Abstract
Dental caries is a ubiquitous disease affecting all age groups and segments of the population. It is known that not all caries lesions progress to cavitation, but little is known regarding the progression pattern of caries lesions. This study’s purpose was to evaluate the natural history of dental caries using a standardized, visually based system, the International Caries Detection and Assessment System (ICDAS). The study population consisted of 565 consenting children, who were enrolled and examined at baseline and at regular intervals over 48 months with ICDAS and yearly bitewing radiographs. Of these, 338 children completed all examinations. Not all lesions cavitated at the same rate, differing by surface type and baseline ICDAS severity score and activity status. With increasing severity, the percentage of lesions progressing to cavitation increased: 19%, 32%, 68%, and 66% for ICDAS scores 1, 2, 3, and 4, respectively. Lesions on occlusal surfaces were more likely to cavitate, followed by buccal pits, lingual grooves, proximal surfaces, and buccal and lingual surfaces. Cavitation was more likely on molars, followed by pre-molars and anterior teeth. Predictors of cavitation included age, gender, surfaces and tooth types, and ICDAS severity/activity at baseline. In conclusion, characterization of lesion severity with ICDAS can be a strong predictor of lesion progression to cavitation.
Keywords: longitudinal study, dental caries, ICDAS, activity, lesion progression, Hispanic
Introduction
Despite our knowledge of the basic concepts of dental caries, little is known regarding the progression of dental caries lesions. It has long been known that not all lesions progress to cavitation (Backer Dirks, 1966). The challenge has been to determine which white-spot lesions will progress to cavitation. Unfortunately, despite all the efforts in caries detection in the past couple of decades, assessment of caries lesion activity at the time of examination is not usually part of the clinical examination (Zero et al., 2011). Thus, the only option available to dentists is to monitor caries lesions longitudinally before deciding on a restorative intervention. Once a tooth surface is restored, it enters a repetitive restorative cycle (Elderton, 1990), leading to a cascade of costly restorative treatments (Zero et al., 2011); therefore, minimizing the need for surgical intervention is the key to improving clinical outcomes.
The International Caries Detection and Assessment System (ICDAS; Pitts, 2004) has been shown to be reproducible and accurate (Jablonski-Momeni et al., 2008) and provides the ability for dentists to visually detect and assess early lesions and provide longitudinal follow-up (Burt et al., 2006; Ekstrand et al., 2007; Finlayson et al., 2007; Ismail et al., 2007, 2008; Sohn et al., 2007; Cook et al., 2008; Jablonski-Momeni et al., 2008; Varma et al., 2008).
The objective of this study was to determine if characteristics of non-cavitated lesions can be used as surrogates for cavitated lesions by longitudinal evaluation of tooth surfaces with the ICDAS criteria.
Materials & Methods
As previously described (Ferreira Zandona et al., 2010; Fontana et al., 2011), a convenience sample of 565 children (kindergarten to 9th grade) from public schools in Aguas Buenas, Puerto Rico, was recruited in January 2007, as approved by the institutional review board committees from Indiana University (IU-IRB #0608-15) and the University of Puerto Rico (UPR-IRB#A1340107). Parental consent was obtained along with assent from the child for children older than 7 yrs. This sample size, based on preliminary data, allowed for a sufficient number of clinically significant lesions at the end of the four-year study. For inclusion in the study, children had to be between 5 and 13 yrs of age, have no medical problem that contraindicated participation, and allow examination of the oral cavity, including radiographs and digital photographs. Caries-free and caries-active children were included. All children were required to have at least 1 permanent molar with at least 1 unrestored surface, with no upper limit to the number of carious surfaces.
