Abstract
Background
Lung cancer is a heterogeneous disease with multiple signaling pathways influencing tumor cell survival and proliferation, and it is likely that blocking only one of these pathways allows others to act as salvage or escape mechanisms for cancer cells. Whether combined inhibition therapy has greater anti-tumor activity than single inhibition therapy is a matter of debate. Hence, a meta-analysis comparing therapy inhibiting both VEGFR and EGFR signaling pathways with that inhibiting EGFR signaling pathway alone was performed.
Methodology and Principal Findings
We searched PubMed, EMBASE database and the proceedings of major conferences for relevant clinical trials. Outcomes analyzed were objective tumor response rate (ORR), progression-free survival (PFS), overall survival (OS) and toxicity. Besides, subgroup analyses were performed to investigate whether the combined inhibition therapy is best performed using combination of selective agents or a single agent with multiple targets.
Six trials recruiting 3,302 patients were included in the analysis. Combined inhibition therapy was associated with a 3% improvement in OS as compared with single-targeted therapy, but this difference was not statistically significant (HR, 0.97; 95% CI, 0.89–1.05; P = 0.472). Patients receiving combined inhibition therapy had significant longer PFS than the group with single-targeted therapy (HR, 0.80; 95% CI, 0.67–0.95; P = 0.011). There was no difference in the ORR between the groups (OR, 1.44; 95% CI, 0.95–2.18; P = 0.085). Subgroup analysis revealed that combined inhibition therapy using combination regimens was associated with statistically significant improvement in both ORR and PFS. Toxicity was greater in combined inhibition therapy.
Conclusions
There is no evidence to support the use of combined inhibition therapy in unselected patients with advanced NSCLC. However, given the significant advantage in ORR and PFS, combined inhibition therapy using combination regimens may be considered for further evaluation in subsets of patients who may benefit from this treatment.
Introduction
Non-small-cell lung cancer (NSCLC) accounts for approximately 80–85% of all cases of lung cancer, and is the most common cause of cancer death in industrialized countries [1]. With the notion that a “efficacy plateau” has been achieved with traditional cytotoxic chemotherapy, the treatment armamentarium for advanced NSCLC has expanded to include molecular targeted therapies that act specifically against key components of cellular pathways involved in tumor growth, progression, and cell death. Vascular endothelial growth factor (VEGF) and epidermal growth factor receptor (EGFR) inhibitors are two key molecular targeted therapies in NSCLC. Vascular endothelial growth factor (VEGF or VEGFA) is a key circulating proangiogenic factor which binds to receptors present on endothelial cells (mainly VEGFR2) [2], [3]. VEGF binding induces receptor dimerization and results in autophosphorylation which promotes binding of a number of signaling molecules and activation of intracellular signaling pathways pivotal to the process of angiogenesis [4]. In the pathologic state, VEGF production is increased by tumor cells, which stimulates the endothelial cells in existing vessels to promote the production of new vasculature via direct stimulation of signaling pathways and induction of downstream gene expression [5]. The EGFR is a receptor tyrosine kinase (TK) of the ErbB/HER family. It is expressed at high levels on the surface of many epithelial tumours, including NSCLC and is activated by a variety of ligands principally transforming growth factor alpha and epidermal growth factor [6]. Ligand binding to EGFR induces receptor homo- or hetero-dimerization and results in the activation of an intracellular tyrosine kinase domain. Receptor activation signals key downstream pathways that regulate cell proliferation, differentiation, and survival [7]. Given their prominent role in tumour growth, invasion, and metastasis, the VEGFR and EGFR signaling pathway present feasible targets for pharmacologic intervention in NSCLC, and several agents have demonstrated encouraging antitumor activity. The addition of bevacizumab, a monoclonal antibody against VEGF, to paclitaxel and carboplatin provided clinical benefit in previously untreated non-squamous advanced NSCLC [8]. And the small–molecule EGFR inhibitors, gefitinib and erlotinib, has both demonstrated anti-tumor activity in the treatment of advanced NSCLC [9]–[11].
Despite all of these improvements, the benefits associated with these agents are modest and serve to stress the need for novel therapeutic approaches. Increasing evidence has suggested that solid tumors have multiple salvage and resistance pathways that allow them to circumvent inhibition of a single signaling pathway [12]. Furthermore, NSCLC is a heterogeneous disease and it is believed that there is multi-level cross-stimulation among targets along several pathways of signal transduction that lead to tumor malignancy [13]. In fact, EGFR is known to regulate the production of VEGF and other proangiogenic factors [14], and increased VEGF expression has been associated with resistance to EGFR inhibition in a human tumor xenograft model of NSCLC [15]. Thus, it is likely that blocking only one of these pathways will be insufficient for providing any meaningful therapeutic outcomes. Therefore, a logical strategy for improving anti-tumor efficacy is inhibition of both VEGFR and EGFR signaling pathways, which may help increase suppression of oncogenic processes involved in disease progression [5], [16]–[18]. Actually, several preclinical studies have showed an enhanced benefit from combination EGFR and VEGFR inhibitors in lung cancer cell lines [19], [20]. And combined blocking of VEGFR and EGFR signaling was found to have the potential to overcome primary or acquired resistance to EGFR inhibitors in xenograft models [15], [21].
