Abstract
Achieving health equity, driven by the elimination of health disparities, is a goal of Healthy People 2020. In recent decades, the improvement in health status has been remarkable for the U.S. population as a whole. However, racial and ethnic minority populations continue to lag behind whites with a quality of life diminished by illness from preventable chronic diseases and a life span cut short by premature death. We examine a conceptual framework of three generations of health disparities research to understand (a) data trends, (b) factors driving disparities, and (c) solutions for closing the gap. We propose a new, fourth generation of research grounded in public health critical race praxis, utilizing comprehensive interventions to address race, racism, and structural inequalities and advancing evaluation methods to foster our ability to eliminate disparities. This new generation demands that we address the researcher’s own biases as part of the research process.
Keywords: health disparities, critical race theory, public health critical race praxis, racial and ethnic minorities, community engagement
INTRODUCTION AND PURPOSE
The World Health Organization has defined health inequality as differences in health status or in the distribution of health determinants between different population groups (29, 77). Disparities in health status and health care would be easy to ignore were they not so well documented. Health inequality exists because of race and ethnicity, which intersect with other social determinants of health. The purpose of this article is to advance fourth-generation health disparities research, framed by public health critical race praxis, to help develop multilevel interventions designed to achieve health equity. Although our focus is on racial and ethnic disparities in the U.S. context, we recognize that socioeconomic disparities are a contributing but not the sole cause of these racial and ethnic health disparities. We also recognize that although it is beyond the scope of the paper to address global health disparities, many of the core concepts are relevant to a global context.
The Demographic Shift in the United States
The existence of compelling DNA evidence to show all humans are indeed one race biologically (1) has done little to eliminate the social presumption of race, which perpetuates discrimination and contributes to health disparities among racial and ethnic minority populations (21, 76). The 2006–2008 American Community Survey revealed that 38.6% of the U.S. population identified their race as nonwhite, black or African American (12.3%), nonwhite, Hispanic or Latino (15.1%), or non-white other (remaining 11.2%) (64). The U.S. Census Bureau (62) projects that by 2050 racial and ethnic minority groups will account for almost half the U.S. population. These statistics are based on the social presumption that individuals in the United States can be readily categorized into definable races despite ample DNA evidence to the contrary that all humans are one race biologically (1). Classification based on race reveals, however, that the overall health of the nation is inextricably intertwined with the health of racial and ethnic minority populations and that discrimination contributes to health disparities affecting these groups (76). As the U.S. demographic shifts away from a white majority, the differential health status between whites and minority groups constitutes a critical challenge for public health professionals.
In this article, we focus our discussion on the two largest minority groups, African Americans/blacks and Latinos/Hispanics,1 with the understanding that health disparities are caused by common factors faced by all minority groups. We acknowledge that American Indian, Alaska Native, Asian, Native Hawaiian, Pacific Islander populations, and other racial/ethnic groups have also experienced systematic discrimination related to health as a consequence of their race/ethnicity and may face unique challenges in health care that cannot be adequately covered here.
CLOSING THE HEALTH DISPARITY GAP
Although health disparities have been evident throughout our nation’s history, federal efforts to address those disparities have waxed and waned. The first federal efforts to address health disparities have their genesis in the Negro Health Movement (1915–1951) and led the U.S. Public Health Service to establish the Office of Negro Health Work (51, 52). More than 30 years later, in 1985, Margaret Heckler, Secretary of the U.S. Department of Health and Human Services (DHHS), released the Secretary’s Task Force Report on Black and Minority Health, which documented excess deaths from cancer, cardiovascular diseases, chemical dependency, diabetes, homicide, unintentional injuries, and infant mortality experienced by minority populations (66) and focused attention on significant gaps in health status between minorities and whites. The report also uncovered decades of neglect in seeking solutions and thrust minority health back onto the national agenda.
The Task Force Report galvanized the DHHS to establish the Office of Minority Health (OMH) in 1986 and charged this agency with the responsibility to implement the report’s recommendations (59). In 1988, the Centers for Disease Control and Prevention (CDC) created the Office of the Associate Director for Minority Health, which became the CDC’s Office of Minority Health in 2002. In 2005, the CDC strengthened its commitment to promote health and quality of life and to eliminate health disparities for vulnerable populations by forming the Office of Minority Health and Health Disparities (OMHD) (12). Similarly, the Director of the National Institutes of Health (NIH) established the Office of Research on Minority Health (ORMH) in 1990 (18, 41, 59). In 2000, the ORMH became the National Center on Minority Health and Health Disparities (NCMHD) within the NIH, which supports and coordinates health disparities research and promotes programs that increase the number of underrepresented minority students and students from health disparity groups in the biomedical and behavioral research workforce (18).
The passage of the Health Care and Education Reconciliation Act of 2010 (H.R. 4872) (65) marks the beginning of a new chapter in American society, bringing the United States one step closer to universal access to health care. The Act authorized the transition of NCMHD to become the National Institute on Minority Health and Health Disparities, expanding its mission to planning, coordinating, reviewing, and evaluating all minority health and health disparities research activities conducted and supported by the NIH institutes and centers (42, p. 1). The Act mandates that insurers provide coverage for preventive services with no copayments or deductibles. The Act authorizes and supports increased efforts by the CDC’s Task Force on Community Preventive Services to evaluate and recommend prioritization of evidence-based and population-based programs, policies, and interventions that improve health and prevent disease. The Act also expands the efforts of the U.S. Preventive Services Task Force—an independent panel of internists, family physicians, pediatricians, gynecologists/obstetricians, nurses, and behavior specialists that reviews the effectiveness of preventive services and publishes recommendations for clinical preventive services (17). The Act encourages better coordination between these two task forces (72).
Specific to health equity, this legislation transfers the Office of Minority Health to the Office of the Secretary of Health and Human Services, headed by the Deputy Assistant Secretary for Minority Health, and provides funding for new initiatives, including grants for Creating Healthier Communities (community transformation grants), Promoting the Community Health Workforce, and Health Professions Training for Diversity (65).
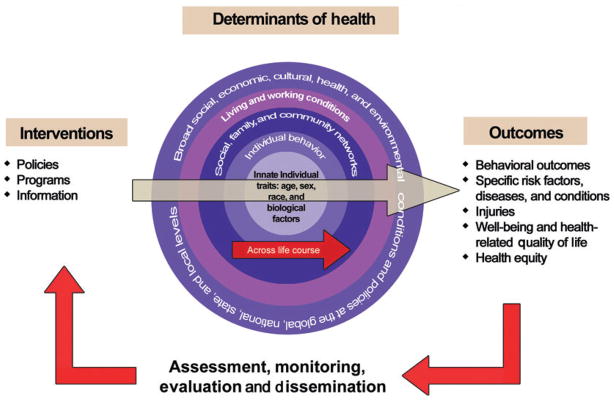
The Act also supports the goals of Healthy People, the U.S. government’s strategic management tool first published in 1979, which identifies preventable threats to health and sets the nation’s agenda for the prevention of disease and reduction of mortality. The first iteration of health objectives for racial and ethnic minority populations was initiated in Healthy People 2000 (67). The elimination of health disparities became an objective in Healthy People 2010 (68). Healthy People 2020 (71) seeks to (a) eliminate preventable disease, disability, injury, and premature death; (b) achieve health equity, eliminate disparities, and improve the health of all groups; (c) create social and physical environments that promote good health for all; and (d) promote healthy development and healthy behaviors across every stage of life. These goals, coupled with an explicit endorsement of an ecological mindfulness and an acknowledgment of social determinants of health, mandate a broadening of current approaches to eliminating health disparities. Healthy People 2020 provides an action model that aligns these approaches and articulates a feedback loop as the nation monitors its progress toward achievement of the goals (71) (see Figure 1).
