Abstract
Appropriate measurement of socioeconomic status (SES) in health research can be problematic. Conventional SES measures based on ‘objective’ indicators such as income, education, or occupation may have questionable validity in certain populations. The objective of this investigation was to determine if a relatively new measurement of SES, subjective social status (SSS), was more consistently and strongly associated with multiple health outcomes for low income mothers. Data available from a large scale community-based study examining maternal and infant health for a low income urban population were used to examine relationships between SSS and a wide range of postpartum physical and emotional health outcomes. Crosstabulations and multivariate analyses focused on the breadth and depth of these relationships; in addition, the relative strength of the relationships between SSS and the health outcomes was compared to that of conventional measures of SES, including both income and education. SSS was significantly related to all physical and emotional health outcomes examined. The overall pattern of findings indicated that these relationships were independent of, as well as more consistent and stronger than, those between conventional measures of SES and postpartum health outcomes. SSS represents an important dimension of the relationship between SES and postpartum physical and emotional health. In low income populations the failure to account for this dimension likely underestimates the influence of SES on postpartum health. This has important implications for the interpretation of findings in empirical studies which seek to control for the effects of SES on maternal health outcomes.
Keywords: Subjective social status, Socioeconomic status, Maternal health outcomes, Postpartum health, Low-income mothers
Introduction
The relationship between low socioeconomic status (SES) and poor health outcomes has been extensively documented through empirical research [1]. The nature of this relationship is, however, highly complex and the precise mechanisms through which SES translates into health disadvantages (for low SES persons) or advantages (for higher SES persons) are not fully understood [2, 3]. One problem is that one’s adult health status may reflect SES-related risk or protective factors which are cumulative in terms of their effects [4–6]. Thus point-in-time indicators of adult SES such as income and educational attainment may not adequately reflect the influences shaped by one’s SES during childhood, which either persisted or changed during the life course [7, 8]. Other influences associated with SES may be difficult to quantify, including homeownership, indebtedness, family wealth, and dynamics operating at the community level such as one’s network of social relationships [3, 9–11].
For the above-mentioned reasons, conventional indicators of SES (which typically refer to income, occupation, and/or educational attainment) may have poor construct validity, highlighting the need for a more critical and careful consideration of how SES is defined and measured in the context of health research [2, 12–14]. Some studies have demonstrated a significant relationship between SES and adult health when measures of SES are based on perceived social ranking, and that one’s perceived status may provide a better conceptual/measurement framework for exploring the associations between adult SES and health outcomes [9, 10, 15]. This may be, in part, because subjective measures are arguably ‘global’ in nature and account for one’s understanding of the stability of their social status, as well as for the prospects of social mobility, while ‘point-in-time’ measures, for example, do not. [10, 15]
Consistent with findings from adult and child health research, low maternal SES has been shown to be persistently and pervasively related to adverse pregnancy and birth outcomes [16–18]. However, we are aware of only one published study that examined the relationship between SES and maternal health, defining SES in terms of a woman’s perceived or subjective social status (SSS) [19]. In that study women who perceived their status as relatively low were found to be in relatively poor health, independent of their income and educational attainment. Moreover, among some ethnic groups, perceived status was reported to be more strongly related to maternal health than income and education. The study was, however, limited to only one measure of maternal health—namely, a woman’s overall self-rated health status during pregnancy. The purpose of our investigation was [1] to assess the extent to which subjective social status is related to a wide variety of maternal health-related outcomes; and [2] to compare and contrast the magnitude of the relationship between subjective social status and maternal health outcomes to conventional measures of SES and maternal outcomes.
Methods
This research was part of a larger, prospective, community-based study examining maternal stress, birth outcomes, and maternal and infant health and health-related behaviors. The study involved recruitment of women who first enrolled for prenatal care at a consortium of six community health centers in Philadelphia, Pennsylvania, between February 2000 and November 2002. It was funded by the Centers for Disease Control and the National Institute for Child Health and Human Development and review for the ethical treatment and study of human subjects was approved by the institutional review boards (IRBs) at Thomas Jefferson University, Drexel University and the University of Pennsylvania. Subject consent was obtained through signed consent forms. Additional findings from, and more details about, the larger study are available elsewhere [20, 21].
Women were recruited and interviewed at the time of prenatal care enrollment, and scheduled for three follow-up surveys in the subjects’ homes, at approximately 3 months postpartum, 11 months postpartum, and at 24 months postpartum. Only information from the prenatal, 3 month, and 11 month postpartum interviews was used for the purposes of this study.
