Abstract
This clinical trial tested the effect of daily application of 10% w/v calcium phosphopeptide-amorphous calcium phosphate (CPP-ACP) paste for 1 yr when added to regular toothbrushing with fluoridated toothpaste to prevent dental caries in pre-school children. High-caries-risk children aged 2½ to 3½ yrs in a suburban area of central Thailand were assigned to receive either CPP-ACP (n = 150) or a placebo control (n = 146) in addition to fluoridated toothpaste. The International Caries Detection and Assessment System (ICDAS) was recorded at baseline, 6 mos, and 1 yr. At 1 yr, a significant increase in mean numbers of enamel and dentin caries lesions, as well as dmfs, was found in both groups (p < 0.001). No significant difference was observed between groups on these 3 outcome measures (p = 0.23, 0.84, and 0.91, respectively). The odds of enamel caries lesion transitions to a state of regression or stability, compared with progression from baseline, was also not different between groups [OR = 1.00, 95% CI (0.86, 1.17)]. This trial found that daily application of 10% w/v CPP-ACP paste on school days for 1 yr, when added to regular toothbrushing with a fluoride toothpaste, had no significant added effect in preventing caries in the primary dentition of these pre-school children (ClinicalTrials.gov number CT01 604109).
Keywords: caries detection/diagnosis/prevention, child dentistry, clinical studies/trials, enamel, preventive dentistry, remineralization
Introduction
Early childhood caries (ECC) is a major public health problem worldwide, especially in Thailand, where water fluoridation is not available and milk fluoridation is limited. According to the 6th National Oral Health Survey in Thailand 2006, 3-year-old children in the central part of the country have the highest caries prevalence rates, 69.8%, with dmft 3.63 (Thai Ministry of Health, 2007). Effective efforts to prevent caries and non-invasive treatment of initial caries lesions in young children are needed. Fluoride is widely accepted as the most effective tool for caries prevention. Current best practice recommends twice-daily toothbrushing with fluoride toothpaste for dentate children (Zero et al., 2012). Higher levels of caries prevention were reported in school or pre-school setting studies with supervised toothbrushing compared with unsupervised brushing at home (Twetman et al., 2003).
There is evidence that casein phosphopeptide-amorphous calcium phosphate, CPP-ACP, can bolster the effects of fluoridated toothpaste alone to prevent caries. The localized CPP-ACP nanocomplexes in plaque and on tooth surfaces can buffer the free calcium and phosphate ion activities, maintain a state of supersaturation with respect to tooth enamel, prevent enamel demineralization, and promote remineralization (Cross et al., 2007). Several studies have shown a synergistic effect of CPP-ACP and fluoride in reducing caries (Cochrane et al., 2008; Reynolds et al., 2008). Almost all clinical trials have investigated the effectiveness of CPP-ACP-containing products in caries prevention and enhancing remineralization of initial caries lesions in the permanent dentition of young adolescents (Andersson et al., 2007; Morgan et al., 2008; Bailey et al., 2009; Rao et al., 2009; Beerens et al., 2010; Brochner et al., 2011; Robertson et al., 2011). The majority of these studies reported the surrogate outcomes of caries and did not present all available caries data for all tooth surfaces or participants.
The purpose of this study was to determine if adding the daily application of a CPP-ACP-containing paste for 1 yr is superior to regular fluoride toothbrushing in preventing caries in high-caries-risk pre-school children.
Materials & Methods
The study design was a one-year, double-blind, placebo-controlled clinical trial. The study protocol was approved by the University of Washington and Thammasat University Human Subjects Divisions. The study took place in two provinces in central Thailand, near Bangkok, where water fluoride concentration is less than 0.1 ppm. Ten public nursery schools, with no organized oral health care program, participated. Power calculations indicated that 101 children per group would yield a power of 80% to detect a 30% difference in the average number of new enamel caries lesions (ds1-3) between groups at a 5% significance level. Previous studies (Andersson et al., 2007; Robertson et al., 2011) had indicated an effect size that includes a 30% reduction in a similar time period. Therefore, the recruitment goal was 150 children per group to allow for attrition.
