Abstract
INTRODUCTION
Primary retroperitoneal tumours of mucinous type are extremely rare and can be further sub-divided into benign, borderline or cystadenocarcinoma. Prompt diagnosis of retroperitoneal tumours is important as the majority are malignant.
PRESENTATION OF CASE
Our case describes a 30 year old woman, presenting with a 3 month history of intermittent right iliac fossa pain. Abdominal examination demonstrated a mass palpable in the right iliac fossa. Ultrasonography of the abdomen demonstrated a cystic mass with a magnetic resonance imaging (MRI) scan of the pelvis further defining the lesion. Laparoscopy was performed to further evaluate and ultimately remove the retroperitoneal mass. Macroscopic and microscopic examination reported mucinous epithelium of endocervical type with no evidence of invasion. Findings were consistent with primary retroperitoneal mucinous cystadenoma.
DISCUSSION
This is the 19th reported case of a benign primary retroperitoneal mucinous cystadenoma in the English literature. The origin of mucinous cystadenomas in the retroperitoneum is widely debated with multiple theories suggested. Diagnosis of retroperitoneal tumours is important but difficult as serological investigations, ultrasonography, computed topography and magnetic resonance imaging, although useful, cannot allow a confident diagnosis.
CONCLUSION
Primary retroperitoneal mucinous cystadenoma is a benign tumour, however because of the malignant nature of the majority of mucinous retroperitoneal tumours they should be considered in the differential of chronic abdominal pain despite their rarity.
Keywords: Primary, Retroperitoneal, Mucinous, Cystadenoma
1. Introduction
Retroperitoneal tumours account for less than 0.2% of all neoplasms.1 Primary retroperitoneal tumours of mucinous type are extremely rare and can be further sub-divided into benign, borderline or cystadenocarcinoma. The patient we present was diagnosed with a primary retroperitoneal mucinous cystadenoma (PRMC) of benign type. To the authors knowledge this is only the eighteenth reported case in published literature (Table 1).
Table 1.
Cases of primary retroperitoneal mucinous cystadenoma of benign type reported in the literature.
| Ref. | Case | Age | Sex | Presenting complaint | Investigations |
|---|---|---|---|---|---|
| 2 | Tapper (2010) | 37 | F | Mass | US, MRI, Lap |
| 3 | Del Gobbo (2010) | 52 | F | Pain | US, MRI, Lap |
| 4 | Rifki-Jai (2009) | 43 | F | Mass | US, CT, MRI, Lap |
| 5 | Abedalthegafi (2009) | 44 | F | Mass | US, MRI, Lap |
| 6 | Yan (2008) | 29 | F | Mass/pain | CT, Lap |
| 7 | Kassab (2007) | 80 | F | Mass | US, CT, Lap |
| 8 | Min (2004) | 38 | F | Pain | CT, Lap |
| 9 | Isse (2004) | 18 | F | Flatulence | US, CT, MRI, Lap |
| 85 | F | Pain | – | ||
| 10 | Arribas (2004) | 39 | F | Incidental | – |
| 11 | Tamura (2003) | 14 | F | Incidental | CT, MRI, Lap |
| 12 | Erdemoglu (2003) | 39 | F | Pain | US, Lap |
| 13 | Balat (2001) | 44 | F | Mass | – |
| 14 | Subramony (2001) | 25 | F | Incidental | US, CT, Lap |
| 15 | Kehegias (1999) | 21 | F | Mass/Pain | US, CT, MRI, FNA, Lap |
| 16 | Yunoki (1998) | 45 | F | Mass | US, CT, Lap |
| 17 | Park (1991) | 40 | F | Mass/Pain | US, CT, Lap |
| 18 | Pennell (1989) | 19 | F | – | – |
F = female, US = ultrasonography, CT = computed topography, MRI = magnetic resonance imaging, Lap = laparoscopic investigation, FNA = fine needle aspiration.
2. Case
Our case describes a 30 year old woman, presenting with a 3 month history of intermittent right iliac fossa pain. Her pain was colicky in nature was reported as six out of ten in severity. There were no associated features, and no aggravating or relieving factors. Her past medical history included an appendicectomy for uncomplicated appendicitis when she was 15 years old.
On abdominal examination there was a non-tender 5 cm mass palpable in the right iliac fossa closely related to the anterior superior iliac spine.