Women with a singleton intrauterine pregnancy who spoke either English or Spanish were considered eligible for enrollment; among those, women with pregnancies ending in a live birth were designated for postpartum follow-up (n = 2,026). More than 98% (n = 1,984) agreed to participate in the follow-up phase of the study, and attempts to complete both the 3 month and 11 month postpartum surveys were successful for 67% (n = 1,322) of those who did agree. Data from the prenatal interviews indicated that women who did not complete the first two postpartum interviews (n = 562) did not differ from those who did with respect to income, education, marital status, or parity (data not shown).
All interviews were based on structured surveys, conducted in English or Spanish by trained female interviewers. To minimize the chances of interviewer bias or misinformation each interviewer received approximately 30 h of training in use of this instrument, including instruction on when and when not to prompt women for responses, and how to explain the meaning of a question should any misunderstanding arise. The training included role playing and each interviewer was assessed and rated as competent by an experienced project supervisor before assignment to the field. For quality control purposes, a ten percent random sample consisting of 10% of all interviews from each interviewer were reviewed. Weekly meetings were held with the interviewers, project staff, and principal investigator (Dr. Jennifer Culhane) to discuss any issues related to the interviewing process.
Study Variables
Preliminary analyses of the data indicated that t he relationships between the health outcomes of interest and three primary measures of social status (SSS, income and education) were ordinal and non-linear in nature. For that reason women were ranked as either being of ‘low’’, ‘medium’ or ‘high’ for each variable, as described below.
Subjective Social Status
The surveys conducted at 11 months postpartum included the MacArthur Scale of Subjective Social Status, a measure which has been shown to be a valid and reliable indicator of one’s perceived status in society [22]. Specifically women were presented with a “social ladder” with 10 rungs and were asked to rank themselves by placing an “X” on the step they felt represented their relative position in society at large. Each rung was numbered and the women were read the following statement: “In our society, at the top, are those who have the most money, education and best jobs; at the bottom are those that have the worse jobs or no jobs. Where do you think you fit in?” Their self-rank on this ladder, ranging from 1–10 was used as the basis for our measure of subjective social status (SSS). Women with a ladder score of 0 through 3 were classified as being in the ‘low’ SSS group; those with a score of 4 through 7 as being in the ‘medium’ SSS group; and those with a score of 8 through 10 as being in the ‘high’ SSS group. The distribution of SSS was approximately normal with a mean value of 5.9 and standard deviation of 1.85. The abovementioned cut-offs for ‘low’ and ‘high’ groups represent scores that were approximately 1.5 standard deviations below the mean and 1.5 standard deviations above the mean of 5.9, respectively. All others between 1.5 standard deviations above and below the mean were classified as being in the ‘medium’ SSS group.
Objective Indicators of Social Status
Several measures of the respondents’ objective indicators of socioeconomic status were used in the analyses. The major indicators were educational attainment and personal income. Income was determined based on response to the question in the 11 month postpartum survey, which appeared as follows: “What is the total amount of money you received from all sources during a typical month?” Respondents were classified based on quartile rankings. Specifically, those in the first quartile of the income distribution for the sample (<$500 per month) were categorized as being the low income group; those in the second or third quartiles were categorized as the ‘medium’ income group ($500–$1200 per month), and those in the highest quartile ([>$1200 per month) were categorized in the ‘high’ income group.
Educational attainment was measured in number of years of education, collected at the time of the initial interview along with other descriptive sociodemographic characteristics such as age, race/ethnicity, and parity. Women were grouped into three categories in terms of their education attainment: low (did not complete high school), medium (completed high school) and high (some college or more). Other variables representing measures of objective social standing that were included in the analyses were public assistance status (on food stamps or state cash welfare payments), homelessness (ever experiencing homelessness since childbirth) and ever having an involuntary utility (water, gas or electric) shut-off.
Health Outcomes
Several measures related to both the mental and physical health of respondents were available from one or both of the surveys and used as the dependent variables in the analyses. They included overall self rated physical and emotional health during pregnancy (reported by respondents at the 3 month postpartum interview) and overall physical and emotional health in the postpartum period (reported by respondents at the 11 month postpartum interview).
All self reported measures of physical and emotional health were dichotomized, with respondents classified as being in relatively good (reporting ‘excellent’, ‘very good’, or ‘good’) as opposed to relatively poor (reporting only ‘fair’ or ‘poor’) health. Other measures of emotional health during the postpartum period used in the analyses included depressive symptomatology and perceived stress (reported at the 11 month interview). Depressive symptomatology was defined as a score of greater than or equal to 23 on the Center for Epidemiological Studies Depression Scale (CES-D). The CES-D is a pre-tested reliable and valid instrument used widely in studies of depression, including postpartum depression; scores of greater than or equal to 23 correspond to the 90th percentile in community samples and has been used by other researchers to define the presence of depressive symptoms in pregnant and postpartum women [23, 24]. Perceived stress was based on the administration of the Cohen Perceived Stress Scale (PSS). The PSS possesses strong psychometric properties, including reliability across gender, socioeconomic status, age groups, race/ethnicity, and other demographic characteristics [25]. This 14 item self report scale measures the degree to which a respondent appraises her life as being stressful. Women scoring below the 75th percentile (<28) were defined as having relatively low stress while those equal to and above that were classified as the relatively “high stress” group. In addition, women were classified in terms of whether or not they had one or more major health problems (heart disease, asthma, diabetes, or high blood pressure) and whether or not they had ever been told by a health professional that their pregnancy was ‘high risk.’ Additional data describing the health outcomes used as the independent variables in the analyis are available from the authors upon request.
