Abstract
Fibrous dysplasia (FD) is a sporadic benign skeletal disorder that can affect one bone (monostotic form) or multiple bones (polyostotic bone). Around 6–20% of monostotic FD occurs in the ribs. The objective of this study was to report our experience in the management of the monostotic FD of the ribs. Between January 2004 and December 2009, seven cases of FD of the rib (six men and one woman, mean age 30.4 years, range 17–40 years) were operated on. The patients were evaluated with plain radiographs and computer tomography (CT). All our patients were symptomatic; two patients presented chest pain and swelling and other patients presented only chest pain. One rib was involved in all our patients (monostotic form): the site was fifth rib (four cases), sixth rib (two cases) or second rib (one case). Radiologically, plain films and CT showed an expansible lesion with a ground-glass centre and thinning of the cortex. Rib resection was performed in all patients; there were no postoperative complications and no recurrence in all cases at mean 43 month follow-up. In symptomatic monostotic FD of ribs, the involved segment of bone may be excised to rule out malignancy and for painful lesions.
Keywords: Fibrous dysplasia, Ribs, Surgical resection
INTRODUCTION
First named by Lichtenstein in 1938 [1], fibrous dysplasia (FD) is a non-inherited, skeletal developmental abnormality, where normal bone is replaced by fibrous tissue and poorly formed area of immature bone. It can be monostotic, involving a single bone, or polyostotic, involving two or more bones. Any bone may be affected, the long bone, skull and ribs most often. Albright's syndrome describes a polyostotic disease associated with pigmented skin lesions, endocrine abnormalities and precocious puberty [1, 2, 4]. FD of ribs accounts for up to 30% of all benign chest wall tumours, and monostotic forms are about four times more common than polyostotic forms. It is typically present in the third or fourth decade of life as an asymptomatic mass [3, 5]. We report on seven cases of monostotic FD of the ribs operated in our service in the last 6 years. In this report, clinical, diagnosis problems and treatment are discussed.
METHODS
This is a retrospective study of seven cases of monostotic FD of the ribs, operated at our department between January 2004 and December 2009. All our patients had a complete clinical examination and were evaluated by plain X-ray and CT. The records of these cases were analysed for age, sex, signs and symptoms at presentation, radiological finding, surgical procedure and follow-up period (Table 1). In our series, diagnosis of FD was confirmed postoperatively by histological examination of surgical specimen.
Table 1:
Patients’ characteristics
| Age sex | Symptoms | Radiological findings |
Surgical resection | Follow-up (months) | |
|---|---|---|---|---|---|
| Chest X-ray | Computed tomography | ||||
| 37 M | Chest pain, swelling | Ground-glass appearance | Expansion and deformity of the posterior aspect of fifth left rib with cortical thinning. Size: 6.5 cm; 1.5 cm | Resection of the left fifth rib | 49 |
| 23 M | Chest pain | Ground-glass appearance | Expansile lesion with cortical thinning of the post aspect of the right fifth rib. Size: 6 cm; 4 cm | Resection and posterior disarticulation of the right fifth rib | 36 |
| 32 M | Chest pain | Ground-glass appearance | Well circumscribed Expansile lesion of the lateral aspect of the right sixth rib. Size: 4 cm; 2.5 cm | Resection of the right sixth rib | 34 |
| 29 M | Chest pain, swelling | Ground-glass appearance | Expansile lesion of the lateral aspect of the left fifth rib with cortical thinning. Size: 6 cm; 4.5 cm | Resection of the left fifth rib | 60 |
| 35 F | Chest pain | Ground-glass appearance | Expansion and deformity of the anterior aspect of second left rib with cortical thinning. Size: 6.5 cm; 4 cm | Resection of the left second rib | 6 |
| 40 M | Chest pain | Ground-glass appearance | Expansile lesion with cortical thinning of the posterior aspect of the left fifth rib. Size: 5 cm; 3.5 cm | Resection of the left fifth rib | 72 |
| 17 M | Chest pain | Ground-glass appearance | Expansile lesion of the posterior aspect of the right Sixth rib with cortical thinning. Size: 6 cm; 4 cm | Resection of the right sixth rib | 46 |
RESULTS
There were six men and one woman, median age was 30.4 years, range 17–40 years. All our patients were symptomatic, two patients presented chest pain and swelling and other patients presented only chest pain. A biological examination (serum levels of calcium, phosphate, alkaline phosphatase) was normal in all our patients. Postero-anterior chest X-ray revealed a unilateral fusiform image with ground-glass appearance in one rib in all patients, CT showed an expansible lesion with cortical thinning and peripheral trabeculations in most cases (Figs 1 and 2). A mean size of lesions was 5.7/3.4 cm. The site of lesions was the fifth rib (four cases), sixth rib (two cases) and the second rib (one case). Posterior aspect of ribs was involved in four cases, lateral aspect in two cases and anterior aspect in one case. The lesions were in the right side in three patients and in the left side in four patients. Surgery was indicated in all our patients for both diagnosis and curative intention. The involved rib was resected with 1 cm clear margins, and posterior rib disarticulation was necessary in only one patient. In all cases, the diagnosis was FD and confirmed postoperatively with histological studies (Fig. 3). The mean hospital stay was 4 days, with no complications in any patient. In this series, the follow-up ranged from 6 to 72 months (mean 43 months). All our patients were asymptomatic, and there was no recurrence of disease.