All children received (at baseline, 8, 12, 20, 24, 28, 32, 36, 40, 44, and 48 mos) an oral soft-tissue examination and an examination by a calibrated examiner using the ICDAS criteria, which range from 0 to 6 (Ferreira Zandona et al., 2010). Additionally, each lesion was given an activity score (active/inactive) at each examination period. The activity score was subjective, based on surface luster (opaque or translucent), texture (rough or smooth), and location (in a plaque stagnation area or not). At each visit, teeth were brushed and flossed by study personnel, air-dried, and assessed under light, without magnification, according to the ICDAS criteria and following ICDAS guidelines (Ismail et al., 2007) and the activity criteria. At baseline and yearly examinations (12, 24, 36, and 48 mos), full-mouth examinations were conducted and up to 4 bite-wing radiographs obtained. Radiographs were independently analyzed by a modified version of the ICDAS criteria (0 = sound surface; 1 = outer ½ of enamel; 2 = inner ½ of enamel including DEJ; 3 = outer 1/3 of dentin; 4 = middle 1/3 of dentin; 5 = middle 1/3 of dentin; 6 = into the pulp). At the interim examinations (8, 20, 28, 32, 40, and 44 mos), only posterior teeth (pre-molars and molars) were examined. The data were collected on tablet PCs equipped with custom-made software (Optiform, Indianapolis, IN, USA). At the yearly examinations, the primary examiner repeated the examination on 10% of the children to assess intra-examiner repeatability, and a back-up examiner examined 10% of the children to evaluate inter-examiner agreement. At every examination, children received a referral form for dental care. This study complied with STROBE guidelines.
Repeatability of the ICDAS examinations was assessed by weighted kappa statistics. DMFS/dmfs counts at baseline were calculated with ICDAS 1, 3, and 5 as thresholds for the decay portion of the counts. Comparisons between children who attended the final study visit and those who did not were made with chi-square tests for differences in ethnicity, race, and sex, and with two-sample t tests for differences in baseline DMFS/dmfs counts. Lesion cavitation was considered as lesions going from ICDAS score 0-4 to ICDAS 5-6 or filled or missing due to caries. Surfaces with orthodontic bands and surfaces on which sealants were placed were evaluated up to banding/sealant placement. The associations of age, sex, tooth type, surface, and baseline ICDAS severity/activity scores with time to cavitation were analyzed by Cox proportional hazards survival analysis, with a frailty term to account for multiple observations per child. The associations of age, sex, tooth type, surface, and baseline ICDAS severity/activity scores with the presence of cavitation during follow-up or within the first 2 yrs of follow-up were analyzed by generalized estimating equation (GEE) methods applied to logistic regression models.
Results
In total, 338 children completed the 48-month examination. Attrition was, on average, 10% per yr, with higher attrition in yr 1 (18.6%) and in the older age group. The vast majority of children were Hispanic (91%), and 51% were boys. Despite over 99% of children having dental insurance, at 48 mos there was only a slight increase in the number of fillings (4.9 ± 6.0 at baseline vs. 5.4 ± 6.7 at 48 mos). There were no differences between children who completed the 48-month examinations and those who did not in terms of ethnicity, race, gender, and combined DMFS/dmfs counts. On average, DMFS/dmfs at threshold ICDAS 1 (initial lesions) was 16.3 ± 13.2, that at threshold ICDAS 3 (moderate lesion) was 8.5 ± 9.2, and that at threshold ICDAS 5 (extensive lesion cavitated into dentin) was 7.6 ± 8.7. Children who completed the 48-month examinations were 1.3 yrs younger than those who did not (p < 0.001) and had significantly lower DMFS scores at all thresholds (ICDAS 1, 3, and 5, DMFS scores 8.7, 3.2, and 2.7, respectively, p ≤ 0.0002) and higher dmfs scores (7.0, 5.4, and 5.0, respectively, p < 0.01). Two calibrated examiners conducted all the examinations, one from baseline to 24 mos and another from 28 to 48 mos. Intra-examiner weighted kappa repeatability ranged from 0.77 to 0.81, and inter-examiner repeatability ranged from 0.54 to 0.62. Analyses of cavitation included only primary lesions on permanent teeth with no fillings at baseline and used both ICDAS and radiograph scores.