Figure 1.
Action model to achieve Healthy People 2020 overarching goals.
ELIMINATING RACIAL AND ETHNIC HEALTH DISPARITIES
Although there has been significant improvements in health status of the U.S. population as a whole, closer examination of epidemiologic trends exposes a troubling truth: Racial and ethnic minority populations lag behind their white peers with respect to morbidity and mortality across a broad spectrum of mostly preventable conditions and diseases. According to the most reliable data from the National Center for Health Statistics (39, 63), white females continue to have the longest life expectancy (80.7 years) followed by black females (77.0 years) (Asian American women may have the longest life expectancy; however, data-collection methods for these and other populations vary widely and cannot be used in direct comparisons). Although the difference in life expectancy between white and black populations has decreased steadily from a difference of 7.1 years in 1989 to 4.8 years in 2007 (63), the U.S. Census Bureau predicts that a gap will continue to exist and estimates life expectancy for whites in 2020 to be 80.0 years compared with 76.1 years for blacks (62).
FRAMING MATTERS: CAUSES OF DEATH
Much of the gap in life expectancy between whites and blacks is tied to the incidence of chronic diseases, which are a suitable focus for reducing disparities (16, 26). “Between 2002 and 2030, the mortality rate for all chronic diseases (e.g., heart disease, cancer, type 2 diabetes) is expected to increase by almost 20% worldwide” (26, p. S25). If we examine both existing racial and ethnic disparities in these diseases today, as well as the disproportionate obesity rates, which place minorities at high risk for chronic disease (22), we can project the continuing presence of disparities well into coming decades. Therefore, we must examine the prevalence of diseases themselves but also consider the actual causes of disease burden.
In 2004, the CDC published “Actual Causes of Death in the United States. 2000” (40), which identified tobacco (435,000 deaths; 18.1% of total U.S. deaths) and poor diet and physical inactivity (400,000 deaths; 16.6% of total U.S. deaths) as the leading contributors to loss of life. “These findings, along with escalating health care costs and aging populations, argued persuasively that the need to establish a more preventive orientation in the U.S. health care and public health systems has become more urgent” (40, p. 1238). The inclusion of a prevention focus in the Patient Protection and Affordable Care Act (72) sets the stage for new actions to achieve health equity. Nonetheless, the success of any future prevention program is dependent on the validity of historical and present research on obesity (69) and tobacco (70) and the acknowledgment that health disparities exist in certain populations.
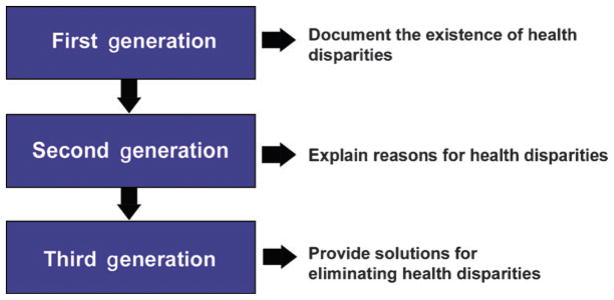
In 2008, we (60) adapted Kilbourne’s (36) three phases of health care disparity research framework to address disparities in nonclinical settings. We proposed three generations of health disparities research as an organizing principle from which to examine the status of such research in non-clinical settings (60) (see Figure 2). First-generation research focuses on detection, identification, and documentation of disparities, including identifying vulnerable populations (36, 60). Second-generation research determines causal relationships that underlie health disparities. Whereas Kilbourne (36) focused heavily on understanding causality in the context of health care disparities, we (60) broadened that focus to include the social determinants that underlie disparities in health status and unequal access to health care. Third-generation research, which provides solutions for eliminating health disparities, mirrors what Kilbourne (36) describes as the third phase in health care disparities research. This research includes examples such as the CDC’s Racial and Ethnic Approaches to Community Health Across the U.S. (REACH 2010) projects (11). Below, we discuss obesity and tobacco use separately in terms of first- and second-generation research and together in terms of third-generation research. We conclude with a proposal to extend our research efforts to a fourth-generation approach.
Figure 2.
FIRST-GENERATION RESEARCH RELATED TO OBESITY: DO DISPARITIES EXIST?
Using data from the National Health and Nutrition Examination Survey (NHANES), Flegal and colleagues (22) report that the “prevalence of obesity in the US is high, exceeding 30% in most age and sex groups” (p. 238). Examination of the data by race and gender highlights the racial and ethnic differences. For example, according to the authors, non-Hispanic white men had an age-adjusted obesity prevalence of 31.9% compared with 37.3% for non-Hispanic black men. The racial disparity was more pronounced among women: The age-adjusted obesity prevalence among non-Hispanic white women was 33.0% compared with 49.6% among non-Hispanic black women (22). Although our ability to detect the obesity epidemic is extensive, the etiology of obesity is complex and our ability to eliminate it is far more limited.
SECOND-GENERATION RESEARCH RELATED TO OBESITY: WHY DO DISPARITIES EXIST?
The disproportionate burden of obesity among African Americans and Latinos compared with the white population is disturbing and not well understood. Socioeconomic status, environment, and lifestyle factors such as physical inactivity and diet have been identified as contributing factors (15, 45). Paeratakul et al. (45) predict that the absence of evidence-based studies and interventions for minority populations will perpetuate the problem (15, 45). Unfortunately, the reductionist nature of randomized controlled trials (RCTs) as the gold standard for scientific evidence (5) has advanced our mechanistic and biomedical understanding of obesity at the expense of understanding social and environmental determinants of the obesity epidemic. The result is an acceleration of surgical and pharmaceutical interventions (13) to the neglect of observational research on the social, policy, and environmental interventions for obesity.
FIRST-GENERATION RESEARCH RELATED TO TOBACCO USE
Tobacco use, predominately cigarette smoking, continues to be the leading cause of preventable morbidity and mortality in the United States. Cigarette smoking is recognized as the cause of multiple cancers, heart disease, stroke, complications in pregnancy, and chronic obstructive pulmonary disease (37, 43, 70) and is responsible for greater than 443,000 annual deaths among adults (10). In 2008, 20.6% (~46 million) of U.S. adults were smokers, resulting in $96 billion in medical costs and $97 billion in lost productivity annually in the United States (2, 9). Thus tobacco use has remained an important challenge facing the public health, medical, and policy communities (10, 43).