Serological investigations revealed a normal full blood count, liver enzymes as well as urea and electrolytes. Ultrasonography of the abdomen demonstrated a 4.9 cm well defined cystic mass separate from the right ovary. Further investigation with a magnetic resonance imaging (MRI) scan of the pelvis revealed a rounded cystic lesion located immediately posterior to the ascending colon (Fig. 1). Diagnostic laparoscopy was performed to further evaluate the mass. The mass was visualised in the retroperitoneum and the procedure was converted to laparotomy. The right side of the colon was mobilised and the retroperitoneal mass was dissected free from surrounding structures and removed intact. The patient made an uncomplicated post-operative recovery. Gross pathology demonstrated a smooth well circumscribed cyst measuring 5 cm in maximal diameter. Microscopic examination reported mucinous epithelium of endocervical type with no evidence of invasion (Figs. 2 and 3). Findings were consistent with primary retroperitoneal mucinous cystadenoma.
Fig. 1.
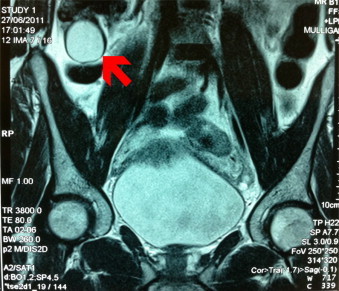
Magnetic resonance image of the pelvis demonstrating a rounded cystic lesion located immediately posterior to the ascending colon.
Fig. 2.
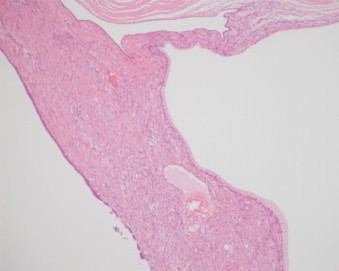
Haematoxylin and eosin stain demonstrating mucinous epithelium of endocervical type with no evidence of invasion (×100).
Fig. 3.
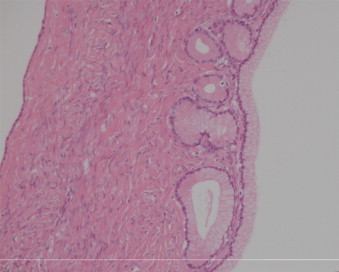
Haematoxylin and eosin stain demonstrating multilocular cystic lesion with mucous producing columnar epithelium (×200).
3. Discussion
This is the 19th reported case of a benign primary retroperitoneal mucinous cystadenoma in the English literature (Table 1). All previous cases were women aged 14–85 with the mean age 39. Presenting symptoms can be at best vague and were predominantly findings of an abdominal mass, chronic abdominal pain or both. There were three incidental presentations with one presentation of flatulence.
The first description of PRMC was undertaken by Handfield-Jones in 1924 in his study on retroperitoneal cysts.19 As there are no epithelial cells in the retroperitoneum, the occurrence of this tumour type is unusual. Mucinous cystadenomas are more commonly found in the pancreas and ovary and therefore the origin of mucinous cystadenomas in the retroperitoneum is widely debated.
One theory involves the seeding of ectopic ovarian tissue in the retroperitoneum.20 Primary retroperitoneal mucinous cystadenomas are histologically similar to mucinous cystadenomas found in the ovaries. Immunohistochemical analysis was found to have a positive match to cytokeratin 7 and cytokeratin 20 antibodies, an identical profile to ovarian mucinous tumours.21 However concomitant ovarian tissue has only been found in few cases.18 In addition PRMC has been previously reported as occurring in male patients.22
Another theory suggests development of a retroperitoneal teratoma with the proliferation of mucinous epithelium.23 Alternatively it is hypothesised that these tumours may arise from multi-potential mesothelial cells that become trapped in the retroperitoneum during embryonic development. These multi-potential cells undergo metaplasia to mucinous epithelium, creating the mucinous cysts with other malignant phenotypes.20,24
Consistent with the majority of previously reported PRMC our patient's presenting symptom was that of chronic abdominal pain. Prompt diagnosis of retroperitoneal tumours is important as the majority are malignant.1 The differential includes fibrosarcomas, liposarcomas, leiomyofibromas, leiomyosarcomas, malignant fibrous histiocytomas, neurofibromas and rhabdomyosarcomas. Therefore the diagnosis of a retroperitoneal tumour must be one of exclusion with radiological imaging or laparoscopy paramount.