However, several randomized trials [22]–[27] comparing therapy inhibiting both VEGFR and EGFR signaling pathways with that inhibiting EGFR signaling pathways alone have been conducted and the results were various. Uncertainty remains regarding the presence and magnitude of any improvement in anticancer efficacy of the strategy of combined inhibition of the VEGFR and EGFR signaling pathways for advanced NSCLC. And we were unable to locate any meta-analyses that analyzed and summarized the evidence on the combined inhibition therapy. Hence, we performed a systematic review and meta-analysis of randomized controlled trials to evaluate the effects of the strategy of combined inhibition of the VEGFR and EGFR signaling pathways on overall survival, progression-free survival, response rate and toxicity in patients with advanced NSCLC.
Methods
Search strategy and selection criteria
For inclusion in this meta-analysis, randomized controlled trials were required to compare therapy inhibiting both VEGFR and EGFR signaling pathways with that inhibiting EGFR signaling pathway alone in the treatment of patients with stage IIIB or IV NSCLC. Approach to inhibiting both VEGFR and EGFR signaling pathways could be a single agent with multiple targets or a combination of targeted agents. Trials comparing the combined inhibition therapy with a combination of an agent targeting EGFR signaling pathway and a cytotoxic chemotherapy were not eligible.
Relevant studies were identified by searching PubMed, and EMBASE up to Nov 2011 without language restrictions. We performed the search by using the terms “NSCLC,” “non-small-cell lung cancer,” “carcinoma and non-small-cell lung,” “VEGFR,” “EGFR,” “clinical trial,” and “randomized trial.” This search was supplemented by a manual search the annual meeting proceedings of American Society of Clinical Oncology (ASCO) and European Society of Medical Oncology (ESMO) from 2004 to 2011. The relevant reviews and meta-analyses regarding the role of combined inhibition therapy for NSCLC patients were examined for potential inclusive trials. Moreover, we also searched in http://www.who.int/triasearch and http://www.ClinicalTrials.gov websites for information on registered randomized controlled trials.
Data extraction and quality assessment
Data abstraction and quality assessment were conducted independently by 2 reviewers using a standardized approach. Disagreements were adjudicated by a third reviewer after referring to the original articles.
Data retrieved from the reports included publication details, methodological components, and trial characteristics such as sample size, interventions, and outcome measures. End points of interest included overall survival (OS), progression-free survival (PFS), objective tumor response rate (ORR) and adverse events (AEs). The quantitative 5-point Jadad scale [28] was used to assess the quality of the inclusive trials based on the reporting of the studies' methods and results.
Statistical analysis
For time-to-event data, the log hazard ratios (HRs) and their variances were estimated using the methods proposed by Parmar [29] when confidence intervals (CIs) of HRs were reported. The summary HRs and their 95% CIs were estimated using a general variance-based method.
For objective tumor response rate (ORR) and toxicities, estimates of the treatment effects were obtained from the number of events reported in each arm and combined using the methods reported by Mantel and Haenszel [30]. To calculate ORR, patients obtaining complete response or partial response were considered as responders. The AEs of treatments were analyzed as drug-related WHO grades 3 or greater toxicity. An odd ratio (OR) >1 indicates a higher tumor response rate and more toxicity in the combined inhibition arm.
The χ2 test and I2 statistic were employed to assess variability across studies attributable to heterogeneity beyond chance [31]. A p-value greater than 0.10 for the χ2 test and an I2 value less than 25% were interpreted as signifying low-level heterogeneity. When there was no statistically significant heterogeneity, a pooled effect was calculated with a fixed-effect model; otherwise, a random-effect model was employed. Subgroup analyses were performed to determine if the results were influenced by different approaches to inhibiting both VEGFR and EGFR signaling pathways (a single agent or a combination of agents). We also assessed the probability of publication bias with Egger's test [32] and Begg-Mazumdar test [33]. Statistical significance was defined as a two-tailed p-value less than 0.05. All statistical analyses were conducted with the software Stata 11.0.
