Abstract
Accessory mitral valve tissue (AMVT) is a rare congenital anomaly of endocardial cushion. Usually, it arises from the anterior mitral leaflet and causes the left ventricular outflow tract obstruction. We report here the first and a rarest presentation of the AMVT in a 19-year old female patient diagnosed to have double outlet right ventricle, ventricular septal defect (VSD), infundibular stenosis and congenital mitral stenosis (MS). She presented with a history of shortness of breath and chest pain over 3 years. Diagnosis was made by chest X-ray, transthoracic and transoesophageal echocardiography, which was confirmed by cardiac catheterization, and angiography. A successful closure of the VSD with excision of the right ventricular bundle and excision of the AMVT was done. Post-operative course was uneventful and an echocardiogram before the discharge showed no residual shunt, no right ventricular outflow gradient or mitral regurgitation, and the gradient across the mitral valve was 5/3 mmHg. We emphasize that, although AMVT commonly produces left ventricular outflow tract obstruction, it should be considered a rare but an important cause of congenital MS.
Keywords: Accessory mitral valve tissue, Congenital mitral stenosis, Echocardiography, Angiography
INTRODUCTION
Congenital mitral stenosis (MS) is a rare congenital cardiac malformation and the obstruction to the flow across the mitral valve is caused by many conditions such as supramitral ring, commissural fusion, short chordae, anomalous mitral arcade, anomalous position of the papillary muscles and the so-called ‘parachute mitral valve’. Accessory mitral valve tissue (AMVT) causing the congenital MS is very rare. We describe here a case of 19-year old female diagnosed to have a double outlet right ventricle (DORV), ventricular septal defect (VSD), infundibular stenosis and congenital MS produced by an AMVT.
CASE REPORT
A 19-year old female presented with complaints of shortness of breath and chest pain over 3 years with the negative history of rheumatic fever. Physical examination revealed grade 4/6 ejection systolic murmur at the left upper parasternal border. Chest radiography showed right ventricular type of apex. Electrocardiogram showed the right-axis deviation. Transthoracic and transesophageal echocardiography revealed a large sub-aortic VSD with bidirectional shunt, overriding of aorta (Fig. 1a), a right ventricular outflow gradient of 57 mmHg and good-sized pulmonary arteries. Mitral valve showed normal leaflets with good mobility and the presence of a homogenous opacity moving along with the posterior mitral leaflet (PML) with normal-sized annulus for the age. There was no supramitral ring, the commissures were free and the sub-valve was normal with normal interpapillary distance and gradient of 17/9 mmHg across the mitral valve (Fig. 1b). Cardiac catheterization showed that the pulmonary-systemic blood flow ratio was 1.71:1. The pulmonary vascular resistance index was 1.45 Wu m2. Pressure study showed right ventricular pressure 125/12 mmHg, pulmonary artery pressure 45/20(31) mmHg, pulmonary artery wedge pressure 25 mmHg, left ventricular pressure 130/9 mmHg and the gradient across the mitral valve 16 mmHg. Saturation study showed oxygen step up of 11% from the right atrium to the right ventricle. Left ventriculogram showed a single large sub-aortic VSD and the right ventricular angiogram showed the presence of anomalous muscle bundles.
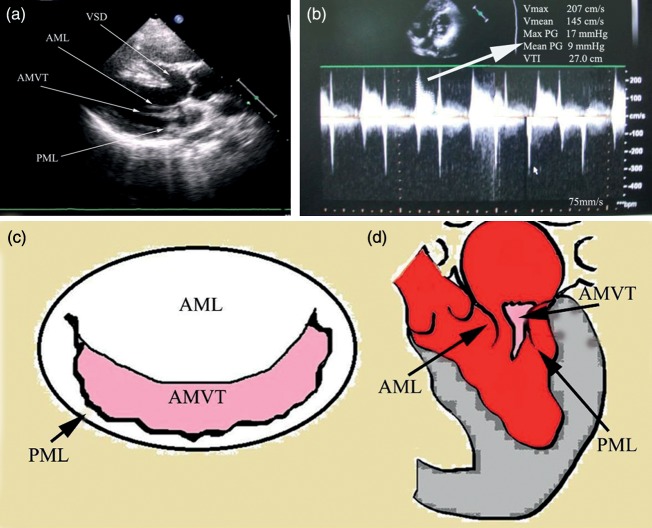
Figure 1:
(a) Long-axis view showing VSD with overriding of aorta and AMVT attached to the PML. (b) Two-dimensional echocardiography showing the gradient across the mitral valve. (c) A line diagram of the mitral valve showing an AMVT arising from the PML. (d) A line diagram in the long-axis view of the left ventricle showing an AMVT projecting between the leaflets more close to the PML. AML, anterior mitral leaflet; PML, posterior mitral leaflet; Ao, aorta; VSD, ventricular septal defect; AMVT, accessory mitral valve tissue; LV, left ventricle; LA, left atrium.
