Abstract
Context:
Multiple factors have been suggested to increase the risk of faulty dynamic alignments that predict noncontact anterior cruciate ligament injury. Few researchers have examined this relationship using an integrated, multifactorial approach.
Objective:
To describe the relationship among static lower extremity alignment (LEA), hip muscle activation, and hip and knee motion during a single-leg squat.
Design:
Descriptive laboratory study.
Setting:
Research laboratory.
Patients or Other Participants:
Thirty men (age = 23.9 ± 3.6 years, height = 178.5 ± 9.9 cm, mass = 82.0 ± 14.1 kg) and 30 women (age = 22.2 ± 2.6 years, height = 162.4 ± 6.3 cm, mass = 60.3 ± 8.1 kg).
Main Outcome Measure(s):
Pelvic angle, femoral anteversion, quadriceps angle, tibiofemoral angle, and genu recurvatum were measured to the nearest degree; navicular drop was measured to the nearest millimeter. The average root mean square amplitude of the gluteus medius and maximus muscles was assessed during the single-leg squat and normalized to the peak root mean square value during maximal contractions for each muscle. Kinematic data of hip and knee were also assessed during the single-leg squat. Structural equation modeling was used to describe the relationships among static LEA, hip muscle activation, and joint kinematics, while also accounting for an individual's sex and hip strength.
Results:
Smaller pelvic angle and greater femoral anteversion, tibiofemoral angle, and navicular drop predicted greater hip internal-rotation excursion and knee external-rotation excursion. Decreased gluteus maximus activation predicted greater hip internal-rotation excursion but decreased knee valgus excursion. No LEA characteristic predicted gluteus medius or gluteus maximus muscle activation during the single-leg squat.
Conclusions:
Static LEA, characterized by a more internally rotated hip and valgus knee alignment and less gluteus maximus activation, was related to commonly observed components of functional valgus collapse during the single-leg squat. This exploratory analysis suggests that LEA does not influence hip muscle activation in controlling joint motion during a single-leg squat.
Keywords: knee injuries, anterior cruciate ligament, risk factors, posture, malalignment
Key Points.
Static lower extremity alignment characteristics and hip muscle activation were directly related to commonly observed components of functional valgus collapse during the single-leg squat.
However, relationships between static lower extremity alignment and hip muscle activation were not observed.
Static lower extremity alignment may not influence hip muscle activation in controlling joint motion during a single-leg squat.
Multiple factors contribute to the increased risk of non-contact anterior cruciate ligament (ACL) injury. In fact, a recent consensus statement1 has highlighted the need for a more integrated approach across risk-factor categories (eg, anatomical, neuromuscular, and biomechanical). A more comprehensive approach to risk-factor assessment may allow clinicians to accurately identify and understand those relevant risk factors that may contribute to “at-risk” knee positions during dynamic activity.
Among the many risk factors suggested to contribute to ACL injury, neuromuscular function (strength and activation) of the hip musculature has received increased attention because it is essential to providing proximal stability for lower extremity motion.2,3 Neuromuscular deficits may compromise the stability of the hip when it is loaded during weight bearing, resulting in faulty dynamic alignment of the lower extremity and potentially increasing the risk of injury. Authors4–10 of retrospective studies have reported decreased strength and activation of the hip abductors in those with low back pain and lower extremity injuries; however, prospective investigations of the relationship between hip muscle function and lower extremity injury are limited. Only one group11 prospectively examined the relationship between hip strength and lower extremity injury in collegiate basketball and track athletes; those who were injured over the course of the season had less hip abduction and hip extension strength than the uninjured athletes. The authors11 suggested that the decreased strength of the hip musculature reduced the ability to stabilize the hip, resulting in adduction and rotation of the lower extremity and, thus, faulty alignment, which contributed to lower extremity injury. This faulty dynamic alignment, commonly termed “functional valgus collapse”12,13 and characterized by adduction and internal rotation of the hip and knee valgus, predicts ACL-injury risk.14 Whether a relationship exists between decreased neuromuscular hip muscle function and increased functional valgus collapse is currently unknown.
In addition, static lower extremity alignment (LEA) has been proposed as an independent, intrinsic risk factor for ACL injury.12,15,18 Authors19–22 of retrospective studies have reported greater pronation, pelvic angle, and genu recurvatum in ACL-injured individuals. These and other LEA characteristics that increase static hip and knee angles may predispose individuals to increased inward collapse of the knee during dynamic activities.
The limitation of previous examinations of the relationship between anatomical alignment and neuromuscular function of the hip musculature is that only one LEA characteristic or select LEA characteristics were examined. No published studies have addressed the relationship among LEA, neuromuscular function of the hip, and dynamic hip and knee motion using a collective set of anatomic alignment variables that are sufficiently descriptive of lower extremity posture. This relationship may be important because one skeletal malalignment may cause compensatory alignment changes at other bony segments, resulting in abnormal stress patterns or compensatory motions along the kinetic chain.
Given the potential link between decreased neuromuscular function of the hip musculature and increased functional valgus collapse, injury-prevention programs have been developed to target the hip musculature.23 However, the underlying causes for this neuromuscular dysfunction of the hip musculature have received little attention. Differences in LEA may alter neuromuscular function of the hip muscles and contribute to functional valgus collapse. This premise is based on research showing that changes in the length, tension, and orientation of the hip musculature directly influence the internal-moment arms of the muscle, resulting in changes in hip muscle functions.24–26
Few authors have examined the direct influence of LEA on hip muscle function, but differences in LEA may be related to changes in the force and activation of the hip musculature. Using a simulated hip model, an increase in gluteus medius (Gmed) force was necessary to maintain a level pelvis when the femur was positioned in a more internally rotated position (a position associated with femoral anteversion) compared with neutral alignment.27 Further, decreased activation of the Gmed as measured by surface electromyography (sEMG) amplitude was demonstrated in those with increased relative femoral anteversion during isometric strength testing.28 Collectively, these findings indicate that individuals with increased femoral anteversion require increased force production to control the hip and pelvis, yet they demonstrate decreased activation; together, these factors may severely reduce frontal-plane and transverse-plane hip control during functional activities. Whether other alignment factors at the pelvis, knee, lower leg, and foot that promote a more inwardly rotated or adducted hip posture further compromise hip muscle function is unknown.
Although it is tenable that differences in LEA characteristics may change the position of the femur relative to the pelvis, thus potentially altering the length, tension, and orientation of the muscles and their ultimate torque-producing capabilities about a joint, these assumptions are based primarily on findings from a static model. Whether these relationships would hold in a dynamic and constantly changing joint during functional activities is unclear.