Statistical Analyses
We first used simple cross tabulation techniques to examine and compare the relationships between all health outcomes and SSS, education, and income. Goodman and Kruskal’s gamma was used to determine statistical significance, magnitude and direction of all relationships. Gamma is based on the correspondence among the rank ordering of observations for any pair of variables ordinal in nature, and is appropriate whenever the relationships are likely or purported to be ordinal, as is the case here. Gamma values are themselves both measures of the degree and strength of the ordinal relationships and are normally distributed for large sample sizes, and thus the calculation of P values is straightforward [26].
Logistic regression (LR) was then used to explore the effects of SSS vs. income, education, and other measures of SES described above on the health outcome variables. Specifically, a series of LR models were created with SSS, and additional SES indicators were entered in a stepwise fashion. In this way, the strength and robustness of the effects of SSS on health, independent of and in contrast to other measures could be quantified by comparing adjusted odds ratios. Confidence intervals associated with all effect parameters were also calculated and are presented in the tables and figures that follow. All analyses were completed using Stata 10.0 [27].
Results
The sociodemographic and health characteristics of the study population are shown in Table 1. African-Americans comprised 70.6%, Whites 9.8%, and Hispanics 16.5% of the 1,322 women for whom the three surveys were available. The age range for this cohort was 13–43 years, with a mean age of 23.9 years. Almost 40% (39.3%) of the women did not graduate from high school, while 17.7% received at least some post high school education. Almost 65% (64.8%) of the women reported a total income of less than $1200 per month. More than 90% (93.6%) of the women reported receiving public assistance. More than 5% (5.2%) indicated that they had experienced a utility shutoff and over 2% (2.6%) reported being homeless at some point since their last childbirth. The distribution of the Subjective Social Status scale indicated that the vast majority of respondents perceived themselves to be average, despite median incomes ($800/month) well below that for the U.S. as a whole. Specifically, more than 7 out of ten (71.9%) placed themselves close to the middle (rung scores from 4 to 7) of the subjective status ladder.
Table 1.
Descriptive characteristics of the study population
| Number (percent) | |
|---|---|
| All women | 1322 (100%) |
| Race/ethnicity | |
| Non-Hispanic White | 130 (9.8) |
| Non-Hispanic Black | 933 (70.6) |
| Hispanic | 218 (16.5) |
| Asian/other | 41 (3.1) |
| Age | |
| <17 years | 89 (6.7) |
| 18–24 | 727 (54.9) |
| 25–29 | 282 (21.3) |
| 30–34 | 144 (10.9) |
| 35+ | 80 (6.1) |
| Personal income | |
| Low ($500/month) | 353 (26.6) |
| Medium ($501–<1200/month) | 505 (38.2) |
| High (≥$1200/month) | 372 (28.1) |
| Subject unable to report | 93 (7.0) |
| Education | |
| Low (<HS) | 519 (39.3) |
| Medium (HS/GED) | 568 (43.0) |
| High (post HS) | 234 (17.7) |
| Receiving public assistance | |
| Yes | 1238 (93.6) |
| Homeless since child’s birth | |
| Yes | 34 (2.6) |
| Experienced utility shut-off | |
| Yes | 69 (5.2) |
| Subjective social | |
| Status ladder | |
| 0 | 17 (1.3), Low |
| 1 | 11 (0.8), Low |
| 2 | 32 (2.4), Low |
| 3 | 77 (5.8), Low |
| 4 | 123 (9.3), Medium |
| 5 | 371 (28.1), Medium |
| 6 | 261 (19.7), Medium |
| 7 | 196 (14.8), Medium |
| 8 | 144 (10.9), High |
| 9 | 45 (3.4), High |
| 10 | 45 (3.4), High |
| Age: mean (SD) | 23.9 (5.9) |
| Median income$ | 800 |
The relationships between subjective social status, income, and education with each of the health outcome variables are provided in Table 2. In general the associations between SSS and health are strong and persistent. Relatively poor overall physical and emotional health during pregnancy, the presence of major health problems, perceived stress and depressive symptomatology are all significantly and inversely related to SSS. For example, compared to women who rated themselves high on the SSS scale, those who rated themselves in the lowest category were more than twice as likely to report their overall physical health during pregnancy (24.6 vs. 11.4%), and their emotional health in the postpartum period (31.4 vs. 14.1%) to be relatively poor. Consistent with these overall self-reported items, women in the lowest compared to highest SSS group were more likely to have indicated one or more major health problems (45.6 vs. 30.8%), far more likely to be in the high stress category (50.4 vs. 20.9%) and to have depressive symptomatology (32.9 vs. 15.4%).
