Abstract
Objectives:
To evaluate the effect of Hip Hop Stroke, a school-based multimedia musical stroke literacy intervention that targets children aged 8−12 in high-risk minority communities, on the long-term learning of stroke knowledge.
Methods:
We enrolled a cohort of 104 fifth and sixth grade children from 2 schools in Central Harlem into a single course of Hip Hop Stroke (3 1-hour classroom sessions, delivered over 3 consecutive days). Tests evaluating knowledge of stroke symptoms and behavioral intent to call 911 using hypothetical stroke scenarios were conducted at baseline, immediately after the intervention, and 15 months after the initial and only intervention. A composite score was created from 5 traditional stroke symptoms plus a distracter (chest pain). Data were analyzed using SAS version 9.2.
Results:
A total of 104 students completed both pretests (PTs) and immediate posttests (IPs), and 85 students completed all 3 tests, including a 15-month delayed posttest (DP) (81.7% retention rate). At pretest, 55.8% correctly identified calling 911. The baseline composite score was 3.24 (SD 1.45). At IP, stroke knowledge increased significantly across all items: calling 911 (85.6%, p < 0.001) and composite score (5.30, p < 0.0001). At 15 months, stroke knowledge increased significantly from PT for all measures except sudden headache with a composite score of 4.73 (p < 0.0001, PT vs DP).
Conclusion:
Three hours of Hip Hop Stroke significantly improved knowledge of stroke symptoms and behavioral intent to call 911 of fifth and sixth grade children living in a high stroke risk neighborhood. This learning persisted for up to 15 months postintervention.
Bystanders and family members, including children, play a role in calling 911 for suspected stroke.1 Programs targeting children may equip them with the ability to recognize stroke symptoms and call 911,1–3 but long-term follow-up data are scarce. Interventions have engaged elementary and middle school children, with program follow-up duration ranging from 10 days4 to 2 months.5 To date, the longest running program targeting children provided a total of 12 hours of classroom instruction over 3 years,6 and although long-term stroke knowledge of the children measured at least 3 and 9 months after the final curriculum session was favorable, no follow-up data on parental knowledge was provided because of poor response rates.
Our group has developed Hip Hop Stroke (HHS), which uses hip hop music and multimedia tools (cartoons, comic books, and video games) to educate children about stroke and also their parents through assigned homework activities brought home by their children. In prior studies, we demonstrated the efficacy of HHS to improve knowledge of the children at 3 months2 and of their parents 1 week after the intervention period.3 In this study, we hypothesized that stroke knowledge among children will be retained 15 months after the completion of the curriculum.
METHODS
Study design.
We compared group level test scores on stroke knowledge domains before, immediately after, and 15 months after the intervention. We did not contact the students during this 15-month period, and the students were not forewarned of our return. All data collected were anonymous. This study was approved by the Columbia University institutional review board.
Setting.