Therefore, we examined whether static LEA characteristics and hip muscle activation were related to hip and knee kinematics during a single-leg squat, while accounting for sex and hip strength. Based on retrospective evidence that ACL-injured individuals had greater magnitudes of static LEA19–22 and the potential for alignment to influence the neuromuscular function of the lower extremity muscles,27,28 we wanted to explore both the direct relationships of LEA and hip muscle activation on lower extremity kinematics and the potential for indirect relationships between LEA and lower extremity kinematics based on the association of LEA with hip muscle activation. Specifically, we hypothesized that (1) greater magnitudes of static alignment of the lower extremity and decreased hip muscle activation would directly predict greater functional valgus collapse (increased hip adduction and internal rotation, knee external rotation, and valgus excursion) during a single-leg squat and (2) indirect relationships would also occur such that greater magnitudes of static LEA would predict decreased Gmed and gluteus maximus (Gmax) activation (abduction and extension) and collectively predict greater functional valgus collapse.
METHODS
Thirty men (age = 23.9 ± 3.6 years, height = 178.5 ± 9.9 cm, mass = 82.0 ± 14.1 kg) and 30 women (age = 22.2 ± 2.6 years, height = 162.4 ± 6.3 cm, mass = 60.3 ± 8.1 kg) were recruited from the university and the surrounding community to participate in the study. Each volunteer provided informed consent as approved by the university's institutional review board. Participants had no history of surgery to either lower extremity and no previous hip joint or knee joint injury within the last 6 months. All measurements were taken on the dominant-stance limb (ie, the stance extremity when kicking a ball).
Alignment Measurements
We measured 6 alignment characteristics on the pelvis and lower extremity. These alignment characteristics were based on commonly identified variables suggested to influence dynamic motion and the risk of lower extremity injuries. All measurement procedures were performed by a single examiner who had previously established good to excellent test-retest reliability on all measures (intraclass correlation coefficient [ICC] [2,3] ≥ 0.87),23,29 using techniques that have been previously described in detail.29–32 All standing measures were taken in a standardized stance, with the left and right feet spaced equal to the width between the left and right acromial processes and toes facing forward. The stance was achieved by instructing participants to march in place and then take a step forward. They were advised to look straight ahead during all standing measures, with weight evenly distributed over both feet. Pelvic angle was measured in a standing position using an inclinometer and represented the angle formed by a line from the anterior-superior iliac spine to the posterior-superior iliac spine relative to the horizontal plane.33 Femoral anteversion was measured in a prone position using the Craig test.34 Quadriceps angle was measured in a standing position and represented the angle formed by a line from the anterior-superior iliac spine to the patella center and a line from the patella center to the tibial tuberosity. Tibiofemoral angle was measured in a standing position and represented the angle formed by the anatomical axis of the femur and tibia in the frontal plane.29 Genu recurvatum was measured in supine position with a bolster positioned under the distal tibia and represented the sagittal-plane alignment of the femur and tibia.29 Navicular drop was measured in a standing position and represented the difference between the height of the navicular in subtalar joint neutral and a relaxed stance.29 Each measure was repeated 3 times.
Electromyography Procedures
Surface electromyography signals of the Gmed and Gmax were obtained using a 16-channel Myopac telemetric system (Run Technologies Company, Mission Viejo, CA) with an amplification of 1 mV/V, frequency bandwidth of 10 to 1000 Hz, common mode rejection ratio of 90 dB minimum at 60 Hz, input resistance of 1 MΩ, and an internal sampling rate of 8 KHz. The sEMG signals were detected with 10-mm bipolar Ag-AgCl surface electrodes (Blue Sensor N-00-S; Ambu Products, ∅1-stykke, Denmark; diameter = 44.8 × 22 mm; skin contact size = 30 × 22 mm) with a center-to-center distance of 20 mm and the electrodes were positioned according to procedures described by Cram and Kasman.35 Electrodes were placed on the Gmed at a position one-third the distance from the greater trochanter to the iliac crest. Electrode placement on the Gmax was midway between the greater trochanter and the first sacral vertebrae. The sEMG electrodes were oriented perpendicular to the length of the muscle fibers and placed over the midbelly. The reference electrode was secured to the medial aspect of the tibia. Before the electrodes were attached, we thoroughly cleaned all skin areas with isopropyl alcohol. Myoelectric data were acquired, stored, and analyzed using DataPac 2K2 laboratory application software (version 3.13; Run Technologies Company) during the maximal voluntary isometric contractions (MVICs) and the single-leg squat.
Strength Assessment
A dynamometer (model 3; Biodex Medical Systems, Inc, Shirley, NY) was used to record hip abduction and hip extension MVICs. Participants performed 3 trials of a 3-second MVIC for each muscle, with a 30-second rest period separating trials. We modified a technique described by Carcia et al36 to measure hip abduction torque in weight bearing. Volunteers stood adjacent to the dynamometer, looking straight ahead, with the trunk erect, feet facing forward, and arms crossed over the chest. The dynamometer axis was aligned with the head of the femur, determined by the intersection of a medially directed horizontal line from the greater trochanter and a distally directed vertical line from the anterior-superior iliac spine.37 The resistance arm of the dynamometer was positioned on the lateral side of the nonstance leg, with the distal edge of the pad approximately 5 cm proximal to the lateral joint line and the hip positioned in approximately 5° of abduction. Each participant performed the MVIC by abducting the hip while supporting his or her body weight on the dominant-stance limb and maintaining an erect posture. For assessment of hip extension torque, each individual performed hip extension in the supine position, with the hip flexed to 90° and the dynamometer axis aligned with the greater trochanter. The resistance arm was positioned on the posterior thigh just proximal to the knee joint line. Previous work in our laboratory using these identical MVIC measurement protocols demonstrated good to excellent day-to-day reliability of torque production for standing hip abduction (ICC[2,k] = 0.91, SEM = 0.03 N·m/kg) and hip extension (ICC[2,k] = 0.80, SEM = 0.46 N·m/kg).
Kinematic Analysis
Kinematic data for the pelvis, thigh, shank, and foot were sampled at 100 Hz using 6–degrees-of-freedom electromagnetic sensors (Ascension Technology Corporation, Burlington, VT) and Motion Monitor Software (Innovative Sports Training, Inc, Chicago, IL) during the single-leg squat. Electromagnetic position sensors were attached with double-sided tape and elastic wrap over the anterior midshaft of the third metatarsal, the midshaft of the medial tibia, and the lateral aspect of the midshaft of the femur of the dominant-stance limb. An additional sensor was secured on the sacrum. Digitization procedures were performed using the default selection with a segmental reference system defining body segments: the positive x-axis was defined as the posterior-to-anterior axis, the positive y-axis was defined as the distal-to-proximal longitudinal axis, and the positive z-axis was defined as the medial-to-lateral axis. An initial neutral position was established in a standardized stance with the left and right feet spaced equal to the width between the left and right acromion processes and the toes facing forward. The ankle and knee joint centers were estimated using the centroid method, whereby the ankle joint center was calculated as the midpoint between the digitized medial and lateral malleoli, and the knee joint center was calculated by the midpoint between the digitized medial and lateral femoral epicondyles. The hip joint center was determined by the Leardini et al38 method.