Results
Trial characteristic
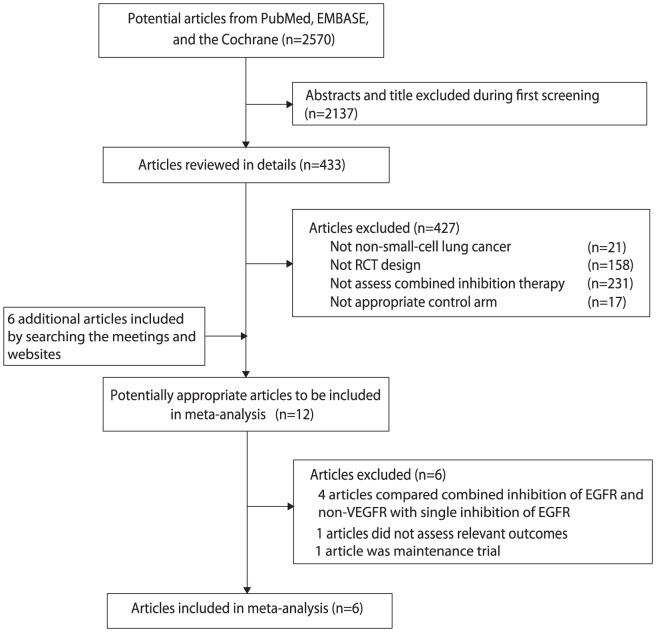
Our systematic search identified 2570 potentially relevant abstracts, of which 12 potentially eligible trials that had investigated combined inhibition therapy versus single inhibition therapy were identified (Figure 1). Of these, six trials were excluded: 4 trials [34]–[37] compared combined inhibition of EGFR and non-VEGFR signaling pathways (c-MET, HDAC, mTOR) with single inhibition of EGFR signaling pathway; 1 trial [38] was maintenance trial and 1 trial [39] did not assess relevant outcomes.
Figure 1. Identification process for eligible studies.
Finally, 6 trials including 3,302 patients that met the inclusion criteria were included in the meta-analysis. Four trials [22]–[24], [27] were published in full articles, while two [25], [26] were published only as meeting abstracts. All trials included patients with stage IIIB to IV NSCLC. 2 trials [22], [23] assessed vandetanib, a single multi-targeted agent inhibiting both VEGFR and EGFR signaling pathways, whereas the other 4 trials [24]–[27] assessed a combination of targeted agents as combined inhibition therapy. Table 1 summarized the characteristics of the 6 included trials.
Table 1. Characteristics of included trials.
| Authors (Year) | Number of Patients | Therapy of Treatment And Control Arm | Male (%) | Median Age (years) | Stage IV (%) | WHO PS = 2 (%) | Jadad Score |
| Ronald B. Natale et al. (2009) [22] | 168 | Vandetanib 300 mg once-daily until PD or PT | 48 (58) | 63 | 69 (83) | 0 (0) | 4 |
| Gefitinib 250 mg once-daily until PD or PT | 52 (61) | 61 | 63 (74) | 0 (0) | |||
| H.J.M.Groen et al. (2010) [25] | 132 | Sunitinib 37.5 mg once daily plus Erlotinib 150 mg once daily until PD or PT | 39 (60) | NR | NR | NR | 4 |
| Placebo plus Erlotinib 150 mg once daily until PD or PT | 45 (67) | NR | NR | NR | |||
| Ronald B. Natale, et al. (2011) [23] | 1240 | Vandetanib 300 mg/d until PD or PT | 381 (61) | 61 | 517 (83) | 65 (10) | 4 |
| Erlotinib 150 mg/d until PD or PT | 393 (64) | 61 | 519 (84) | 77 (13) | |||
| Roy S.Herbst et al. (2011) [24] | 636 | Bevacizumab 15 mg/kg on the first day of 3-week cycles (±4 days) plus Erlotinib 150 mg/day until PD or PT | 171 (54) | 65 | NR | 23 (7) | 5 |
| Placebo 15 mg/kg on the first day of 3-week cycles (±4 days) plus Erlotinib 150 mg/day until PD or PT | 170 (54) | 65 | NR | 20 (6) | |||
| David R.Spigel et al. (2011) [27] | 166 | Sorafenib 400 mg orally twice a day plus Erlotinib 150 mg orally daily until PD or PT | 62 (56) | 65 | NR | 13(12) | 4 |
| Placebo plus Erlotinib 150 mg orally daily until PD or PT | 26 (47) | 65 | NR | 10(18) | |||
| R. Govindan et al. (2011) [26] | 960 | Sunitinib 37.5 mg once daily plus Erlotinib 150 mg once daily until PD or PT | 297 (62) | 61 | 438 (91) | 2 (0.4) | 4 |
| lacebo plus Erlotinib 150 mg once daily until PD or PT | 284 (59) | 61 | 448 (93) | 1 (0.2) |
Abbreviations: NR, not reported; PD, disease progression; PT, prohibitive toxicity.
Jadad scale was used to assess the quality of the included trials. Overall, one trial [24] had a Jadad score of 5, and five [22], [23], [25]–[27] scored 4.
