Abstract
Background
Patients with chronic heart failure (HF) and with elevated depression symptoms are at greater risk of morbidity and mortality. Somatic symptoms of depression are particularly prevalent in HF and are related to worse disease prognosis. T'ai chi practice is related to increased emotional well-being in various clinical populations; however, relatively little is known about t'ai chi's effects on somatic versus cognitive symptom dimensions of depression in HF.
Purpose
The objective of the study was to measure whether a t'ai chi intervention effectively reduces somatic and/or cognitive symptoms of depression in patients with HF.
Methods
Patients with HF were assigned to either t'ai chi training (n=16) or a usual-care group (n=12). At baseline and after the 12-week intervention period, participants were evaluated for changes in depressive symptoms using Beck Depression Inventory (BDI) total scores (BDI-t) and subcategorized scores of BDI-somatic (BDI-s) and BDI-cognitive (BDI-c), and for symptoms of fatigue using the Multidimensional Fatigue Symptom Inventory–Short Form.
Results
Patients with HF in the t'ai chi group compared to the usual-care group had reduced BDI-s (p≤0.017), but not BDI-c (p=0.50) scores from pre- to postintervention. Although t'ai chi did not significantly reduce fatigue, changes in physical fatigue (p≤0.05) were independently associated with changes in BDI-t scores.
Conclusions
T'ai chi practice reduced somatic symptoms of depression, which have been linked to worse prognosis in HF. Reductions in fatigue appear to explain some but not all of the reductions in somatic symptoms of depression.
Introduction
Heart failure (HF) affects between 5 and 6 million North Americans, and rates of new diagnoses are predicted to triple in the next 3 decades as the population ages.1 Comorbid depressive disorders are present in up to 40% of HF patients,2,3 which in turn are associated with increased mortality, clinical events, rehospitalization, and general health care use,4 yet the efficacy of antidepressant therapy in patients with coronary heart disease (CHD) has had only minor effects on reducing depressive symptoms.5 One reason for the lack of depression treatment efficacy in patients with HF may be the heterogeneity of depression as a syndrome in this population.6 Various investigations have attempted to distinguish somatic from cognitive dimensions of depression for patients with CHD,7 and research shows that somatic symptoms of depression are both highly prevalent8 and have a greater relationship with cardiovascular disease prognosis in patients with CHD.9–11 More specifically, patients with HF with elevated somatic depressive symptoms have an increased incidence of mortality over a 3-year follow-up period, while patients with heightened cognitive depressive symptoms do not.6
Research suggests that somatic symptoms such as fatigue and sleep disturbances, which are common in patients with HF,12 may lead to physical inactivity and create a spiraling decline in physical and cardiac function. Recent evidence indicates that physical inactivity may be one mediator of HF disease outcomes.13 Nonpharmacological behavioral/lifestyle changes may therefore be useful to reduce somatic symptoms that may be associated with decrements in cardiac function in patients with HF.14 Standard exercise programs, such as home-based walking, and group aerobic exercise such as bicycle and treadmill, result in improvements in physical function and cardiac functional capacity.15 However, HF exercise studies have been conducted with relatively young patients (e.g., average age of 59 years in the HF ACTION study) having little comorbidity,16 yet 88% of patients with HF are over the age of 65.17 Furthermore, such exercise interventions are associated with low compliance rates,18 which may result from patients with HF finding standard aerobic exercise regimens too arduous and exhausting. In fact, one investigation observed that due to safety considerations for home-exercise walking interventions, less than half of patients treated by specialist HF services were eligible for participation.19 Thus, development of exercise interventions for patients with HF with a wide range of ages and physical function is needed.