The starting position for participants was feet shoulder-width apart, hips and knees extended, toes facing forward, equal weight on both feet, and thumbs lightly touching the iliac crests (Figure 1). A plywood board was positioned at a distance anterior to the knee while volunteers performed a double-leg squat to 60° of knee flexion based on real-time goniometer values. The plywood board was positioned to provide individuals with feedback indicating that they had reached 60° of knee flexion during each trial and while performing a double-leg squat to ensure proper placement of the board. They then performed a single-leg squat with instructions to squat straight down until they touched the board with the knee while looking straight ahead. A string was positioned perpendicular to the first toe at the level of the chest to monitor forward flexion of the trunk (Figure 2). Participants were instructed to maintain an upright position without flexing the trunk forward or to the side in order to limit the influence of trunk motion on the hip musculature. Although we recognize that this is a constrained task, the rationale for this standardized positioning was to account for a potential confounding factor that may have contributed to conflicting results in previous studies of hip muscle activation during dynamic tasks.39,40 Compared with men, women had greater Gmax activation during a single-leg squat39 but less activation during single-leg landings.40 Small sample sizes and methodologic considerations in performing the tasks may explain these contrasting findings. Specifically, trunk motion, which has a direct influence on activation of the hip musculature, did not appear to be controlled in these studies.41
Figure 1.
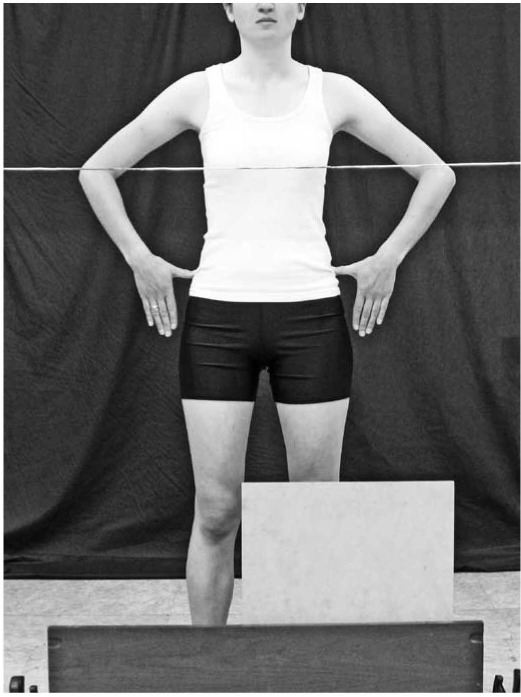
Starting position for the kinematic data collection with feet shoulder-width apart, hips and knees extended, toes facing forward, equal weight on both feet, and thumbs lightly touching the iliac crests.
Figure 2.
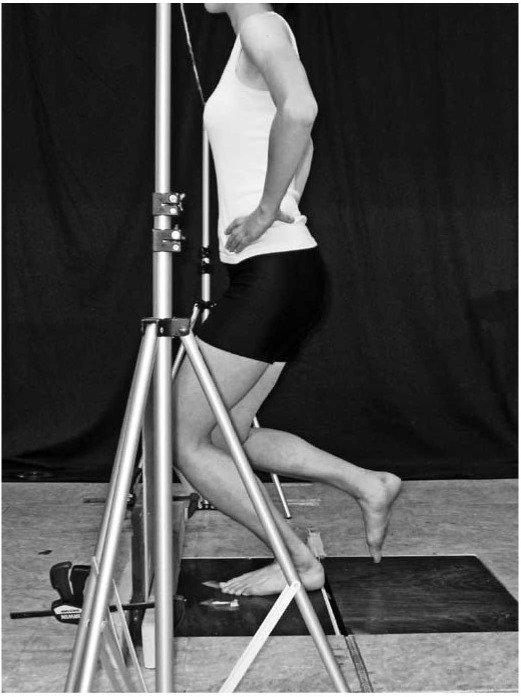
The single-leg squat was performed to 60° of knee flexion. A string was positioned perpendicular to the first toe at the level of the chest to monitor forward flexion of the trunk during the single-leg squat.
Each single-leg squat trial was initiated by a verbal command from the examiner and performed at a speed of 5 seconds from the starting position to 60° of knee flexion. The rate of the task was controlled by a metronome set at a cadence of 60 beats per minute. Participants transitioned from bilateral stance to single-leg stance during the first 2 beats with the nonstance knee and hip flexed approximately 45° and 0°, respectively. The squat then began on the third beat and ended at 60° of knee flexion on the fifth beat (total squat time = 2 seconds). A force plate marked the transition from double-leg stance to single-leg stance, and 60° of knee flexion marked the end of the trial. Volunteers were allowed sufficient practice to ensure that the task was performed properly, and data were then collected during 5 acceptable trials. A trial was deemed unacceptable if the individual (1) touched the string (indicating increased forward flexion of the trunk), (2) touched the nonstance leg to the ground or the stance leg, (3) lifted either hand off the iliac crest, or (4) failed to reach 60° of knee flexion as confirmed by real-time goniometry.
Data Reduction and Analyses
The average of 3 measurements for each LEA characteristic was used for analyses. Dynamometer torque data were recorded as the maximum peak torque obtained from 3 MVIC trials each for hip abduction and hip extension. Peak torque was then normalized to the participant's body mass and reported in newton-meters per kilogram of body mass. Kinematic signals from the position sensors were low-pass filtered at 12 Hz using a fourth-order, zero-lag Butterworth filter. Hip and knee angles were calculated using Euler angle definitions with a rotational sequence of Z X′ Y″.42 Initial joint angles were calculated as the average joint positions during the first second after transition from double-leg to single-leg stance. Final joint angles were determined as the value when participants achieved 60° of knee flexion. Single-leg squat joint excursions were calculated as the difference (final minus initial) for each trial, and the average across 5 trials was used for statistical analysis.
The sEMG of the Gmed, and Gmax during the MVIC and single-leg squat trials was filtered from 10 Hz to 350 Hz using a fourth-order, zero-lag Butterworth filter and then processed using a centered root mean square (RMS) algorithm with 100-millisecond time constant. The peak RMS value obtained over 3 MVIC trials for each muscle was used to normalize the sEMG data during the single-leg squat. The average RMS amplitude of the 5 single-leg squat trials across the entire trial (after transition to single-leg weight bearing to 60°) was then normalized to the individual's MVIC peak RMS value and reported as a percentage of the MVIC.