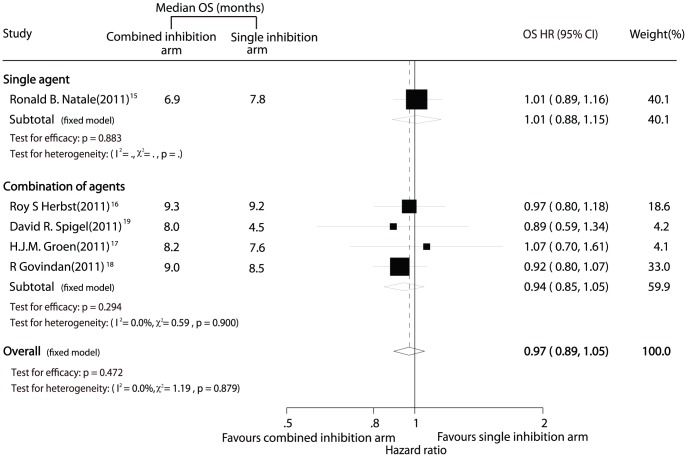
Overall Survival (OS)
Data for OS were available from 5 trials [23]–[27] including 3,134 patients. The data of the trial by Natale et al. [22] was excluded from the analysis of OS in our meta-analysis because the two-part crossover design might confound assessment of the effect of vandetanib on OS. Combined inhibition therapy was associated with a 3% improvement in OS as compared with single inhibition therapy, but this difference was not statistically significant (HR, 0.97; 95% CI, 0.89–1.05; P = 0.472; Figure 2). There was no significant heterogeneity for OS among the individual trials (P = 0.88; I2 = 0.0%), and no evidence of significant publication bias was detected (Egger test, P = 0.956; Begg-Mazumdar test, P = 1.000).
Figure 2. Comparison of overall survival between combined inhibition therapy and single inhibition therapy.
Results were similar when subgroup analyses were conducted, with no differences detected between single inhibition therapy and combined inhibition therapy with either a single agent or a combination of agents (Figure 2).
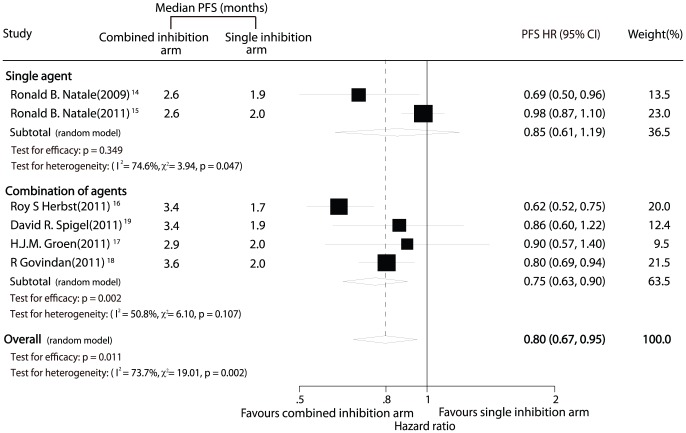
Progression-Free Survival (PFS)
All 6 trials [22]–[27] including 3,302 patients provided PFS results. The meta-analysis revealed that combined inhibition therapy yielded a clinically and statistically significant 21% improvement in PFS compared with single inhibition therapy (HR, 0.80; 95% CI, 0.67–0.95; P = 0.011; Figure 3).
Figure 3. Comparison of progression-free survival between combined inhibition therapy and single inhibition therapy.
Nevertheless, there might be substantial heterogeneity in the HRs for PFS from the individual trials (P = 0.002; I2 = 73.7%) and we incorporated it into random-effects model. Furthermore, subgroup analysis was conducted according to the different approaches to inhibiting both VEGFR and EGFR signaling pathways. Combined inhibition therapy using combination regimen demonstrated clinically substantial and statistically significant improvement in PFS (HR, 0.75; 95% CI, 0.63–0.90; P = 0.002, Figure 3) with much less heterogeneity ((P = 0.13; I2 = 47%). However, no significantly statistical differences in PFS were detected between combined inhibition therapy with a single multi-targeted agent and single inhibition therapy (HR, 0.85; 95% CI, 0.61–1.19; P = 0.349, Figure 3).
No evidence of publication bias was found using Egger test (P = 0.596) or Begg-Mazumdar test (P = 1.000).
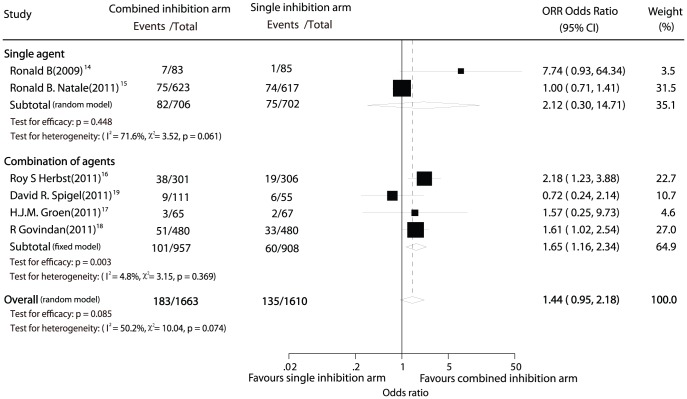
Objective Tumor Response Rate (ORR)
Data for ORR was available from 6 trials [22]–[27] including 3,273 patients. Combined inhibition therapy was associated with 11.00% absolute tumor response rate while single inhibition therapy yielded 8.39%, however, this difference was not statistically significant (OR, 1.44; 95% CI, 0.95–2.18; P = 0.085; Figure 4). There was some evidence of heterogeneity for ORR among the individual trials (P = 0.07; I2 = 50%). No evidence of significant publication bias was detected (Egger test, P = 0.421; Begg-Mazumdar test, P = 0.452).