Participants and Recruitment
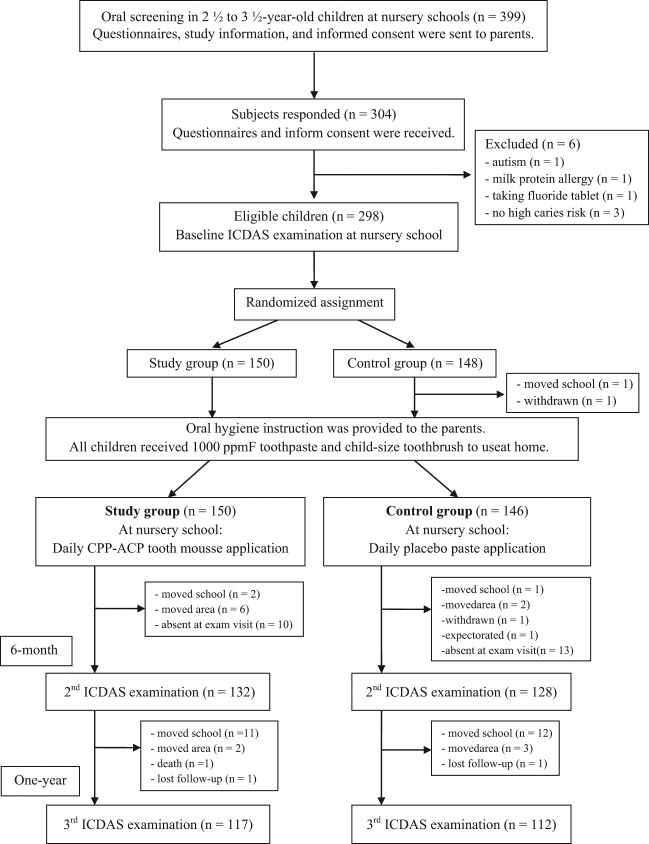
The participants were healthy Thai boys and girls aged between 2½ and 3½ yrs with normal development of dentition and diagnosed as high-caries-risk based on a subset of items from the Caries-risk Assessment Tool (AAPD, 2008). The recruitment began in June, 2010. The exclusion criteria were the chronic use of medications or antibiotics, lack of cooperation in the oral examination, allergies to milk protein or benzoate preservatives, presence of oral soft-tissue lesions or enamel hypoplasia at baseline examination, or have received a fluoride supplement or professional topical fluoride application at least 3 mos before or during the study period. The results of the oral screening of 399 children deemed eligible for the study were sent to their parents with questionnaires on the child’s general and oral health, parents’ demographics, and informed consent. In total, 296 children enrolled in the study (Fig.). Oral examination at baseline, according to the International Caries Detection and Assessment System (ICDAS), was performed in July-August, 2010, with the last follow-up examination taking place in September, 2011.
Figure.
Flow sheet of research methodology and participant disposition.
Assignment to Conditions and Description of the Intervention
After baseline ICDAS, children were systematically allocated to two groups, and the allocation of treatment to each group was done randomly. The allocation of experimental or control group was determined by an assistant who was not involved in the clinical aspects of the study, to reduce potential biases. To facilitate the logistics involving participation of children from 10 schools, within each province, sequential identification numbers were assigned to the alphabetical lists of participants’ names (1-191 and 1-107, respectively). Randomly, those with odd ID numbers were assigned to the experimental treatment, and those with even ID numbers to the control treatment. Those in the experimental group were assigned to receive 10% w/v CPP-ACP paste, Tooth Mousse® (GC Corporation, Tokyo, Japan) daily; those in the control group received a placebo paste that had identical packaging, color, and taste, since it was prepared and provided by the same manufacturer. All staff, teachers, and participating children were blinded to the group assignment and did not know which paste is more effective in caries prevention. The paste code was retained by the manufacturer and broken only after analysis of the study results.
The paste was applied by trained teachers every school day, using each child’s coded paste, following toothbrushing with fluoridated toothpaste after lunch. For each application, approximately 0.4 g of paste was used and applied to tooth surfaces by means of a disposable cotton-tipped applicator. After that, children were encouraged to delay swallowing and avoid expectoration, then took their afternoon nap. An application checklist was collected each month to ensure the consistency of paste application and compliance of the teachers.