T'ai chi may be ideal for a broader range of patients with HF; it is composed of low-impact, mindfully meditative movements with integrated breathing techniques that generate an aerobic workout.20 The level of intensity is adjustable by using larger or smaller movements, and works the entire body. Many t'ai chi interventions have been studied specifically in elderly and frail cohorts with various comorbidities21 and are well tolerated across fitness levels in patients with HF.22 Furthermore, t'ai chi practice is beneficial in patients with HF with a range of depression symptom levels, not just those with major depression.23 However, little is known about the effectiveness of t'ai chi practice specifically on somatic and cognitive dimensions of depression, which could impact HF prognosis. In order to determine whether t'ai chi practice reduces symptoms of depression and evaluate whether these changes are principally due to decreases in somatic symptoms, the present study measured alterations in Beck Depression Index scores subcategorized into somatic/affective (BDI-s) and cognitive/affective (BDI-c) symptoms.24 In addition, the specific influence of fatigue was examined to further understand potential mechanisms of t'ai chi-associated changes in depressive symptoms.
Methods
The present study included patients with HF (NYHA class II) who were 43–83 years old (mean age=67.0 standard deviation [SD]=11.9) and 87.5% male. They were assigned to either Yang-style T'ai Chi Chuan-Short Form (first third) (Table 1) training twice per week for 60 minutes per session for 12 weeks (n=16) or a usual-care control group (n=12). T'ai chi participants were asked to practice at home for 10–20 minutes per day, on days they were not attending the t'ai chi classes. The t'ai chi instructor is a certified holistic health practitioner and Asian Bodywork Therapist, a Black belt in Shaolin Kempo, is currently training in Ba Gua Zhang Kung fu, and has 10 years of experience teaching t'ai chi to chronically ill and older adults. Patients were recruited from the VA San Diego Medical Center and the University of California (UCSD) Medical Center from 2006 to 2008 and consented to be included in the UCSD Institutional Review Board–approved research study. To limit the likelihood of changes in treatments during the course of the study, strict inclusion and exclusion criteria were established. Subjects were required to be clinically stable (defined as not having been hospitalized for a 3-month period), to be on stable doses of neurohormonal blocking agents and diuretics for at least 3 months, and to have had no cardiac surgeries for at least 6 months. Participants in both groups (t'ai chi group and usual-care controls) were not concurrently enrolled in any exercise programs during the study period. All participants (t'ai chi group and usual-care controls) continued to receive usual care, which included regular visits to their cardiologist, primary care physicians, and other health specialists.
Table 1.
Warm-up Exercises and T'ai Chi Chuan Yang–Style Short Form–First Third
| Warm-up exercises |
| 1. Waist turns |
| 2. T'ai chi beginning |
| 3. Pushing the wave |
| 4. Wave hands like clouds |
| 5. Embracing the tree standing posture |
| T'ai chi movements |
| 1. Preparation |
| 2. Beginning |
| 3. Ward off left |
| 4. Ward off right |
| 5. Roll back |
| 6. Press |
| 7. Withdraw and push |
| 8. Single whip |
| 9. Lifting hands |
| 10. Shoulder strike |
| 11. White crane spreads wings |
| 12. Brush knee |
| 13. Play guitar |
| 14. Brush knee |
| 15. Deflect downward and punch |
| 16. Withdraw and push |
| 17. Cross hands |
At baseline and after the 12-week intervention period, participants were evaluated for changes in depressive symptoms using BDI total scores (BDI-t) and subcategorized scores of BDI-s and BDI-c, as well as for symptoms of fatigue measured using the Multidimensional Fatigue Symptom Inventory–Short Form.25 Linke et al. (2009)10 determined a two-factor structure within the BDI, a somatic/affective (12 items) and a cognitive/affective factor (9 items). Other studies confirm this model in both patient and healthy groups.26,27
Mixed-design analyses of covariance (ANCOVA) were performed to examine between factors (t'ai chi versus usual care) and within factors (pre- and postintervention) while controlling for age, gender, cardiac ejection fraction (EF) as an indicator of HF severity, and category of HF (preserved versus unpreserved systolic function). Influences of fatigue were examined as covariates in the ANCOVA equations. Exploratory analyses were performed including the use of a nonparametric Friedman Test for descriptive purposes to determine the rank order of the 21 BDI items contributing to baseline BDI-t scores. Also, exploratory ANCOVA analyses were performed on a subgroup of patients in the top 75% of BDI-t scores, with mean scores above the clinical cut-point ≥10 (Beck et al. 1996)24 to determine whether patients with elevated BDI-t scores had significant reductions associated with t'ai chi practice compared with controls.
