda I, Byron PR. Perspectives on the Biopharmacy of Inhalation Aerosols. Drug Development and Industrial Pharmacy. 1978;4(3):243–259. [Google Scholar]
- 20.Hickey AJ, Martonen TB. Behavior of Hygroscopic Pharmaceutical Aerosols and the Influence of Hydrophobic Additives. Pharmaceutical Research. 1993;10(1):1–7. doi: 10.1023/a:1018952425107. [DOI] [PubMed] [Google Scholar]
- 21.Hickey AJ, et al. Effect of hydrophobic coating on the behavior of a hygroscopic aerosol powder in an environment of controlled temperature and relative humidity. Journal of Pharmaceutical Sciences. 1990;79(11):1009–1014. doi: 10.1002/jps.2600791113. [DOI] [PubMed] [Google Scholar]
- 22.Hindle M, et al. High efficiency fine particle generation using novel condensation technology. In: Dalby RN, Byron PR, Farr SJ, editors. Proceedings of Respiratory Drug Delivery VI. Buffalo Grove, IL: Interpharm Press, Inc; 1998. pp. 97–102. [Google Scholar]
- 23.Dalby R, Spallek M, Voshaar T. A review of the development of Respimat soft mist inhaler. International Journal of Pharmaceutics. 2004;283:1–9. doi: 10.1016/j.ijpharm.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 24.Longest PW, Hindle M. Evaluation of the Respimat Soft Mist inhaler using a concurrent CFD and in vitro approach. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2009;22(2):99–112. doi: 10.1089/jamp.2008.0708. [DOI] [PubMed] [Google Scholar]
- 25.Longest PW, et al. Numerical simulations of capillary aerosol generation: CFD model development and comparisons with experimental data. Aerosol Science and Technology. 2007;41:952–973. [Google Scholar]
- 26.Zierenberg B. Optimizing the in vitro performance of Respimat. Journal of Aerosol Medicine. 1999;12 (Suppl 1):S19–24. doi: 10.1089/jam.1999.12.suppl_1.s-19. [DOI] [PubMed] [Google Scholar]