Figure 4. Comparison of objective tumor response rate between combined inhibition therapy and single inhibition therapy.
In the subgroup analysis of combined inhibition therapy using a single multi-targeted agent, the result was consistent, with no significant difference in ORR between combined inhibition therapy and single inhibition therapy (OR, 2.12; 95% CI, 0.30–14.71; P = 0.448, Figure 4).
However, combined inhibition therapy using combination regimen was associated with statistically significant improvement in ORR compared with single inhibition therapy (OR, 1.66; 95% CI, 1.19–2.32; P = 0.003, Figure 4). And the effect estimate was not heterogeneous among studies (P = 0.37; I2 = 5%).
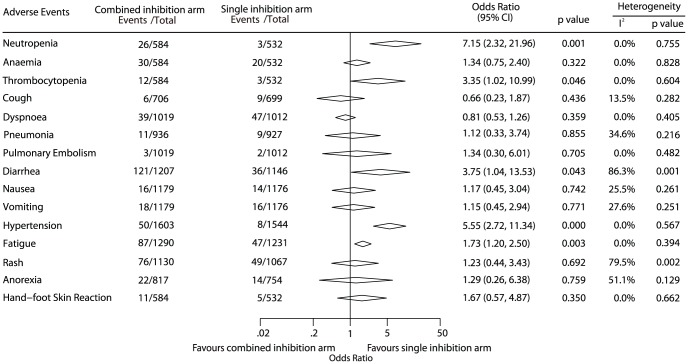
Adverse events
A summary of WHO grade 3 or greater adverse events is reported in Figure 5. Considerable variability in the completeness of toxicity reporting was found among the studies. Overall, combined inhibition therapy was associated with a significant increase in the risk for neutropenia (OR, 7.15; 95% CI, 2.32–21.96), thrombocytopenia (OR, 3.35; 95% CI, 1.02–10.99), diarrhea (OR, 3.75; 95% CI, 1.04–13.53), hypertension (OR, 5.55; 95% CI, 2.72–11.34), and fatigue (OR, 1.73; 95% CI, 1.20–2.50). Heterogeneity among individual trials was found in some adverse events analyses, possibly due to the different agents.
Figure 5. Summary of toxicities grade 3 or greater.
Discussion
NSCLC is a heterogeneous disease and multiple signaling pathways influence tumor cell survival and proliferation. Previous studies tested the hypothesis that the therapy inhibiting both VEGFR and EGFR signaling pathways could improve survival. Although all randomised trials failed to prove gain in overall survival, some researchers advocated that new trials with bigger sample size or proper strategy would be necessary to increase overall survival. A meta-analysis of the previous publications could answer some of the questions, including if the combined inhibition therapy would really benefit the patients and which combined inhibition approach is better. This systematic review represents the best current evidence about the combined inhibition therapy in treatment of advanced NSCLC.
The pooled analysis, with data obtained from 3,302 NSCL patients, found that the treatment inhibiting both VEGFR and EGFR signaling pathways does not improve overall survival among unselected patients. Hence, existing evidence from randomized controlled trials does not support the use of combined inhibition therapy for unselected patients with advanced NSCLC. However, the subset analyses of the trial by Spigel et al. [27] suggested that sorafenib plus erlotinib was associated a statistically significant improvement in OS compared with erlotinib alone among the EGFR wild-type (WT) patients (HR, 0.53; 95% CI, 0.29–0.98; one-sided P = 0.019). Similarly, OS advantage for sorafenib plus erlotinib compared with erlotinib alone was also suggested among patients with EGFR FISH–negative cancers (median OS: 10.55 months for sorafenib plus erlotinib vs 4.60months for erlotinib; one-sided P = 0.064) [27]. And despite lack of statistical significance, results of the trial which assessed the efficacy of addition of bevacizumab to erlotinib also suggested that patients with EGFR-mutant tumours may benefit from the combined inhibition therapy (median OS: 18 months for bevacizumab plus erlotinib vs 12 months for erlotinib; HR, 0.44; 95% CI, 0.11–1.67). These suggest that combined inhibition therapy has a potential advantage in the treatment of advanced NSCLC compared with single inhibition therapy, if the subsets of patients who may benefit from this treatment are identified.
Differently, the results of this meta-analysis demonstrated that combined inhibition therapy yielded a statistically significant benefit in PFS as compared with single inhibition therapy. However, it should be noted progression-free survival was not improved when a single multi-targeted agent (vandetanib) was used to inhibit both the VEGFR and EGFR signaling pathways while delay in disease progression was observed when a combination of targeted agents was used for combined inhibition therapy. Similarly to progression-free survival, improvement in response rate was only found in combined inhibition therapy using combination regimen. One potential explanation for the negative results of combined inhibition therapy using one multi-targeted agent is its effect on inhibition both the VEGFR and EGFR signaling pathways is not as specific as that of single-targeted therapy (e.g. bevacizumab, erlotinib), which may compromise its overall anti-tumor efficacy. Although tumor biomarker analyses from the ZODIAC study [40] suggested that consistent trends toward improved OS, PFS, and objective response rate for patients with EGFR gene copy number (FISH+) or EGFR mutation status (MT) tumors were seen with vandetanib group plus docetaxel versus docetaxel alone, it is not clear whether vandetanib has a potential advantage in patients with specific biomarkers as compared with single EGFR signaling pathways inhibition therapy (e.g. erlotinib). Hence, solid recommendation of a single multi-targeted agent as combined inhibition therapy could not be given based on current evidence.