Serological investigations are rarely of use in providing definitive diagnosis. Tumour markers such as carcinoembryonic antigen (CEA), carbohydrate antigen (CA) 19–9, CA 15–3, CA 125 and alpha feta protein have not been shown to be sensitive or specific. Previous cases have demonstrated an increase in CEA.2,3 Similarly it has been reported that an increased level of CA 19–9 is associated with PRMC.3,9 However these are isolated case studies. With regard to radiological investigation, ultrasonography lacks specificity.22 Computed topography (CT) of the area can be beneficial in differentiating between a cystic teratoma and cystadenoma through detection of calcification within the cyst. Overall MRI offers optimal description of the tumour in relation to soft tissue and radiological evidence of origin of the tumour.2 Laparoscopy and laparotomy can be utilised to provide both diagnostic and therapeutic roles. Radical resection is the treatment of choice.2
4. Conclusion
Our case presented typically for PRMC with regard to demographic features and presenting complaint. Primary retroperitoneal mucinous cystadenoma is a benign tumour, however because of the malignant nature of the majority of mucinous retroperitoneal tumours they should be considered in the differential of chronic abdominal pain despite their rarity.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Navin P wrote the content and worked along with Meshkat B in data collection and they teamed with all excepting Beegan C to review the work, yet Beegan and Leen endeavoured the preparation and analysis of histopathological sample.
References
- 1.Calo P.G., Congiou A., Ferreli C., Nikolosi A., Tarquin A. Primary retroperitoneal tumors. Our experience. Minerva Chirurgica. 1994;49:43–49. [PubMed] [Google Scholar]
- 2.Tapper E.B., Shrewsberry A.B., Oprea G., Majmudar B. A unique benign mucinous cystadenoma of the retroperitoneum: a case report and review of the literature. Archives of Gynecology and Obstetrics. 2010;281(January (1)):167–169. doi: 10.1007/s00404-009-1118-9. [Epub 2009 May 16] [DOI] [PubMed] [Google Scholar]
- 3.Del Gobbo A., Bimbatti M., Ferrero S. A case report of mesenteric mucinous cystoadenoma with review of the literature. BMC Gastroenterology. 2010;10(September):105. doi: 10.1186/1471-230X-10-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rifki Jai S., Bouffetal R., Chehab F., Khaiz D., Bouzidi A. Primary retroperitoneal mucinous cystadenoma. Archives of Gynecology and Obstetrics. 2009;280(September (3)):479–483. doi: 10.1007/s00404-008-0925-8. [DOI] [PubMed] [Google Scholar]
- 5.Abedalthagafi M., Jackson P.G., Ozdemirli M. Primary retroperitoneal mucinous cystadenoma. Saudi Medical Journal. 2009;30(January (1)):146–149. [PubMed] [Google Scholar]
- 6.Yan S.L., Lin H., Kuo C.L., Wu H.S., Huang M.H., Lee Y.T. Primary retroperitoneal mucinous cystadenoma: report of a case and review of the literature. World Journal of Gastroenterology. 2008;14:5769–5772. doi: 10.3748/wjg.14.5769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kassab A., El-Bialy G., Clark J., Callen P., Powary M., Jones H. Unusual presentation of 22-kilogram retroperitoneal mullerian serous cystadenoma. Gynecologic Oncology. 2007;104:257–259. doi: 10.1016/j.ygyno.2006.08.055. [DOI] [PubMed] [Google Scholar]
- 8.Min B.W., Kim J.M., Um J.W., Lee E.S., Son G.S., Kim S.J. The worst case of primary retroperitoneal mucinous cystadenoma in Korea: a case report. Korean Journal of Internal Medicine. 2004;19(4):282–284. doi: 10.3904/kjim.2004.19.4.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Isse K., Harada K., Suzuki Y., Ishiguro K., SasaKi M., Kajiura S. Retroperitoneal mucinous cystadenoma: report two cases and review of literature. Pathology International. 2004;54:132–138. doi: 10.1111/j.1440-1827.2004.01595.x. [DOI] [PubMed] [Google Scholar]