We enrolled a convenience sample of 104 fifth and sixth grade students aged 9–12 years from 2 public schools in Central Harlem, New York, an economically disadvantaged, high stroke risk community. Of the students, 75% were non-Hispanic black and 25% were Hispanic; 67% fulfilled federal poverty criteria required to be eligible for free meals in school.
Intervention.
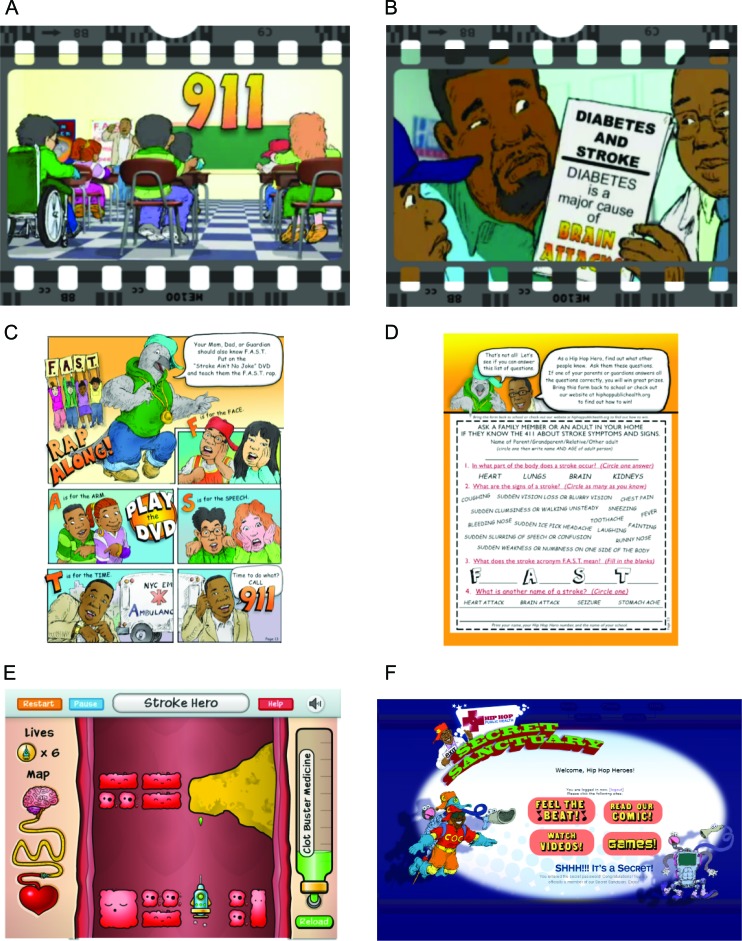
HHS is a multimedia stroke literacy intervention based on validated theoretical models of behavior change that targets children aged 9−12 and their parents through what we have called Child-Mediated Stroke Communication,1,2 involving specific homework activities designed for child-parent engagement. The curriculum is delivered in3 1-hour assembly-setting sessions administered over 3 consecutive days. HHS uses rap music, cartoons, a video game, a comic, and role-play to teach children to recognize stroke symptoms and take urgent action. Multimedia can be viewed at http://hiphoppublichealth.org/HHS_Educational_Tools. Homework activities include reading a stroke comic and completing a quiz with a parent and playing a stroke video game in a password-protected online Secret Sanctuary that children are given access to, where they can view cartoons and download stroke-relevant rap songs (figure 1). Theoretical underpinnings of HHS are based on 2 theories demonstrated to be important predictors of behavior change: self-efficacy theory,7 which posits feedback loops that increase children's confidence in their mastery of understanding stroke symptoms, and reasoned action theory,8 which suggests that a series of related cognitive constructs operate to produce an intention to act, serving as a precursor to the desired outcome (that is, making use of stroke information as part of standard practice). These constructs, when presented to children in the context of a systematic intervention, take advantage of their potential role in the health management family structure and of promoting their self-perception as agents of change in this regard.
Figure 1. Multimedia.
(A) Scene from “Stroke Ain't No Joke” stroke recognition animated cartoon video. (B) Scene from “Keep Your Brain Healthy” stroke prevention animated cartoon video. (C) Excerpt from “Stroke Ain't No Joke” stroke recognition comic book. (D) “Stroke Ain't No Joke” stroke recognition comic book homework quiz. (E) Screen shot from Clotbuster stroke video game. (F) Password protected Secret Sanctuary at http://www.hiphoppublichealth.org.
Assessments.
Baseline surveys evaluated stroke knowledge using multiple-choice questions, and stroke action (calling 911) was assessed using hypothetical stroke scenarios. Testing was conducted at baseline (pretest [PT]), immediately after the intervention (immediate posttest [IP]), and 15 months after the intervention (delayed posttest [DT]). Only children who acknowledged participating in the initial HHS program were enrolled in the DP. A composite score was created by counting the number of correct responses to the traditional 5 stroke symptoms (except that facial weakness was taught in the context of unilateral weakness) and a distracter (chest pain) (maximum score = 6). Wireless audience response systems given to each child were used for data collection and rapid analysis of group level test performance.
Statistical analysis.