Prior to the study, there was a meeting between the dental staff and the parents for oral hygiene instruction, information on hands-on toothbrushing techniques, and distribution of the 1,000-ppm fluoridated toothpaste and toothbrushes to brush each child’s teeth at home during the study period. All children received professionally applied fluoride varnish at the end of the study.
Measurement
Dental caries clinical examinations were conducted according to ICDAS II criteria that classify severity of dental lesions, ranging from the early clinically visible change in enamel to extensive cavitation, and presenting 6 stages of the caries process in ordinal code (Ismail et al., 2007). There were 88 coronal tooth surfaces for each child examined. Prior to the examination, the child’s teeth were cleaned by means of a slow-speed handpiece with a brush and non-fluoride prophylaxis paste. All children were examined at the nursery schools by one pediatric dentist who was blinded to the child’s group assignment. The ICDAS training exercise was carried out 3 days before the examinations. Intra-examiner reliability, based on approximately 10% of the children and computed by the weighted kappa statistic at baseline, 6 mos, and 1 yr, was high: 0.80, 0.79, and 0.87, respectively.
Statistical Methods
All data were processed by SPSS 16.0 (SPSS Inc., Chicago, IL, USA). Independent t tests and repeated-measures analysis of variance were used to test differences between the two study groups in mean number of surfaces with dental caries per child. The primary outcome was the mean number of enamel caries lesions (ds1-3).
The transitional scores of enamel caries lesions from baseline to 6 mos and 1 yr were calculated and recoded as (lesion) regression, stable, or progression (i.e., follow-up ICDAS score minus baseline ICDAS score ≥ 1), to monitor the transition of lesions during the study period. In this calculation, all treated surfaces (sealants, restorations, and extractions) at 6 mos and 1 yr were excluded. The logistic regression model was used to analyze the efficacy of the CPP-ACP-containing paste; stable or regressed lesions were combined into one category and compared with progressed lesions, assuming independent behavior of all lesions.
Results
There were 296 high-caries-risk pre-school children enrolled in the study (143 boys, 153 girls). Of these, 150 were assigned to the experimental condition and 146 to the control condition. The average age was 36.9 ± 2.9 mos in the experimental group and 37.2 ± 3.0 mos in the control group. After 1 yr, 229 children remained in the study; the drop-out rates of the experimental and the control groups were 22.0% and 23.3% (p = 0.79). Two major reasons for drop-out were children’s transfer to higher level schools and families moving out of the area (Fig.). The outcome analyses were limited to the 213 children who participated in all 3 oral examinations, 110 from the experimental group and 103 from the control group. Neither side-effects from nor adverse reaction to paste application occurred in this study.
At baseline, the two groups were comparable in terms of potential confounders with respect to age, gender, eating behaviors, toothbrushing behavior, and parents’ socio-economic status, except that more children in the experimental group reported falling asleep with a bottle (p = 0.008). However, this was not diagnosed as a risk factor for all caries outcome measures of this study. The baseline dmfs/dmft score for both groups was high, 9.1/4.3 and 9.4/4.3, respectively (Table 1), whereas the overall treated surfaces (mfs) were extremely low (0.11) (Table 2). The difference in baseline dmfs/dmft observed between two groups was not statistically significant (p = 0.88 and p = 0.91) (Table 1).
Table 1.