- 10.Arribas D., Cay A., Latorre A., Còrdoba E., Martìnez F., Lagos J. Retroperitoneal mucinous cystadenoma. Archives of Gynecology and Obstetrics. 2004;270(4):292–293. doi: 10.1007/s00404-003-0515-8. [DOI] [PubMed] [Google Scholar]
- 11.Tamura T., Yamataka A., Murakami T., Okada Y., Kobayashi H., Ohshiro K. Primary mucinous cystadenoma arising from behind the posterior peritoneum of the descending colon in a child: a case report. Asian Journal of Surgery. 2003;26(4):237–239. doi: 10.1016/S1015-9584(09)60313-4. [DOI] [PubMed] [Google Scholar]
- 12.Erdemoglu E., Aydogdu T., Tokyol C Primary retro peritoneal mucinous cystadenoma. Acta Obstetricia et Gynecologica Scandinavica. 2003;82(5):486–487. doi: 10.1034/j.1600-0412.2003.00158.x. [DOI] [PubMed] [Google Scholar]
- 13.Balat O., Aydin A., Sirikci A., Kutlar I., Aksoy F. Huge primary mucinous cystadenoma of the retroperitoneum mimicking a left ovarian tumor. European Journal of Gynaecological Oncology. 2001;22:454–455. [PubMed] [Google Scholar]
- 14.Subramony C., Habibpour S., Hashimoto L.A. Retroperitonealmucinous cystadenoma. Archives of Pathology and Laboratory Medicine. 2001;125:691–694. doi: 10.5858/2001-125-0691-RMC. [DOI] [PubMed] [Google Scholar]
- 15.Kehagias D.T., Karvounis E.E., Fotopoulos A., Gouliamos A.D. Retroperitoneal mucinous cystadenoma. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 1999;82:213–215. doi: 10.1016/s0301-2115(98)00254-1. [DOI] [PubMed] [Google Scholar]
- 16.Yunoki Y., Oshima Y., Murakami I., Takeuchi H., Yasui Y., Tanakaya K. Primary retroperitoneal cystadenoma. Acta Obstetricia et Gynecologica Scandinavica. 1998;77:357–358. [PubMed] [Google Scholar]
- 17.Park U., Han K.C., Chang H.K., Huh M.H. A primary mucinous cystoadenocarcinoma of the retroperitoneum. Gynecologic Oncology. 1991;42:64–67. doi: 10.1016/0090-8258(91)90232-t. [DOI] [PubMed] [Google Scholar]
- 18.Pennell T.C., Gusdon J.P., Jr. Retroperitoneal mucinous cystadenoma. American Journal of Obstetrics and Gynecology. 1989;160:1229–1231. doi: 10.1016/0002-9378(89)90201-9. [DOI] [PubMed] [Google Scholar]
- 19.Handfield Jones R. Retroperitoneal cysts: their pathology, diagnosis, and treatment. British Journal of Surgery. 1924;12:119–134. [Google Scholar]
- 20.Matsubara M., Shiozawa T., Tachibana R., Hondo T., Osasda K., Kawaguchi K. Primary retroperitoneal mucinous cystadenoma of borderline malignancy: a case report and review of the literature. International Journal of Gynecological Pathology. 2005;24:218–223. doi: 10.1097/01.pgp.0000161313.30054.1d. [DOI] [PubMed] [Google Scholar]
- 21.Lai K.K.T., Chan Y.Y.R., Chin A.C.W., Ng W.F., Huang Y.H.H., Mak Y.L.M. Primary retroperitoneal mucinous cystadenoma in a 52-year-old man. Journal of Hong Kong College of Radiologists. 2004;7:223–225. [Google Scholar]
- 22.Lai K.K.T., Chan Y.Y.R., Chin A.C.W., Ng W.F., Huang Y.H.H., Mak Y.L.M. Primary retroperitoneal mucinous cystadenoma in a 52-year-old man. Journal of Hong Kong College Of Radiologists. 2004;7:223–225. [Google Scholar]
- 23.Papadogiannakis N., Gad A., Ehliar B. Primary retroperitoneal mucinous tumor of low malignant potential: histogenetic aspects and review of the literature. Acta Pathologica, Microbiologica et Immunologica. 1997;105:483–486. doi: 10.1111/j.1699-0463.1997.tb00597.x. [DOI] [PubMed] [Google Scholar]
- 24.Fujii S., Konishi I., Okamura H., Mori T. Mucinous cystadenocarcinoma of the retroperitoneum: a light and electron microscopic study. Journal of Gynaecological Oncology. 1986;24:103–112. doi: 10.1016/0090-8258(86)90013-2. [DOI] [PubMed] [Google Scholar]


