Abstract
AIM: To investigate matrix metalloproteinases (MMPs) and their tissue inhibitors (TIMPs) in pouch mucosa of pediatric onset ulcerative colitis (UC).
METHODS: In this cross-sectional study, 28 patients with pediatric onset UC underwent ileal pouch biopsy 13 years (median) after proctocolectomy. Expression of MMPs-3, -7, -8, -9, -12 and -26 and TIMPs-1, -2 and -3 in samples was examined using immunohistochemichal methods, and another biopsy was used to evaluate the grade of histological inflammation. Two investigators independently graded the immunohistochemical specimens in a semiquantitative fashion, using a scale marking staining intensity as follows: 0 = less than 20 positive cells; 1 = 20-50 positive cells; 2 = 50-200 positive cells; 3 = over 20 positive cells. Fecal calprotectin and blood inflammatory markers [serum C-reactive protein (CRP) and erythrocyte sedimentation rate] were determined during a follow-up visit to examine correlations between these markers and the expression of MMPs and TIMPs.
RESULTS: Of the 28 patients with pediatric onset UC, nine had not experienced pouchitis, whereas thirteen reported a single episode, and six had recurrent pouchitis (≥ 4 episodes). At the time of the study, six patients required metronidazole. In all of the others, the most recent episode of pouchitis had occurred over one month earlier, and none were on antibiotics. Only four samples depicted no sign of inflammation, and these were all from patients who had not had pouchitis. Two samples were too small to determine the grade of inflammation, but both had suffered pouchitis, the other recurrent. No sample depicted signs of colonic metaplasia. Most pouch samples showed expression of epithelial (e) and stromal (s) MMP-3 (e, n = 22; s, n = 20), MMP-7 (e, n = 28; s, n = 27), MMP-12 (e, n = 20; s, n =24), TIMP-2 (e, n = 23; s, n = 23) and MMP-3 (e, n = 23; s, n = 28) but MMP-8 (e, n = 0; s, n = 1), MMP-9 (e, n = 0; s, n = 9) and MMP-26 (e, n = 0; s, n = 3) and TIMP-1 (n = 0, both) were lacking. In samples with low grade of inflammatory activity, the epithelial MMP-3 and MMP-7 expression was increased (r = -0.614 and r = -0.472, respectively, P < 0.05 in both). MMPs and TIMPs did not correlate with the markers of inflammation, fecal calprotectin, erythrocyte sedimentation rate, or CRP, with the exception of patients with low fecal calprotectin (< 100 μg/g) in whom a higher expression of epithelial MMP-7 was found no differences in MMP- or TIMP-profiles were seen in patients with a history of pouchitis compared to ones with no such episodes. Anastomosis with either straight ileoanal anastomosis or ileoanal anastomosis with J-pouch did depict differences in MMP- or TIMP-expression.
CONCLUSION: The expression of MMPs pediatric UC pouch in the long-term shares characteristics with inflammatory bowel disease, but inflammation cannot be classified as a reactivation of the disease.
Keywords: Children, Matrix metalloproteinase 3, Tissue inhibitor of matrix metalloproteinase 3, Matrix metalloproteinase 7, Pouchitis, Ulcerative colitis
INTRODUCTION
In children, ulcerative colitis (UC) appears to present more aggressively than in adults[1,2]. The number of pediatric UC cases requiring colectomy within the first decade after diagnosis may reach 24%[1]. Restorative proctocolectomy with ileoanal anastomosis (IAA) and an ileal pouch-anal anastomosis is the surgical treatment of choice in UC[2].
In proctocolectomized patients, pouchitis is a common complication, and over two thirds of children undergoing proctocolectomy will suffer at least one episode of pouchitis during the following decade[2]. Yet, studies on pouchitis in children are limited. Pouchitis is an idiopathic inflammatory condition of the ileal reservoir occurring frequently after colectomy with IAA[3]. The etiology of pouchitis is poorly understood, but it is associated with risk factors such as extensive colonic disease preoperatively and young age at proctocolectomy[4]. The incidence of pouchitis is higher in UC than in familial adenomatous polyposis[5], and pouchitis has been considered a recurrent form of colitis[5,6]. Ileal pouch mucosa may acquire colonic characteristics[7,8], and colonic metaplasia is more pronounced in patients with pouchitis[9]. This mucosal transformation could have a role in the pathogenesis of pouchitis, possibly allowing the recurrence of inflammatory bowel disease (IBD) and may represent a novel manifestation IBD[7-9].
Matrix metalloproteinases (MMPs) are a family of 24 zinc-dependent enzymes implicated in mucosal damage in IBD[10]. MMPs take part in normal mucosal defense, and are capable of degrading extracellular matrix and basement membrane proteins in tissue remodeling processes both in normal and in pathological conditions[10]. In IBD, MMP-9 is the most abundantly expressed MMP, and it shows increased activity in inflamed UC mucosa[11]. Other MMPs have also been linked to inflammation severity in IBD, such as MMP-7[12]. Our group has demonstrated enhanced MMPs-1, -3 and -7 expression in IBD, and shown MMP-10 expression in IBD granulation tissue[13,14]. In pediatric IBD, we have described increased expression of epithelial MMP-10 and stromal tissue inhibitor (TIMP)-3[15].
The pathogenesis of pouchitis is unknown, and it is debated whether or not the inflammation is similar to that found in UC, or whether it is inflammation of a novel kind. The management of pouchitis by antibiotics and probiotics is widely accepted. Yet, according to a recent review, antibiotics are not significantly better than a placebo, compared to the high dose probiotics. By altering the endogenous flora and the expression of inflammation parameters, as well as competing with pathogens for receptor binding, nutrients, and growth factors, the high dose probiotics are effective in treatment of pouchitis[16]. The occurring inflammation and acquisition of colonic characteristics[7,8] inspires an interest in the MMP and TIMP-profile of pouch. We are aware of only two studies of MMP expression in pouchitis in adults[17,18]. Expression of MMP-1 and MMP-2 in pouchitis is different from normal ileal mucosa, but is similar to expression in active UC colitis[17]. We examined the MMP and TIMP profiles of pouch patients who had undergone proctocolectomy in their childhood or adolescence, and to find clues to the type of inflammation appearing in the pouch. It is important to determine whether this inflammation is IBD-like or of a novel kind, to appropriately prevent and manage pouchitis in the future.