Results
Twenty-four (24) of 28 patients with HF completed the study. Four (4) patients dropped out of the t'ai chi group due to scheduling conflict (n=1), lack of interest (n=1), foot injury outside of class (n=1), and HF exacerbation unrelated to t'ai chi (n=1). Baseline BDI-t scores did not differ between those completing and dropping out (p=0.54). There were no significant differences between groups for ejection fraction, gender, number of HF patients with preserved systolic function, body–mass index (BMI), or BDI scores. However, the t'ai chi participants were significantly older than the controls (Table 2). A nonparametric Friedman Test determined the rank order of the 21 BDI items contributing to baseline BDI-t scores; fatigue, work difficulty, and dissatisfaction were the top three items ranked, respectively, suggesting that they exerted the greatest influence on baseline BDI-t. Mean BDI-t baseline scores for the t'ai chi (7.95±4.0) versus control (9.3±6.6) group were not significantly different (p=0.54). Participants completed a mean of 21 of 24 classes (SD=1.4). BMI was not correlated with BDI-t (r=−0.38, p=0.12).
Table 2.
Characteristics of Heart Failure Patients at Baseline
| T'ai chi group (n=12) | Control group (n=12) | p-Value | |
|---|---|---|---|
| Ejection fraction (mean %, SD) | 39.1 (14.9) | 30.9 (8.0) | 0.16 |
| HF with Preserved Systolic (n) | 3 | 2 | 0.51 |
| Body–mass index | 29.7 (5.03) | 31.4 (8.8) | 0.65 |
| Female (n) | 2 | 1 | 0.75 |
| Age (mean years, SD) | 72.6 (6.2) | 63.9 (12.0) | 0.04* |
| BDI baseline score (mean, SD) | 7.95 (4.0) | 9.2 (6.6) | 0.54 |