Participant Characteristics
| Characteristics | Experimental Group | Control Group | p-valuea | |
|---|---|---|---|---|
| Number of participants | 110 | 103 | ||
| Average age, months (mean ± SD) | 36.8 ± 3.0 | 37.2 ± 3.0 | 0.39 | |
| Gender, % | Boy | 53.6 | 50.5 | 0.65 |
| Girl | 46.4 | 49.5 | ||
| Snack between meals, % | None | 11.2 | 5.9 | 0.48 |
| Once a day | 25.2 | 22.5 | ||
| Twice a day | 29.9 | 35.3 | ||
| Three or more times a day | 33.6 | 36.3 | ||
| Child still uses bottle, % | No | 28.2 | 30.4 | 0.72 |
| Yes | 71.8 | 69.6 | ||
| Child sleeps with bottle, % | Sometimes or never | 78.0 | 91.2 | 0.008* |
| Every day | 22.0 | 8.8 | ||
| Brushing time per wk (mean ± SD) | 8.1 ± 5.3 | 7.1 ± 5.1 | 0.45 | |
| Who brushes the child’s teeth, % | Child brushes his/her own teeth without supervision | 1.9 | 3.0 | 0.63 |
| Child brushes his/her own tooth with supervision | 61.0 | 66.0 | ||
| Parent or caregiver brushes the child’s teeth | 37.1 | 31.0 | ||
| Child uses fluoride toothpaste, % | No | 1.9 | 2.0 | 1.00 |
| Yes | 98.1 | 98.0 | ||
| Family income, % | < 21,000 Baht | 75.9 | 77.2 | 0.82 |
| ≥ 21,000 Baht | 24.1 | 22.8 | ||
| Parent education, % | Primary school or less | 18.3 | 8.7 | 0.13 |
| Secondary school | 54.1 | 63.1 | ||
| College or 2-year associate degree | 9.2 | 13.6 | ||
| 4-year college degree or higher | 18.3 | 14.6 | ||
| Dental caries at baseline (mean ± SD) | dmfs | 9.1 ± 10.6 | 9.4 ± 12.9 | 0.88 |
| dmft | 4.3 ± 4.2 | 4.3 ± 4.7 | 0.91 |
p-value for the comparison of participant characteristics between the experimental and the control groups
Significant at p-value < 0.05.
Table 2.
Mean Number of Caries Outcome Measures at Baseline, 6 mos, and 1 yr
| ds1-3 |
ds4-6 |
ds5-6 mfs |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Time | Experimental Group | Control Group | p-value2 | Experimental Group | Control Group | p-value | Experimental Group | Control Group | p-value |
| Baseline | 13.49 ± 7.91 | 15.22 ± 10.07 | 0.23 | 10.20 ± 11.01 | 10.47 ± 12.90 | 0.84 | 9.14 ± 10.56 | 9.38 ± 12.91 | 0.91 |
| 6-month | 14.92 ± 7.55 | 16.00 ± 8.93 | 11.75 ± 12.71 | 12.14 ± 14.69 | 11.97 ± 12.72 | 12.23 ± 15.40 | |||
| One-year | 17.04 ± 8.11 | 18.29 ± 9.33 | 12.68 ± 13.16 | 13.14 ± 14.98 | 13.37 ± 13.8 | 13.50 ± 15.91 | |||
| p-value1 | < 0.001* | < 0.001* | < 0.001* | < 0.001* | < 0.001* | < 0.001* | |||
| One-year caries increment | 3.55 ± 5.27 | 3.07 ± 5.86 | 0.52a | 2.48 ± 4.48 | 2.67 ± 4.42 | 0.76 | 4.23 ± 5.14 | 4.13 ± 5.08 | 0.88 |
Data presented as mean ± SD.
ds1-3 = enamel caries lesions (ICDAS score 1, 2, 3).
ds4-6 = dentin caries lesions (ICDAS score 4, 5, 6).
ds5-6mfs = decay, missing, and filled surfaces (dmfs).
p-value1 = tests of within-subject effects (difference within group): based on repeated-measures analysis of variance.
p-value2 = tests of between-subject effects (difference between groups): based on repeated-measured analysis of variance.
a = p-value of the test of differences in 1-year caries increment between groups: based on independent t test.
Overall, mfs (mean) at baseline and 1 yr = 0.11 and 0.74, respectively.
Comparison of background characteristics and baseline dmfs/dmft between the remaining 213 children and the 86 children who dropped out demonstrated no statistically significant difference, except for gender, with significantly more girls in the drop-out group (p = 0.036).