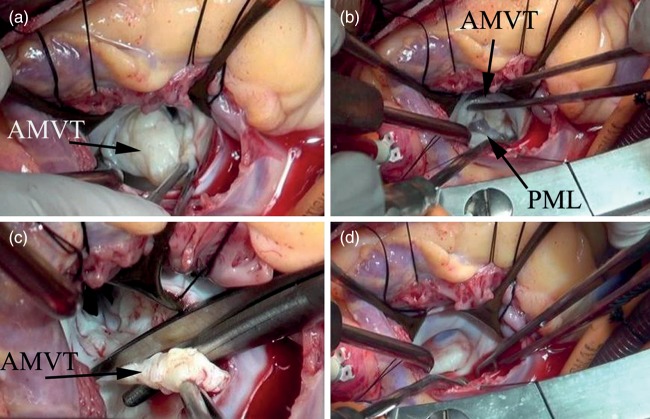
The procedure was performed through a median sternotomy and the cardiopulmonary bypass was established with aortic and bicaval cannulation. Moderate hypothermia and cold blood antegrade root cardioplegia were used to arrest the heart. After cross-clamping the aorta, the right atrium and the interatrial septum were opened. The anatomy showed a DORV with single large sub-aortic VSD and tight os infundibulum with thickened muscle bundles. The mitral valve showed a thickened fibrotic extra leaflet-like tissue of about 3 cm × 3 cm size arising from the PML (Figs 1c and d, 2a and b) and which was free from the subvalvar tissue of the mitral apparatus. Both anterior and the posterior leaflets were normal without commissural or subvalvar fusion. The infundibular os was excised, the muscle bands and bundles were cut and the right ventricular outflow tract was sized up to 22 Hegars. VSD was closed with partially cut Hemashield tube graft using 4-O interrupted polypropylene sutures. The AMVT was excised (Fig. 2c) and the valve tested was found to be competent (Fig. 2d). Weaning from the cardiopulmonary bypass was done in a usual way. Intraoperative transoesophageal echocardiogram showed no residual VSD and the gradient across the mitral valve was 4/2 mmHg with mild mitral regurgitation. The post-operative course was uneventful and an echocardiogram before the discharge revealed no residual shunt, no right ventricular outflow gradient or mitral regurgitation, and the gradient across the mitral valve was 5/3 mmHg.
Figure 2:
(a) AMVT arising from the PML. (b) AMVT lifted from the PML. (c) Accessory mitral tissue being excised. (d) Competent mitral valve after excising the accessory mitral valve tissue. AMVT, accessory mitral valve tissue; PML, posterior mitral leaflet.
DISCUSSION
AMVT is a rare congenital anomaly [1–3]. Embryologically, it develops as a result of an incomplete separation of the mitral valve from the endocardial cushion tissue [1]. AMVT commonly produces signs of left ventricular outflow tract obstruction [2, 3]. The congenital MS produced by an AMVT is not reported in the literature till now. This is the first case of an AMVT producing the congenital MS associated with DORV, VSD and PS. AMVT can vary in appearance from ‘amorphous gelatinous tissue’ to a ‘mature duplicate’ of the mitral valve and has been described in several ways, including sac, balloon, parachute, sail, leaflet, sheet, membranous or pedunculated [4]. In our case, it was like an extra leaflet arising from the PML and was free from the subvalvar apparatus. The transthoracic and transoesophageal echocardiography is a very important tool in establishing the diagnosis [3]. From a surgical point of view, congenital MS may produce particular technical problems because of associated lesions, and the relatively limited experience in each institution [5, 6]. It is important to identify intraoperatively the anatomic relationship between the accessory tissue and the mitral valve, to prevent the valve injury. In our case, the closure of the VSD with excision of right ventricular bundle along with excision of the AMVT was done successfully. The histopathological analysis also confirmed it as a normal leaflet tissue with myxoid degeneration.
In conclusion, the diagnostic modalities and the surgical strategy outlined herein were successful in relief of a rare form of congenital MS, and we recommend the same for similar cases.
Conflict of interest: none declared.
REFERENCES
- 1.Streeter GL. Developmental horizons in human embryos: description of groups XI, 13–20 somites, and age group XII, 21–29 somites. Contrib Embryol. 1942;30:211–46. [Google Scholar]
- 2.Yoshimura N, Yamaguchi M, Oshima Y, Oska S, Ootaki Y, Tei T, et al. Clinical and pathological features of accessory valve tissue. Ann Thorac Surg. 2000;69:1205–8. doi: 10.1016/s0003-4975(99)01580-5. [DOI] [PubMed] [Google Scholar]
- 3.Ow EP, DeLeon SY, Freeman JE, Freeman JR, Quinones JA, Bell TJ, et al. Recognition and management of accessory mitral tissue causing severe subaortic stenosis. Ann Thorac Surg. 1994;57:952–5. doi: 10.1016/0003-4975(94)90212-7. [DOI] [PubMed] [Google Scholar]
- 4.Prifti E, Frati G, Bonacchi M, Vanini V, Chauvaud S. Accessory mitral tissue causing left ventricular outflow tract obstruction: case reports and literature review. J Heart Valve Dis. 2001;10:774–9. [PubMed] [Google Scholar]
- 5.Coles JG, Williams WG, Watanabe T. Surgical experience with reparative techniques in patients with congenital mitral valvular anomalies. Circulation. 1987;76(Suppl III):III-117–22. [PubMed] [Google Scholar]
- 6.Stellin G, Bortolotti U, Mazzucco A. Repair of congenitally malformed mitral valve in children. J Thorac CardioVasc Surg. 1988:480–5. [PubMed] [Google Scholar]