Looking closely at current data, the smoking prevalence in 2008 was higher among men (23.1%) than among women (18.3%). Among racial/ethnic groups, Asians had the lowest prevalence (9.9%), followed by Hispanics (15.8%), non-Hispanic blacks (21.3%), and non-Hispanic whites (22.0%). American Indians/Alaska Natives had the highest prevalence of current smoking compared with any other racial or ethnic group (32.4%) (10).
Smoking cessation campaigns and health education efforts have contributed to a substantial decline in the smoking rates over the past 40 years, although the decline has remained unchanged at ~20% among adults 18 years and older during the past five years, according to the CDC (10). Unfortunately, progress has also stalled in reducing smoking rates among young persons and minorities (2, 10).
SECOND-GENERATION RESEARCH ON TOBACCO
Tobacco use is a multilevel problem that is influenced by a number of factors (43), including socioeconomic correlates such as race and ethnicity, gender, level of education, occupation, and income and wealth, as well as other individual-level factors that affect tobacco use, including age of smoking onset, adverse childhood experiences, and self-esteem (3, 9, 70).
Environmental factors include familial, social, cultural, economic, historical, political, and media influences (43). For example, the presence of smoking peers, siblings, and parents, as well as norms established at home, can influence uptake (70, 75). Moreover, the use of higher tar-yield brands has been associated with nicotine dependence among black smokers (43, 48, 49). Other environmental factors identified as contributors to disparities in tobacco use include targeted tobacco advertising and promotion, including billboards and advertisements in media that appeal to racial/ethnic minorities, and cultivation of a prosmoking environment (27, 32).
THIRD-GENERATION RESEARCH IN OBESTITY AND TOBACCO USE RELATED TO HEALTH DISPARITIES: DO INTERVENTIONS WORK?
With a focus on development and implementation of interventions, third-generation research is necessary before distilled knowledge can be implemented in standards of practice (61). Although the nascent status of third-generation research is apparent in the lack of evidence for solutions to address the obesity epidemic and tobacco use among racial and ethnic minorities, we examined the CDC’s Guide to Community Preventive Services, which reports results of greater than 200 interventions, to determine what works when addressing obesity- and tobacco-related disparities (56):
Which program and policy interventions have been proven effective?
Are there effective interventions that are right for my community?
What might effective interventions cost and what is the likely return on investment?
In Table 1, we concentrate on obesity and tobacco use prevention, previously discussed as examples in first- and second-generation research in health disparities.
Table 1.
Task Force on Community Preventive Services recommended interventions for prevention of obesity and tobacco use. Source: Adapted from The Guide to Community Preventive Services (56, 57)
| Condition | Guide to Community Preventive Services recommended intervention | Number of articles in systematic review | Reported impact on racial and ethnic minority populations |
|---|---|---|---|
| Obesity prevention | Community-based behavioral interventions to reduce screen time | 7 | “Because limited race and ethnicity data were available, it is unknown if the intervention had differential effects for different racial or ethnic groups” (56) |
| Work site programs to control overweight and obesity | 47 | “Forty percent of the studies lacked information to determine differential effects according to blue or white collar job status. Those that did report occupational status included predominantly white collar workers.” Race and ethnicity data were also limited. | |
| Reducing tobacco use initiation | Increasing the unit price for tobacco products | 8 | Unknown. Scientific evidence of effectiveness is unknown for racial and ethnic minorities. |
| Mass media education campaigns combined with other interventions | 12 | Unknown. Scientific evidence of effectiveness is unknown for racial and ethnic minorities. | |
| Increasing tobacco use cessation | Provider reminder systems when used alone | 7 | Unknown. The impact on race and ethnicity is identified as “research gapsa.” |
| Increasing the unit price for tobacco products | 17 | Unknown. The impact on race and ethnicity is identified as “research gapsa.” | |
| Mass media campaigns when combined with additional interventions | 15 | Unknown. The impact on race and ethnicity is identified as “research gapsa.” | |
| Provider reminder systems with provider education | 31 | Unknown. The impact on race and ethnicity is identified as “research gapsa.” | |
| Reducing client out-of-pocket costs for cessation therapies | 5 | Unknown. The impact on race and ethnicity is identified as “research gapsa.” | |
| Multicomponent interventions that include telephone support | 32 | Unknown. The impact on race and ethnicity is identified as “research gapsa.” | |
| Reducing exposure to environmental tobacco smoke | Smoking bans and restrictions are policies, regulations, and laws that limit smoking in work places and other public areas | 10 | The impact on race and ethnicity is unknown. |
| Restricting minors’ access to tobacco products | Community mobilization with additional interventions such as those aimed at focusing public attention on the issue of youth access to tobacco products and mobilizing community support for additional efforts to reduce that access | 9 | Interventions were implemented in communities that included predominantly African American, Hispanic, or white populations, yet no racial or ethnic-specific data were reported. |
| Decreasing tobacco use in work site settings | Smoke-free policies to reduce tobacco use among workers | 35 | The impact on race and ethnicity is unknown. |
| Worksite-based incentives and competitions when combined with additional interventions to increase smoking cessation among workers | 12 | The impact on race and ethnicity is unknown. |
Unanswered questions (e.g., which interventions work, for whom, under which conditions, and at what cost) that can be addressed by future research.
The criteria for inclusion of interventions in the Guide to Community Preventive Services systematic review are biased toward RCT research, the gold standard for NIH-funded research. As such, the underrepresentation of racial and ethnic minority populations in RCT research has yielded a color-blind evidence base, with few, if any, studies that explicitly cite evidence of effectiveness with minority communities. Research is urgently needed that builds the evidence base of effective and culturally appropriate interventions for racial and ethnic minority populations. To address this need, we call for strong third-generation research that explicitly includes racial and ethnic minorities in RCT studies to build the evidence base. Additionally, we proposed that this research rest on three pillars: (a) transdisciplinary research, (b) community engagement, and (c) translational research (60).
LIMITATIONS OF THIRD-GENERATION RESEARCH
Despite our call for more third-generation research to build the evidence base, using this type of research to address the elimination of racial and ethnic health disparities is inherently limited. Typically, third-generation research is composed largely of categorical interventions focused on a specific disease outcome. In this research, race is often treated superficially, either as a demographic variable or as a proxy for culture, but rarely understood in its more complex linkage to racism and structural determinants of health (e.g., poverty, institutional factors, policy factors). Moreover, many third-generation research interventions have functioned within what Resnicow & Braithwaite (53) refer to as the “surface structure” dimension of intervention development and implementation: “the extent to which interventions fit within the culture, experience, and behavioral patterns of the audience” (p. 518, emphasis in original). However, race and racism are far less frequently the explicit focus of RCT research. In fact, we argue that such color blindness, which does not address issues of racism, has contributed to the knowledge gap in the Guide on Community Preventive Services with regard to evidence-based interventions that target racial and ethnic minority populations. Furthermore, even in third-generation research, interventions that focused heavily on individual behaviors have failed to address in a meaningful way the broader structural determinants of health. Although the strength of many third-generation studies was their increasing focus on community engagement and transdisciplinary research, there remained too few strong translations of research results into interventions that targeted racial and ethnic populations. In hindsight, despite our proposal for third-generation research, we realize that such research, while aimed at providing solutions, still falls short of being capable of truly achieving health equity.