Structural equation modeling was used to evaluate whether increased LEA and decreased hip muscle activation (Gmed and Gmax, considered separately) predicted greater functional valgus collapse (characterized by increased hip adduction and internal rotation, knee external rotation, and valgus excursion) during a single-leg squat while accounting for the individual's sex and hip strength. Our rationale in accounting for these additional variables was that LEA characteristics31 and hip strength11,43–45 are known to differ by sex and that muscle-activation amplitude of the primary hip abductor (Gmed) and hip extensor (Gmax) muscles may, in part, depend on their absolute force-producing capabilities.46 Hip abduction and hip extension strength were included only in the specific path models that examined the relationships of Gmed and Gmax activation, respectively, as they are the primary muscles that perform hip abduction and hip extension. The path diagram examining these relationships is illustrated in Figure 3.
Figure 3.
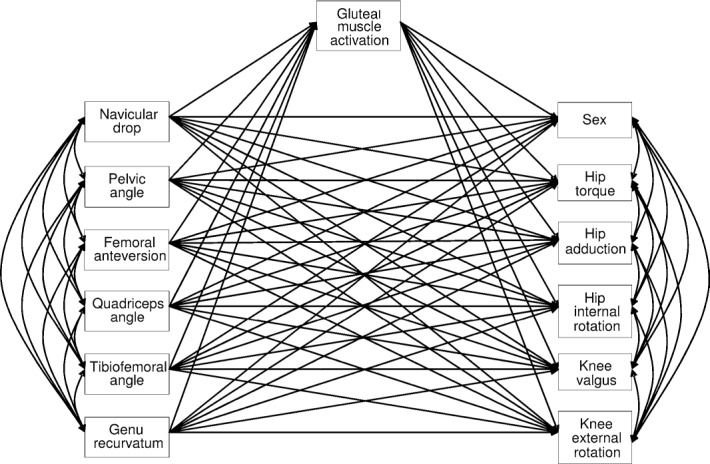
Full path model for the dependent variables gluteal muscle activation and functional valgus collapse.
Path analysis is an extension of multiple linear regressions with the purpose of modeling explanatory chained relationships between observed variables. It provides estimates of the magnitude and significance of hypothesized causal connections among sets of variables. Path analysis provides a statistical approach to understanding comparative strengths of direct and indirect relationships among a set of variables.47 Because the total number of variables being estimated was greater than the total sample size (resulting in the variable estimates being highly unreliable), each full model was reduced to a more stable model by first removing the dependent measures that had no statistically significant paths (ie, variables that had no significant predictors), followed by removing the predictor variables that did not approach significance or were nonsignificant in explaining any of the remaining outcome measures (dependent variables). Statistical significance was determined by the t-value statistic, which reflects the ratio of the variable estimate to its standard error. A t value greater than +2 or less than −2 is considered statistically significant.47 All path analyses were performed using LISREL (version 8.72; Scientific Software International, Inc, Lincoln wood, IL).
RESULTS
Measures of LEA, hip muscle activation, joint excursion during the single-leg squat, and hip torque are summarized in Table 1. The mean static alignment values are within the range of normal values reported in healthy adults using identical measurement methods.29–31 Sex was related to LEA characteristics and hip muscle activation (all P < .05): women had greater pelvic angle (t = 2.23), femoral anteversion (t = 4.60), quadriceps angle (t = 2.58), tibiofemoral angle (t = 3.09), genu recurvatum (t = 3.84), and Gmax activation (t = 2.44) than men. The inferential goodness-of-fit index indicated that both full models were a perfect fit (χ20 = 0.00, P = 1.00, RMS error of approximation = 0.00) because the model was saturated with 0 degrees of freedom.
Table 1.
Descriptive Statistics for Dependent and Predictor Variables
| Measure | Mean ± SD | Median | Range |
| Lower extremity alignment | |||
| Pelvic angle, ° | 11.1±4.6 | 11.0 | 0.0 to 21.0 |
| Hip anteversion, ° | 10.7 ± 5.2 | 9.8 | 1.0 to 27.7 |
| Quadriceps angle, ° | 12.9 ± 5.6 | 12.0 | 1.0 to 29.0 |
| Tibiofemoral angle, ° | 10.7 ± 2.0 | 10.7 | 5.0 to 15.3 |
| Genu recurvatum, ° | 3.8 ± 3.8 | 3.0 | −1.3 to 14.3 |
| Navicular drop, mm | 6.6 ± 6.0 | 6.3 | −4.0 to 25.7 |
| Muscle activation, % maximum voluntary isometric contraction | |||
| Gluteus medius | 0.27 ± 0.13 | 0.23 | 0.11 to 0.72 |
| Gluteus maximus | 0.20 ± 0.19 | 0.14 | 0.03 to 1.04 |
| Joint excursion, ° | |||
| Hip adduction | 11.4 ± 10.4 | 12.0 | −15.3 to 35.5 |
| Hip internal rotation | −2.3 ± 5.9 | −1.6 | −16.4 to 12.8 |
| Knee valgus | −0.1 ± 8.0 | −0.4 | −23.5 to 17.0 |
| Knee external rotation | 2.7 ± 6.1 | 2.2 | −9.8 to 20.2 |
| Hip strength, N·m/kg | |||
| Hip-abduction torque | 0.69 ± 0.19 | 0.66 | 0.37 to 1.33 |
| Hip-extension torque | 3.46 ± 1.05 | 3.43 | 1.87 to 5.80 |
Relationship Among LEA, Gmed Activation, and Joint Excursion
The full model used to examine the extent to which LEA characteristics predicted Gmed activation and the variables' collective influence on dynamic alignment during a single-leg squat while accounting for sex and hip abduction torque was reduced to a more stable model (Figure 4). The variables that remained in the model were the dependent variables of hip internal-rotation and knee external-rotation excursions and the predictor variables of pelvic angle, femoral anteversion, tibiofemoral angle, and navicular drop. The coefficients, standard errors of the coefficients, and t statistics for paths P1–15 that represent the relationships among the remaining variables are shown in Table 2.
Figure 4.
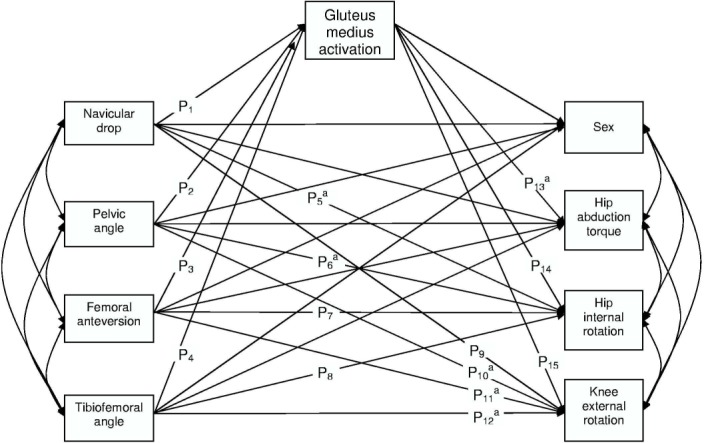
Final model for the dependent variables gluteus medius activation and dynamic valgus alignment. aIndicates significant path coefficient. See Table 2 for path coefficient values.
Table 2.