Progression of lesions to cavitation varied according to surface type and lesion severity and activity status at baseline (Tables 1 and 2). Only 3% of surfaces that were sound at baseline progressed during the study period, and 1% progressed within the first 2 yrs. Of the teeth that were unerupted at baseline that erupted during the study period, 1% of the surfaces cavitated. Almost 19% of the surfaces scored as ICDAS 1 cavitated, 8% during the first 2 yrs. Over 32% of the surfaces scored as ICDAS 2 lesions cavitated, 17% within the first 2 yrs. Almost 68% of the lesions scored as ICDAS 3 cavitated, 46% within the first 2 yrs. All of the ICDAS 4 lesions were considered active and were most likely to cavitate during the study. Significance tests indicated cavitation differences for (in order) ICDAS 4 or 3, 2-active, 2-inactive/1-active/1-inactive, sound, and unerupted (significant p values were p ≤ 0.001, 1-inactive vs. 1-active vs. 2-inactive, p = 1.00, 2-inactive vs. 2-active, p = 0.07, and 3 vs. 4, p = 1.00). Lesions on occlusal surfaces were more likely to cavitate, ranging from 7% (surfaces unerupted at baseline) to 78% (ICDAS 3 at baseline), followed by cavitation on buccal pits and lingual grooves, proximal surfaces, and buccal and lingual surfaces.
Table 1.
Percentage (%) of Lesions Progressing to Cavitation According to ICDAS and Activity Scores at Baseline
| Baseline ICDAS | Active Lesion | Total Number of Surfaces | Ever Progressed, N (%) | Progressed within First 2 yrs, N (%) |
|---|---|---|---|---|
| Unerupted | No | 21,786 | 307 (1%) | 71 (0%) |
| 0 | No | 37,549 | 1,114 (3%) | 513 (1%) |
| 1 | No | 429 | 98 (23%) | 47 (11%) |
| 1 | Yes | 1,614 | 286 (18%) | 122 (8%) |
| 2 | No | 125 | 22 (18%) | 17 (14%) |
| 2 | Yes | 1,039 | 353 (34%) | 182 (18%) |
| 3 | No | 4 | 1 (25%) | 1 (25%) |
| 3 | Yes | 155 | 107 (69%) | 72 (46%) |
| 4 | Yes | 116 | 76 (66%) | 54 (47%) |
Table 2.
Percentage (%) of Lesions Progressing to Cavitation According to Surface Type and ICDAS and Activity Scores at Baseline
| Baseline ICDAS | Active Lesion | Surface Type | Total Number of Surfaces | Ever Progressed, N (%) | Progressed within First 2 yrs, N (%) |
|---|---|---|---|---|---|
| Unerupted | No | B | 4,243 | 12 (0%) | 3 (0%) |
| 0 | No | B | 7,905 | 105 (1%) | 49 (1%) |
| 1 | No | B | 84 | 6 (7%) | 3 (4%) |
| 1 | Yes | B | 361 | 24 (7%) | 8 (2%) |
| 2 | No | B | 25 | 1 (4%) | 1 (4%) |
| 2 | Yes | B | 267 | 41 (15%) | 15 (6%) |
| 3 | No | B | 2 | 0 (0%) | 0 (0%) |
| 3 | Yes | B | 8 | 2 (25%) | 1 (13%) |
| Unerupted | No | L | 4,246 | 11 (0%) | 2 (0%) |
| 0 | No | L | 8,305 | 138 (2%) | 54 (1%) |
| 1 | No | L | 56 | 3 (5%) | 1 (2%) |
| 1 | Yes | L | 150 | 19 (13%) | 6 (4%) |
| 2 | No | L | 13 | 0 (0%) | 0 (0%) |
| 2 | Yes | L | 151 | 21 (14%) | 5 (3%) |
| 3 | Yes | L | 4 | 3 (75%) | 2 (50%) |