| Physical function: 6 min-walk test (mean meters, SD) | 334.7 (116.7) | 312.7 (97.3) | 0.67 |
p≤.05.
SD, standard deviation; BDI, Beck Depression Inventory Score.
Dimensions of depression
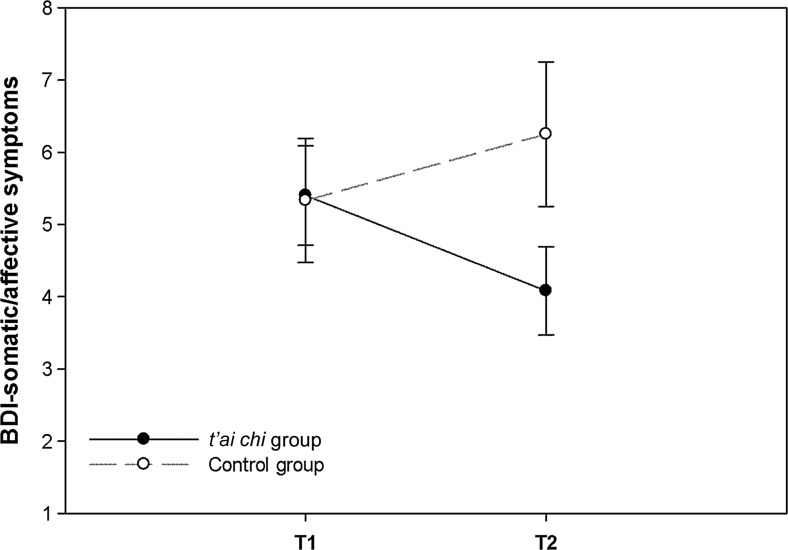
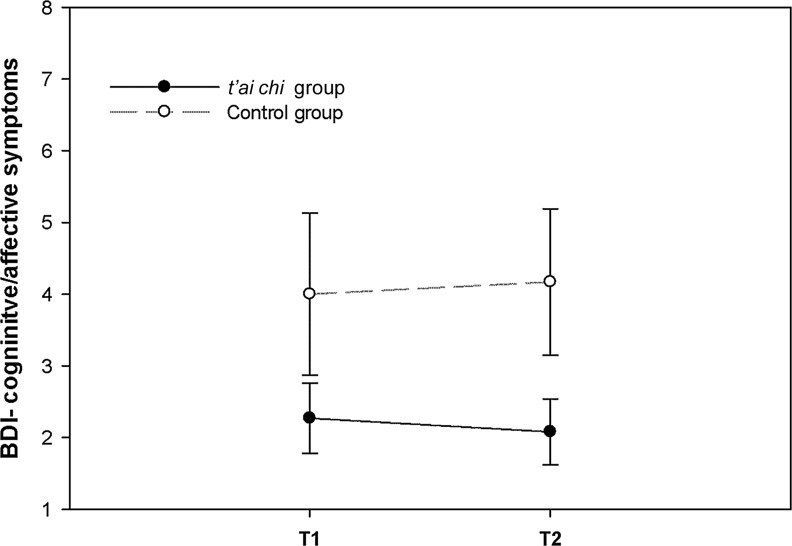
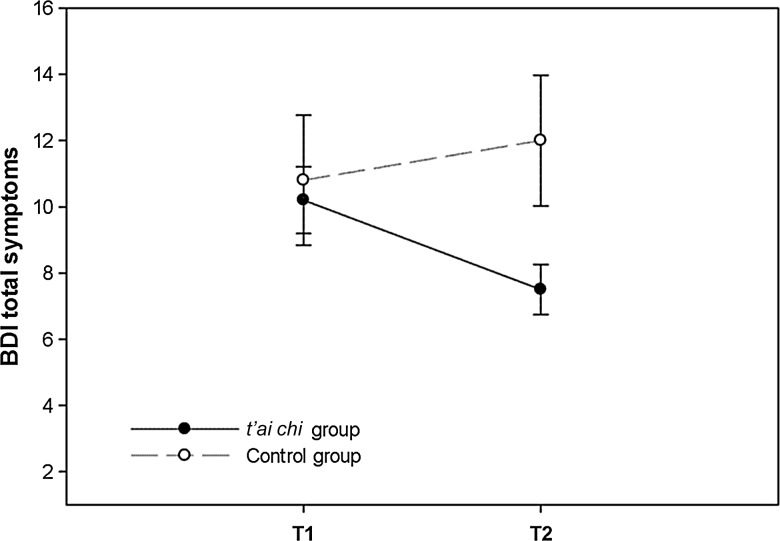
Compared to controls, patients with HF in the t'ai chi group experienced reduced BDI-t symptom scores from pre- to postintervention, with a significant group-by-time interaction (F[4, 19]=4.5, p<0.05, partial η2=0.28) after controlling for age, gender, EF and category of HF. A significant group-by-time interaction was also detected for BDI-s (F[4, 19]=4.5, p<0.05), but not for BDI-c (p=0.16) after controlling for age, gender, EF, and type of HF (Figs. 1 and 2). Thirty-eight percent (38%) of t'ai chi participants compared with none of the controls showed improvements by at least 1 SD in BDI-t symptom scores. Similarly, 33% of t'ai chi participants and none of the controls showed improvements by at least 1 SD in BDI-s symptom scores. Eight percent (8%) of t'ai chi participants and no controls showed improvements by at least 1 SD in BDI-c symptoms. An exploratory analyses revealed that in a subgroup of patients in the top 75% of BDI-t scores (n=18, mean BDI-t=10.5±4.9; controls=10.8±6.2 and t'ai chi group=10.2±2.9) with mean scores above the clinical cut-point ≥10, there was a significant group-by-time interaction (F[3, 14]=5.1, p<0.05) whereby BDI-t was reduced to 7.5 in the t'ai chi group compared with the control group, which had an increase to 12.0 (Fig. 3).
FIG. 1.