Path Coefficients of Lower Extremity Alignment Predicting Gluteus Medius Activation, Hip Internal Rotation, and Knee External Rotation
| Lower Extermity Alignment | Gluteus Medius Activation |
Hip Internal Rotation |
Knee External Rotation |
|||||||||
| Path | Path Coefficient | Standard Error | t value | Path | Path Coefficient | Standard Error | t value | Path | Path Coefficient | Standard Error | t value | |
| Navicular drop | P1 | 0.13 | 0.15 | 0.87 | P5 | 0.36 | 0.14 | 2.67a | P9 | 0.17 | 0.13 | 1.33 |
| Pelvic angle | P2 | −0.03 | 0.14 | −0.21 | P6 | −0.30 | 0.13 | −2.29a | P10 | −0.29 | 0.13 | −2.31a |
| Femoral anteversion | P3 | 0.04 | 0.14 | 0.31 | P7 | 0.21 | 0.13 | 1.60 | P11 | 0.34 | 0.12 | 2.77a |
| Tibiofemoral angle | P4 | 0.13 | 0.14 | 0.92 | P8 | −0.03 | 0.13 | −0.21 | P12 | 0.27 | 0.12 | 2.14a |
| Gluteus medius activation | P14 | −0.03 | 0.12 | −0.20 | P15 | 0.21 | 0.12 | 1.73 | ||||
aSignificant path coefficient (P < .05)
The model explained 17% of the variance in hip internal-rotation excursion and 24% of the variance in knee external-rotation excursion during the single-leg squat. Smaller pelvic angle (P6) and greater navicular drop (P5) predicted greater hip internal-rotation excursion, whereas smaller pelvic angle (P10) and greater femoral anteversion (P11) and tibiofemoral angle (P12) predicted greater knee external-rotation excursion during the single-leg squat. The model did not identify any indirect (ie, “sequential” or “chained”) relationships between LEA and Gmed activation in predicting joint excursion during the single-leg squat.
Relationship Among LEA, Gmax Activation, and Joint Excursion
The full model used to examine the extent to which static LEA predicted Gmax activation and the variables' collective influence on dynamic alignment during a single-leg squat while accounting for sex and hip extension torque was also reduced to a more stable model (Figure 5). The variables that remained in the model were the dependent variables of hip internal-rotation, knee valgus, and knee external-rotation excursion and the predictor variables of pelvic angle, femoral anteversion, tibiofemoral angle, and navicular drop. The coefficients, standard errors of the coefficients, and t statistics for paths P1–P20 that represent the relationships among the remaining variables are shown in Table 3.
Figure 5.
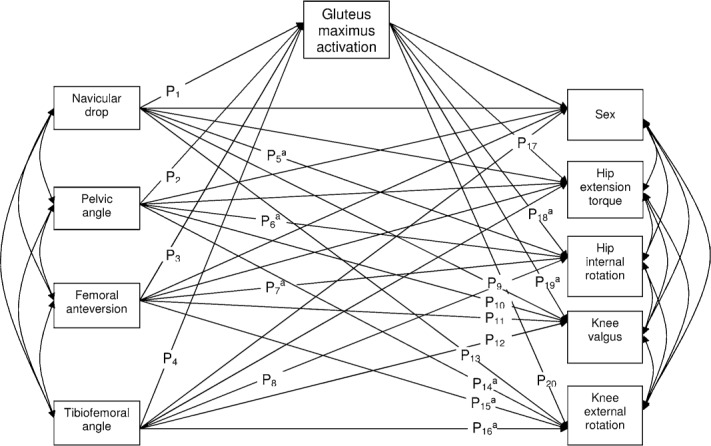
Final model for the dependent variables gluteus maximus activation and dynamic valgus alignment. aIndicates significant path coefficient. See Table 3 for path coefficient values.
Table 3.
Path Coefficients of Lower Extremity Alignment Predicting Gluteus Maximus Activation, Hip Internal Rotation, Knee Valgus and Knee External Rotation
| Lower Extermity Alignment | Gluteus Medius Activation |
Hip Internal Rotation |
Knee Valgus |
Knee External Rotation |
||||||||||||
| Path | Path Coefficient | Standard Error | t value | Path | Path Coefficient | Standard Error | t value | Path | Path Coefficient | Standard Error | t value | Path | Path Coefficient | Standard Error | t value | |
| Navicular drop | P1 | −0.03 | 0.14 | −0.19 | P5 | 0.35 | 0.13 | 2.76a | P9 | 0.09 | 0.14 | 0.68 | P13 | 0.20 | 0.13 | 1.50 |
| Pelvic angle | P2 | 0.14 | 0.14 | 1.01 | P6 | −0.26 | 0.13 | −2.04a | P10 | 0.14 | 0.13 | 1.08 | P14 | −0.30 | 0.13 | −2.26a |
| Femoral anteversion | P3 | 0.19 | 0.14 | 1.42 | P7 | 0.27 | 0.12 | 2.17a | P11 | 0.03 | 0.13 | 0.19 | P15 | 0.36 | 0.13 | 2.74a |
| Tibiofemoral angle | P4 | 0.04 | 0.14 | 0.31 | P8 | −0.02 | 0.12 | −0.14 | P12 | 0.13 | 0.13 | 1.04 | P16 | 0.29 | 0.13 | 2.32a |
| Gluteus maximus activation | P18 | −0.32 | 0.12 | −2.70a | P19 | 0.31 | 0.13 | 2.41a | P20 | −0.01 | 0.13 | −0.10 | ||||
aSignificant path coefficient (P < .05)
The model explained 27% of the variance in hip internal-rotation excursion, 17% of the variance in knee valgus excursion, and 20% of the variance in knee external-rotation excursion during the single-leg squat. Smaller pelvic angle (P6) and greater femoral anteversion (P7) and navicular drop (P5) predicted greater hip internal-rotation excursion, whereas smaller pelvic angle (P14) and greater femoral anteversion (P15) and tibiofemoral angle (P16) predicted greater knee external-rotation excursion during the single-leg squat. Decreased Gmax activation predicted greater hip internal-rotation (P18) and decreased knee valgus (P19) excursion. Similar to the previous model, we did not identify any indirect relationships between LEA and Gmax activation in predicting joint excursion during the single-leg squat.
DISCUSSION
The primary findings were that LEA characteristics were directly related to dynamic alignment during a single-leg squat, with greater femoral anteversion, tibiofemoral angle, and navicular drop predicting greater hip internal-rotation excursion and knee external-rotation excursion. Interestingly, greater pelvic angle predicted decreased hip and knee rotation. Direct relationships were also noted between gluteal activation and dynamic alignment, with decreased Gmax activation predicting greater hip internal-rotation excursion but decreased knee valgus excursion. These results provide empirical support for previous theories that differences in static LEA and gluteal muscle activation contribute to greater hip joint and knee joint excursions during functional activities. However, no indirect (ie, sequential or chained) relationships were noted between LEA and gluteal activation in predicting dynamic motion: no LEA characteristic predicted Gmed or Gmax muscle activation during the single-leg squat once an individual's sex and muscle strength were accounted for.