Descriptive statistics were prepared for all responses to questions using frequencies and percentages. The composite score was summarized using a mean and SD. Comparisons between PT and IP, PT and DT, or IP and DP were made using independent samples testing methods because pretests and posttests were not tracked at the individual level. We imputed missing responses as incorrect. χ2 tests were used for all comparisons except the composite score for which a two-sample t test was used. All analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
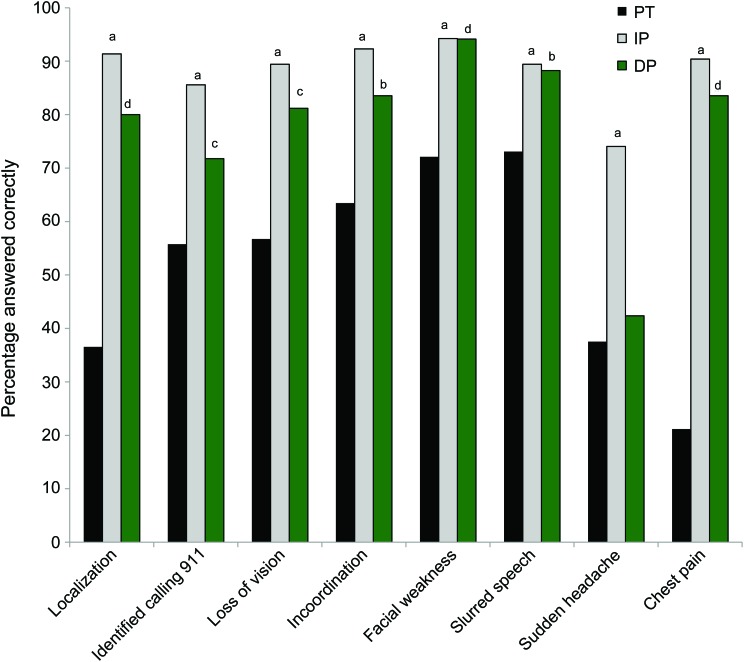
A total of 104 students completed the PT and IP; 85 students completed all 3 measures, which included a 15-month DP (81.7% retention rate). Responses to questions are summarized in figure 2. We had a missing data rate of 8.5%. The baseline composite score was 3.2 (SD 1.5). At IP, stroke knowledge increased significantly across all items: stroke localization (91.4%, p < 0.0001), calling 911 (85.6%, p < 0.001), and composite score (5.3, SD 1.0, p < 0.0001) (table). At DP, the composite score was 4.7 (SD 1.1), which was a significant increase from pretest (p < 0.0001, PT vs DP), and knowledge of stroke localization (80.0%, p < 0.0001, PT vs DP) also increased significantly from pretest. Stroke knowledge was retained for all measures except sudden headache, decreasing by less than 15% from IP to 15-month DP, and the composite score decreased by less than 1 point (table).
Figure 2. Frequency of correct stroke knowledge responses.
Pretest (PT) vs immediate posttest (IP, 3 days): ap < 0.001; PT vs delayed posttest (DP, 15 months): bp < 0.05, cp < 0.01, dp < 0.001; PT vs IP and PT vs DP: p values are based on χ2 tests.
Table.
Responses to stroke knowledge questions across the entire testing sequence
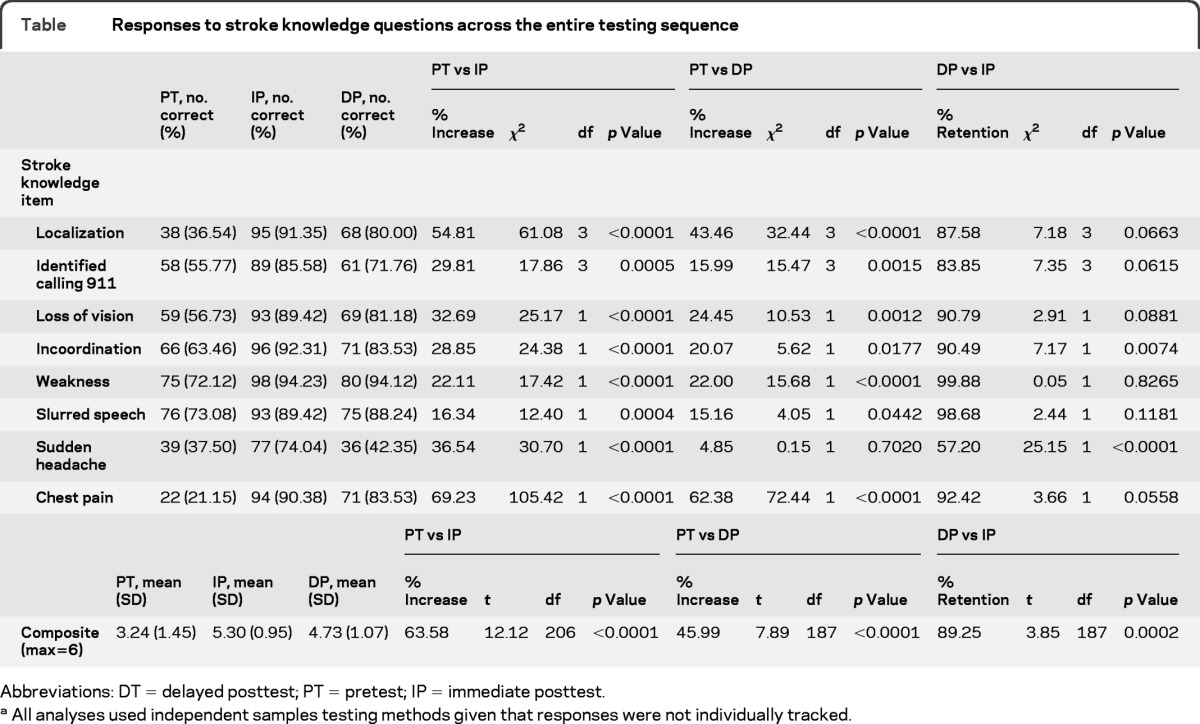
Abbreviations: DT = delayed posttest; PT = pretest; IP = immediate posttest.