| 4 | Yes | L | 3 | 2 (67%) | 1 (33%) |
| Unerupted | No | D | 4,245 | 17 (0%) | 4 (0%) |
| 0 | No | D | 8,344 | 196 (2%) | 80 (1%) |
| 1 | No | D | 2 | 0 (0%) | 0 (0%) |
| 1 | Yes | D | 213 | 33 (15%) | 15 (7%) |
| 2 | Yes | D | 76 | 26 (34%) | 11 (14%) |
| 3 | Yes | D | 8 | 2 (25%) | 1 (13%) |
| 4 | Yes | D | 22 | 15 (68%) | 10 (45%) |
| Unerupted | No | M | 4,245 | 14 (0%) | 4 (0%) |
| 0 | No | M | 7,916 | 174 (2%) | 72 (1%) |
| 1 | No | M | 21 | 2 (10%) | 0 (0%) |
| 1 | Yes | M | 459 | 72 (16%) | 20 (4%) |
| 2 | No | M | 47 | 6 (13%) | 4 (9%) |
| 2 | Yes | M | 125 | 49 (39%) | 22 (18%) |
| 3 | No | M | 1 | 0 (0%) | 0 (0%) |
| 3 | Yes | M | 18 | 11 (61%) | 7 (39%) |
| 4 | Yes | M | 36 | 29 (81%) | 22 (61%) |
| Unerupted | No | BP | 999 | 42 (4%) | 7 (1%) |
| 0 | No | BP | 1,312 | 113 (9%) | 61 (5%) |
| 1 | No | BP | 30 | 8 (27%) | 3 (10%) |
| 1 | Yes | BP | 49 | 18 (37%) | 9 (18%) |
| 2 | No | BP | 5 | 2 (40%) | 2 (40%) |
| 2 | Yes | BP | 64 | 31 (48%) | 19 (30%) |
| 3 | Yes | BP | 14 | 12 (86%) | 8 (57%) |
| 4 | Yes | BP | 5 | 5 (100%) | 4 (80%) |
| Unerupted | No | LG | 972 | 9 (1%) | 5 (1%) |
| 0 | No | LG | 1,269 | 74 (6%) | 38 (3%) |
| 1 | No | LG | 87 | 24 (28%) | 13 (15%) |
| 1 | Yes | LG | 76 | 16 (21%) | 6 (8%) |
| 2 | No | LG | 8 | 2 (25%) | 1 (13%) |
| 2 | Yes | LG | 55 | 19 (35%) | 11 (20%) |
| 3 | Yes | LG | 9 | 4 (44%) | 4 (44%) |
| 4 | Yes | LG | 4 | 0 (0%) | 0 (0%) |
| Unerupted | No | O | 2,836 | 202 (7%) | 46 (2%) |
| 0 | No | O | 2,498 | 314 (13%) | 159 (6%) |
| 1 | No | O | 149 | 55 (37%) | 27 (18%) |
| 1 | Yes | O | 306 | 104 (34%) | 58 (19%) |
| 2 | No | O | 27 | 11 (41%) | 9 (33%) |
| 2 | Yes | O | 301 | 166 (55%) | 99 (33%) |
| 3 | No | O | 1 | 1 (100%) | 1 (100%) |
| 3 | Yes | O | 94 | 73 (78%) | 49 (52%) |
| 4 | Yes | O | 46 | 25 (54%) | 17 (37%) |
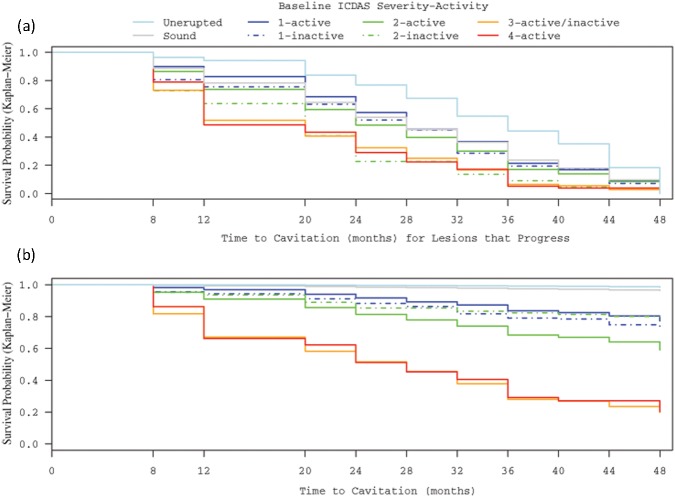
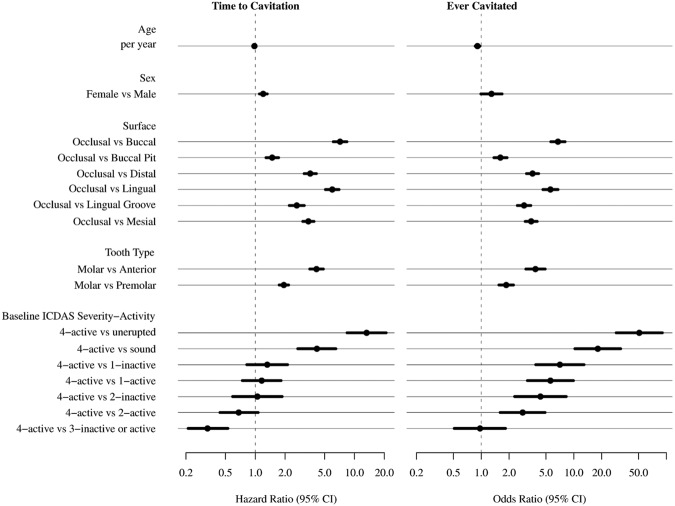
Some important findings were related to how fast lesions progressed (Figs. 1a, 1b). A greater percentage of lesions scored as ICDAS 3 and 4 progressed within 1 yr of baseline examinations. Cavitation of lesions initially scored as ICDAS 1 was spread throughout the 4 yrs, while cavitation of lesions initially scored ICDAS 2 was more concentrated in the first 2 yrs of the study (Fig. 1). Lesions cavitated more quickly and more frequently in girls and in younger children (Fig. 2). Lesions on occlusal surfaces cavitated sooner than lesions on other surfaces, followed by buccal pits, lingual grooves, and interproximal sites, with time to cavitation longest on smooth surfaces (significant p values were p ≤ 0.001, and B vs. L, p = 0.31, D vs. M vs. LG surfaces, p > 0.08). Molar teeth progressed the fastest, followed by premolars and then anteriors. In contrast to the frequency of cavitation, time to cavitation was significantly shortest for ICDAS 3 and also shorter for 2-active than for ICDAS 4 (Fig. 2). Also of interest is that when cavitation was limited to within 2 yrs, age and gender were no longer significant predictors.