Effects of LEA and Hip Muscle Activation on Lower Extremity Joint Excursion
Based on prevailing theories, greater static hip and knee alignment and decreased hip activation were hypothesized to predict greater frontal- and transverse-plane joint excursion during the single-leg squat. Specifically, individuals with more femoral anteversion and navicular drop went into more hip internal-rotation excursion and individuals with greater tibiofemoral angle and femoral anteversion went into greater knee external-rotation excursion, with both motions considered important components of functional valgus collapse.12 The direct relationship between greater femoral anteversion and greater rotation of both the hip and knee during dynamic motion seems logical given that more femoral anteversion has previously been associated with hip internal rotation and contributes to a compensatory increase in knee external rotation.48 These observed relationships suggest that static LEA characteristics may directly influence dynamic hip and knee angles during functional activities and may offer a potential mechanism by which greater navicular drop and static knee valgus angles were associated with ACL injury.19–22 An explanation for greater pelvic angle predicting decreased hip internal-rotation and knee external-rotation excursion is unclear. Based on retrospective evidence21 that suggests a relationship between greater anterior pelvic angle and ACL injury, our expectation was that more anterior pelvic tilt would be related to more dynamic joint excursion. Additional work is needed to better understand the interaction between the pelvis and the femur and its influence on dynamic alignment and ACL injury.
The hypothesized relationship between hip muscle activation and functional valgus collapse was partially supported. Decreased Gmax activation predicted greater hip internal-rotation excursion. Although we found no studies that directly examined the relationship between hip muscle activation and joint motion in healthy individuals, this observed relationship does support current theories that decreased hip muscle activation may affect dynamic stability of the hip, resulting in an inability to maintain neutral alignment during single-limb weight-bearing activities.39,49–51 However, the positive relationship of greater Gmax activation predicting greater knee valgus excursion is the opposite of what we expected. An explanation of this positive relationship is unclear, but it may be that hip activation strategies are different when controlling motions at the hip compared with motions at the knee. Dynamic knee valgus observed during functional tasks may reflect a combined motion of knee valgus and hip internal rotation, which would further suggest a positive relationship between Gmax activation and these motions. However, further examination of our data indicated that hip internal rotation was negatively correlated with knee valgus excursion (r = −0.370, P = .004). This observed relationship between hip joint and knee joint motion may be specific to a single-leg squat task, and, therefore, further studies are needed to determine whether the observed relationships between hip muscle activation and lower extremity kinematics are consistent across functional tasks.
Although we observed direct relationships between LEA and joint excursion, it is unclear from these data alone if static LEA directly predisposes individuals to the rotational hip and knee components of functional valgus collapse or whether these postural effects act through resulting biomechanical changes (ie, decreased hip muscle activation) to increase dynamic hip and knee malalignments. The use of a path analysis model was a novel approach toward examining multiple risk factors, which allowed us to examine the indirect relationships between LEA and functional valgus collapse by way of their effects on hip muscle activation. We hypothesized that static malalignments would directly predict decreased hip muscle activation, which would further predict increased joint excursion.
However, this sequential or chained relationship was not observed: no static LEA characteristic was related to dynamic hip muscle activation. Relationships between LEA and hip muscle function have been observed using static models, but our results do not support this relationship during dynamic activities when joint position is constantly changing. These findings suggest that static LEA alone may predispose individuals to greater hip and knee rotations during dynamic activity, independent of Gmax or Gmed activation during dynamic tasks.
Accounting for Sex and Hip Muscle Strength
We chose to account for sex in the path-analysis models because many of the LEA characteristics31 and hip muscle-activation measures39,40 we examined are known to differ by sex. By accounting for sex in the model, we confirmed that sex was related to LEA characteristics and hip muscle activation such that women had greater pelvic angle, femoral anteversion, quadriceps angle, tibiofemoral angle, genu recurvatum, and Gmax activation than men. These sex differences in LEA characteristics and hip muscle activation may in part explain why females demonstrate greater dynamic knee angles and an increased risk of ACL injury. Future authors should examine males and females separately because the relationships between many of the postulated risk factors and ACL injury may not be the same for each sex.
The purpose of accounting for hip abduction and hip extension strength in the path analyses was to better clarify the relationship between hip muscle activation and functional valgus collapse by taking into consideration variations in the levels of hip strength among participants, which may itself explain differences in functional valgus collapse. Although authors have examined activation of the hip musculature during functional activities such as single-leg landings and single-leg squats, either kinematic data were not collected40 or hip strength was not reported.39,40 Based on these studies, the relationship between posterior-lateral hip muscle function and dynamic joint motion remains unclear. In theory, greater hip muscle activation would be necessary to successfully perform a desired motion in the presence of reduced hip muscle strength. The negative relationships we observed between hip abduction torque and Gmed activation (r = −0.275, P = .034) and between hip extension torque and Gmax activation (r = −0.612, P < .001) confirm that greater posterior-lateral hip muscle activation was required in those individuals with decreased hip strength to successfully perform the single-leg squat. This inverse relationship between hip muscle strength and activation suggests that relative increases in gluteal muscle activation may or may not, by themselves, indicate better hip control, depending on the actual torque-producing capabilities of the muscles.
Limitations
We acknowledge that measurement of femoral anteversion using clinical methods has the potential for inconsistencies, with a range of reliabilities and validities of this measure reported in the literature. The measurement technique we used was based on original work by Ruwe et al,34 who reported good reliability between testers and high correlations with intraoperative measurements. Consistent with other authors who have reported high intratester29,52 and intertester reliability,52 the tester in this study had more than 10 years of clinical experience and had established a high level of reliability on this measure. However, a recent group53 has since reported that clinical measurements of femoral anteversion were underestimates compared with values obtained via magnetic resonance imaging, questioning the validity of the Craig test in assessing femoral anteversion. Our observed relationships between femoral anteversion and dynamic alignment, which were consistent with our hypotheses, indicate that the clinical measurement of femoral anteversion represents some anatomical aspect of hip rotation and remains an important factor to consider when examining risk of ACL injury. Further work is needed to identify the underlying characteristics being assessed using the clinical measurement method.
Aside from femoral anteversion, all primary variables were assessed while the participants were weight bearing in an effort to better represent a functional position. However, hip extension torque was measured nonweight bearing, and more work is required to confirm if relationships between strength and Gmax activation would remain consistent if both were assessed in a more functional position. Our findings are limited to the dominant-stance limb of healthy, college-aged adults and should not be generalized to other populations. Further, these findings are limited to a controlled, functional single-leg squat task performed in an upright position. Although we felt it was important to control the influence of various trunk positions on hip muscle activation41 that might have contributed to inconsistent findings from previous studies,39,40 we acknowledge that this upright position may not be fully representative of more unconstrained dynamic tasks potentially associated with ACL injury.