MATERIALS AND METHODS
Patients and setting
Between 1985 and 2005, 81 pediatric patients with UC underwent proctocolectomy with ileal anastomosis at Tampere University Hospital or Children’s Hospital, Helsinki. Of these colectomized patients, one died of an unrelated cause and one emigrated. Thus, 79 patients were traced from the database of the Population Register Centre and contacted by mail during 2006. Thirty-five patients agreed to participate for a follow up visit described elsewhere in detail[2], but seven had been rediagnosed as Crohn’s disease (CD). The 28 UC cases were included in this study (Table 1). All proctocolectomies included transanal mucosectomy and a hand-sewn anastomosis. Twenty-one patients had an IAA with J-pouch, and 7 had straight ileoanal anastomosis (SIAA). Patients filled out a questionnaire surveying the current diagnosis, complications, medical therapy and pouchitis. To map the latter two, we asked about medications to control stool frequency, and the history and treatment of pouchitis. During the outpatient visit, biopsy of the pulled through ileum, and stool and blood samples were obtained. The Ethical Committee of the Helsinki University Hospital approved the and the participants (or their guardians) gave informed consent.
Table 1.
Patient characteristics
| Patient characteristics | Median (range) |
| Number of patients (male) | 28 (9) |
| Age (yr); median (range) | |
| At diagnosis | 12 (1-15) |
| At operation | 13 (2-19) |
| At the time of study | 25 (8-41) |
| Duration from surgery to study | 13 (4-22) |
| Clinical inflammation markers; mean (range) | |
| Fecal calprotectin (μg/g) | 371 (12-2859) |
| ESR (mm/h) | 14 (2-69) |
| CRP (mg/L) | 3 (0-19) |
ESR: Erythrocyte sedimentation rate; CRP: C-reactive protein.
Fifteen UC patients had other chronic illnesses: sclerosing cholangitis, active hepatitis, gastroeosophageal reflux, gallstones, rheumatoid arthritis, sacroiliac-joint arthritis, knee arthritis, hyperthyroidism, cardiac arrythmias, psychiatric illness, endometriosis, fibromyalgia, osteoporosis, asthma, atopic skin and contact allergy. Specific medications at the time of the study are shown in Table 2. Post-operatively, 18 (64%) UC patients had received antibiotics as treatment for pouchitis, and of these, 7 (25%) also had received corticosteroids.
Table 2.
Medications at the time of study
| Intestinal inflammation | n |
| 5-ASA | 1 |
| 5-ASA + antibiotics | 1 |
| Antibiotics | 5 |
| Bowel function | |
| To decrease bowel motility | 10 |
| To increase bulk mass | 1 |
| Analgesics | 1 |
| Lactic acid bacteria | 1 |
| Other chronic illnesses | |
| Cholangitis | 1 |
| Mood stabilizing agents | 2 |
| Antibiotics for acne | 1 |
| Gastro-esophageal reflux | 1 |
| Cardiac arrythmias | 1 |
| Infertility | 1 |
| Asthma | 1 |
| Hyperthyroidism | 1 |
5-ASA: 5-Aminosalicylic acid formulations.
Blood inflammatory markers and fecal calprotectin
Inflammation biomarkers in blood [erythrocyte sedimentation rate, erythrocyte sedimentation rate (ESR), and serum concentration of C-reactive protein (CRP)] and fecal calprotectin (quantitative enzyme immunoassay, PhiCal test, Calpro AS, Oslo, Norway) were routinely determined[18]. For immunohistochemistry, biopsies from pouch were used. The histological grade of inflammation in the samples was assessed according to the scoring system for pathological changes in the ileal reservoir mucosa[7,19].
Immunohistochemistry
One biopsy was analyzed for the grade of histological inflammation, the other biopsy was used for MMP immunohistochemistry. Immunohistochemistry was performed using sreptavidin-biotin-peroxidase complex technique (DakoCytomation, StreptABComplex/HRP Duet, Mouse/Rabbit, Glostrup, Denmark; and Elite goat Vectastain ABC kit, Vector laboratories, Burligame, CA, United States) or the antibody-polymer detection technique (ImmPRESS universal reagent, Anti-Mouse/Rabbit IG, Vector laboratories Burligame, CA, United States). Diaminobenzidine or NovaRED (Vector Laboratories) were used as chromogenic substrates and Mayer’s hematoxylin as counterstain. Monoclonal antibodies were used to stain for MMP-7 (1:600, MAB3315, Millipore, Temecula, CA, United States)[15], MMP-8 (1:100, IM38, Calbiochem, La Jolla, CA, United States)[15], MMP-9 (1:100, MS-569-P1, Lab Vision Corporation Neomarkers, Fremont, CA, United States)[15], TIMP-1 (1:50, IM63, Calbiochem)[15], TIMP-2 (1:600, IM56, Calbiochem) and TIMP-3 (1:300, IM43L, Calbiochem)[15]. Polyclonal antibodies were used for MMP-3 (1:50, ab32607, Abcam Ltd, Cambridge, United Kingdom), MMP-12 (1:80, sc-12361, Santa Cruz Biotechnology, CA, United States)[15] and MMP-26 (1:120, a gift from Professor Isaka K, Tokyo Medical University)[15]. MMP-8 and MMP-9 were pretreated with 1% trypsin solution for 30 min at 37 °C. MMP-3, MMP-7, MMP-26, TIMP-1, TIMP-2 and TIMP-3 were pretreated in a 95 °C water bath for 30 min (Dako retrieval solution pH 6; Dakocytomation). MMP-12 required no pre-treatment. The incubation conditions for the antibodies were: 4 °C overnight for MMPs-7, -9, -12 and TIMPs-1, -2, -3; 1 h 45 min at 37 °C for MMP-8 and 1 h at room temperature for MMP-3 and MMP-26. For negative controls, parallel sections of the same samples were processed using preimmune sera or normal rabbit or mouse immunoglobulin. As positive controls, we used formalin fixed, paraffin embedded sections of hailey-hailey, pyoderma gangrenosum and dermatitis herpetiformis (MMP-3), adenocarcinoma (MMP-7), squamous cell cancer (MMP-8), chronic wounds (MMP-9 and TIMP-2 and -3), foreign body reaction (MMP-12), endometrium (MMP-26), and pyoderma gangrenosum (TIMP-1). Immunohistochemical specimens were graded independently by two different investigators (Mäkitalo L, Piekkala M) in a semiquantitative fashion under a light-field microscope at × 100 magnification using a scale marking staining intensity as follows: 0 = less than 20 positive cells; 1 = 20-50 positive cells; 2 = 50-200 positive cells; 3 = over 200 positive cells[15,20]. The identity of the cell types producing each MMP or TIMP was confirmed together with an experienced pathologist (Karikoski R).