TOWARD A FOURTH GENERATION OF HEALTH DISPARITIES RESEARCH
Today, we believe that third-generation research is necessary but not sufficient to eliminate disparities and to move toward health equity. Transformational thinking beyond our standard research paradigms is needed (16). Therefore, we propose the health equity action research trajectory (HEART) as a platform for fourth-generation research (see Figure 3). The proposed HEART paradigm is anchored by the three pillars of our generation-based model of health disparities research (detect, understand, and provide solutions) but adopts key bioethics principles of justice to facilitate action to eliminate health disparities. For example, HEART proposes research that takes action by (a) utilizing public health critical race praxis (PHCR) as our conceptual framework (25), (b) addressing structural determinants of health through comprehensive multilevel interventions, (c) utilizing comprehensive evaluation, and (d ) necessitating explicit attention to self-reflection by the researcher.
Figure 3.
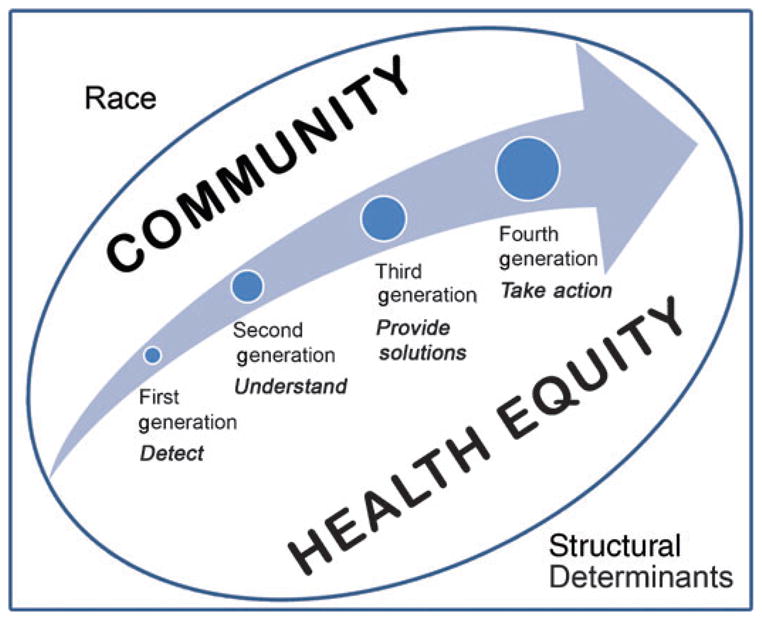
Health equity action research trajectory.
Public Health Critical Race Praxis: The Framework of Fourth-Generation Research
W.E.B. DuBois, noted African American sociologist, declared, “the problem of the twentieth century is the problem of the color line” (20, p. XV). Thomas echoed, “The ‘color line’ is not fixed but ripples through time, finding expression at distinct stages of our development as a nation” (58, p. 1046). Race and racism are persistent themes throughout our history and must not be limited by focusing primarily on the black experience, owing to the historical institution of slavery. Today, there is an increasingly racialized focus on the experience of Latinos, owing to polarization of public opinion regarding immigration into the United States.
Although some (14, 28) argue that we should abandon the concept of race for the purpose of surveillance and instead use ethnicity as the classification schema for public health research and practice, we believe that the shift away from race to ethnic group minimizes the health impact of racism for populations subjected to social prejudice because of their skin color and facial features. Much of the public health literature to date has not effectively engaged the complex and persistent impact of racism. To a large extent, research utilizes race as a demographic variable without fully grappling with race and racism in contemporary society. Sophisticated research tools have been developed to measure the impact of racism and discrimination; however, these tools have not been widely adopted.
Ford & Airhihenbuwa (25) make a convincing argument that critical race theory (CRT) is a transdisciplinary approach that offers much to health disparities research. For example, race consciousness is defined as “the explicit acknowledgment of the workings of race and racism in social contexts or in one’s personal life and color blindness as positing that nonracial factors explain racial phenomena” (24, p. s31). Additionally, CRT integrates Gilmore’s definition of racism, “the state-sanctioned and/or extralegal production and exploitation of group differentiated vulnerability to premature death” (31, p. 247). Today, the overt demonstrations of racism exist in the margins of our society, but it is still possible for racism to be made visible to all, as seen in the beating deaths of individuals from protected classes (e.g., racial/ethnic minorities) and passage of hate crime laws. However, racism also plays out more in what is termed as ordinariness, where it is a more subtle part of daily life (24). By incorporating this concept of racism, researchers can better examine the impact of routine exposure to racism on health behaviors and health status. Moreover, adopting race consciousness and beginning the research process from the perspective of racial and ethnic minorities, which Ford & Airhihenbuwa (24) called “centering in the margins” rather than from perspectives of majority white researchers, would essentially shift the entire research process toward a different level of engagement around race and racism, demanding that the researchers examine their own lived experiences and the interaction of race, power, and class. Thus, the research endeavor would aim for praxis, where “knowledge gained from theory, research, personal experiences and practice inform one another” (24, p. s31). In summary, we concur with the assertion that
Critical Race Theory can contribute…a comprehensive framework for connecting these research endeavors, a vocabulary for advancing understandings of racial constructs and phenomena, critical analyses of knowledge production processes, and praxis that building on community-based participatory approaches linking research, practice and communities. (24, p. s32)
We propose adoption of Ford & Airhihenbuwa’s PHCR praxis (25) as the framework for fourth-generation research in health disparities. They state that “public health critical race praxis assists public health researchers to carryout health equity research with fidelity to CRT” (25, p. 1390). Both CRT and PHCR praxis go beyond simply documenting, understanding, and proposing solutions to health disparities toward action aimed at eliminating health disparities. PHCR is based on four focuses and ten principles (see Table 2 for definition of principles). The four focuses are (a) contemporary racial relations, guided by the principles of the primacy of race, race as a social construct, the ordinariness of racism, and structural determinism; (b) knowledge production, guided by the social construction of knowledge, critical approaches, and voice; (c) conceptualization and measurement, guided by race as a social construct and intersectionality; and (d ) action, guided by critical approaches, voice, intersectionality, and disciplinary self-critique (25). According to the authors, race consciousness is at the heart of working through the four focuses and is also informed by theory, qualitative data, and unlike much current research, personal self-reflection.
Table 2.