CONCLUSIONS
A more integrated approach to risk-factor assessment is needed to accurately identify and understand those relevant risk factors that may contribute to at-risk knee positions during dynamic activity. The overall findings of this study revealed that LEA characteristics clinically associated with static malalignment and hip muscle activation were directly related to commonly observed components of functional valgus collapse during the single-leg squat. However, this exploratory analysis did not identify any indirect relationships between LEA and Gmax activation in predicting joint excursion and suggests that LEA does not influence hip muscle activation in controlling joint motion during a single-leg squat. Future researchers should continue to examine the other factors that influence hip muscle activation and the mechanisms that explain the relationships between static and dynamic malalignments.
Although the identified relationships were statistically significant, the associated path coefficients were somewhat low, which indicates that other factors could combine with LEA and hip muscle activation to further affect dynamic motion. Future investigators should confirm whether the relationship among LEA, hip muscle activation, and dynamic malalignment is consistent across a variety of functional tasks. In addition, continued examination of differences in LEA characteristics among both older and younger individuals is needed to determine whether these postures change with maturity. This research will aid clinicians in determining the most appropriate time to initiate posterior-lateral hip strengthening programs with the goal of reducing injury. Continued work in these areas will help clinicians more effectively identify those at greater risk for injury and, therefore, help us to develop intervention strategies to reduce the risk of noncontact ACL injury.
Acknowledgments
This study was funded in part by the NATA Research & Education Foundation.
REFERENCES
- 1.Shultz SJ, Schmitz RJ, Nguyen AD. Research Retreat IV: ACL injuries— the gender bias: April 3–5, 2008, Greensboro, NC. J Athl Train. 2008;43(5):530–531. doi: 10.4085/1062-6050-43.5.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumagai M, Shiba N, Higuchi F, Nishimura H, Inoue A. Functional evaluation of hip abductor muscles with use of magnetic resonance imaging. J Orthop Res. 1997;15(6):888–893. doi: 10.1002/jor.1100150615. [DOI] [PubMed] [Google Scholar]
- 3.Moore KL. Clinically Oriented Anatomy. Baltimore, MD: Williams & Wilkins; 1992. p. 917. [Google Scholar]
- 4.Beckman SM, Buchanan TS. Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Arch Phys Med Rehabil. 1995;76(12):1138–1143. doi: 10.1016/s0003-9993(95)80123-5. [DOI] [PubMed] [Google Scholar]
- 5.Ireland ML, Wilson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33(11):671–676. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- 6.Brindle TJ, Mattacola C, McCrory J. Electromyographic changes in the gluteus medius during stair ascent and descent in subjects with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2003;11(4):244–251. doi: 10.1007/s00167-003-0353-z. [DOI] [PubMed] [Google Scholar]
- 7.Friel K, McLean N, Myers C, Caceres M. Ipsilateral hip abductor weakness after inversion ankle sprain. J Athl Train. 2006;41(1):74–78. [PMC free article] [PubMed] [Google Scholar]
- 8.Nadler SF, Malanga GA, DePrince M, Stitik TP, Feinberg JH. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000;10(2):89–97. doi: 10.1097/00042752-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Bullock-Saxton JE. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther. 1994;74(1):17–28. doi: 10.1093/ptj/74.1.17. [DOI] [PubMed] [Google Scholar]
- 10.Jaramillo J, Worrell TW, Ingersoll CD. Hip isometric strength following knee surgery. J Orthop Sports Phys Ther. 1994;20(3):160–165. doi: 10.2519/jospt.1994.20.3.160. [DOI] [PubMed] [Google Scholar]
- 11.Leetun DT, Ireland ML, Wilson JD, Ballantyne BT, Davis IM. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926–934. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- 12.Ireland ML. Anterior cruciate ligament injury in female athletes: epidemiology. J Athl Train. 1999;34(2):150–154. [PMC free article] [PubMed] [Google Scholar]
- 13.Olsen O, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 14.Hewett TE, Myer GD, Ford KR. Biomechanical measures or neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. et al. [DOI] [PubMed] [Google Scholar]
- 15.Griffin LY, Agel J, Albohm MJ. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150. doi: 10.5435/00124635-200005000-00001. et al. [DOI] [PubMed] [Google Scholar]
- 16.Hutchinson MR, Ireland ML. Knee injuries in female athletes. Sports Med. 1995;19(4):288–302. doi: 10.2165/00007256-199519040-00006. [DOI] [PubMed] [Google Scholar]
- 17.Ireland ML, Gaudette M, Crook S. ACL injuries in the female athlete. J Sport Rehabil. 1997;6(2):97–110. [Google Scholar]
- 18.McClay Davis I, Ireland ML. ACL injuries: the gender bias. J Orthop Sports Phys Ther. 2003;33(8):A2–A8. [PubMed] [Google Scholar]
- 19.Beckett ME, Massie DL, Bowers KD, Stoll DA. Incidence of hyperpronation in the ACL injured knee: a clinical perspective. J Athl Train. 1992;27(1):58–62. [PMC free article] [PubMed] [Google Scholar]
- 20.Loudon JK, Jenkins W, Loudon KL. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther. 1996;24(2):91–97. doi: 10.2519/jospt.1996.24.2.91. [DOI] [PubMed] [Google Scholar]
- 21.Hertel J, Dorfman JH, Braham RA. Lower extremity malalignments and anterior cruciate ligament injury history. J Sports Sci Med. 2004;3(4):220–225. [PMC free article] [PubMed] [Google Scholar]
- 22.Woodford-Rogers B, Cyphert L, Denegar CR. Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train. 1994;29(4):343–346. [PMC free article] [PubMed] [Google Scholar]
- 23.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 24.Dostal WF, Andrews JG. A three-dimensional biomechanical model of hip musculature. J Biomech. 1981;14(11):803–812. doi: 10.1016/0021-9290(81)90036-1. [DOI] [PubMed] [Google Scholar]
- 25.Delp SL, Hess WE, Hungerford D, Jones LC. Variation of rotation moment arms with hip flexion. J Biomech. 1999;32(5):493–501. doi: 10.1016/s0021-9290(99)00032-9. [DOI] [PubMed] [Google Scholar]