Figure 1.
Survival analyses of lesions according to ICDAS scores and activity scores at baseline. (a) Time to cavitation for the surfaces that progressed to cavitation; and (b) time to cavitation including all surfaces.
Figure 2.
Hazard ratio and odds ratio of progression to cavitation by predictors.
Discussion
Modern management of dental caries involves: detecting and assessing caries lesions at an earlier stage; making a diagnosis as to whether the disease is actually present; determining the caries risk status of the patient; establishing a prognosis; applying intervention strategies focused on preventing, arresting, and possibly reversing the caries process; and delaying restorative treatment until absolutely necessary (Zero et al., 2011). Identification of at-risk active sites is a core component for the principles for the modern management of dental caries, and it is one of the biggest challenges faced by dentists. To date, the practice has been mostly to characterize lesions as a “watch” until it is deemed that progression warrants surgical intervention. There is a tendency to opt for early restorative intervention of many lesions (Doméjean-Orliaguet et al., 2004; Tellez et al., 2011; Traebert et al., 2011), despite evidence that early lesions on occlusal surfaces can often be sealed (Beauchamp et al., 2008), hampering further progression. This leads to an irreversible restorative cycle (Tellez et al., 2011). Analysis of the data in this study indicates that careful monitoring of dental surfaces by the ICDAS criteria can identify predictors of progression and rate of progression. This can be a valuable tool for dentists to use to determine treatment decisions and surface prognosis. To our knowledge, the only other study that examined the natural history of dental caries longitudinally using detailed criteria was the study by Backer Dirks in 1966. Despite the subjectivity of the activity criteria used in the current study, it is notable that, for all ICDAS scores, a greater percentage of lesions that were considered active at baseline progressed to cavitation.
We confirmed some findings that had been previously reported: Molars are more susceptible to caries, followed by premolars and anterior teeth (Mejàre and Stenlund, 2000); and occlusal surfaces are more susceptible to dental caries than other surfaces (Richardson and McIntyre, 1996). In this population, lesions in younger children progressed faster, likely due to eruption stage (Carlos and Gittelsohn, 1965). Gender, as previously reported (Lukacs and Largaespada, 2006), was also found to be a predictor of the rate and odds of progression.