As expected, some toxicity was significantly more severe in patients who received combined inhibition therapy. Symptomatic improvement due to tumor shrinkage should be balanced with increased toxic effects of combined inhibition therapy. And Concerns remain regarding the impact of the increased toxicity of combined inhibition therapy on patients' quality of life. Unfortunately, data on quality of life were rarely available in these trials and no conclusions could be drawn. However, significant increase in some adverse events (like hypertention, diarrhea or fatigue) in the combined inhibition therapy arm may impair quality of life.
The main purpose of the meta-analysis was to present all available evidence in a systematic, quantitative, and unbiased fashion. Several technical limitations of this meta-analysis should be acknowledged. The analysis is not based on individual patient data, which might provide further insight into the efficacy of the combined inhibition therapy [41]. Heterogeneity among trials can be another limitation of our meta-analysis. We applied a random-effect model that takes possible heterogeneity into consideration and preformed subgroup analyses according to the combined inhibition approach to further explore the source of heterogeneity. It is of interest that most of the variability comes from studies using a single multi-targeted agent as combined inhibition therapy, whereas the trials using combination regimen are much more consistent with one another. Other limitations include publication status and treatment regimens.
A number of other dual-inhibition strategies (e.g. m-TOR, c-Met, IGF-1R or histone deacetylase (HDAC) inhibitor plus EGFR inhibitor) have been studied. The addition of c-Met inhibitor to erlotinib has demonstrated promising clinical activity in phase II studies [34], [42] when compared with erlotinib alone, particularly among patients with Met over expression and nonsquamous histology. MET amplification leads to EGFR-independent activation of the PI3K/Akt pathway through the activation of erbB-3-dependent signalling and thereby could lead to EGFR inhibitor resistance [43]. Thus, dual EGFR-Met inhibition has a theoretic advantage for overcoming Met-mediated resistance to EGFR inhibitors [44]. The subset analyses of the trial by Spigel et al [42] suggested that MetMab plus erlotinib were associated with increased PFS and OS as compared with erlotinib alone in patients with Met over expression. And in the study [34] comparing ARQ 197–209 plus erlotinib with erlotinib, a statistically significant improvement in OS was also found in non-squamous patients in favor of ARQ 197–209 and erlotinib combination. Again, identification of predictive markers which may enable treatments to be targeted to specific patient groups is critical.
In conclusion, the findings of this study corroborate the previous findings that the combined inhibition of the VEGFR and EGFR signaling pathways does not improve overall survival among unselected patients. However, evidences of a significant difference in PFS and ORR were found to support further study of combined inhibition therapy using combination regimen. And subgroup analyses of previous studies suggested that overall survival might be improved by sorafenib/erlotinib combination in patients with EGFR WT and EGFR FISH–negative tumors and by bevacizumab/erlotinib combination in patients with EGFR-mutant tumors. Additional study of these combinations in selected patients is warranted.
Funding Statement
The work was supported by the National Nature Science Foundation of China (30872186, 81072388), a grant from the leading talents of science in Shanghai 2010 (022), a grant sponsored by Program of Shanghai Subject Chief Scientist (09XD1405500) and a grant from the innovative program for PhD in Second Military Medical University. The funders had no role in study design, data collection, analysis, decision to publish or preparation of the manuscript.