Table 2.
Relationship between heath outcomes and subjective social status (SSS), income, and education (GAMMA = γ)
| N (%) | SSS |
Income |
Income |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | Medium | High | γ | Low | Medium | High | γ | Low | Medium | High | γ | ||
| All women | 1,322 (100%) | ||||||||||||
| Physical health | |||||||||||||
| Overall during pregnancy only fair or poor | 207 (18.1) | 29 (24.6) | 155 (18.8) | 23 (11.4) | −0.25*** | 53 (17.4) | 79 (18.2) 5 | 58 (18.4) | 0.02 | 85 (18.9) | 90 (18.3) | 32 (15.9) | −0.05 |
| Overall postpartum: only fair or poor | 183 (14.1) | 26 (19.7) | 132 (14.1) | 25 (10.9) | −0.18* | 51 (14.9) | 70 (14.0) 5 | 50 (13.8) | −0.03 | 88 (17.5) | 63 (11.2) | 31 (13.5) | −0.15* |
| Emotional health | |||||||||||||
| Overall during pregnancy: only fair or poor | 405 (35.0) | 54 (45.8) | 297 (36.1) | 54 (26.9) | −0.22*** | 85 (27.9) | 172 (39.7) | 116 (36.7) | 0.12* | 166 (37.1) | 162 (32.9) | 77 (38.3) | −0.01 |
| Overall postpartum: only fair or poor | 235 (17.8) | 43 (31.4) | 159 (16.8) | 33 (14.1) | −0.26*** | 63 (17.9) | 105 (20.9) | 46 (12.4) | −0.13* | 120 (23.2) | 78 (13.8) | 36 (15.4) | −0.22*** |
| Additional measures of physical health | |||||||||||||
| One or more major health problems | 480 (36.4) | 62 (45.6) | 346 (36.5) | 72 (30.8) | −0.16*** | 117 (33.3) | 188 (37.4) | 134 (36.1) | 0.04 | 202 (39.1) | 209 (36.9) | 69 (29.5) | −0.11* |
| High risk pregnancy | 367 (27.9) | 42 (30.7) | 273 (29.0) | 52 (22.2) | −0.13* | 77 (22.3) | 152 (30.1) | 112 (30.2) | 0.12* | 139 (26.9) | 155 (27.5) | 73 (31.3) | 0.05 |
| Additional measures of emotional l health | |||||||||||||
| Perceived stress: high | 380 (28.8) | 69 (50.4) | 262 (27.6) | 49 (20.9) | −0.33*** | 124 (35.2) | 153 (30.4) | 74 (19.9) | −0.24*** | 178 (34.4) | 142 (25.0) | 60 (25.6) | −0.17*** |
| Depressive symptoms | 245 (18.6) | 45 (32.9) | 164 (17.3) | 36 (15.4) | −0.24*** | 70 (19.9) | 103 (20.4) | 50 (13.3) | −0.14* | 126 (24.3) | 88 (15.5) | 31 (13.3) | −0.26*** |
p-value < 0.05,
p-value < 0.01,
p-value < 0.005
Income and education were inversely related to some of the health outcomes, although not as strongly or as consistently as was the case for SSS. Physical health during pregnancy was unrelated to either income or education, while overall physical health was related to education but not to income. Overall emotional health in the postpartum period was related to both income and education, but overall emotional health during pregnancy was related only to income. As was the case for SSS, perceived stress and depressive symptomatology were related to both income and education, although the relationships were somewhat stronger for SSS.
The results from the logistic regression analyses are presented in Tables 3 and 4. Models A, B and C show the unadjusted odds ratios for SSS, Income and Education, respectively. Model D presents the odds ratios adjusted for income and education; and in Model E the odds ratios are adjusted for all additional measures of social status. Presenting the results in this manner allows us to compare the relative strength and robustness of the relationship between SSS and high stress (Table 3) and self-rated poor physical health (Table 4), when all other measures of SES are taken into account. As we can see in Table 3, the relationship between SSS and high stress is strong and persistent even after accounting for objective SES measures. Women in the low SSS category were far more likely than women in the highest category to have high stress levels, even after controlling for income and education (OR 3.66; 95% CI 2.25, 5.95). Even after adjusting for all other SES measures those in the low SSS category were still far more likely than those in the highest category to have high stress levels (OR 3.24; 95% CI 1.98, 5.30). Note that after adjusting for SSS, education is unrelated to high stress and income is only weakly related. Women in the lowest income group were somewhat more likely to have high stress levels compared to women with the most income after adjusting for SSS (OR 1.87; 95% CI 1.31, 2.68), but the effect size is considerably smaller than that for SSS.