Changes in Beck Depression Inventory Score (BDI) somatic/affective symptoms (means±standard error of the mean) from T1 (baseline) to T2 (post-12-week intervention period) in patients with heart failure trained in t'ai chi versus usual-care controls.
FIG. 2.
Changes in Beck Depression Inventory Score (BDI) cognitive/affective symptoms (means±standard error of the mean) from T1 (baseline) to T2 (post-12-week intervention period) in patients with heart failure trained in t'ai chi versus usual-care controls.
FIG. 3.
Changes in Beck Depression Inventory Score (BDI) total symptoms (means±standard error of the mean) in patients with heart failure with baseline BDI scores in the top 75% from T1 (baseline) to T2 (post-12-week intervention period) in patients trained in t'ai chi versus usual-care controls.
Influence of fatigue on depressive symptoms
Changes in Multidimensional Fatigue Symptom Inventory (MFSI) physical fatigue from pre- to postintervention were independently associated with changes in BDI-t scores, even after controlling for age and EF (β=0.510, p=0.027). Although patients with HF in the t'ai chi group had reduced MFSI total fatigue (F[4, 19]=4.2, p≤0.05, r=0.43) from the pre- to postintervention period compared with controls, controlling for EF attenuated group-by-time interaction effects and were no longer significant (p=0.19).
Discussion
The present study determined that t'ai chi was effective in patients with HF for reducing both total depression scores and somatic/affective symptoms of depression compared to usual-care patients. T'ai chi–associated diminishment of fatigue was related to reductions of total depression symptoms regardless of HF severity. However, t'ai chi practice did not appear to reduce overall fatigue as an independent symptom when HF severity was taken into account. Thus, t'ai chi seems to be effective in reducing a composite of variables, including fatigue, that make up somatic/affective symptoms of depression. Moreover, the average age of patients in the present study was greater than that in most previous HF exercise studies,16,28 which is consistent with studies suggesting that t'ai chi is well tolerated across fitness and age levels in patients with HF.29
Although the findings are promising and suggest that t'ai chi is beneficial for reducing depressive symptoms, particularly somatic, the main limitation of this pilot study is the modest sample size. Larger investigations with a bigger HF sample size are needed to replicate these findings. Furthermore, the average BDI-t score for patients in both groups was lower than considered clinically significant, which is described in the literature as ≥10.24 However, when a subgroup of patients with BDI-t scores in the top 75% were examined independently, with average BDI scores ≥10, t'ai chi practice was associated with reductions of depressive symptoms to below clinical levels, suggesting that t'ai chi practice may be clinically effective. These preliminary findings should be replicated in larger cohorts of patients with HF with elevated depressive symptoms. Additional limitations of the present pilot study include the lack of a follow-up period to determine how long the effects of performing t'ai chi lasted on depression symptoms or whether the participants continued to practice t'ai chi after their involvement in the study ended. Thus, future studies should be undertaken to explore the enduring effects of t'ai chi practice within this population. Finally, future studies are needed to determine whether alterations in depressive symptoms relate to improved HF prognosis, which was beyond the scope of the present pilot study. The strengths of the study include a carefully selected group of patients with HF and a highly standardized t'ai chi intervention that the vast majority of participants were able to complete. There was a 20% dropout rate in the t'ai chi group, which compared with other exercise studies for HF is much higher.18
This study may have particular clinical relevance since a recent American Heart Association recommendation was made to assess depression in all patients with coronary artery disease/cardiovascular disease.30 The current study may further indicate that clinical assessment of depression should address the unique dimensions of depression as they each can impact health behaviors differently and potentially long-term health outcomes. It has been suggested that somatic symptoms may drive depression-related poorer cardiovascular disease prognosis in CHD9–11 and in patients with HF.6 Thus, t'ai chi has promise as an additional intervention for the 20%–40% patients with HF who will screen positive for depression. Antidepressants are validated, but far from universally effective in patients with heart disease.31 Combined with the aging and growing HF population, new treatments for depression are needed.
Conclusions
In conclusion, participating in a t'ai chi program may be beneficial for patients with HF to reduce somatic symptoms of depression, including fatigue, across age and fitness levels.