Applying the public health critical race praxis: toward fourth-generation disparities researcha
| PHCR Principles (25, p. 1394) | Definition (25, p. 1394) | Selected third-generation Healthy Black Family Project Intervention components (8, 23, 30, 38, 60, 74) | Proposed fourth-generation Healthy Black Family Project intervention components |
|---|---|---|---|
| Race consciousness | Deep awareness of one’s racial position; awareness of racial stratification processes operating in color-blind contexts | Engaged health professionals and researchers to conduct health education and clinical outreach to HBFP participants by working in local barber shops and beauty salons, followed by debriefing discussions, as part of the urban immersion program | Engage all health professionals, researchers, and staff working with HBFP in the Undoing Racism Workshop series |
| Primacy of racialization | The fundamental contribution of racial stratification to societal problems; the central focus of CRT scholarship on explaining racial phenomena | Completed a qualitative CBPR study with HBFP members that integrated community voices with quantitative data on grocery store practices and policies shaped by structural racism and resulting in poor access to full-service grocery stores in segregated black neighborhoods | Mobilize consumer demand for access to full-service grocery stores in black neighborhoods using data from mixed-methods research to posit a social justice alternative to the prevailing market justifications for the food desert status quo |
| Race as social construct | Significance that derives from social, political, and historical forces | Created HBFP and its associated media campaign in a deliberate way to overcome the negative image of black families as a means to seize race and the family as positive constructs | Although the HEZ was established on the basis of historical geographic patterns of racial segregation, poverty, and unearned disadvantages, use the mass media platform to redefine the HEZ as the geographic space for targeted investments designed to promote social cohesion and direct political power needed to achieve health equity |
| Ordinariness of racism | Racism is embedded in the social fabric of society | After the Undoing Racism Workshops, health professionals, researchers, and HBFP members meet to work jointly on the development of a study of how exposure to racism impacts their mental health | |
| Structural determinism | The fundamental role of macrolevel forces in driving and sustaining inequities across time and contexts; the tendency of dominant group members and institutions to make decisions or take action that preserves existing power hierarchies | Created the HEZ using census and county health data to identify residential racial segregation, poverty, and chronic disease to target HBFP | Create a Black Leadership Commission on Health Equity charged with developing an advocacy agenda with leadership from community members focused on addressing racialized structural determinants that could eliminate disparities |
| Social construction of knowledge | The claim that established knowledge within a discipline can be reevaluated using antiracism modes of analysis | Develop a community-driven request for proposals for academic researchers to engage in relevant research on problems identified by the community | |
| Critical approaches | To dig beneath the surface; to develop a comprehensive understanding of one’s biases | Engage health professionals and researchers to participate in community-based dialogue with HBFP participants about race and the impact of racism on research recruitment | |
| Intersectionality | The interlocking nature of co-occurring social categories (e.g., race and gender) and the forms of social stratification that maintain them | Engage HBFP male participants in the examination of how race, gender, and current structure of activities impact male involvement in HBFP | |
| Disciplinary self-critique | The systematic examination by members of a discipline of its conventions and impacts on the broader society | Conduct annual retreat of all HBFP investigators on how we have operationalized race and racism in survey instruments and intervention designs and published articles to determine the intended and unintended impacts on health disparities research | |
| Voice | Prioritizing the perspectives of marginalized persons; privileging the experiential knowledge of outsiders within | Established a Community Research Advisory Board as a monthly forum designed for members of the African American community to share their perspectives with investigators on research being proposed for their community | Engage HBFP members in interpreting research results and considering implications for community action |
Abbreviations: CBPR, community-based participatory research; CRT, critical race theory; HEZ, health empowerment zone; HBFP, The Healthy Black Family Project; PHCR, public health critical race praxis.
Adopting PHCR praxis as the framework for fourth-generation research goes against a growing consensus that the United States is now a postracial society, as evidenced by the election of President Barack H. Obama. Nevertheless, in the context of the continuing tragedy of racial and ethnic health disparities, we believe that only by directly confronting race and racism can we truly eliminate health disparities and achieve health equity.
The Call for Comprehensive, Multilevel Interventions
Although significant second-generation research has aimed to understand the linkage between structural determinants and health status of racial and ethnic minority populations, the challenge of addressing those determinants in interventions is daunting. In their book, Vlahov et al. (73) critique categorical interventions, which focus on a specific disease outcome and frequently focus more on intrapersonal and interpersonal levels for interventions than on broader social, economic, cultural, and environmental determinants. Vlahov et al. (73) argue that these interventions fit the current paradigm, which allows for assessment of effectiveness of a specific intervention on a specific outcome. With the launch of Healthy People 2020, we welcome the inclusion of social determinants of health (http://www.healthypeople.gov) and agree that social, economic, cultural, and environmental factors are vitally important as targets for interventions. However, we believe that Ford & Airhihenbuwa (25) go further with structural determinism, which calls attention to the underlying dynamic power structure that perpetuates inequities. Therefore, we utilize their term, structural determinism, which explicitly demands that we address racism. Consequently, to a large extent, we have yet to realize the promise of integrating our increasing understanding of structural determinants of health with comprehensive interventions that address multiple levels simultaneously.
A comprehensive intervention focuses on multiple outcomes as well as multiple levels of the socioecological model (71, 73). Such interventions are at the heart of fourth-generation research and are responsive to the Healthy People 2020 action model aimed at achieving health equity. From the PHCR perspective, four key principles should inform intervention research: the primacy of racialization, structural determinism, critical approaches, and intersectionality.
In fourth-generation research, guided by PHCR, it is essential to remember that the goal is ultimately to take action to eliminate health disparities. In that context, the voice of community members is an absolute necessity. Fourth-generation research is deeply rooted in community and the racialized context of the populations who reside within them. Community-engaged research considers the actions that communities can take to promote health and represents a fundamental shift in emphasis from an individualistic biomedical model of health to a public health focus on populations in community-based settings.
The emergence of community-based participatory research (CBPR) (33) has represented a fundamental change from a sole focus on the individual as an autonomous being to a complex understanding of how health and behavior are shaped by the environment. Although CBPR is a valuable tool, it is only one means of community engagement. Community engagement is essential to fully understand and grapple with the impact of the ordinariness of racism on community members’ lives, to expand our understanding of race and racism as well as the intersectionality of other factors such as gender on their lives, and to engage community members fully as partners in action.
In the inaugural issue of the Journal of Mixed Methods Research, Tashakkori & Creswell (55) globally defined mixed methods research as utilizing both qualitative and quantitative strategies to collect and analyze data, to integrate findings, and to draw conclusions in a single study. The central tenet of the definition is the integration of the combined analyses of the data. We concur with the definition set forth by the authors and further embrace the extended definition proposed by Johnson et al. (34):
Mixed methods research is an intellectual and practical synthesis based on qualitative and quantitative research; it is the third methodological or research paradigm (along with qualitative and quantitative research). It recognizes the importance of traditional quantitative and qualitative research, but also offers a powerful third paradigm choice that often will provide the most informative, complete, balanced, and useful research results. (34, p. 129)
To this end, fourth-generation research demands a sophisticated mixed methods approach that can evaluate comprehensive, multilevel interventions. The mixed methods research paradigm is inherently rigorous and sensitive to the PHCR praxis principles of voice and the social construction of knowledge. More important, at its core, mixed methods research is grounded in and embraces the principles of intersectionality and critical approaches in the development and conduct of scientific investigations. As a result, this paradigm fits well with moving toward a fourth-generation of health disparities research.