ICDAS is a set of visual criteria based on the examination of clean, dry surfaces. ICDAS 0 is for sound surfaces, ICDAS 1 and 2 are scores for initial lesions (or early, white-spot lesions), and ICDAS 3 and 4 are moderate or established lesions. These lesions do not have frank cavitations exposing the dentin, although they might have microcavitations (ICDAS 3/4), and histologically have reached the dentin (ICDAS 2/3/4). ICDAS scores 5 and 6 are extensive, frank cavitations, with dentin exposure and different levels of surface destruction. Traditionally, dentists do not detect ICDAS score 1 (it requires focused surface-drying) and place a “watch” on lesions with ICDAS scores of 2 and 3. Although a greater percentage of lesions scored as ICDAS 4 progressed to cavitation, lesions scored as ICDAS 3 progressed at a faster rate. The clinical implications of these findings are that in younger children, especially girls, on occlusal surfaces with lesions scored as ICDAS 4 and 3, an intervention strategy (therapeutic sealant) should be instituted sooner rather than later. If these lesions show on bite-wing radiographs as affecting the middle third of the dentin, the dentin is heavily infected, and thus minimal surgical intervention is indicated (Ricketts et al., 2002). On surfaces with lesions considered active and scored as ICDAS 1 and 2, the treatment plan should not be a “watch” but rather a therapeutic intervention, such as therapeutic sealant placement on occlusal surfaces, fluoride varnishes on smooth surfaces, and/or infiltrants. For lesions that are progressing faster (within 2 yrs), which were mostly the lesions scored ICDAS 4, 3, and 2, age and gender were not significant predictors. This indicates that, for these more established lesions, surface, tooth type, ICDAS score, and activity status are more important predictors than age and gender. This knowledge should support the implementation of these non-surgical approaches to caries management, since the careful monitoring of the lesions allows for delay or elimination of the need for restorative intervention. Additional analyses of these data on outcomes of restorative interventions based on ICDAS scores at baseline can provide greater insight into intervention thresholds.
We acknowledge that these results are based on a high-risk, rather uniform rural population of Hispanic schoolchildren in Puerto Rico, and the results many not be applicable to other populations. However, there are certainly implications for clinical research on preventive/therapeutic interventions for high-risk populations in whom detailed criteria such as ICDAS can be used to determine outcomes at shorter intervals than in traditional caries trials. For reasons unrelated to the study, the first examiner was not available after the 24-month examinations, when the back-up examiner took over the study. The examiners had been previously calibrated against each other in a different group of individuals and achieved a kappa threshold of 0.89 at the cavitation level. As a precaution, the back-up examiner had examined a group of children at 12 and 24 mos, but the agreement was lower than during calibration. However, since the outcome of the study was cavitation, inter-examiner agreement at the cavitation thereshold was 0.64, and the baseline ICDAS code was used to determine progression, we do not believe that this was a cause for concern regarding the analyses reported here.
In conclusion, surfaces that are sound or with initial caries lesions (ICDAS 1 or 2) that transition to moderate lesions (ICDAS 3 or 4) can be used as surrogates of cavitation (ICDAS 5 and 6) in high-risk populations. Careful monitoring and non-surgical management of initial active caries lesions can minimize avoidable restorative intervention, leading to improved clinical outcomes.
Acknowledgments
The authors thank the following individuals for their assistance: Ms. Gwinn, Ms. Hernandez, Ms. Riviera, Ms. Tran, Drs. Delgado, Eggertsson, Hernandez, and Gomez and the supporting staff at OHRI and the University of Puerto Rico.
Footnotes
This study was supported by the National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD 20892, USA (NIH-RO1 DEO17890).