Between baseline and 1 yr, the mean number of caries outcome measures within both groups increased significantly (p < 0.001) However, differences between groups were not statistically significant (Table 2). Children in the experimental group showed a higher number of caries increment outcomes, except for the dentin caries lesion increment, which was slightly greater in the control group.
Overall, at 1 yr, the difference in the distribution of enamel caries lesion transitions between the two groups was not statistically significant [OR = 1.002, 95% CI (0.86, 1.17)]. In addition, there were no significant differences in the enamel caries lesion transition scores between the two groups at the first or second 6 mos of the one-year study (Table 3).
Table 3.
Frequency Distributions of Enamel Caries Lesion (ds1-3) Transitions from Baseline and 6-month Clinical Assessments by Two Groups
| Study Period | Transition | Experimental Group n (%) | Control Group n (%) | OR* | 95 % CI | p-value |
|---|---|---|---|---|---|---|
| Baseline to 6-month | Regression | 413 (28.35%) | 440 (28.08%) | 1.005 | (0.85, 1.18) | 0.95 |
| Stable | 653 (44.82%) | 705 (44.99%) | ||||
| Progression | 391 (26.84%) | 422 (26.93%) | ||||
| 6-month to 1-year | Regression | 413 (22.41%) | 367 (21.50%) | 1.12 | (0.95, 1.32) | 0.17 |
| Stable | 909 (53.72%) | 933 (54.66%) | ||||
| Progression | 370 (21.87%) | 407 (23.84%) | ||||
| Baseline to 1-year | Regression | 317 (21.97%) | 333 (21.35%) | 1.002 | (0.86, 1.17) | 0.97 |
| Stable | 643 (44.56%) | 704 (45.13%) | ||||
| Progression | 483 (33.47%) | 523 (33.53%) |
n (%) = number (percentage) of enamel caries lesions (ds1-3 or ICDAS score 1, 2, 3).
The odds of the enamel caries lesion transitions to a stage of regression or stability, compared with progression between the experimental and the control groups.
Discussion
This study was a double-blind, placebo-controlled clinical trial to compare the effect of daily application of CPP-ACP paste in pre-school children against that of a placebo paste.
All study children resided in non-fluoridated areas and were diagnosed as high-caries-risk, with evidence of visible plaque, dmfs, and enamel caries. Concurrently, the results of parent questionnaires administered at baseline revealed that more than 70% of these pre-school children were bottle-fed, and some slept with bottles. Approximately one-third of the children had 3 or more snacks between meals a day. Parents reported that the children’s teeth were brushed approximately once a day at home, and that the majority of the children (> 63%) brushed by themselves. This finding was consistent with those of the 6th national oral health survey in 2006, which reported that only 36.35% of 3-year-old children’s parents brushed their child’s teeth. Thus, we could not anticipate the oral cleanliness of these children, which depends on parental awareness. The caries experience (dmfs/t), therefore, was extremely high in Thai pre-school children. In addition, two-thirds (67.61%) of the children in this study were classified as having severe ECC (dmfs of upper anterior teeth ≥ 1). Therefore, oral hygiene and hands-on toothbrushing instructions were provided to all parents prior to the study, with the expectation that parents would have more awareness of their children’s oral health.
Clinical examinations were recorded according to ICDAS II criteria, an effective assessment tool for caries in the primary dentition, with acceptable reproducibility and validity with histological depth (Braga et al., 2009; Shoaib et al., 2009). ICDAS scores of 5 and 6 were used to represent the decay index of the dmfs/dmft indices, since WHO criteria diagnosed dental caries in cavitated dentin. This study concentrated on the caries- preventive ability of CPP-ACP paste based on previous reports which demonstrated significant regression of white-spot lesions by CPP-ACP paste in post-orthodontic patients (Andersson et al., 2007; Bailey et al., 2009). Moreover, the enamel caries lesions (13-15 surfaces/child) were a major caries finding in these high-caries-risk children. Therefore, the enamel caries lesion (ds1-3) was focused upon as a primary outcome and used in sample size calculation.