Statistical analysis
Non-parametric Mann-Whitney’s test, Spearman’s correlation test and independent samples t test were performed with the SPSS 17.0 for Windows (Chicago, IL) to investigate the significance of results. A P < 0.05 was considered significant.
RESULTS
Of the 28 patients with pediatric onset UC, nine (32.1%) had not experienced pouchitis, whereas 13 (46.4%) reported a single episode, and six (21.4%) had recurrent pouchitis (≥ 4 episodes)[19]. Six patients were on metronidazole medication at the time of the study (Table 2) one of them also on a 5-aminosalicylic acid formulation and showed inflammation of grades 1 to 3[7,20]. In all the others the last episode of pouchitis had occurred more than one month earlier, in most cases several months earlier and they were not on antibiotics. Only four samples (14%) depicted no signs of inflammation, and these were all from patients who had not experienced pouchitis. Of the 19 patients who had experienced pouchitis, 7 showed mild inflammation, 3 depicted moderate and 7 severe inflammation in the biopsy. Two samples were too small to determine the grade of inflammation, but both had suffered pouchitis, the other recurrent. No sample depicted signs of colonic metaplasia.
Expression of MMP-3 was seen in the majority of the samples in the epithelium and in stroma in plasma cells, macrophages and eosinophils (Table 3 and Figure 1A, B). Also, MMP-3 positive endothelium was observed (Figure 1B1, B4). Epithelial MMP-7 was present in all samples, and stromal MMP-7 in 27 samples in plasma cells, macrophages and eosinophils, as well as endothelium (Table 3 and Figure 1C, D). Conversely, stromal MMP-9 was present in 9 samples in macrophages, plasma cells and eosinophils, and in intraepithelial neutrophils, but no positive enterocytes could be found (Table 3 and Figure 2D, E). MMP-12 was found in the majority of the samples in the epithelium and in stroma in macrophages, plasma cells, and eosinophils and intraepithelial neutrophils (Table 3 and Figure 2F, G1). Stromal cells showed positivity for MMP-26 in 3 samples in neutrophils and plasma cells but epithelial cells were negative for this MMP (Table 3 and Figure 2B). MMP-26 positive neutrophils were present in blood vessels (Figure 2B3). TIMP-2 was positive in the majority of samples in the epithelium and in stromal cells including plasma cells, eosinophils and macrophages (Table 3 and Figure 1E, F). TIMP-3 was found in enterocytes in 23 (82%) samples and in all samples in plasma cells and macrophages in stroma (mean 2.39) (Table 3 and Figure 1G). Endothelial cells were also positive for TIMP-3 (Figure 1G1, G2). Expression of MMP-8 and TIMP-1 was generally absent, although a few neutrophils in stroma were positive for MMP-8 and cryptal cells showed positivity for TIMP-1 (Figure 2A, C).
Table 3.
Expression profiles of matrix metalloproteinases and tissue inhibitor of matrix metalloproteinase in ulcerative colitis samples
| Number of positive samples | mean±SEM1 | |
| MMP-3 | ||
| Epithelium | 22 | 0.93 ± 0.114 |
| Stroma | 20 | 1.25 ± 0.183 |
| MMP-7 | ||
| Epithelium | 28 | 1.36 ± 0.092 |
| Stroma | 27 | 1.89 ± 0.149 |
| MMP-8 | ||
| Epithelium | 0 | 0.00 ± 0.000 |
| Stroma | 1 | 0.04 ± 0.036 |
| MMP-9 | ||
| Epithelium | 0 | 0.00 ± 0.000 |
| Stroma | 9 | 0.32 ± 0.090 |
| MMP-12 | ||
| Epithelium | 20 | 0.75 ± 0.098 |
| Stroma | 24 | 1.46 ± 0.141 |
| MMP-26 | ||
| Epithelium | 0 | 0.00 ± 0.000 |
| Stroma | 3 | 0.11 ± 0.060 |
| TIMP-1 | ||
| Epithelium | 0 | 0.00 ± 0.000 |
| Stroma | 0 | 0.00 ± 0.000 |
| TIMP-2 | ||
| Epithelium | 23 | 0.89 ± 0.094 |
| Stroma | 23 | 1.75 ± 0.203 |
| TIMP-3 | ||
| Epithelium | 23 | 1.04 ± 0.120 |
| Stroma | 28 | 2.39 ± 0.130 |
| Histology | ||
| Neutrophils | 0.85 ± 0.154 | |
| Lymphocytes | 1.07 ± 0.185 | |
| Eosinophils | 1.04 ± 0.167 | |
| Villus atrophy | 1.19 ± 0.227 | |
| Grade | 1.95 ± 0.203 |
mean calculated from values: 0 = less than 20 positive cells; 1 = 20-50 positive cells; 2 = 50-200 positive cells; 3 = over 200 positive cells; Grade: Grade of inflammation; MMPs: Matrix metalloproteinases; TIMP: Tissue inhibitor of matrix metalloproteinase.
Figure 1.