The Challenge of Multilevel Interventions
Vlahov et al. (73) also caution that as we move toward more comprehensive, multilevel interventions, we face new challenges. They describe the challenges faced when making inferences from comprehensive interventions in which the interactions among the levels of intervention themselves, as well as with the social context, make it more difficult to tease out specific inferences of impact. The use of multilevel modeling in research is often an attempt by investigators to address more than one factor and more than one level other than individual behavior. Multilevel models allow for simultaneous examination of two levels of data (e.g., individual and neighborhood) and examination of the effects of one factor at one level while controlling for potential confounders at another level or interaction of factors at different levels. Yet, as with most models, impact is limited. As a result, we suggest that these new challenges require new methods informed by PHCR principles of structural determinism, critical approaches, intersectionality, disciplinary self-critique, and race as a social construct. The PHCR praxis demands that race and racism remain explicitly at the forefront of the analysis. Ford & Airhihenbuwa (25) clearly state their caution and concern regarding fidelity to critical race theory:
[W]hile it is entirely appropriate to apply most public health theories in a formulaic fashion, similar ‘application’ of Critical Race Theory would constitute a gross violation of its critical approach. CRT is praxis, not a standard theory. Its constituent constructs cannot be used merely to quantify relations between raced risk factors and individual-level health outcomes. (25, p. 1397, emphasis in original)
The Self-Reflective Researcher
There has been much focus in recent years on enhancing the cultural competence of health professionals. This focus on cultural competence contributes to the use of attendance at workshops as evidence of competence. Our concern is that the proliferation of cultural competence workshops and guides may create an artificial sense of efficacy with regard to engaging people of different racial and ethnic backgrounds (44).
We have to move beyond the mere synthesis and application of awareness, knowledge, and sensitivity gained from a discrete end point like a cultural competence workshop (46) to the belief that one can be committed to self-reflection and critique over one’s life span (4, 7). We describe this process as cultural confidence. Cultural confidence is a lifelong process based on the individual’s self-reflection about their personal biases and prejudices. We define a culturally confident person as someone who is flexible and humble enough to admit ignorance and is willing to be uncomfortable addressing complex racialized issues. This new approach is guided by race consciousness, the social construct of race, intersectionality, critical approaches, and disciplinary self-critique, which demand continual discussion and reflection about race and racism. This approach also demands that our professional preparation programs revamp their training to address race and racism more explicitly. To do so will require that academicians and researchers are also willing to engage in these same processes and that their capacity to work effectively with racial and ethnic minority communities is strengthened.
The Healthy Black Family Project
The Healthy Black Family Project (HBFP) is a third-generation research example of translating an RCT into a community-based, culturally appropriate health-promotion and disease-prevention program (60). The goal of the HBFP was to translate the lifestyle interventions found to be effective in the Diabetes Prevention Project (19) into a culturally appropriate program in a low-income, black community. For example, the HBFP sought to lower the common risk factors for type-2 diabetes and hypertension by providing physical activity classes such as African dance, body toning, walking, and yoga; providing nutrition classes; and engaging members in other research activities, including community forums on research (23, 60).
When HBFP was being developed in 2006, we lacked a strong framework that allowed us to address race and racism explicitly and their associated complex structural determinants. Now, with the creation of the 2010 PHCR praxis framework, we propose to look at HBFP with fresh and provocative eyes. In Table 2, we illustrate the principles of PHCR in the context of the HBFP. In hindsight, we recognize that we had actually addressed some of the PHCR principles but had not done so in the systematic manner that Ford & Airhihenbuwa (24, 25) proposed. Additionally, in Table 2, we present new interventions to move HBFP to a fourth-generation research study.
DANGER AND OPPORTUNITY
We have articulated an ambitious agenda for fourth-generation research. Critics could argue that it is unattainable, too costly, too time-consuming, and too idealistic. The danger is to assume that (a) racism is not relevant in the scientific pursuit of solutions for the elimination of health disparities, (b) some populations will always suffer premature illness and death by virtue of their culture-bound lifestyle choices, and thus (c) the elimination of disparities is impossible and health equity unachievable in a free-market society.
The opportunity is to recognize health disparities as an ethical issue of justice because specific groups were subjected to systematic racial discrimination and denied the basic benefits of society, a violation of the social contract (6). As Powers & Faden (50) state,
One critical moral function of public health…is to monitor the health of those who are experiencing systematic disadvantage as a function of group membership, to be vigilant for evidence of inequities relative to those in privileged social groups and to intervene to reduce those inequalities. (p. 88)
Because this situation places health disparities in a category of injustices deemed morally problematic (35), it demands achieving what we have thus far failed to do adequately, such as critically examine racism and race in a meaningful way and develop interventions that allow us to take direct action to eliminate health disparities.
ACHIEVING HEALTH EQUITY
There is an emerging consensus within the NIH, best articulated by John Ruffin (54), Director of the National Institute on Minority Health and Health Disparities:
[W]e can no longer be victims of inaction. Our role as scientists is to provide the knowledge and perspectives for effective practice and policies…. We have a moral obligation in our society to do what is necessary to improve health, and the health disparities research community should be in the vanguard of that movement. (p. s9)
Utilizing the framework of PHCR praxis, the health equity action research trajectory provides a transformational approach for action aimed at achieving the Healthy People 2020 goal of health equity for all.
Acknowledgments
This research was supported by the National Institutes of Health (NIH), National Institute on Minority Health and Health Disparities (PG60MD000207, S.B. Thomas, PI) and the NIH Office of the Director (7RC2MD004766, S.C. Quinn, PI). In addition, Drs. J. Butler, C.S. Fryer and M.A. Garza are all recipients of Mentored Career Development Awards (K01) from the NIH, National Cancer Institute. Additional financial support was provided by the Robert Wood Johnson Foundation, the Pittsburgh Foundation, the DSF Charitable Foundation, the Highmark Foundation, and Dr. Judith Davenport. We graciously thank our community participants in the Healthy Black Family Project and the black barbershop and beauty salon network, Health Advocates In-Reach and Research who shared their knowledge, expertise, and insight over a decade of work. Finally, we thank Dr. Janey Whalen for her superb review and feedback on early drafts of the manuscript.
Footnotes
These terms are used interchangeably throughout this review.
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
Contributor Information
Stephen B. Thomas, Email: sbt@umd.edu.
Sandra Crouse Quinn, Email: scquinn@umd.edu.
James Butler, Email: jbutler9@umd.edu.
Craig S. Fryer, Email: csfryer@umd.edu.
Mary A. Garza, Email: magarza@umd.edu.
LITERATURE CITED
- 1.Am. Assoc. Phys. Anthropol. (AAPA) Statement on biological aspects of race. Am J Phys Anthropol. 1996;101:569–70. [Google Scholar]
- 2.Am. Cancer Soc. Cancer Facts and Figures for African Americans 2005–2006. Atlanta: Am. Cancer Soc; 2005. [Google Scholar]
- 3.Anda RF, Croft JB, Felitti VJ, Nordenberg D, Giles WH, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282:1652–58. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 4.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 5.Black N. Why we need observational studies to evaluate the effectiveness of health care. Br Med J. 1996;312:1215–18. doi: 10.1136/bmj.312.7040.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boucher D, Paul K, editors. The Social Contract from Hobbes to Rawls. New York: Routledge; 1994. [Google Scholar]
- 7.Brach C, Fraserirector I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57(Suppl 1):181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Browne M. Full service: talking about fighting prostate cancer—in the barber shop! Health Educ Behav. 2007;34:557–58. [Google Scholar]
- 9.Cent. Dis. Control Prev. (CDC) Smoking attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR. 2008;57:1226–28. [PubMed] [Google Scholar]
- 10.Cent. Dis. Control Prev. (CDC) Cigarette smoking among adults and trends in smoking cessation—United States, 2008. MMWR. 2009;58:1227–32. [PubMed] [Google Scholar]
- 11.Cent. Dis. Control Prev. (CDC) Racial ethnic approaches community health. 2010 http://www.cdc.gov/reach/reach_2010/index.htm.