Acknowledgment
This study was funded by National Institutes of Health, National Center for Complementary and Alternative Medicine, grant number 1 R21 AT001910-01A2.
Disclosure Statement
No financial conflicts exist.
References
- 1.York KM. Hassan M. Sheps DS. Psychobiology of depression/distress in congestive heart failure. Heart Fail Rev. 2009;14:35–50. doi: 10.1007/s10741-008-9091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jiang W. Kuchibhatla M. Cuffe MS, et al. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110:3452–3456. doi: 10.1161/01.CIR.0000148138.25157.F9. [DOI] [PubMed] [Google Scholar]
- 3.Norra C. Skobel EC. Arndt M. Schauerte P. High impact of depression in heart failure: Early diagnosis and treatment options. Int J Cardiol. 2008;125:220–231. doi: 10.1016/j.ijcard.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 4.Rutledge T. Reis VA. Linke SE, et al. Depression in heart failure: A meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 5.Thombs BD. de Jonge P. Coyne JC, et al. Depression screening and patient outcomes in cardiovascular care: A systematic review. JAMA. 2008;300:2161–2171. doi: 10.1001/jama.2008.667. [DOI] [PubMed] [Google Scholar]
- 6.Schiffer AA. Pelle AJ. Smith OR, et al. Somatic versus cognitive symptoms of depression as predictors of all-cause mortality and health status in chronic heart failure. J Clin Psychiatry. 2009;70:1667–1673. doi: 10.4088/JCP.08m04609. [DOI] [PubMed] [Google Scholar]
- 7.de Jonge P. Ormel J. van den Brink RH, et al. Symptom dimensions of depression following myocardial infarction and their relationship with somatic health status and cardiovascular prognosis. Am J Psychiatry. 2006;163:138–144. doi: 10.1176/appi.ajp.163.1.138. [DOI] [PubMed] [Google Scholar]
- 8.Martens EJ. Denollet J. Pedersen SS, et al. Relative lack of depressive cognitions in post-myocardial infarction depression. J Affect Disord. 2006;94:231–237. doi: 10.1016/j.jad.2006.04.023. [DOI] [PubMed] [Google Scholar]
- 9.Martens EJ. Hoen PW. Mittelhaeuser M, et al. Symptom dimensions of post-myocardial infarction depression, disease severity and cardiac prognosis. Psychol Med. 2010;40:807–814. doi: 10.1017/S0033291709990997. [DOI] [PubMed] [Google Scholar]
- 10.Linke S. Rutledge T. Johnson B, et al. Depressive symptom dimensions and cardiovascular prognosis among women with suspected myocardial ischemia: A report from the National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation. Arch Gen Psychiatry. 2009;66:499–507. doi: 10.1001/archgenpsychiatry.2009.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoen PW. Whooley MA. Martens EJ, et al. Differential associations between specific depressive symptoms and cardiovascular prognosis in patients with stable coronary heart disease. J Am Coll Cardiol. 2010;56:838–844. doi: 10.1016/j.jacc.2010.03.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Redeker N. Somatic symptoms explain differences in psychological distress in heart failure patients vs a comparison group. Prog Cardiovasc Nurs. 2006;21:182–189. doi: 10.1111/j.0889-7204.2006.05643.x. [DOI] [PubMed] [Google Scholar]
- 13.Whooley M. de Jonge P. Vittinghoff E, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coats A. Advances in the non-drug, non-surgical, non-device management of chronic heart failure. Int J Cardiol. 2005;100:1–4. doi: 10.1016/j.ijcard.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Bensimhon D. Leifer E. Ellis S, et al. Reproducibility of peak oxygen uptake and other cardiopulmonary exercise testing parameters in patients with heart failure (from the Heart Failure and A Controlled Trial Investigating Outcomes of exercise traiNing) Am J Cardiol. 2008;102:712–717. doi: 10.1016/j.amjcard.2008.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Witham M. Daykin A. McMurdo M. Pilot study of an exercise intervention suitable for older heart failure patients with left ventricular systolic dysfunction. Eur J Cardiovasc Nurs. 2008;7:303–306. doi: 10.1016/j.ejcnurse.2008.01.109. [DOI] [PubMed] [Google Scholar]