References
- 1. Jemal A, Siegel R, Ward E, Hao Y, Xu J, et al. (2009) Cancer statistics, 2009. CA Cancer J Clin 59: 225–249. [DOI] [PubMed] [Google Scholar]
- 2. Ferrara N, Davis-Smyth T (1997) The biology of vascular endothelial growth factor. Endocr Rev 18: 4–25. [DOI] [PubMed] [Google Scholar]
- 3. Fontanini G, Vignati S, Boldrini L, Chine S, Silvestri V, et al. (1997) Vascular endothelial growth factor is associated with neovascularization and influences progression of non-small cell lung carcinoma. Clin Cancer Res 3: 861–865. [PubMed] [Google Scholar]
- 4. Ferrara N, Gerber HP, LeCouter J (2003) The biology of VEGF and its receptors. Nat Med 9: 669–676. [DOI] [PubMed] [Google Scholar]
- 5. Pennell NA, Lynch TJ Jr (2009) Combined inhibition of the VEGFR and EGFR signaling pathways in the treatment of NSCLC. Oncologist 14: 399–411. [DOI] [PubMed] [Google Scholar]
- 6. Ciardiello F, Tortora G (2008) EGFR antagonists in cancer treatment. N Engl J Med 358: 1160–1174. [DOI] [PubMed] [Google Scholar]
- 7. Sibilia M, Kroismayr R, Lichtenberger BM, Natarajan A, Hecking M, et al. (2007) The epidermal growth factor receptor: from development to tumorigenesis. Differentiation 75: 770–787. [DOI] [PubMed] [Google Scholar]
- 8. Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, et al. (2006) Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 355: 2542–2550. [DOI] [PubMed] [Google Scholar]
- 9. Maemondo M, Inoue A, Kobayashi K, Sugawara S, Oizumi S, et al. (2010) Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 362: 2380–2388. [DOI] [PubMed] [Google Scholar]
- 10. Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, et al. (2005) Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med 353: 123–132. [DOI] [PubMed] [Google Scholar]
- 11. Kim ES, Hirsh V, Mok T, Socinski MA, Gervais R, et al. (2008) Gefitinib versus docetaxel in previously treated non-small-cell lung cancer (INTEREST): a randomised phase III trial. Lancet 372: 1809–1818. [DOI] [PubMed] [Google Scholar]
- 12. Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, et al. (2007) MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 316: 1039–1043. [DOI] [PubMed] [Google Scholar]
- 13. Maione P, Gridelli C, Troiani T, Ciardiello F (2006) Combining targeted therapies and drugs with multiple targets in the treatment of NSCLC. Oncologist 11: 274–284. [DOI] [PubMed] [Google Scholar]
- 14. Ciardiello F, Troiani T, Bianco R, Orditura M, Morgillo F, et al. (2006) Interaction between the epidermal growth factor receptor (EGFR) and the vascular endothelial growth factor (VEGF) pathways: a rational approach for multi-target anticancer therapy. Ann Oncol 17 Suppl 7: vii109–114. [DOI] [PubMed] [Google Scholar]
- 15. Naumov GN, Nilsson MB, Cascone T, Briggs A, Straume O, et al. (2009) Combined vascular endothelial growth factor receptor and epidermal growth factor receptor (EGFR) blockade inhibits tumor growth in xenograft models of EGFR inhibitor resistance. Clin Cancer Res 15: 3484–3494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Belani CP, Goss G, Blumenschein G Jr (2011) Recent clinical developments and rationale for combining targeted agents in non-small cell lung cancer (NSCLC). Cancer Treat Rev doi:10.1016/j.ctrv.2011.1005.1009. [DOI] [PubMed] [Google Scholar]
- 17. Scagliotti GV (2007) Potential role of multi-targeted tyrosine kinase inhibitors in non-small-cell lung cancer [abstract]. Ann Oncol 18: x32–41. [DOI] [PubMed] [Google Scholar]
- 18. Cascone T, Gridelli C, Ciardiello F (2007) Combined targeted therapies in non-small cell lung cancer: a winner strategy? Curr Opin Oncol 19: 98–102. [DOI] [PubMed] [Google Scholar]
- 19. Wu W, Onn A, Isobe T, Itasaka S, Langley RR, et al. (2007) Targeted therapy of orthotopic human lung cancer by combined vascular endothelial growth factor and epidermal growth factor receptor signaling blockade. Mol Cancer Ther 6: 471–483. [DOI] [PubMed] [Google Scholar]
- 20. Martinelli E, Troiani T, Morgillo F, Rodolico G, Vitagliano D, et al. Synergistic antitumor activity of sorafenib in combination with epidermal growth factor receptor inhibitors in colorectal and lung cancer cells. Clin Cancer Res 16: 4990–5001. [DOI] [PubMed] [Google Scholar]
- 21. Ciardiello F, Bianco R, Caputo R, Damiano V, Troiani T, et al. (2004) Antitumor activity of ZD6474, a vascular endothelial growth factor receptor tyrosine kinase inhibitor, in human cancer cells with acquired resistance to antiepidermal growth factor receptor therapy. Clin Cancer Res 10: 784–793. [DOI] [PubMed] [Google Scholar]
- 22. Natale RB, Bodkin D, Govindan R, Sleckman BG, Rizvi NA, et al. (2009) Vandetanib versus gefitinib in patients with advanced non-small-cell lung cancer: results from a two-part, double-blind, randomized phase ii study. J Clin Oncol 27: 2523–2529. [DOI] [PubMed] [Google Scholar]
- 23. Natale RB, Thongprasert S, Greco FA, Thomas M, Tsai CM, et al. (2011) Phase III trial of vandetanib compared with erlotinib in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol 29: 1059–1066. [DOI] [PubMed] [Google Scholar]
- 24. Herbst RS, Ansari R, Bustin F, Flynn P, Hart L, et al. (2011) Efficacy of bevacizumab plus erlotinib versus erlotinib alone in advanced non-small-cell lung cancer after failure of standard first-line chemotherapy (BeTa): a double-blind, placebo-controlled, phase 3 trial. Lancet 377: 1846–1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Groen HJM, Socinski M, Grossi F, Juhasz E, Gridelli C, et al. (2010) Randomized phase II study of sunitinib(SU) plus erlotinib (E) VS. placebo (P) plus E for the treatment of metastatic non-small-cell lung cancer [abstract]. Ann Oncol 21: viii122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Govindan R, Krzakowski M, Szczesna A, Strausz J, Makhson A, et al. (2011) Sunitinib in combination with erlotinib for the treatment of advanced/metastatic Non-small Cell Lung Cancer(NSCLC):a phase III study. Available: http://www.astro.org/Meetings/UpcomingMeetings/Thoracic/ScientificProgram/pres/documents/ThorPlenaryGovindan.pdf. Assessed 2011 Jul 10.