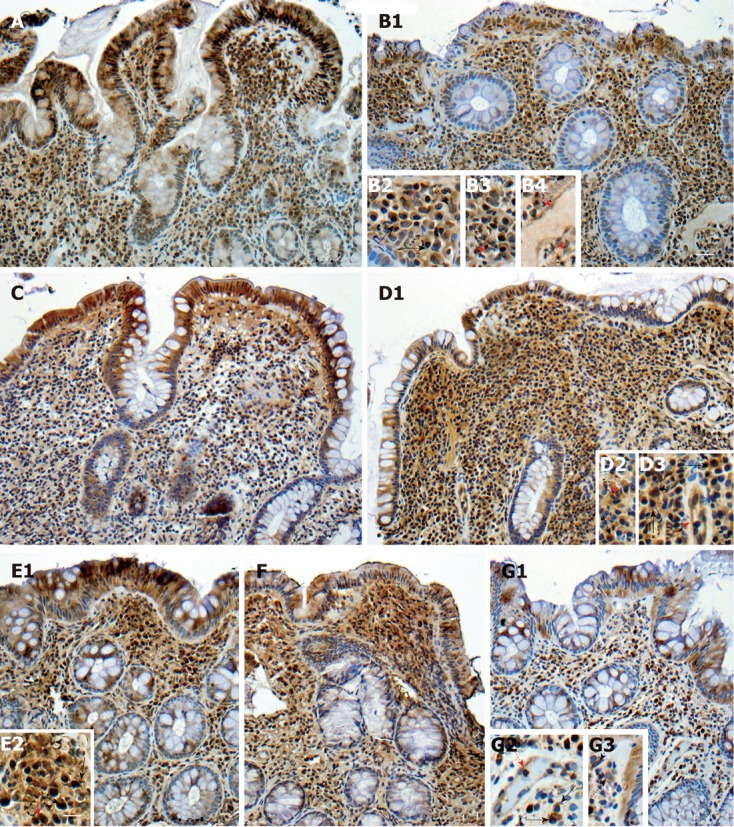
Matrix metalloproteinases-3, matrix metalloproteinases-7 and tissue inhibitor of matrix metalloproteinase-2 in lower (A, C, E1, respectively) and higher grade of inflammation and calprotectin levels (B1, D1, F, respectively), tissue inhibitor of matrix metalloproteinase-3 in pouch (G1). Black solid arrows plasma cells, black dotted arrows macrophages, red solid arrows eosinophils and red dotted arrows endothelium. Scale bars: 15 μm (A, B1, C, D1, E1, F, G1); 7.5 μm (B2-B4, D2, D3, E2, G2, G3). Stainings were performed using diaminobenzidine or NovaRED as chromogenic substrates and Mayer’s hematoxylin as counterstain. Images were obtained using a light-field microscope, and edited using Adobe Photoshop 7.0 (Adobe Systems Incorporated).
Figure 2.
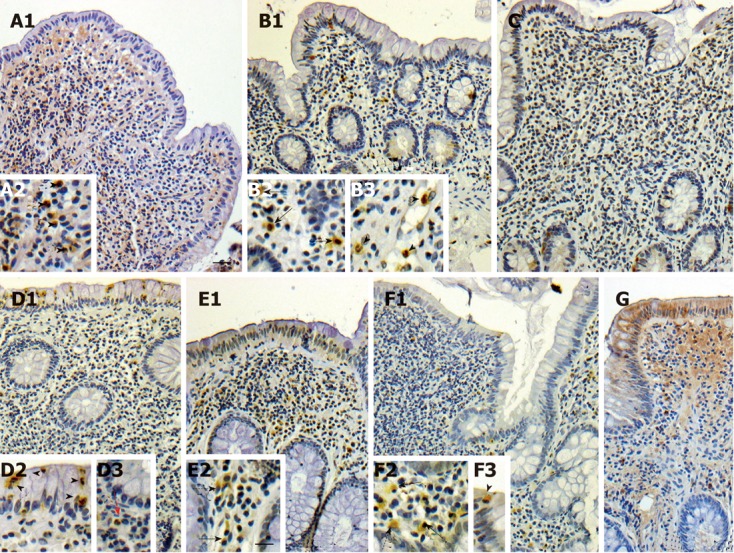
matrix metalloproteinases-8 (A1), matrix metalloproteinases-9 (D1, E1), matrix metalloproteinases-12 (F1, G), matrix metalloproteinases-26 (B1) and tissue inhibitor of matrix metalloproteinase-1 (C) in pouch. Inset g’ added to figure from another sample, not shown in here in lesser magnification. Arrowheads depict neutrophils, black solid arrows plasma cells, black dotted arrows macrophages, red solid arrows eosinophils. Scale bars: 15 μm (A1, B1, C, D1, E1, F1,G); 7.5 μm (A2, B2, B3, D2, D3, E2, F2, F3). Stainings were performed using diaminobenzidine or NovaRED as chromogenic substrates and Mayer’s hematoxylin as counterstain. Images were obtained using a light-field microscope, and edited using Adobe Photoshop 7.0 (Adobe Systems Incorporated).
No differences in MMP- or TIMP-profiles were seen when comparing samples from patients that had experienced pouchitis (single or several episodes) (n = 19) to ones that had not (n = 9). The same was true when performing comparisons related to the frequency of pouchitis (data not shown). When comparing patients with SIAA to those with SIAA with J-pouch, no differences in MMP- and TIMP-expression profiles or the frequency of pouchitis episodes could be found.
MMPs and TIMPs did not generally correlate with inflammation markers fecal calprotectin, ESR and CRP. However, patients considered have no active inflammation (fecal calprotectin < 100 μg/g) showed higher expression of epithelial MMP-7 (Figure 1C) in their pouch biopsies compared to samples from those with active inflammation (fecal calprotectin ≥ 100 μg/g)[21] (Figure 1D1; means 1.75 vs 1.14, P = 0.020, respectively). The grade of inflammation in histological assessment[7] correlated negatively with epithelial MMP-3 (Table 4) (r = -0.614, P = 0.002) (Figure 1A, B1) and MMP-7 (r = -0.472, P = 0.027) (Figure 1C, D1).
Table 4.
Matrix metalloproteinases and tissue inhibitor of matrix metalloproteinase that correlated with inflammation indicators
| Inflammation indicators |
Correlation coefficients values |
||||
|
MMP-3 |
MMP-7 |
MMP-12 |
TIMP-2 |
||
| Epithelium | Epithelium | Epithelium | Stroma | Epithelium | |
| Fecal calprotectin | NS | NS | -0.350 | NS | NS |
| C-reactive protein | NS | NS | NS | -0.422 | NS |
| Grade of inflammation | -0.614 | -0.472 | NS | NS | -0.420 |
NS: Not significant; MMPs: Matrix metalloproteinases; TIMP: Tissue inhibitor of matrix metalloproteinase. Correlations were calculated using Spearman’s correlation test.