- 12.Cent. Dis. Control Prev., Off. Minor. Health Health Disparities. History of the office. 2010 http://www.cdc.gov/omhd/about/about.htm.
- 13.Colquitt J, Clegg A, Sidhu M, Royle P. The Cochrane Library. 3. Oxford: Update Software; 2003. Surgery for morbid obesity (Cochrane Review) [DOI] [PubMed] [Google Scholar]
- 14.Cooper RS. A case study in the use of race and ethnicity in public health surveillance. Public Health Rep. 1994;109:46–52. [PMC free article] [PubMed] [Google Scholar]
- 15.Cossrow N, Falkner B. Race/ethnic issues in obesity and obesity-related comorbidities. J Clin Endocrinol Metab. 2004;89:2590–94. doi: 10.1210/jc.2004-0339. [DOI] [PubMed] [Google Scholar]
- 16.Dankwa-Mullan I, Rhee KB, Stoff DM, Pohlhaus JR, Sy FS, Stinson N, Jr, et al. Moving toward paradigm-shifting research in health disparities through translational, transformational, and transdisciplinary approaches. Am J Public Health. 2010;100(Suppl 1):S19–24. doi: 10.2105/AJPH.2009.189167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dept. Health Hum. Serv. About the US Preventive Services Task Force. 2010 http://www.uspreventiveservicestaskforce.org/about.htm.
- 18.Dept. Health Hum. Serv. History: National Center on Minority Health and Health Disparities. 2010 http://ncmhd.nih.gov/about_ncmhd/history.asp and http://ncmhd.nih.gov/about_ncmhd/mission.asp.
- 19.Diabetes Prev. Progr. Res. Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention of metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du Bois WEB. The Souls of Black Folk. Oxford: Oxford Univ. Press; 1903. [Google Scholar]
- 21.Fine MJ, Ibrahim SA, Thomas SB. The role of race and genetics in health disparities research. Am J Public Health. 2005;95:2125–28. doi: 10.2105/AJPH.2005.076588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 23.Ford AF, Reddick K, Browne MC, Robins A, Thomas SB, Quinn S. Beyond the cathedral: building trust to engage the African American community in health promotion and disease prevention. Health Promot Pract. 2009;10:485–89. doi: 10.1177/1524839909342848. [DOI] [PubMed] [Google Scholar]
- 24.Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health. 2010;100(Suppl 1):S30–35. doi: 10.2105/AJPH.2009.171058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ford CL, Airhihenbuwa C. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. 2010;71(8):1390–98. doi: 10.1016/j.socscimed.2010.07.030. [DOI] [PubMed] [Google Scholar]
- 26.Freudenberg N, Olden K. Finding synergy: reducing disparities in health by modifying multiple determinants. Am J Public Health. 2010;100(Suppl 1):S25–30. doi: 10.2105/AJPH.2009.166389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fryer CS. Smoke what?: The nicotine dependence experiences of urban, African American youth. Presented at Annu. Meet. Expos. Am. Public Health Assoc. (APHA), 137th; Philadelphia. 2009. [Google Scholar]
- 28.Fullilove MT. Comment: abandoning “race” as a variable in public health research—an idea whose time has come. Am J Public Health. 1998;88:1297–98. doi: 10.2105/ajph.88.9.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gakidou EE, Murray CJL, Frenk J. Defining and measuring health inequality: an approach based on the distribution of health expectancy. Bull WHO. 2000;78:42–54. [PMC free article] [PubMed] [Google Scholar]
- 30.Gilbert K, Quinn S, Thomas S, Ford A. The urban context: a place to eliminate health disparities and build organizational capacity. J Prev Interv Commun. 2011;39:1–16. doi: 10.1080/10852352.2011.530168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gilmore RW. Golden Gulag: Prisons, Surplus, Crisis, and Opposition in Globalizing. Berkeley: Univ. Calif. Press; 2007. [Google Scholar]
- 32.Giovino GA. Epidemiology of tobacco use in the United States. Oncogene. 2002;21:7326–40. doi: 10.1038/sj.onc.1205808. [DOI] [PubMed] [Google Scholar]
- 33.Horowitz CR, Robinson M, Seifer S. Community-based participatory research from the margin to the mainstream: Are researchers prepared? Circulation. 2009;119(19):2633–42. doi: 10.1161/CIRCULATIONAHA.107.729863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson RB, Onwuegbuzie AJ, Turner LA. Toward a definition of mixed methods research. J Mixed Methods Res. 2007;1(2):112–33. [Google Scholar]
- 35.Jones C. The moral problem of health disparities. Am J Public Health. 2010;100(S1):47–51. doi: 10.2105/AJPH.2009.171181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kilbourne A, Switzer G, Hyman K, Crowley-Matoka M, Fine M. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96:2113–21. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.King G, Polednak A, Bendel R, Vilsaint MC, Nahata S. Disparities in smoking cessation between African Americans and whites: 1990–2000. Am J Public Health. 2004;94:1965–71. doi: 10.2105/ajph.94.11.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kumar S, Quinn S, Kriska A, Thomas S. “Food is directed to the area”: African Americans’ perceptions of the neighborhood nutrition environment in Pittsburgh. Health Place. 2011 doi: 10.1016/j.healthplace.2010.11.017. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miniño A, Xu J, Kochanek K, Tejada-Vera B. Death in the United States. 2007. Natl Cent Health Stat Data Brief. 2009;(26) http://www.cdc.gov/nchs/data/databriefs/db26.pdf. [PubMed]
- 40.Mokdad A, Marks J, Stroup D, Gerberding J. Actual causes of death in the United States. 2000. J Am Med Assoc. 2004;291:1238–45. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 41.Natl. Inst. Health (NIH) The NIH almanac—organization: National Center on Minority Health and Health Disparities. 2005 http://www.nih.gov/about/almanac/organization/NCMHD.htm.
- 42.Natl. Inst. Health (NIH) NIH announces Institute on Minority Health and Health Disparities: transition from center to institute highlights expanded responsibilities. 2010 http://www.nih.gov/news/health/sep2010/nimhd-27.htm.