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
References
- Backer Dirks O. (1966). Posteruptive changes in dentaldEnamel. J Dent Res 45:503-510 [Google Scholar]
- Beauchamp J, Caufield PW, Crall JJ, Donly K, Feigal R, Gooch B, et al. (2008). Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 139:257-268 [DOI] [PubMed] [Google Scholar]
- Burt BA, Kolker JL, Sandretto AM, Yuan Y, Sohn W, Ismail AI. (2006). Dietary patterns related to caries in a low-income adult population [see comment]. Caries Res 40:473-480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlos JP, Gittelsohn AM. (1965). Longitudinal studies of the natural history of caries. II. A life-table study of caries incidence in the permanent teeth. Arch Oral Biol 10:739-751 [DOI] [PubMed] [Google Scholar]
- Cook SL, Martinez-Mier EA, Dean JA, Weddell JA, Sanders BJ, Eggertsson H, et al. (2008). Dental caries experience and association to risk indicators of remote rural populations. Int J Paediatr Dent 18:275-283 [DOI] [PubMed] [Google Scholar]
- Doméjean-Orliaguet S, Tubert-Jeannin S, Riordan PJ, Espelid I, Tveit AB. (2004). French dentists’ restorative treatment decisions. Oral Health Prev Dent 2:125-131 [PubMed] [Google Scholar]
- Ekstrand KR, Martignon S, Ricketts DJ, Qvist V. (2007). Detection and activity assessment of primary coronal caries lesions: a methodologic study. Oper Dent 32:225-235 [DOI] [PubMed] [Google Scholar]
- Elderton RJ. (1990). Clinical studies concerning re-restoration of teeth. Adv Dent Res 4:4-9 [DOI] [PubMed] [Google Scholar]
- Ferreira Zandona A, Santiago E, Eckert G, Fontana M, Ando M, Zero DT. (2010). Use of ICDAS combined with quantitative light-induced fluorescence as a caries detection method. Caries Res 44:317-322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlayson TL, Siefert K, Ismail AI, Sohn W. (2007). Psychosocial factors and early childhood caries among low-income African-American children in Detroit. Community Dent Oral Epidemiol 35:439-448 [DOI] [PubMed] [Google Scholar]
- Fontana M, Santiago E, Eckert GJ, Ferreira-Zandona AG. (2011). Risk factors of caries progression in a Hispanic school-aged population. J Dent Res 90:1189-1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail AI, Sohn W, Tellez M, Amaya A, Sen A, Hasson H, et al. (2007). The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol 35:170-178 [DOI] [PubMed] [Google Scholar]
- Ismail AI, Sohn W, Tellez M, Willem JM, Betz J, Lepkowski J. (2008). Risk indicators for dental caries using the International Caries Detection and Assessment System (ICDAS). Community Dent Oral Epidemiol 36:55-68 [DOI] [PubMed] [Google Scholar]
- Jablonski-Momeni A, Stachniss V, Ricketts DN, Heinzel-Gutenbrunner M, Pieper K. (2008). Reproducibility and accuracy of the ICDAS-II for detection of occlusal caries in vitro. Caries Res 42:79-87 [DOI] [PubMed] [Google Scholar]
- Lukacs JR, Largaespada LL. (2006). Explaining sex differences in dental caries prevalence: saliva, hormones, and “life-history” etiologies. Am J Hum Biol 18:540-555 [DOI] [PubMed] [Google Scholar]
- Mejàre I, Stenlund H. (2000). Caries rates for the mesial surface of the first permanent molar and the distal surface of the second primary molar from 6 to 12 years of age in Sweden. Caries Res 34:454-461 [DOI] [PubMed] [Google Scholar]
- Pitts N. (2004). “ICDAS”—an international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent Health 21:193-198 [PubMed] [Google Scholar]
- Richardson PS, McIntyre IG. (1996). Susceptibility of tooth surfaces to carious attack in young adults. Community Dent Health 13:163-168 [PubMed] [Google Scholar]
- Ricketts DN, Ekstrand KR, Kidd EA, Larsen T. (2002). Relating visual and radiographic ranked scoring systems for occlusal caries detection to histological and microbiological evidence. Oper Dent 27:231-237 [PubMed] [Google Scholar]
- Sohn W, Ismail A, Amaya A, Lepkowski J. (2007). Determinants of dental care visits among low-income African-American children. J Am Dent Assoc 138:309-318 [DOI] [PubMed] [Google Scholar]
- Tellez M, Gray SL, Gray S, Lim S, Ismail AI. (2011). Sealants and dental caries: dentists’ perspectives on evidence-based recommendations. J Am Dent Assoc 142:1033-1040 [DOI] [PubMed] [Google Scholar]
- Traebert J, Jinbo Y, de Lacerda JT. (2011). Association between maternal schooling and caries prevalence: a cross-sectional study in southern Brazil. Oral Health Prev Dent 9:47-52 [PubMed] [Google Scholar]
- Varma S, Banerjee A, Bartlett D. (2008). An in vivo investigation of associations between saliva properties, caries prevalence and potential lesion activity in an adult UK population. J Dent 36:294-299 [DOI] [PubMed] [Google Scholar]
- Zero DT, Zandona AF, Vail MM, Spolnik KJ. (2011). Dental caries and pulpal disease. Dent Clin North Am 55:29-46 [DOI] [PubMed] [Google Scholar]