DISCUSSION
In pediatric patients, these MMPs and TIMPs have not been studied in pouches, and in adults, reports of only MMPs 1-3 and MMP-9 exist[17,18]. This study reports for the first time expression of MMPs-7, -8, -12, TIMP-2, and TIMP-3 in ileal reservoir mucosa. In long-term, the MMP- and TIMP-profiles in pouch demonstrate similarities with IBD, but profiles in pouch cannot be said to replicate those in UC colon.
In adult inflamed and non-inflamed pouches of UC patients, MMP-3 activity is considered weak[18]. Here, MMP-3 was present in all but few samples in epithelium and stroma. In pediatric IBD, MMP-3 is elevated in endoscopically abnormal colon compared to healthy colon[22]. MMP-3 plays an important role in T-cell- and tumor necrosis factor (TNF)-α-mediated gut injury[23,24], and IBD gut plasma cells produce more MMP-3 than those of healthy controls[25]. Here, expression of epithelial MMP-3 associated with the degree of inflammation, complying with animal studies where lack of MMP-3 associated with impaired wound healing[26]. The present findings suggest that MMP-3 is an important MMP in pouch mucosa, resembling IBD. However, its relationship to the development of pouchitis is unclear. Similar to MMP-3, we found TIMP-3 in a large number of cells in stroma, expression paralleling reports in IBD colon[15,20]. Our group has noted that in intestinal ulcerations in IBD, TIMP-3 is expressed in a greater number of stromal cells compared to normal intestine[14]. TIMP-3 inhibits TNF-α[27], an important cytokine in IBD inflammation[28], and elevated TIMP-3 protein is likely to associate with elevated TNF-α-levels as seen in a human colonic cell line[29]. Also, abundant TIMP-3 expression in stroma in pouch resembles that found in pediatric UC[15], possibly preventing destructive activity as suggested for other autoimmune diseases[30].
Of the other MMPs, expression of MMP-7, MMP-8, and MMP-9 was not IBD-like. Unlike MMP-8 and MMP-9, stromal MMP-7 was present in notable numbers of cells in almost all samples. We recently examined MMP-7 expression in pediatric IBD colon, and found weaker expression in epithelium in UC samples[15]. Here, MMP-7 was found in a smaller number of epithelial cells in samples with higher grade of histological inflammation and fecal calprotectin levels. This contradicts earlier results in UC[12,31]. However, MMP-7 contributes to intestinal wound closure but over-expression may delay epithelial wound healing[32]. Epithelial expression in pouch thus may be due to a regenerative process. MMP-7 has also been suggested to aid the growth of myofibroblasts and their function[33] and stromal MMP-7 may take part in maintaining mucosal homeostasis. In normal colon, MMP-8 is undetectable[10] but it may be involved in ulcer formation[34] as elevated levels are found in ulcer bases of both UC and CD[10]. We are not aware of previous studies of MMP-8 in pouch mucosa, but in our study, MMP-8 was generally absent from pouches. MMP-9 is important in IBD-related inflammation, and has also been shown to correlate with disease activity[10]. We found expression of MMP-9 in only a few samples, not suggestive of IBD-like inflammation.
In our study, MMP-12 was found in almost all pouch samples, although it is not expressed in normal adult ileum[14,35]. While it’s role in IBD is unknown, this MMP may take part in macrophage migration and can activate TNF-α[10,36]. MMP-12 has been proposed to be a final step in tissue injury in celiac disease[37] and might have a pathological role in pouch mucosa. Its expression suggests that pouch mucosa is dissimilar to normal ileal mucosa, even in the absence of inflammation.
In the present study, expression of MMP-26 was rare. We have proposed that immunosuppressive drugs modulate disease activity in CD by downregulating MMP-26[20]. It is found in the colon of pediatric IBD patients[15], but also in healthy ileum[38], and expression is not IBD-specific. TIMP-1 is present in greater amount in inflamed adult IBD than in healthy mucosa[31], whereas in pediatric IBD, we have reported weak TIMP-1 expression[15]. We found no expression of TIMP-1 in the pouch, but epithelial and stromal TIMP-2 was found in most samples. Structural features of TIMP-2 suggest that it is expressed in constant amount[39], and it has been reported to be present in normal-appearing IBD mucosa, with no significant increase in inflamed mucosa[40]. Expression of MMP-26, TIMP-1 and TIMP-2 were inconclusive, neither supporting of contradicting IBD-etiology.
Taken together, earlier studies on MMPs and TIMPs in pouch are scarce, but in adults elevated MMP-1 and MMP-2 have been found in pouchitis mucosa[17]. Due to small sizes of the biopsy and limited stainable slides, these MMPs were not studied here. The presence of MMP-3 and TIMP-3 in our samples is comparable to findings in IBD. In line with this, MMP-12 is detected in active IBD but not in normal ileum[14,35,41], and here, expression of MMP-12 in pouch suggests altered mucosa. The lack of proper MMP-8 and MMP-9 expression in the pouch, however, contradicts IBD-related inflammation, as does the expression profile of MMP-7.
The results here are based on immunohistochemistry only, a limitation of this study, and further research using other techniques, e.g., Western blotting and polymerase chain reaction, would be necessary to verify the findings. We could not include a side-by-side analysis of samples from active UC and normal ileum and colon. Parallel analysis of ileal and colonic samples is challenging, as the follow up lasted until early adulthood. It is possible, that the use of medication in some cases may affect the expression of MMPs and TIMPs. It has been put forth, that probiotic use - that seems to elevate interleukin-10 in the gut-might downregulate the expression of MMP activity in the pouch mucosa and alter the expression of other proinflammatory cytokines[18], but this finding needs more systematic studies. However, due to small sample size, we focused on comparing the expression patterns with established markers depicting the activity of inflammation. Interestingly, we found no differences in MMP or TIMP expression depending on the frequency of pouchitis, but most samples depicted inflammation with concurrent elevated calprotectin. It seems reasonable that since there was no variation in MMP- or TIMP-profile according to the frequency of pouchitis, that inflammation markers depict very little correlation with MMPs. While even a longer follow-up may be necessary to further investigate the nature of pouch mucosa, the strength of the study is the long follow-up of the patients with pediatric onset disease, up to two decades after surgery.