Table 3.
Logistic regression results: relationships between SSS, income, education, selected measures of impoverishment and high stress levelsa
| Model A | Model B | Model C | Model D | Model E | |
|---|---|---|---|---|---|
| SSS | |||||
| High | 1.0 | 1.0 | 1.0 | ||
| Medium | 1.44 (1.02, 2.03) | 1.53 (1.06, 2.21) | 1.42 (0.98, 2.06) | ||
| Low | 3.83 (2.42, 6.07) | 3.66 (2.25, 5.94) | 3.24 (1.98, 5.30) | ||
| Income | |||||
| High | 1.0 | 1.0 | 1.0 | ||
| Medium | 1.75 (1.28, 2.41) | 1.57 (1.13, 2.17) | 1.51 (1.08, 2.12) | ||
| Low | 2.19 (1.57, 3.06) | 1.92 (1.35, 2.72) | 1.87 (1.31, 2.68) | ||
| Educ: | |||||
| High | 1.0 | 1.0 | 1.0 | ||
| Medium | 0.97 (0.68, 1.37) | 0.94 (0.65, 1.37) | 0.94 (0.64, 1.37) | ||
| Low | 1.52 (1.08,2.14) | 1.27(0.87, 1.86) | 1.22(0.83, 1.79) | ||
| Utility shut-off | |||||
| No | 1.0 | ||||
| Yes | 1.96 (1.16, 3.32) | ||||
| Public assistance | |||||
| No | 1.0 | ||||
| Yes | 2.13 (0.98,4.60) | ||||
| Homeless | |||||
| No | 1.0 | ||||
| Yes | 3.11(1.45, 6.69) | ||||
| Model p-values | <.0001 | <.0001 | <.005 | <.0001 | M.0001 |
Note: Multicollinearity associated among all variables shown was assessed using the variance inflation factor (VIF). The average VIF was less than 1.5, with a maximum value of 2.1
Dependent variable is high stress score (at or above the 75th percentile on Cohen perceived stress scale) vs. others
Table 4.
Logistic regression results: relationships between SSS, income, education, selected measures of impoverishment, and mother’s overall physical healtha
| Model A | Model B | Model C | Model D | Model E | |
|---|---|---|---|---|---|
| SSS | |||||
| High | 1.0 | 1.0 | 1.0 | ||
| Medium | 1.34 (0.85, 2.12) | 1.34 (0.83, 2.16) | 1.28 (0.80, 2.07) | ||
| Low | 2.01 (1.11, 3.65) | 2.15 (1.16, 3.99) | 2.04 (1.09, 3.82) | ||
| Income | |||||
| High | 1.0 | 1.0 | 1.0 | ||
| Medium | 1.02 (0.69, 1.51) | 0.89 (0.60, 1.34) | 0.91(0.60, 1.37) | ||
| Low | 1.09 (0.72, 1.61) | 0.94 (0.60,1.46) | 0.94(0.60, 1.47) | ||
| Educ: | |||||
| High | 1.0 | 1.0 | 1.0 | ||
| Medium | 0.81 (0.51,1.28) | 0.81 (0.50, 1.31) | 0.82 (0.50, 1.32) | ||
| Low | 1.36 (0.87, 2.11) | 1.32 (0.82, 2.13) | 1.32 (0.82, 2.14) | ||
| Utility shut-off | |||||
| No | 1.0 | ||||
| Yes | 2.11 (1.18, 3.81) | ||||
| Public assistance | |||||
| No | 1.0 | ||||
| Yes | 0.88 (0.42, 1.86) | ||||
| Homeless | |||||
| No | 1.0 | ||||
| Yes | 1.02 (0.38, .2.77) | ||||
| Model p-values | <.10 | N.S. | <.05 | <.05 | <.05 |
Dependent variable is self reported physical health fair/poor vs. excellent/very good/good
The relationship between SSS and self-rated physical health was also persistent even after accounting for objective SES measures (Table 4). Specifically, women in the low SSS category were far more likely than women in the highest category to rate their overall postpartum physical health as poor, even after controlling education and income (OR 2.15; 95% CI 1.16, 3.99). After adjusting for all other SES measures those in the low SSS category were still far more likely than those in the highest category to have relatively poor postpartum physical health (OR 2.04; 95% CI 1.09, 3.82). Note that after adjusting for SSS, income and education were unrelated to poor physical health.