At the conclusion of the intervention, the increment in mean numbers of enamel caries lesions in the experimental and the control groups (3.55 and 3.07 surfaces, respectively) indicated a large increase in new enamel caries lesions from previously sound enamel over the one-year period. The dmfs incremental rate of both groups was 4.23 and 4.12 surfaces, respectively, with no significant difference. This rate is slightly greater than findings from a one-year monitoring study of 9- to 18-month-old Thai children whose parents received hands-on toothbrushing instruction with fluoridated toothpaste. That study reported a dmfs incremental rate of 3.3 surfaces, whereas the group without hands-on toothbrushing instruction showed a dmfs incremental rate as high as 18.9 surfaces (Thanakanjanaphakdee and Triratvorakul, 2010). Another study, of Chinese children aged 3-4 years, found dmfs increased by 5 within 2 yrs (Jiang et al., 2005).
In the present study, we expected that ds1-3, ds4-6, and dmfs increment would be lower in the experimental group than in the control group. However, the results did not support this expectation.
Our results showed that approximately 33.5% of enamel caries lesions progressed during the one-year follow-up period, which is less than shown in a study in southern Thai children aged 12 to 18 mos, which reported that approximately 40% of initial enamel caries lesions progressed to cavitated dentin during 3 to 9 mos (Thitasomakul et al., 2006). The odds of enamel lesions regressing or remaining stable did not show a greater effect of CPP-ACP paste than the placebo paste at any of the follow-up periods. This result did not support the findings, which showed an enhancement in white-spot lesion (ICDAS score 2-3) regression by 12-week use of CPP-ACP paste (Bailey et al., 2009). However, in that study, if ICDAS score 1 was included in the transitional analysis, their result did not show significant difference between two pastes.
In the present study, the pastes were applied by the children’s teachers within 10 min following the children’s toothbrushing with fluoridated toothpaste and immediately before the afternoon nap. The reason for this choice was a synergistic effect with fluoride and longer contact with the teeth. We found little evidence of beneficial effects of CPP-ACP paste, and this might be due to the strong positive effects of the fluoridated toothpaste. Further studies might be conducted for longer follow-up time, other application times, or the absence of fluoridated toothpaste.
In conclusion, in a study that focused on caries prevention and initial enamel caries lesion remineralization in the primary dentition of high-caries-risk pre-school children, this clinical trial did not detect any difference between daily application of CPP-ACP-containing paste immediately following brushing with fluoridated toothpaste and brushing with fluoridated toothpaste alone at nursery schools for a one-year study period.
Acknowledgments
The authors acknowledge the nursery school teachers of Patumthani and Saraburi provinces as well as the pre-school children and their parents for their cooperation.
Footnotes
This study was supported by the Fogarty International NIH grant #D43TW007768. The CPP-ACP and placebo pastes were provided by GC Corporation, Japan.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- American Academy of Pediatric Dentistry (2008). Policy on use of a caries-risk assessment tool (CAT) for infants, children, and adolescents (Reference manual 2008-2009). Pediatr Dent 30(7 Suppl):29S-33S [PubMed] [Google Scholar]
- Andersson A, Skold-Larsson K, Hallgren A, Petersson LG, Twetman S. (2007). Effect of a dental cream containing amorphous cream phosphate complexes on white spot lesion regression assessed by laser fluorescence. Oral Health Prev Dent 5:229-233 [PubMed] [Google Scholar]
- Bailey DL, Adams GG, Tsao CE, Hyslop A, Escobar K, Manton DJ, et al. (2009). Regression of post-orthodontic lesions by a remineralizing cream. J Dent Res 88:1148-1153 [DOI] [PubMed] [Google Scholar]