In conclusion, in long-term, MMP expression in pouch shares characteristics with UC, but inflammation cannot be classified as a reactivation per se. Expression of MMP-3 and TIMP-3 in pouch resembles that of IBD, but the lack of MMP-9 contradicts an IBD-like pathomechanism. To the best of our knowledge, this study is the first to show that MMPs-7, -12, and TIMP-2 are also important in pouch mucosa. Further studies on the role of MMP profiles in etiopathology and the development of pouchitis in pediatric onset UC are warranted.
ACKNOWLEDGMENTS
The authors thank Professor Isaka K, University of Tokio, for MMP-26 antibodies, Ms. Tallqvist A for skilful technical assistance and Ms. Nikkonen A for excellent help in collecting the patient data.
COMMENTS
Background
Approximately 24% of pediatric ulcerative colitis (UC) patients undergo colectomy with ileal pouch anal anastomosis within the first decade after diagnosis. Pouchitis is the most common complication occurring in approximately two thirds of the patients at least once during the following decade. The etiology of pouchitis is unknown and it is debated whether the inflammation is a novel kind or similar to that of found in UC. Matrix metalloproteinases (MMPs) have been linked to both physiological and pathological event in inflammatory bowel disease (IBD) mucosa.
Research frontiers
In pediatric IBD MMP 10 and tissue inhibitor of matrix metalloproteinase (TIMP) 3 have been linked to the colonic inflammation. Most abundantly expressed MMP in IBD-like inflammation is MMP-9 and the MMP-7 is linked to the severity of inflammation. There are no reports of MMP expression in pediatric pouch. Thus, the authors studied the expression of MMPs-3, -7, -8, -9 and -12 and TIMPs-1, -2, and -3 from the biopsies of pediatric UC patients’ pouches to find MMPs and TIMPs specific to the pediatric pouchitis.
Innovations and breakthroughs
The expression of MMPs and TIMPs in pediatric pouches has not been studied previously and adult reports of only MMPs-1, -3 and -9 exist. This study, for first time, reports the epithelial and stromal expression of MMP-3, -7 -12, TIMP-2, and -3 and the lack of MMPs-8, -9, -26, and TIMP-1 expression in pediatric ileal reservoirs. The presence of MMPs-3, -12 and TIMP-3 share some similarities with IBD, but the lack of MMP-9 contradicts the IBD-like inflammation.
Applications
By understanding the MMP- and TIMP-profile of pouch mucosa, this study takes part in characterizing molecular environment in pouch, which may in turn aid in finding specific biomolecular targets for treatment of pouchitis.
Terminology
UC is chronic disease of the mucosa of the colon and the rectum characterized by bloody diarrhea, abdominal pain, and weight loss. Pouchitis is the inflammation of the ileal reservoir that is made after colectomy to avoid permanent ostomy. MMPs are a family of 24 zinc-dependent enzymes that are capable to degrade nearly all extracellular matrix and basement membrane proteins and take part to both normal and pathological tissue remodeling. TIMPs inhibit the action of MMPs but the actions of TIMPs are not restricted to the MMP-inhibition, they also modulate other cellular processes.
Peer review
This is a study on matrix metalloproteinases and their tissue inhibitors in pouch mucosa of pediatric onset UC. This is a good study and the topic is so important because pouchitis is often seen in those who have undergone ileal pouch-anal anastomosis.
Footnotes
Supported by The Academy of Finland, Finska Läkaresällskapet, Helsinki University Central Hospital Research Fund, Finnish Cultural Foundation (to Mäkitalo L); Biomedicum Helsinki Foundation (to Mäkitalo L), Finland; the Swedish Research Council, Sweden (to Saarialho-Kere U); the Päivikki and Sakari Sohlberg Foundation (to Kolho KL); and the Finnish Pediatric Research Foundation (to Kolho KL)
Peer reviewers: Mohammad Abdollahi, Professor, Faculty of Pharmacy and Pharmaceutical Sciences Research Center, Tehran University of Medical Sciences, Tehran 14176-14411, Iran; Ioannis Kanellos, Professor, 4th Surgical Department, Aristotle University of Thessaloniki, Antheon 1, Panorama, 55236 Thessaloniki, Greece
S- Editor Lv S L- Editor A E- Editor Xiong L
References
- 1.Turunen P, Ashorn M, Auvinen A, Iltanen S, Huhtala H, Kolho KL. Long-term health outcomes in pediatric inflammatory bowel disease: a population-based study. Inflamm Bowel Dis. 2009;15:56–62. doi: 10.1002/ibd.20558. [DOI] [PubMed] [Google Scholar]
- 2.Pakarinen MP, Natunen J, Ashorn M, Koivusalo A, Turunen P, Rintala RJ, Kolho KL. Long-term outcomes of restorative proctocolectomy in children with ulcerative colitis. Pediatrics. 2009;123:1377–1382. doi: 10.1542/peds.2008-2086. [DOI] [PubMed] [Google Scholar]
- 3.Seetharamaiah R, West BT, Ignash SJ, Pakarinen MP, Koivusalo A, Rintala RJ, Liu DC, Spencer AU, Skipton K, Geiger JD, et al. Outcomes in pediatric patients undergoing straight vs J pouch ileoanal anastomosis: a multicenter analysis. J Pediatr Surg. 2009;44:1410–1417. doi: 10.1016/j.jpedsurg.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Coffey JC, McCarthy E, Kavanagh E, Redmond HP, Kirwan WO. Pouchitis: an evolving clinical enigma--a review. Dis Colon Rectum. 2009;52:140–153. doi: 10.1007/DCR.0b013e31819739d6. [DOI] [PubMed] [Google Scholar]