- 27. Spigel DR, Burris HA III, Greco FA, Shipley DL, Friedman EK, et al. (2011) Randomized, Double-Blind, Placebo-Controlled, Phase II Trial of Sorafenib and Erlotinib or Erlotinib Alone in Previously Treated Advanced Non-Small-Cell Lung Cancer. J Clin Oncol 29: 2582–2589. [DOI] [PubMed] [Google Scholar]
- 28. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, et al. (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17: 1–12. [DOI] [PubMed] [Google Scholar]
- 29. Parmar MK, Torri V, Stewart L (1998) Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 17: 2815–2834. [DOI] [PubMed] [Google Scholar]
- 30.Deeks J, Higgins JPT (2011) Analysing data and undertaking meta-analyses. Cochrane Handbook for Systematic Reviews of Interventions 5.0.0. Available: http://www.cochrane-handbook.org. Accessed 2011 Jul 15.
- 31. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–1101. [PubMed] [Google Scholar]
- 34. Schiller JH, Akerley WL, Brugger W, Ferrari D, Garmey EG, et al. (2010) Results from ARQ 197–209: A global randomized placebo-controlled phase II clinical trial of erlotinib plus ARQ 197 versus erlotinib plus placebo in previously treated EGFR inhibitor-naive patients with locally advanced or metastatic non-small cell lung cancer (NSCLC) [abstract]. J Clin Oncol 28. [Google Scholar]
- 35. Spigel DR, Ervin TJ, Ramlau R, Daniel DB, Goldschmidt JH Jr, et al. (2011) Final efficacy results from OAM4558g, a randomized phase II study evaluating MetMAb or placebo in combination with erlotinib in advanced NSCLC [abstract]. J Clin Oncol 29. [Google Scholar]
- 36. Lynch TJ, Fenton D, Hirsh V, Bodkin D, Middleman EL, et al. (2009) A randomized phase 2 study of erlotinib alone and in combination with bortezomib in previously treated advanced non-small cell lung cancer. J Thorac Oncol 4: 1002–1009. [DOI] [PubMed] [Google Scholar]
- 37. Leighl NB, Soria J, Bennouna J, Blais N, Traynor AM, et al. (2010) Phase II study of everolimus plus erlotinib in previouly treated patients with advanced non-small cell lung cancer (NSCLC). [abstract]. J Clin Oncol 28. [DOI] [PubMed] [Google Scholar]
- 38. Miller VA, O'Connor P, Soh CH, Kabbinavar F (2009) A randomized, double-blind, placebo-controlled, phase IIIb trial (ATLAS) comparing bevacizumab (B) therapy with or without erlotinib (E) after completion of chemotherapy with B for first-line treatment of locally advanced, recurrent, or metastatic non-small cell lung cancer (NSCLC) [abstract]. J Clin Oncol 27. [DOI] [PubMed] [Google Scholar]
- 39.Kim ES, Herbst RS, Wistuba II, Lee JJ, Blumenschein GR Jr, et al.. (2011) The BATTLE trial :personalizing therapy for lung cancer CANCER DISCOVERY 1: doi:10.1158/2159-8274.CD-1110-0010. [DOI] [PMC free article] [PubMed]
- 40. Johnson BE, Ryan AJ, Heymach J, Stephens C, Kennedy SJ, et al. (2010) Tumor biomarker analyses from the phase III ZODIAC study of docetaxel (D) plus or minus vandetanib (VAN) in second-line advanced NSCLC [abstract]. J Clin Oncol 28. [Google Scholar]
- 41. Stewart LA, Parmar MK (1993) Meta-analysis of the literature or of individual patient data: is there a difference? Lancet 341: 418–422. [DOI] [PubMed] [Google Scholar]
- 42. Spigel DR, Ervin TJ, Ramlau R, Daniel DB, Goldschmidt JH Jr, et al. (2011) Final efficacy results from OAM4558g, a randomized phase II study evaluating MetMAb or placebo in combination with erlotinib in advanced NSCLC [abstract]. J Clin Oncol 29. [Google Scholar]
- 43. Cappuzzo F, Marchetti A, Skokan M, Rossi E, Gajapathy S, et al. (2009) Increased MET gene copy number negatively affects survival of surgically resected non-small-cell lung cancer patients. J Clin Oncol 27: 1667–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kim ES, Salgia R (2009) MET pathway as a therapeutic target. J Thorac Oncol 4: 444–447. [DOI] [PMC free article] [PubMed] [Google Scholar]