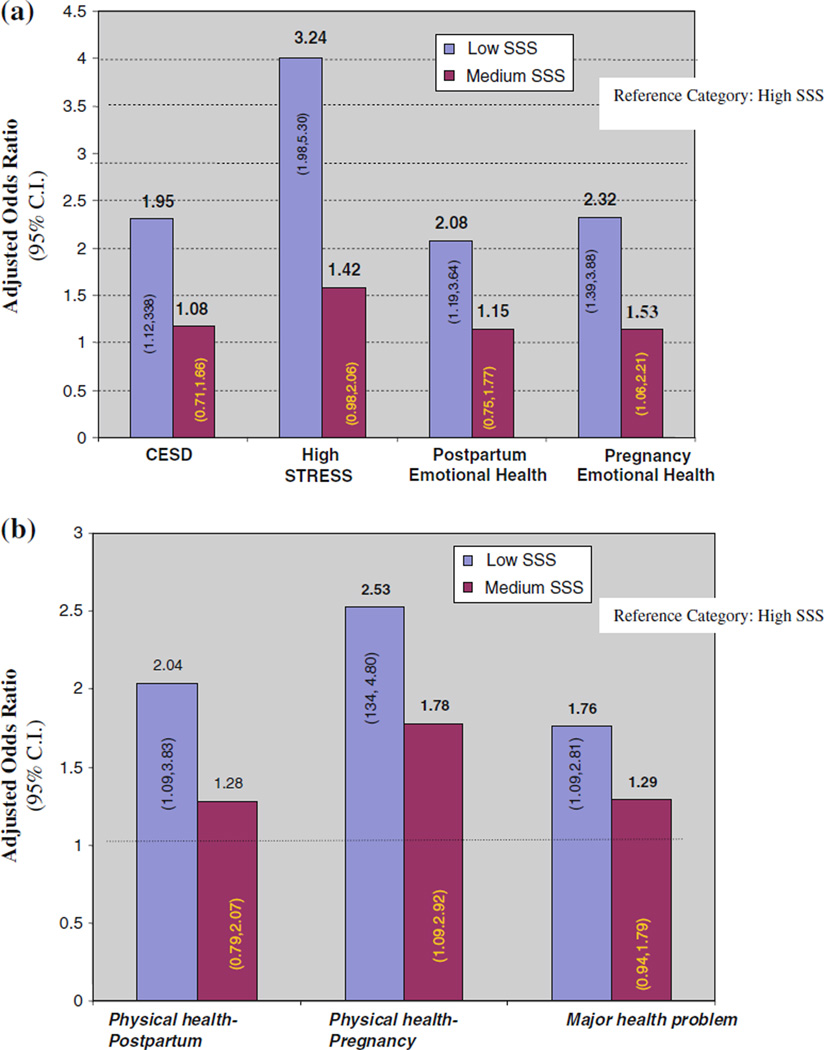
A summary of results for additional health outcomes is reported in Fig. 1. Adjusted odds ratios and 95% confidence intervals associated with low and medium compared to high SSS are presented, in each case after adjusting for income, education and all three other objective SES measures. The results show that for every other outcome, women in the low SSS category were significantly more likely to have worse health outcomes, even after adjusting for SES measures. Women in the low SSS category, for example, were 1.95 times more likely than women in the high SSS category to have depressive symptomatology (OR 1.95; 95% CI 1.1.12, 3.38) (Fig. 1a), as well as two times more likely to report being in relatively poor physical health in pregnancy (OR 2.53; 95% CI 1.34, 4.80) (Fig. 1b).
Fig. 1.
The relationship of subjective social status on health outcomes. a. Adjusted odds ratios: summary of effects of SSS on measures of emotional health; b. Adjusted odds ratios: effects of SSS on measures of physical health
Discussion
The analyses of the relationship between our measure of subjective social status (SSS) and several emotional and physical health outcomes revealed the following: [1] SSS was related to all health outcomes; [2] this relationship exists independently of the influence of more conventional or objective measures of socioeconomic status; and [3] the relationship between SSS and health appears to be more robust than that for objective measures of socioeconomic status.
Our findings are consistent with those from other studies of adolescent, middle-aged, and older populations [28–30] demonstrating a significant relationship between measures of subjective social status and overall physical health, independent of measures of objective social status. They also lend support to the notion that, in some cases, measures of SES based on subjective indicators may in fact be more sensitive than those based on objective indicators [3]. Measuring subjective social status may be particularly important, as is the case here, where the study population is relatively poor. Income levels, for example, may be relatively restricted in terms of the range of values in low income populations. Similarly, subtle but important differences along other dimensions of status—such as savings/wealth, the quality of education received, and access to social and community-level resources—may be overlooked. SES-related influences on health behaviors or outcomes may, therefore, go undetected. This highlights the concern raised by other observers, of the need to carefully consider how SES is defined and measured in the context of health research, and how problems associated with concept validity may have important implications for the interpretation of empirical results [2, 3]. A great deal of empirical health research in the U.S., for example, is designed to assess racial/ethnic differences in health behavior and outcomes ‘‘independent’’ of SES differences. To a large extent, however, the integrity and the interpretation of these findings hinges on an adequate and appropriate measurement of SES itself [2, 31, 32]. In summary, our findings suggest that subjective social status may be a critical assessment tool for the measurement of socioeconomic status in low income populations.