- 5.Lohmuller JL, Pemberton JH, Dozois RR, Ilstrup D, van Heerden J. Pouchitis and extraintestinal manifestations of inflammatory bowel disease after ileal pouch-anal anastomosis. Ann Surg. 1990;211:622–627; discussion 622-627. [PMC free article] [PubMed] [Google Scholar]
- 6.Coffey JC, Winter DC, Neary P, Murphy A, Redmond HP, Kirwan WO. Quality of life after ileal pouch-anal anastomosis: an evaluation of diet and other factors using the Cleveland Global Quality of Life instrument. Dis Colon Rectum. 2002;45:30–38. [PubMed] [Google Scholar]
- 7.Shepherd NA, Jass JR, Duval I, Moskowitz RL, Nicholls RJ, Morson BC. Restorative proctocolectomy with ileal reservoir: pathological and histochemical study of mucosal biopsy specimens. J Clin Pathol. 1987;40:601–607. doi: 10.1136/jcp.40.6.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Silva HJ, Millard PR, Kettlewell M, Mortensen NJ, Prince C, Jewell DP. Mucosal characteristics of pelvic ileal pouches. Gut. 1991;32:61–65. doi: 10.1136/gut.32.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luukkonen P, Järvinen H, Tanskanen M, Kahri A. Pouchitis--recurrence of the inflammatory bowel disease? Gut. 1994;35:243–246. doi: 10.1136/gut.35.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ravi A, Garg P, Sitaraman SV. Matrix metalloproteinases in inflammatory bowel disease: boon or a bane? Inflamm Bowel Dis. 2007;13:97–107. doi: 10.1002/ibd.20011. [DOI] [PubMed] [Google Scholar]
- 11.Baugh MD, Perry MJ, Hollander AP, Davies DR, Cross SS, Lobo AJ, Taylor CJ, Evans GS. Matrix metalloproteinase levels are elevated in inflammatory bowel disease. Gastroenterology. 1999;117:814–822. doi: 10.1016/s0016-5085(99)70339-2. [DOI] [PubMed] [Google Scholar]
- 12.Matsuno K, Adachi Y, Yamamoto H, Goto A, Arimura Y, Endo T, Itoh F, Imai K. The expression of matrix metalloproteinase matrilysin indicates the degree of inflammation in ulcerative colitis. J Gastroenterol. 2003;38:348–354. doi: 10.1007/s005350300062. [DOI] [PubMed] [Google Scholar]
- 13.Saarialho-Kere UK, Vaalamo M, Puolakkainen P, Airola K, Parks WC, Karjalainen-Lindsberg ML. Enhanced expression of matrilysin, collagenase, and stromelysin-1 in gastrointestinal ulcers. Am J Pathol. 1996;148:519–526. [PMC free article] [PubMed] [Google Scholar]
- 14.Vaalamo M, Karjalainen-Lindsberg ML, Puolakkainen P, Kere J, Saarialho-Kere U. Distinct expression profiles of stromelysin-2 (MMP-10), collagenase-3 (MMP-13), macrophage metalloelastase (MMP-12), and tissue inhibitor of metalloproteinases-3 (TIMP-3) in intestinal ulcerations. Am J Pathol. 1998;152:1005–1014. [PMC free article] [PubMed] [Google Scholar]
- 15.Mäkitalo L, Kolho KL, Karikoski R, Anthoni H, Saarialho-Kere U. Expression profiles of matrix metalloproteinases and their inhibitors in colonic inflammation related to pediatric inflammatory bowel disease. Scand J Gastroenterol. 2010;45:862–871. doi: 10.3109/00365520903583863. [DOI] [PubMed] [Google Scholar]
- 16.Nikfar S, Darvish-Damavandi M, Abdollahi M. A review and meta-analysis of the efficacy of antibiotics and probiotics in management of pouchitis. Int J Pharmacol. 2010;6:826–835. [Google Scholar]
- 17.Stallmach A, Chan CC, Ecker KW, Feifel G, Herbst H, Schuppan D, Zeitz M. Comparable expression of matrix metalloproteinases 1 and 2 in pouchitis and ulcerative colitis. Gut. 2000;47:415–422. doi: 10.1136/gut.47.3.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ulisse S, Gionchetti P, D'Alò S, Russo FP, Pesce I, Ricci G, Rizzello F, Helwig U, Cifone MG, Campieri M, et al. Expression of cytokines, inducible nitric oxide synthase, and matrix metalloproteinases in pouchitis: effects of probiotic treatment. Am J Gastroenterol. 2001;96:2691–2699. doi: 10.1111/j.1572-0241.2001.04139.x. [DOI] [PubMed] [Google Scholar]
- 19.Pakarinen MP, Koivusalo A, Natunen J, Ashorn M, Karikoski R, Aitola P, Rintala RJ, Kolho KL. Fecal calprotectin mirrors inflammation of the distal ileum and bowel function after restorative proctocolectomy for pediatric-onset ulcerative colitis. Inflamm Bowel Dis. 2010;16:482–486. doi: 10.1002/ibd.21069. [DOI] [PubMed] [Google Scholar]
- 20.Mäkitalo L, Sipponen T, Kärkkäinen P, Kolho KL, Saarialho-Kere U. Changes in matrix metalloproteinase (MMP) and tissue inhibitors of metalloproteinases (TIMP) expression profile in Crohn's disease after immunosuppressive treatment correlate with histological score and calprotectin values. Int J Colorectal Dis. 2009;24:1157–1167. doi: 10.1007/s00384-009-0756-5. [DOI] [PubMed] [Google Scholar]
- 21.Kolho KL, Raivio T, Lindahl H, Savilahti E. Fecal calprotectin remains high during glucocorticoid therapy in children with inflammatory bowel disease. Scand J Gastroenterol. 2006;41:720–725. doi: 10.1080/00365520500419623. [DOI] [PubMed] [Google Scholar]
- 22.Heuschkel RB, MacDonald TT, Monteleone G, Bajaj-Elliott M, Smith JA, Pender SL. Imbalance of stromelysin-1 and TIMP-1 in the mucosal lesions of children with inflammatory bowel disease. Gut. 2000;47:57–62. doi: 10.1136/gut.47.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pender SL, Tickle SP, Docherty AJ, Howie D, Wathen NC, MacDonald TT. A major role for matrix metalloproteinases in T cell injury in the gut. J Immunol. 1997;158:1582–1590. [PubMed] [Google Scholar]