- 43.NIH State-of-the-Science Panel. National Institutes of Health state-of-the-science conference statement on tobacco use: prevention, cessation, and control. Ann Intern Med. 2006;145:839–44. doi: 10.7326/0003-4819-145-11-200612050-00141. [DOI] [PubMed] [Google Scholar]
- 44.Paasche-Orlow M. The ethics of cultural competence. Acad Med. 2004;79:347–50. doi: 10.1097/00001888-200404000-00012. [DOI] [PubMed] [Google Scholar]
- 45.Paeratakul S, Lovejoy JC, Ryan DH, Bray GA. The relation of gender, race and socioeconomic status to obesity and obesity comorbidities in a sample of US adults. Int J Obes Relat Metab Disord. 2002;26:1205–10. doi: 10.1038/sj.ijo.0802026. [DOI] [PubMed] [Google Scholar]
- 46.Papadopoulous I, Lees S. Developing culturally competent researchers. J Adv Nurs. 2002;37:258–64. doi: 10.1046/j.1365-2648.2002.02092.x. [DOI] [PubMed] [Google Scholar]
- 47.Deleted in proof
- 48.Perez-Stable EJ, Herrera B, Jacob P, III, Benowitz NL. Nicotine metabolism and intake in black and white smokers. JAMA. 1998;280:152–56. doi: 10.1001/jama.280.2.152. [DOI] [PubMed] [Google Scholar]
- 49.Pletcher MJ, Hulley BJ, Houston T, Kiefe CI, Benowitz N, Sidney S. Menthol cigarettes, smoking cessation, atherosclerosis, and pulmonary function: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Arc Intern Med. 2006;166:1915–22. doi: 10.1001/archinte.166.17.1915. [DOI] [PubMed] [Google Scholar]
- 50.Powers M, Faden R. Social Justice: Moral Foundations of Public Health and Health Policy. New York: Oxford Univ. Press; 2006. [DOI] [PubMed] [Google Scholar]
- 51.Quinn S. The National Negro Health Movement: lessons for eliminating health disparities today. Minor Health Today. 2001;2:42–43. [Google Scholar]
- 52.Quinn S, Thomas S. The National Negro Health Week, 1915 to 1951: a descriptive account. J Wellness Perspect. 1996;12:172–79. [Google Scholar]
- 53.Resnicow K, Braithwaite R. Cultural sensitivity in public health. In: Braithwaite R, Taylor S, editors. Health Issues in the Black Community. 2 San Francisco: Jossey-Bass; 2001. pp. 516–42. [Google Scholar]
- 54.Ruffin J. The science of eliminating health disparities: embracing a new paradigm. Am J Public Health. 2010;100:S8–9. doi: 10.2105/AJPH.2010.191957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tashakkori A, Creswell JW. Editorial: the new era of mixed methods. J Mixed Methods Res. 2007;1:3–7. [Google Scholar]
- 56.Task Force Community Prev. Serv. The Guide to Community Preventive Services: What Works to Promote Health? Oxford: Oxford Univ. Press; 2005. Updates: Preventing http://www.thecommunityguide.org/obesity/index.htm. [Google Scholar]
- 57.Task Force Community Prev. Serv. The Guide to Community Preventive Services: What Works to Promote Health? Oxford: Oxford Univ. Press; 2005. Updates: Tobacco Use, http://www.thecommunityguide.org/tobacco/index.html. [Google Scholar]
- 58.Thomas SB. The color line: race matters in the elimination of health disparities. Am J Public Health. 2001;91:1046–48. doi: 10.2105/ajph.91.7.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thomas SB, Benjamin GC, Almario D, Lathan MJ. Historical and current policy efforts to eliminate racial and ethnic health disparities in the United States: future opportunities for public health education research. Health Promot Pract. 2006;7:324–30. doi: 10.1177/1524839906289379. [DOI] [PubMed] [Google Scholar]
- 60.Thomas SB, Quinn SC. Poverty and elimination of urban health disparities: challenge and opportunity. Ann N Y Acad Sci. 2008;1136:111–25. doi: 10.1196/annals.1425.018. [DOI] [PubMed] [Google Scholar]
- 61.Tumiel-Berhalter LM, McLaughlin-Diaz V, Vena J, Crespo CJ. Building community research capacity: process evaluation of community training and education in a community-based participatory research program serving a predominately Puerto Rican community. Prog Commun Health Partnerships: Res Educ, Action. 2007;1:89–97. doi: 10.1353/cpr.0.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.U.S. Census Bur. An older and more diverse nation by midcentury. 2008 From http://www.census.gov/newsroom/releases/archives/population/cb08-123.html.
- 63.U.S. Census Bur. Expectation of life at birth, 1970 to 2006, and projections, 2010 to 2020. 2010 http://www.census.gov/compendia/statab/2010/tables/10s0102.pdf.
- 64.U.S. Census Bur. Fact Sheet. 2006–2008 American community survey 3-year estimates. 2010 http://factfinder.census.gov/servlet/SAFFPopulation.
- 65.U.S. Congress. Health Care and Education Reconciliation Act of 2010. 2010 (H.R. 4872). http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=111_cong_public_laws&docid=f:publ152.111.pdf.
- 66.U.S. Dep. Health Hum. Serv. Report of the Secretary’s Task Force on Black and Minority Health. Washington, DC: U.S. GPO; 1985. [Google Scholar]
- 67.U.S. Dep. Health Hum. Serv. Healthy people 2000: National health promotion and disease prevention objectives. Washington, DC: U.S. GPO; 1991. [Google Scholar]
- 68.U.S. Dep. Health Hum. Serv. Healthy People 2010: Understanding and Improving Health. 2 Washington, DC: U.S. GPO; 2000. [Google Scholar]
- 69.U.S. Dep. Health Hum. Serv. The Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity. Rockville, MD: U.S. Dep. Health Hum. Serv, Public Health Serv., Off. Surg. Gen; 2001. http://www.surgeongeneral.gov/topics/obesity/calltoaction/CalltoAction.pdf. [PubMed] [Google Scholar]
- 70.U.S. Dep. Health Hum. Serv. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta, GA: US Dep. Health Hum. Serv., Cent. Dis. Control Prev., Natl. Cent. Chronic Dis. Prev. Health Promot., Off. Smok. Health; 2004. http://www.cdc.gov/tobacco/data_statistics/sgr/sgr_2004/index.htm. [Google Scholar]
- 71.U.S. Dep. Health Hum. Serv. Healthy People 2020. Framework. 2009 http://www.healthypeople.gov/hp2020/advisory/PhaseI/PhaseI.pdf.
- 72.U.S. Senate. Patient Protection and Affordable Care Act. 2010 http://democrats.senate.gov/reform/patient-protection-affordable-care-act-as-passed.pdf.
- 73.Vlahov D, Galea S, Freudenberg N. Creating healthier cities: Where do we go from here? In: Freudenberg N, Galea S, Vlahov D, editors. Cities and the Health of the Public. Nashville, TN: Vanderbilt Univ. Press; 2006. pp. 327–43. [Google Scholar]
- 74.Vogel K, Murthy V, Dudley B, Grubs R, Gettig E, et al. The use of family health histories to address health disparities in an African American community. Health Promot Pract. 2007;8(4):350–57. doi: 10.1177/1524839906293395. [DOI] [PubMed] [Google Scholar]
- 75.Wakefield MA, Chaloupka FJ, Kaufman NJ, Orleans CT, Barker DC, Ruel EE. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: cross sectional study. Br Med J. 2000;321:333–37. doi: 10.1136/bmj.321.7257.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Williams D. Race, socioeconomic status, and health: the added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–88. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 77.World Health Organ. (WHO) Health impact assessment glossary of terms. 2010 http://www.who.int/hia/about/glos/en/index1.html.