- 17.Prescott E. Hjardem-Hansen R. Dela F, et al. Exercise training in older patients with systolic heart failure: Adherence, exercise capacity, inflammation and glycemic control. Scand Cardiovasc J. 2009;43:249–255. doi: 10.1080/14017430802593427. [DOI] [PubMed] [Google Scholar]
- 18.Barbour K. Miller N. Adherence to exercise training in heart failure: A review. Heart Fail Rev. 2008;13:81–89. doi: 10.1007/s10741-007-9054-x. [DOI] [PubMed] [Google Scholar]
- 19.Jolly K. Taylor R. Lip G, et al. The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: Cost-effectiveness and patient adherence. Health Technol Assess. 2007;11:1–118. doi: 10.3310/hta11350. [DOI] [PubMed] [Google Scholar]
- 20.Irwin M. Pike J. Oxman M. Shingles immunity and health functioning in the elderly: Tai Chi Chih as a behavioral treatment. Evid Based Complement Alternat Med. 2004;1:223–232. doi: 10.1093/ecam/neh048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang C. Collet JP. Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: A systematic review. Arch Intern Med. 2004;164:493–501. doi: 10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- 22.Yeh G. Wood MJ. Lorell BH, et al. Effects of tai chi mind–body movement therapy on functional status and exercise capacity in patients with chronic heart failure: A randomized controlled trial. Am J Med Sci. 2004;117:541–548. doi: 10.1016/j.amjmed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 23.Barrow D. Bedford A. Ives G, et al. An evaluation of the effects of Tai Chi Chuan and Chi Kung training in patients with symptomatic heart failure: A randomised controlled pilot study. Postgrad Med J. 2007;83:717–721. doi: 10.1136/pgmj.2007.061267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beck AT. Steer RA. Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 25.Stein KD. Martin SC. Hann DM. Jacobsen PB. A multidimensional measure of fatigue for use with cancer patients. Cancer Pract. 1998;6:143–152. doi: 10.1046/j.1523-5394.1998.006003143.x. [DOI] [PubMed] [Google Scholar]
- 26.Kojima M. Furukawa TA. Takahashi H, et al. Cross-cultural validation of the Beck Depression Inventory-II in Japan. Psychiatric Res. 2002;110:291–299. doi: 10.1016/s0165-1781(02)00106-3. [DOI] [PubMed] [Google Scholar]
- 27.Grothe KB. Dutton GR. Jones GN, et al. Validation of the Beck Depression Inventory–II in a low-income African American sample of medical outpatients. Psychol Assessment. 2005;17:110–114. doi: 10.1037/1040-3590.17.1.110. [DOI] [PubMed] [Google Scholar]
- 28.Haykowsky MJ. Liang Y. Pechter D, et al. A meta-analysis of the effect of exercise training on left ventricular remodeling in heart failure patients: The benefit depends on the type of training performed. J Am Coll Cardiol. 2007;49:2329–2336. doi: 10.1016/j.jacc.2007.02.055. [DOI] [PubMed] [Google Scholar]
- 29.Yeh G. Mietus J. Peng C, et al. Enhancement of sleep stability with Tai Chi exercise in chronic heart failure: Preliminary findings using an ECG-based spectrogram method. Sleep Med. 2007;9:527–536. doi: 10.1016/j.sleep.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lichtman JH. Bigger JT., Jr Blumenthal JA, et al. Depression and coronary heart disease: Recommendations for screening, referral, and treatment. A science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: Endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 31.Huynh NN. McIntyre RS. What are the implications of the STAR*D Trial for Primary Care? A review and synthesis. Prim Care Companion J Clin Psychiatry. 2008;10:91–96. doi: 10.4088/pcc.v10n0201. [DOI] [PMC free article] [PubMed] [Google Scholar]