- 24.Pender SL, Fell JM, Chamow SM, Ashkenazi A, MacDonald TT. A p55 TNF receptor immunoadhesin prevents T cell-mediated intestinal injury by inhibiting matrix metalloproteinase production. J Immunol. 1998;160:4098–4103. [PubMed] [Google Scholar]
- 25.Gordon JN, Pickard KM, Di Sabatino A, Prothero JD, Pender SL, Goggin PM, MacDonald TT. Matrix metalloproteinase-3 production by gut IgG plasma cells in chronic inflammatory bowel disease. Inflamm Bowel Dis. 2008;14:195–203. doi: 10.1002/ibd.20302. [DOI] [PubMed] [Google Scholar]
- 26.Bullard KM, Lund L, Mudgett JS, Mellin TN, Hunt TK, Murphy B, Ronan J, Werb Z, Banda MJ. Impaired wound contraction in stromelysin-1-deficient mice. Ann Surg. 1999;230:260–265. doi: 10.1097/00000658-199908000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amour A, Slocombe PM, Webster A, Butler M, Knight CG, Smith BJ, Stephens PE, Shelley C, Hutton M, Knäuper V, et al. TNF-alpha converting enzyme (TACE) is inhibited by TIMP-3. FEBS Lett. 1998;435:39–44. doi: 10.1016/s0014-5793(98)01031-x. [DOI] [PubMed] [Google Scholar]
- 28.Fréour T, Jarry A, Bach-Ngohou K, Dejoie T, Bou-Hanna C, Denis MG, Mosnier JF, Laboisse CL, Masson D. TACE inhibition amplifies TNF-alpha-mediated colonic epithelial barrier disruption. Int J Mol Med. 2009;23:41–48. [PubMed] [Google Scholar]
- 29.Cesaro A, Abakar-Mahamat A, Brest P, Lassalle S, Selva E, Filippi J, Hébuterne X, Hugot JP, Doglio A, Galland F, et al. Differential expression and regulation of ADAM17 and TIMP3 in acute inflamed intestinal epithelia. Am J Physiol Gastrointest Liver Physiol. 2009;296:G1332–G1343. doi: 10.1152/ajpgi.90641.2008. [DOI] [PubMed] [Google Scholar]
- 30.Mohammed FF, Smookler DS, Khokha R. Metalloproteinases, inflammation, and rheumatoid arthritis. Ann Rheum Dis. 2003;62 Suppl 2:ii43–ii47. doi: 10.1136/ard.62.suppl_2.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rath T, Roderfeld M, Graf J, Wagner S, Vehr AK, Dietrich C, Geier A, Roeb E. Enhanced expression of MMP-7 and MMP-13 in inflammatory bowel disease: a precancerous potential? Inflamm Bowel Dis. 2006;12:1025–1035. doi: 10.1097/01.mib.0000234133.97594.04. [DOI] [PubMed] [Google Scholar]
- 32.Hayden DM, Forsyth C, Keshavarzian A. The role of matrix metalloproteinases in intestinal epithelial wound healing during normal and inflammatory states. J Surg Res. 2011;168:315–324. doi: 10.1016/j.jss.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 33.Bamba S, Lee CY, Brittan M, Preston SL, Direkze NC, Poulsom R, Alison MR, Wright NA, Otto WR. Bone marrow transplantation ameliorates pathology in interleukin-10 knockout colitic mice. J Pathol. 2006;209:265–273. doi: 10.1002/path.1967. [DOI] [PubMed] [Google Scholar]
- 34.Pirilä E, Ramamurthy NS, Sorsa T, Salo T, Hietanen J, Maisi P. Gelatinase A (MMP-2), collagenase-2 (MMP-8), and laminin-5 gamma2-chain expression in murine inflammatory bowel disease (ulcerative colitis) Dig Dis Sci. 2003;48:93–98. doi: 10.1023/a:1021790532723. [DOI] [PubMed] [Google Scholar]
- 35.Salmela MT, Pender SL, Reunala T, MacDonald T, Saarialho-Kere U. Parallel expression of macrophage metalloelastase (MMP-12) in duodenal and skin lesions of patients with dermatitis herpetiformis. Gut. 2001;48:496–502. doi: 10.1136/gut.48.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chandler S, Cossins J, Lury J, Wells G. Macrophage metalloelastase degrades matrix and myelin proteins and processes a tumour necrosis factor-alpha fusion protein. Biochem Biophys Res Commun. 1996;228:421–429. doi: 10.1006/bbrc.1996.1677. [DOI] [PubMed] [Google Scholar]
- 37.Ciccocioppo R, Di Sabatino A, Bauer M, Della Riccia DN, Bizzini F, Biagi F, Cifone MG, Corazza GR, Schuppan D. Matrix metalloproteinase pattern in celiac duodenal mucosa. Lab Invest. 2005;85:397–407. doi: 10.1038/labinvest.3700225. [DOI] [PubMed] [Google Scholar]
- 38.Bister VO, Salmela MT, Karjalainen-Lindsberg ML, Uria J, Lohi J, Puolakkainen P, Lopez-Otin C, Saarialho-Kere U. Differential expression of three matrix metalloproteinases, MMP-19, MMP-26, and MMP-28, in normal and inflamed intestine and colon cancer. Dig Dis Sci. 2004;49:653–661. doi: 10.1023/b:ddas.0000026314.12474.17. [DOI] [PubMed] [Google Scholar]
- 39.Hammani K, Blakis A, Morsette D, Bowcock AM, Schmutte C, Henriet P, DeClerck YA. Structure and characterization of the human tissue inhibitor of metalloproteinases-2 gene. J Biol Chem. 1996;271:25498–25505. doi: 10.1074/jbc.271.41.25498. [DOI] [PubMed] [Google Scholar]
- 40.von Lampe B, Barthel B, Coupland SE, Riecken EO, Rosewicz S. Differential expression of matrix metalloproteinases and their tissue inhibitors in colon mucosa of patients with inflammatory bowel disease. Gut. 2000;47:63–73. doi: 10.1136/gut.47.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pender SL, Li CK, Di Sabatino A, MacDonald TT, Buckley MG. Role of macrophage metalloelastase in gut inflammation. Ann N Y Acad Sci. 2006;1072:386–388. doi: 10.1196/annals.1326.019. [DOI] [PubMed] [Google Scholar]