Study Limitations
The findings are of course limited with regard to both the characteristics of the sample and the study design. As noted earlier the study sample was derived from data collected as part of a larger, longitudinal investigation of the relationships between maternal stress, prenatal and postpartum health and infant birth outcomes. The protocol for that larger study involved the administration of the SSS Scale at 11 months postpartum. At least in some cases SSS was related here to health measures collected at earlier points in time. As a result the extent of the causal nature of relationships between socioeconomic status, including those as measured by SSS, was beyond the scope of this paper to address.
Recruitment for the larger study occurred at prenatal sites in very low-income urban neighborhoods and yielded a study cohort with a medium income of less than $10,000 per year. The extent to which the findings reported here can be generalized to poorer, or non-impoverished populations is unclear; as a result further research may be warranted in order to establish the generalizability of our findings.
Finally, it is worth noting that the criteria used to categorize the original SSS ladder scores into groups resulted in a relatively small percentage (10.3%, n = 137) of women being categorized as ‘low’. Since it was possible that the findings may, therefore, have been partly a statistical artifact of an ‘outlier’, low SSS group, we replicated the analyses which included women with a ladder score of ‘4’ in the low as opposed to medium SSS group. The pattern of results did not change, and the magnitude of the differences between the low, medium and high SSS groups for all the health outcomes was virtually identical to that reported here.
Research Box.
What is already known about this topic
Conventional socio-economic status indicators such as income and education may have poor construct validity in health outcomes research, especially in homogenous low-income populations.
What this study adds
This study has strengthened the evidence that subjective self-assessment of one’s social standing should be considered in any empirical study that explores relationships between socioeconomic status and maternal health outcomes.
Acknowledgments
This work was supported by the National Institutes of Health and Human Development [R01HD36462-01 A1]; The National Institute of Nursing Research [K23 NR010747-01A1] and the Center for Disease Control and Prevention/ATPM [TS-0626, and TS-0561].
Footnotes
Conflict of interest None declared.
Contributor Information
Erika Fitzpatrick Dennis, Email: dennise@email.chop.edu, Division of Neonatology, Children’s Hospital of Philadelphia, Philadelphia, PA, USA; Center for Outcomes Research, Children’s Hospital of Philadelphia, 3535 Market Street, Suite 1029, Philadelphia, PA 19104, USA.
David A. Webb, Division of Adolescent Medicine, Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Scott A. Lorch, Division of Neonatology, Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Leny Mathew, Division of Adolescent Medicine, Children’s Hospital of Philadelphia, Philadelphia, PA, USA.
Joan R. Bloch, College of Nursing and Health Professions and School of Public Health, Drexel University, Philadelphia, PA, USA
Jennifer F. Culhane, Department of Pediatrics, University of Pennsylvania’s School of Medicine, Philadelphia, PA, USA
References
- 1.Lynch J, Kaplan G. Socioeconomic position. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. pp. 13–35. [Google Scholar]
- 2.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: One size does not fit all. JAMA. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 3.Shavers VL. Measurement of socioeconomic status in health disparities research. Journal of the National Medical Association. 2007;99:1013–1023. [PMC free article] [PubMed] [Google Scholar]
- 4.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity and Disease. 1992;2:207–221. [PubMed] [Google Scholar]
- 5.Geronimus AT. Understanding and eliminating racial inequalities in women’s health in the United States: The role of the weathering conceptual framework. Journal of the American Medical Women’s Association. 2001;56:133–136. [PubMed] [Google Scholar]
- 6.Geronimus AT, Hicken M, Keene D, et al. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Astone NM, Misra D, Lynch C. The effect of maternal socio-economic status throughout the lifespan on infant birthweight. Paediatric and Perinatal Epidemiology. 2007;21:310–318. doi: 10.1111/j.1365-3016.2007.00821.x. [DOI] [PubMed] [Google Scholar]
- 8.Tiedje LB. Psychosocial pathways to prematurity: Changing our thinking toward a lifecourse and community approach. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2003;32:650–658. doi: 10.1177/0884217503257529. [DOI] [PubMed] [Google Scholar]