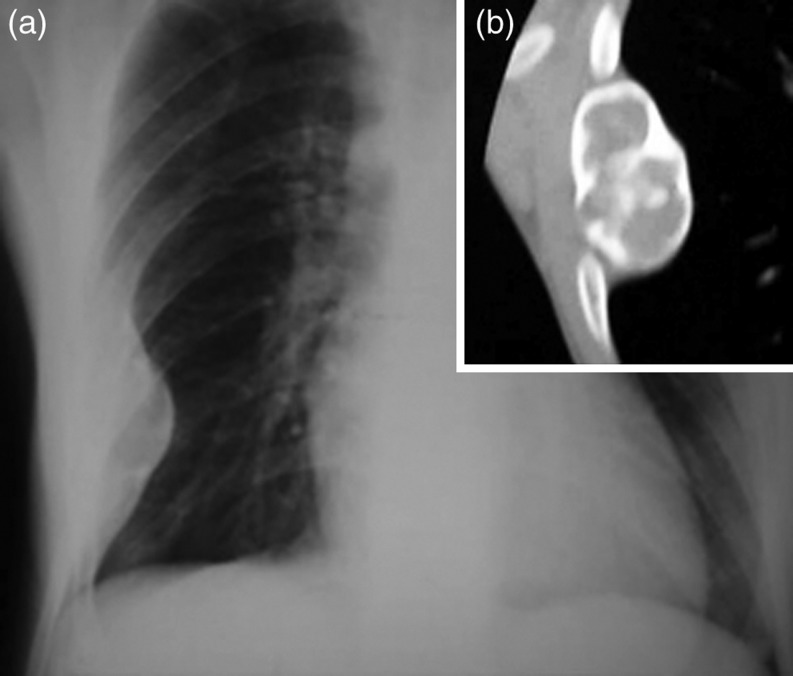
Figure 1:
Patient 3. (a) Chest radiograph showing fusiform expansion and deformity, with ground glass appearance, of the lateral aspect of the right sixth rib. (b) Computer tomography (CT) image showing well-circumscribed expansible lesion of the lateral aspect of the right sixth rib.
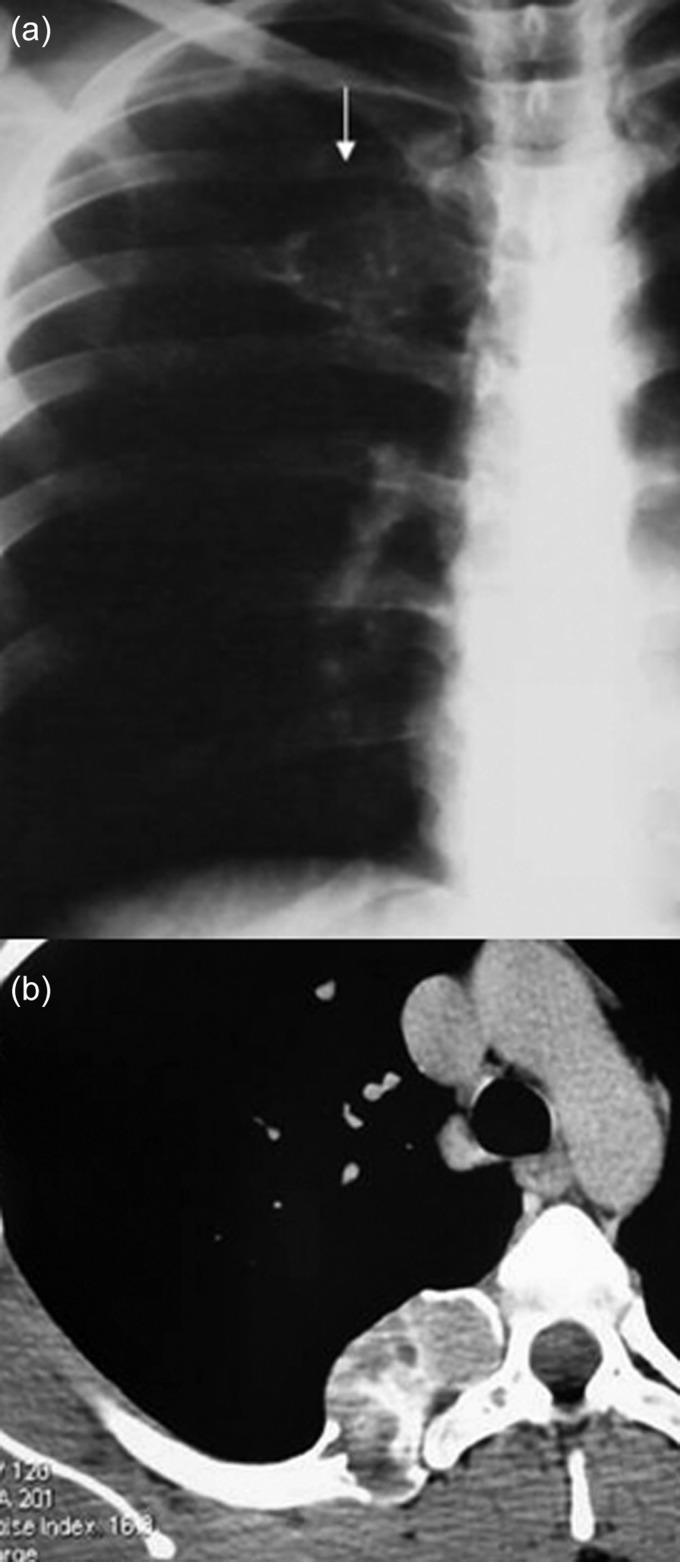
Figure 2:
Patient 2. (a) Chest radiograph showing well-circumscribed lesion, with ground glass appearance, of the post aspect of the right fifth rib. (b) CT image showing an expansible lesion with cortical thinning of the post aspect of the right fifth rib.
Figure 3:
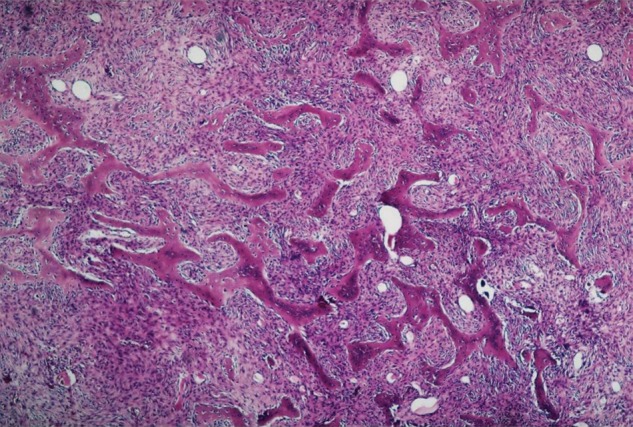
Histological aspect of an FD lesion showing an irregularly mineralized trabecular detaching from a background of fibroblasts (HE, GX200).
DISCUSSION
FD is a benign bone disease characterized by the progressive replacement of normal bone elements by fibrous tissue and immature woven bone. Around 6–20% of monostotic FD occurs in the ribs in the third or fourth decade of life, and both sexes are equally affected [1–3]. It has now become evident that FD is a genetic disease caused by somatic activating mutation of the Gsα subunit of G protein-coupled receptor, resulting in upregulation of cyclic adenosine monophosphate (cAMP) [12]. It presents later in the ribs, probably because it is often asymptomatic in this site [6]. In our series, all patients were symptomatic. Biological examinations were normal in our patients, but alkaline phosphatase may be elevated in 25% of patients with monostotic disease [9]. In the plain radiographs and CT, the lesions are classically described by their ground-glass appearance characterized by a variable degree of mineralization with a faint homogeneous increase in density. Although non-specific, bone scintigraphy is sensitive in the identification of the extent of skeletal FD, particularly in polyostotic form [7, 8, 10]. The differential diagnosis might include ossifying-fibroma, osteoma, bone cyst, giant cell tumour or a malignancy of osseous origin [2, 8, 9]. The role for PET scan in differential diagnosis is minor, because hyperfixation in benign pathology, such as FD, is often a source of a false-positive scan. Malignant degeneration has been reported to occur in monostotic FD in 0.5% of patients [14]. When the diagnosis is suspected in CT and/or magnetic resonance imaging (MRI), histological confirmation by bone biopsy or surgical resection is necessary. The most common histology is osteosarcoma, followed by fibrosarcoma and chondrosarcoma [9, 14].