- Beerens MW, van der Veen MH, van Beek H, ten Cate JM. (2010). Effects of casein phosphopeptide amorphous calcium fluoride phosphate paste on white spot lesions and dental plaque after orthodontic treatment: a 3-month follow-up. Eur J Oral Sci 118:610-617 [DOI] [PubMed] [Google Scholar]
- Braga MM, Oliveira LB, Bonini GA, Bonecker M, Mendes FM. (2009). Feasibility of the International Caries Detection and Assessment System (ICDAS-II) in epidemiological surveys and comparability with standard World Health Organization criteria. Caries Res 43:245-249 [DOI] [PubMed] [Google Scholar]
- Brochner A, Christensen C, Kristensen B, Tranaeus S, Karlsson L, Sonnesen L, et al. (2011). Treatment of post-orthodontic white spot lesions with casein phosphopeptide-stabilised amorphous calcium phosphate. Clin Oral Investig 15:369-373 [DOI] [PubMed] [Google Scholar]
- Cochrane NJ, Saranathan S, Cai F, Cross KJ, Reynolds EC. (2008). Enamel subsurface lesion remineralisation with casein phosphopeptide stabilised solutions of calcium, phosphate and fluoride. Caries Res 42:88-97 [DOI] [PubMed] [Google Scholar]
- Cross KJ, Huq NL, Reynolds EC. (2007). Casein phosphopeptides in oral health—chemistry and clinical applications. Curr Pharm Des 13:793-800 [DOI] [PubMed] [Google Scholar]
- Ismail AI, Sohn W, Tellez M, Amaya A, Sen A, Hasson H, et al. (2007). The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol 35:170-178 [DOI] [PubMed] [Google Scholar]
- Jiang H, Bian Z, Tai BJ, Du MQ, Peng B. (2005). The effect of a bi-annual professional application of APF foam on dental caries increment in primary teeth: 24-month clinical trial. J Dent Res 84:265-268 [DOI] [PubMed] [Google Scholar]
- Morgan MV, Adams GG, Bailey DL, Tsao CE, Fischman SL, Reynolds EC. (2008). The anticariogenic effect of sugar-free gum containing CPP-ACP nanocomplexes on approximal caries determined using digital bitewing radiography. Caries Res 42:171-184 [DOI] [PubMed] [Google Scholar]
- Rao SK, Bhat GS, Aradhya S, Devi A, Bhat M. (2009). Study of the efficacy of toothpaste containing casein phosphopeptide in the prevention of dental caries: a randomized controlled trial in 12- to 15-year-old high caries risk children in Bangalore, India. Caries Res 43:430-435 [DOI] [PubMed] [Google Scholar]
- Reynolds EC, Cai F, Cochrane NJ, Shen P, Walker GD, Morgan MV, et al. (2008). Fluoride and casein phosphopeptide-amorphous calcium phosphate. J Dent Res 87:344-348 [DOI] [PubMed] [Google Scholar]
- Robertson MA, Kau CH, English JD, Lee RP, Powers J, Nguyen JT. (2011). MI Paste Plus to prevent demineralization in orthodontic patients: a prospective randomized controlled trial. Am J Orthod Dentofacial Orthop 140:660-668 [DOI] [PubMed] [Google Scholar]
- Shoaib L, Deery C, Ricketts DN, Nugent ZJ. (2009). Validity and reproducibility of ICDAS II in primary teeth. Caries Res 43:442-448 [DOI] [PubMed] [Google Scholar]
- Thai Ministry of Health (2007). The 6th national oral health survey in 2005-2006, Thailand. Bangkok: Ministry of Public Health [Google Scholar]
- Thanakanjanaphakdee W, Triratvorakul C. (2010). Effectiveness of parental hands-on toothbrushing instruction toward the 1-year incremental dmf rate of 9-18 month-old children. J Dent Assoc Thai 60:85-93 [Google Scholar]
- Thitasomakul S, Thearmontree A, Piwat S, Chankanka O, Pithpornchaiyakul W, Teanpaisan R, et al. (2006). A longitudinal study of early childhood caries in 9- to 18-month-old Thai infants. Community Dent Oral Epidemiol 34:429-436 [DOI] [PubMed] [Google Scholar]
- Twetman S, Axelsson S, Dahlgren H, Holm AK, Kallestal C, Lagerlöf F, et al. (2003). Caries-preventive effect of fluoride toothpaste: a systematic review. Acta Odontol Scand 61:347-355 [DOI] [PubMed] [Google Scholar]
- Zero DT, Marinho VC, Phantumvanit P. (2012). Effective use of self-care fluoride administration in Asia. Adv Dent Res 24:16-21 [DOI] [PubMed] [Google Scholar]