All analyses used independent samples testing methods given that responses were not individually tracked.
DISCUSSION
In this study, we show that 9- to 12-year-old students living in a high stroke risk community can learn and retain stroke knowledge for up to 15 months after a brief 3-hour intervention. Our findings suggest that 1) the HHS intervention had a strong positive effect on the target group in terms of learning and retention and 2) a 3-hour per year frequency of the intervention incorporated into a school health education curriculum may be sufficient to maintain meaningful stroke knowledge over the long term. To the best of our knowledge, our results represent the longest postintervention follow-up stroke knowledge assessment among young children published to date.
Our study had several limitations. Knowledge is necessary but may not be sufficient to enact behaviors such as calling 911 immediately in the event of a stroke. The use of closed-ended questions may have influenced some responses, particularly behavioral intent to call 911. Analyses were performed at the group level and not at the individual level because we did not track individuals across the testing sequence. We found less retention of headache as a stroke symptom, which may be related to the ubiquitously benign nature of this symptom and the relative lack of emphasis on headache in our song lyrics, video game, and stroke cartoons. Finally, our study sample was small, and we used a pretest-posttest nonrandomized design without a control group. We were unable to control for the possible exposure to other local stroke campaigns during the study period, although our group was not aware of such activities in Central Harlem.
Taken together with our group's prior work,2,3 a 3-hour HHS curriculum divided into 1-hour classes and repeated annually in a school setting may represent a useful strategy for maintaining the awareness of stroke symptoms and their urgency among low-income children and their parents.
ACKNOWLEDGMENT
The authors thank our Hip Hop Stroke Master Trainers, Adrian Harris and Tiffany Denise Newton, our resident artists Doug E. Fresh and Artie Green, and Electric Black Experience for the production of our multimedia materials.
GLOSSARY
- DP
delayed posttest
- HHS
Hip Hop Stroke
- IP
immediate posttest
- PT
pretest
AUTHOR CONTRIBUTIONS
O. Williams: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, acquisition of data, statistical analysis, study supervision, obtaining funding. A. DeSorbo: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, acquisition of data. J. Noble: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, study supervision. M. Shaffer: analysis or interpretation of data, statistical analysis. W. Gerin: drafting/revising the manuscript, analysis or interpretation of data.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1. Morgenstern LB, Rosamond W, Alberts MJ, et al. Increasing Public Recognition and Rapid Response to Stroke: A National Institute of Neurological Disorders and Stroke Symposium: Improving the Chain of Recovery for Acute Stroke in Your Community. Bethesda, MD: National Institutes of Health, Department of Health and Human Services, Office of Communications and Public Liaison, National Institute of Neurological Disorders and Stroke; 2003:1–9 [Google Scholar]
- 2. Williams O, Noble JM. ‘Hip-hop' stroke: a stroke educational program for elementary school children living in a high-risk community. Stroke 2008;39:2809–2816 [DOI] [PubMed] [Google Scholar]
- 3. Williams O, DeSorbo A, Noble JM, Gerin W. Child-Mediated Stroke Communication: findings from the Hip Hop Stroke program. Stroke 2012;43:163–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dressman LA, Hunter J. Stroke awareness and knowledge retention in children: the Brain Child Project. Stroke 2002;33:623–625 [DOI] [PubMed] [Google Scholar]
- 5. Miller ET, King KA, Miller R, Kleindorfer D. Fast stroke prevention educational program for middle school students: pilot study results. J Neurosci Nurs 2007;39:236–242 [DOI] [PubMed] [Google Scholar]
- 6. Morgenstern LB, Gonzales NR, Maddox KE, et al. A randomized, controlled trial to teach middle school children to recognize stroke and call 911: the KIDS identifying and defeating stroke project. Stroke 2007;38:2972–2978 [DOI] [PubMed] [Google Scholar]
- 7. Allen NA. Social cognitive theory in diabetes exercise research: an integrative literature review. Diabetes Educ 2004;30:805–819 [DOI] [PubMed] [Google Scholar]
- 8. Fishbein M. A reasoned action approach to health promotion. Med Decis Making 2008;28:834–844 [DOI] [PMC free article] [PubMed] [Google Scholar]