Histologically, FD consists of an overgrowth of fibrous tissue with disorganized bony trabeculae and spindle cells surrounded by fibrous matrix [2, 5]. Different histological patterns have been described [15]. The severity of the outcome is proportional to the extent of the bone disease and association with other pathology MacCune-Albright syndrome (MAS). In patients with monostotic disease, the long-term prognosis is excellent. Treatment of FD is not codified and, generally, asymptomatic and stable lesions should simply be monitored. Surgery is indicated for confirmatory biopsy, correction of deformity, prevention of pathologic and/or eradication of symptomatic lesions [10, 11]. When surgery is not possible, and in the polyostotic form, bisphosphonate therapy is indicated with positive effects exerted on bony density and the reduction of pain [13]. Some authors [2, 10] prefer a surgical management than simple surveillance, especially in ribs location of FD, because it can raise the difficult problem of differential diagnosis with malignant tumours.
We believe that in ribs location of symptomatic monostotic FD, excised involved bone must be indicated for both curative and diagnosis intention, to rule out malignancy and provide relief from symptoms.
Conflict of interest: none declared.
REFERENCES
- 1.Albright F, Butler AM, Hampton AO, Smith PH. Syndrome characterized by ostitis fibrosa disseminata, areas of pigmentation and endocrine dysfunction, with precocious puberty in females: report of five cases. N Engl J Med. 1937;216:727–46. [Google Scholar]
- 2.Ayadi-Kaddour A, Ben Slama S, Marghli A, Mehouachi R, Djilani H, Kilani T, et al. Fibrous dysplasia of the rib. Ten case reports. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:301–7. doi: 10.1016/j.rco.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Hughes EK, James SL, Butt S, Davies AM, Saifuddin A. Benign primary tumours of the ribs. Clin Radiol. 2006;61:314–22. doi: 10.1016/j.crad.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Chapurlat RD, Meunier PJ. Fibrous dysplasia of bone. Baillieres Best Pract Res Clin Rheumatol. 2000;14:385–98. doi: 10.1053/berh.1999.0071. [DOI] [PubMed] [Google Scholar]
- 5.DiCaprio MR, Enneking WF. Fibrous dysplasia. Pathophysiology, evaluation, and treatment. J Bone Joint Surg Am. 2005;87:1848–64. doi: 10.2106/JBJS.D.02942. [DOI] [PubMed] [Google Scholar]
- 6.Henry A. Monostotic fibrous dysplasia. J Bone Joint Surg Br. 1969;51:300–6. [PubMed] [Google Scholar]
- 7.Kransdorf MJ, Moser RP, Jr, Gilkey FW. Fibrous dysplasia. Radiographics. 1990;10:519–37. doi: 10.1148/radiographics.10.3.2188311. [DOI] [PubMed] [Google Scholar]
- 8.Parekh SG, Donthineni-Rao R, Ricchetti E, Lackman RD. Fibrous dysplasia. J Am Acad Orthop Surg. 2004;12:305–13. doi: 10.5435/00124635-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Orten SS, Hanna E. Fibrous dysplasia: Biology and indications for surgery. Operat Techniq Otolaryngol Head Neck Surg. 1999;10:109–12. [Google Scholar]
- 10.Shields TW, LoCicero J, Ponn RB, Rusch VW. General Thoracic Surgery. Philadelphia: Lippincott Williams and Wilkins; 2005. [Google Scholar]
- 11.Demiralp B, Ozturk C, Ozturan K, Sanisoglu YS, Cicek IE, Erler K. Prophylactic intramedullary nailing in monostotic fibrous dysplasia. Acta Orthop Belg. 2008;74:386–90. [PubMed] [Google Scholar]
- 12.Feller L, Wood NH, Khammissa RA, Lemmer J, Raubenheimer EJ. The nature of fibrous dysplasia. Head Face Med. 2009;5:22. doi: 10.1186/1746-160X-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chapurlat R. Medical therapy in adults with fibrous dysplasia of bone. J Bone Miner Res. 2007;21:114–7. doi: 10.1359/jbmr.06s222. [DOI] [PubMed] [Google Scholar]
- 14.Ruggieri P, Sim FH, Bond JR, Unni KK. Malignancies in fibrous dysplasia. Cancer. 1994;73:1411–24. doi: 10.1002/1097-0142(19940301)73:5<1411::aid-cncr2820730516>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 15.Riminucci M, Liu B, Corsi A, Shenker A, Spiegel AM, Robey PG, et al. The histopathology of fibrous dysplasia of bone in patients with activating mutations of the Gs alpha gene: site-specific patterns and recurrent histological hallmarks. J Pathol. 1999;187:249–58. doi: 10.1002/(SICI)1096-9896(199901)187:2<249::AID-PATH222>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]