- 9.Adler NE, Epel ES, Lynch C, et al. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychology. 2000;19:586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- 10.Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its association with measures of ill-health in the Whitehall II study. Social Science and Medicine. 2003;56:1321–1333. doi: 10.1016/s0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- 11.Kawachi I. Social capital and community effects on population and individual health. Annals of the New York Academy of Sciences. 1999;896:120–130. doi: 10.1111/j.1749-6632.1999.tb08110.x. [DOI] [PubMed] [Google Scholar]
- 12.Jackson PB. Health inequalities among minority populations. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2005;60:63–67. doi: 10.1093/geronb/60.special_issue_2.s63. [DOI] [PubMed] [Google Scholar]
- 13.Schnittker J, Bhatt M. The role of income and race/ethnicity in experiences with medical care in the United States and United Kingdom. International Journal of Health Services. 2008;38:671–695. doi: 10.2190/HS.38.4.f. [DOI] [PubMed] [Google Scholar]
- 14.Schnittker J, McLeod JD. Health inequalities among minority populations. Journals of Gerontology. 2005;60B:63–67. doi: 10.1093/geronb/60.special_issue_2.s63. [DOI] [PubMed] [Google Scholar]
- 15.Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosomatic Medicine. 2005;67:855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [DOI] [PubMed] [Google Scholar]
- 16.Kramer MS, Seguin L, Lyndon J, et al. Socio-economic disparities in pregnancy outcome: Why do the poor fare so poorly? Paediatric and Perinatal Epidemiology. 2000;14:194–210. doi: 10.1046/j.1365-3016.2000.00266.x. [DOI] [PubMed] [Google Scholar]
- 17.Parker JD, Schoendorf KC, Kiely JL. Associations between measures of socioeconomic status and low birth weight, small for gestational age, premature delivery in the United States. Annals of Epidemiology. 1994;4:271–278. doi: 10.1016/1047-2797(94)90082-5. [DOI] [PubMed] [Google Scholar]
- 18.Starfield B, Shapiro S, Weiss J. Race, family income, and low birth weight. American Journal of Epidemiology. 1991;134:1167–1174. doi: 10.1093/oxfordjournals.aje.a116020. [DOI] [PubMed] [Google Scholar]
- 19.Ostrove JM, Adler NE, Kuppermann M, et al. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychology. 2000;19:613–618. doi: 10.1037//0278-6133.19.6.613. [DOI] [PubMed] [Google Scholar]
- 20.Chung EK, McCullum KF, Elo IT, et al. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113:e523–e529. doi: 10.1542/peds.113.6.e523. [DOI] [PubMed] [Google Scholar]
- 21.Culhane JF, Raugh V, McCullum KF, et al. Exposure to chronic stress and ethnic differences in rates of bacterial vaginosis among pregnant women. American Journal of Obstetrics and Gynecology. 2002;187:1272–1276. doi: 10.1067/mob.2002.127311. [DOI] [PubMed] [Google Scholar]
- 22.Operario D, Adler NE, Williams DR. Subjective Social Status: Reliability and predictive utility for global health. Psychology and Health. 2004;19(2):237–246. [Google Scholar]
- 23.Campbell SB, Cohn JF. Prevalence and correlates of postpartum depression in first-time mothers. Journal of Abnormal Psychology. 1991;100:594–599. doi: 10.1037//0021-843x.100.4.594. [DOI] [PubMed] [Google Scholar]
- 24.Radloff LS. The CES-D scale. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 25.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- 26.Agresti A. An introduction to categorical data analysis. 2nd ed. New York: Wiley-Interscience; 1996. [Google Scholar]
- 27.Stata. STATA. College Station, TX: Stata Corporation; 2007. Stata statistical software: Release 10.0. [Google Scholar]
- 28.Chen E, Paterson LQ. Neighborhood, family, and subjective socioeconomic status: How do they relate to adolescent health? Health Psychology. 2006;25:704–714. doi: 10.1037/0278-6133.25.6.704. [DOI] [PubMed] [Google Scholar]
- 29.Demakakos P, Nazroo J, Breeze E, et al. Socioeconomic status and health: The role of subjective social status. Social Science and Medicine. 2008;67:330–340. doi: 10.1016/j.socscimed.2008.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kopp MS, Skrabski A, Kawachi I, et al. Low socioeconomic status of the opposite sex is a risk factor for middle aged mortality. Journal of Epidemiology and Community Health. 2005;59:675–678. doi: 10.1136/jech.2004.027284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krieger N. Stormy weather: Race, gene expression, and the science of health disparities. American Journal of Public Health. 2005;95:2155–2160. doi: 10.2105/AJPH.2005.067108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krieger N. Why epidemiologists cannot afford to ignore poverty. Epidemiology. 2007;18:658–663. doi: 10.1097/EDE.0b013e318156bfcd. [DOI] [PubMed] [Google Scholar]