- 26.Dostal WF, Soderberg GL, Andrews JG. Actions of hip muscles. Phys Ther. 1986;66(3):351–361. doi: 10.1093/ptj/66.3.351. [DOI] [PubMed] [Google Scholar]
- 27.Merchant AC. Hip abductor muscle force; an experimental study of the influence of hip position with particular reference to rotation. J Bone Joint Surg Am. 1965;47:462–476. [PubMed] [Google Scholar]
- 28.Nyland J, Kuzemchek S, Parks M, Caborn DN. Femoral anteversion influences vastus medialis and gluteus medius EMG amplitude: composite hip abductor EMG amplitude ratios during isometric combined hip abduction-external rotation. J Electromyogr Kinesiol. 2004;14(2):255–261. doi: 10.1016/S1050-6411(03)00078-6. [DOI] [PubMed] [Google Scholar]
- 29.Shultz SJ, Nguyen A, Windley TC, Kulas AS, Botic TL, Beynnon BD. Intratester and intertester reliability of clinical measures of lower extremity anatomic characteristics; implications for multicenter studies. Clin J Sport Med. 2006;16(2):155–161. doi: 10.1097/00042752-200603000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Shultz SJ, Nguyen AD, Levine BJ. The relationship between lower extremity alignment characteristics and anterior knee joint laxity. J Sports Health. 2009;1(1):54–60. doi: 10.1177/1941738108326702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nguyen AD, Shultz SJ. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther. 2007;37(7):389–398. doi: 10.2519/jospt.2007.2487. [DOI] [PubMed] [Google Scholar]
- 32.Shultz SJ, Nguyen AD, Schmitz RJ. Differences in lower extremity anatomical and postural characteristics in males and females between maturation groups. J Orthop Sports Phys Ther. 2008;38(3):137–149. doi: 10.2519/jospt.2008.2645. [DOI] [PubMed] [Google Scholar]
- 33.Gilliam J, Brunt D, MacMillan M, Kinard RE, Montgomery WJ. Relationship of the pelvic angle to the sacral angle: measurement of clinical reliability and validity. J Orthop Sports Phys Ther. 1994;20(4):193–199. doi: 10.2519/jospt.1994.20.4.193. [DOI] [PubMed] [Google Scholar]
- 34.Ruwe PA, Gage JR, Ozonoff MB, De-Luca PA. Clinical determination of femoral anterversion: a comparison with established techniques. J Bone Joint Surg Am. 1992;74(6):820–830. [PubMed] [Google Scholar]
- 35.Cram JR, Kasman GS. The Basics of Surface Electromyography. Gaithersburg, MD: Aspen Publishers; 1998. [Google Scholar]
- 36.Carcia CR, Eggen JM, Shultz SJ. Hip-abductor fatigue, frontal-plane landing angle, and excursion during a drop jump. J Sport Rehabil. 2005;14(4):317–327. [Google Scholar]
- 37.Nyland J, Smith S, Beickman K, Armsey T, Caborn DN. Frontal plane knee angle affects dynamic postural control strategy during unilateral stance. Med Sci Sports Exerc. 2002;34(7):1150–1157. doi: 10.1097/00005768-200207000-00016. [DOI] [PubMed] [Google Scholar]
- 38.Leardini A, Cappozzo A, Cantani F. Validation of a functional method for the estimation of hip joint centre location. J Biomech. 1999;32(1):99–103. doi: 10.1016/s0021-9290(98)00148-1. et al. [DOI] [PubMed] [Google Scholar]
- 39.Zeller BL, McCrory JL, Kibler WB, Uhl TL. Differences in kinematics and electromyographic activity between men and women during the single-legged squat. Am J Sports Med. 2003;31(3):449–456. doi: 10.1177/03635465030310032101. [DOI] [PubMed] [Google Scholar]
- 40.Zazulak BT, Ponce PL, Straub SJ, Medvecky MJ, Avedisian L, Hewett TE. Gender comparison of hip muscle activity during single-leg landing. J Orthop Sports Phys Ther. 2005;35(5):292–299. doi: 10.2519/jospt.2005.35.5.292. [DOI] [PubMed] [Google Scholar]
- 41.Schmitz RJ, Riemann BL, Thompson T. Gluteus medius activity during isometric closed-chain hip rotation. J Sport Rehabil. 2002;11(3):179–188. [Google Scholar]
- 42.Kadaba MP, Ramakrishnan HK, Wootten ME, Gainey J, Gorton G, Cochran GV. Repeatability of kinematic, kinetic, and electromyographic data in normal adult gait. J Orthop Res. 1989;7(6):849–860. doi: 10.1002/jor.1100070611. [DOI] [PubMed] [Google Scholar]
- 43.Murray MP, Sepic SB. Maximum isometric torque of hip abductor and adductor muscles. Phys Ther. 1968;48(12):1327–1335. doi: 10.1093/ptj/48.12.1327. [DOI] [PubMed] [Google Scholar]
- 44.Bohannon RW. Reference values for extremity muscle strength obtained by hand-held dynamometry from adults aged 20 to 79 years. Arch Phys Med Rehabil. 1997;78(1):26–32. doi: 10.1016/s0003-9993(97)90005-8. [DOI] [PubMed] [Google Scholar]
- 45.Cahalan TD, Johnson ME, Liu S, Chao EY. Quantitative measurements of hip strength in different age groups. Clin Orthop Relat Res. 1989;246:136–145. [PubMed] [Google Scholar]
- 46.Shultz SJ, Nguyen AD, Leonard MD, Schmitz RJ. Thigh strength and activation as predictors of knee biomechanics during a drop jump task. Med Sci Sports Exerc. 2009;41(4):857–866. doi: 10.1249/MSS.0b013e3181e3b3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Raykov T, Marcoulides GA. A First Course in Structural Equation Modeling. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 48.Hvid I, Andersen LI. The quadriceps angle and its relation to femoral torsion. Acta Orthop Scand. 1982;53(4):577–579. doi: 10.3109/17453678208992261. [DOI] [PubMed] [Google Scholar]
- 49.Ferber R, Davis IM, Williams DS., 3rd Gender differences in lower extremity mechanics during running. Clin Biomech (Bristol, Avon) 2003;18(4):350–357. doi: 10.1016/s0268-0033(03)00025-1. [DOI] [PubMed] [Google Scholar]
- 50.Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech (Bristol, Avon) 2001;16(5):438–445. doi: 10.1016/s0268-0033(01)00019-5. [DOI] [PubMed] [Google Scholar]
- 51.Lephart SM, Ferris CM, Riemann BL, Myers JB, Fu FH. Gender differences in strength and lower extremity kinematics during landing. Clin Orthop Relat Res. 2002;401:162–169. doi: 10.1097/00003086-200208000-00019. [DOI] [PubMed] [Google Scholar]
- 52.Jonson SR, Gross MT. Intraexaminer reliability, interexaminer reliability, and mean values for nine lower extremity skeletal measures in healthy naval midshipmen. J Orthop Sports Phys Ther. 1997;25(4):253–263. doi: 10.2519/jospt.1997.25.4.253. [DOI] [PubMed] [Google Scholar]
- 53.Souza RB, Powers CM. Concurrent criterion-related validity and reliability of a clinical test to measure femoral anteversion. J Orthop Sports Phys Ther. 2009;39(8):586–592. doi: 10.2519/jospt.2009.2996. [DOI] [PubMed] [Google Scholar]


