Abstract
Background
Incorrect condom use is a common problem that can undermine their prevention impact. We assessed the prevalence of two condom use problems, breakage/slippage and partial use, compared problems by partnership type, and examined associations with respondent, partner, and partnership characteristics.
Methods
Data were collected at 3-month intervals over a 12-month period (1999–2000) among urban STD clinic users. Condom use problems were compared between partnership types using z-tests for equality of proportions. Logistic generalized estimating equations modeling accounted for within-participant correlation of repeated measures.
Results
Overall, 3,297 respondents reported 9,304 main and 6,793 non-main partnerships; condoms were used at least once in 4,942 (53.0%) and 4,523 (66.6%) of these partnerships respectively. Condom breakage/slippage was reported during 6.0% of uses (5.1% main, 9.4% non-main) and partial use during 12.5% of uses (12.8% main, 11.5% non-main). The proportion of respondents experiencing any condom use problem in the prior 3 months was higher among main compared to non-main partnerships: 39.1% v. 29.9% had either problem; 22.5% v. 19.0% had breakage/slippage only; 21.8% v. 18.7%, partial use; and 8.7% v. 7.1% had both use problems. In multivariable analysis, factors associated with condom use problems varied by partnership type and respondent sex. The most common predictors of problems across models were sex while high and inconsistent condom use.
Conclusions
This study highlights the diverse set of risk factors for condom use problems at the individual, partner and partnerships levels.
Keywords: condom use problems, sexual partnerships
Introduction
Consistent and correct use of latex condoms reduces risk for HIV as well as other sexually transmitted infections1–3 Although most STI/HIV transmission takes place when condoms are not used,4,5 and mechanical condom failures are relatively rare,6 the effectiveness of condoms is jeopardized by commonly experienced problems with use resulting in breakage, slippage and partial use (i.e. delayed application or early removal).7–9
Many investigations have focused on associations between sexual risk factors and the consistency of self-reported condom use, but few have reported on use problems associated with condoms.3,8 A systematic review of studies examining condom use and risk of gonorrhea and chlamydia found that of 45 studies evaluated, only 2 measured condom use problems.10 Studies which examined condom use problems have documented a high prevalence of these outcomes.11 For example, Project RESPECT, a study of HIV counseling interventions among STD clinic clients, reported high rates of use problems; 41 percent of users experienced at least one problem (i.e., breakage, slippage, leakage during withdrawal and partial use) during a three-month follow-up period, and nearly one in 10 condom uses involved a use problem that could increase STI risk. Further, approximately two-thirds of use problems were related to late application or early removal of condoms during intercourse (and were thus potentially modifiable), whereas largely unintentional use problems (breakage, slippage, leakage) accounted for only one-third overall problems.12 Other studies have reported similarly high rates.13 Factors associated with condom use problems have primarily focused on risk factors at the individual level and have included inexperience with condoms, inconsistent use, prior condom breakage or multiple use problems,12,14 poor condom fit,15,16 use of oil-based lubricant, difficulties applying and removing condoms after ejaculation, and multiple sex partners.17
Some investigators have examined partnership characteristics and inconsistent condom use, and, less frequently, condom use problems. Previous studies have found that relationship status is significantly related to condom use problems,5 with cohabiting couples less likely to experience breakage or slippage compared to non-cohabiting couples. Other studies have documented the association between men’s unilateral decision to use condoms (versus a shared decision with the partner) and increased odds for breakage, slippage and partial use, and perceived partner motivation to use condoms with breakage and slippage. 13 Better understanding of the prevalence of, and factors associated with, condom use errors by partnership type may allow for more personalized risk reduction and condom use messaging.
Using data collected in RESPECT-2, a randomized trial of STI/HIV prevention interventions among urban STD clinic users, we sought to expand on previous studies by exploring how characteristics of heterosexual partnerships affect the odds of experiencing two condom use problems (condom breakage/slippage and partial use) during vaginal intercourse. Specifically, we 1) assessed the prevalence of condom use problems; 2) compared problems by partner type (main and non-main partnerships); and 3) examined how characteristics of respondents, partners, and partnerships affect the odds of experiencing condom breakage/slippage or partial use.
Materials and Methods
Data were analyzed from RESPECT-2. The study design and primary outcome results for RESPECT-2 have been described elsewhere.18
Recruitment
Participants were recruited from STD clinics in three cities (Denver, Colorado; Long Beach, California; and Newark, New Jersey) between February 1999 and December 2000. Eligible clients presented to the clinics seeking a full diagnostic STD examination: additional eligibility criteria included HIV-negative status at enrollment, vaginal or anal sex in the preceding 3 months, and being ages 15–39 years. A total of 3,297 men (54%) and women (46%) were enrolled. Structured interviews using audio computer-assisted self-interviewing methodology occurred at baseline and at 3-month intervals for a 12-month period during which respondents described sexual behaviors, individual characteristics, partner, and partnership characteristics for up to 3 partners.
Measures
Detailed information was collected on condom use frequency and problems. Condom use problems were measured with the following two questions: “Of the # times you used a condom, how many times did the condom break or slip off, either during sex or while you/he were/was pulling out?” and, “Of the # times you used a condom, how many times did you/he put the condom on after you started having sex or take it off before you finished having sex?” These variables were dichotomized into zero times vs. one or more times. (Condom breakage and slippage were combined in RESPECT-2 because both problems may be device-related as well as user-related and thus are only partially modifiable. Partial use of condoms, conversely, is entirely user-related and thus fully modifiable.) For each sexual partner, respondents were asked, “Which of these best describes (first name given to partner 1, 2, and 3)?” The possible responses were “main partner,” “one-time partner,” or “other partner,” and were recoded as main partner vs. non-main partner (i.e. one time + other partner). Thus, respondents were able to name both main and non-main partners (and multiple main or non-main partners) during the same 3-month interval. While the status of these partnerships could have changed during the course of the study and/or the same partnerships could have been reported on during multiple intervals, respondents were not asked to provide this information.
The following characteristics were examined to assess their relationships with each condom use problem for both main and non-main partnerships: Respondent: age, race, gender and education level, number of past 3-month sex partners, had sex while high, STI history and symptoms previous 3 months. Partner: age, partner had sex with others, intravenous drug user, perceived partner risk for STI (very likely, likely or unlikely v. very unlikely), and partner STI history and symptoms previous 3 months. Partnership: how long the couple was acquainted before initiating sex (< 1 month v. > 1 month), length of sexual relationship (> 1 month v. < 1 month), whether STIs or condoms were discussed, number of times a condom was used for vaginal sex acts (continuous variable), and condom use consistency (100% v. <100%). Interview time (baseline, 3, 6, 9, or 12 months), and intervention assignment were included as control variables.
Analysis
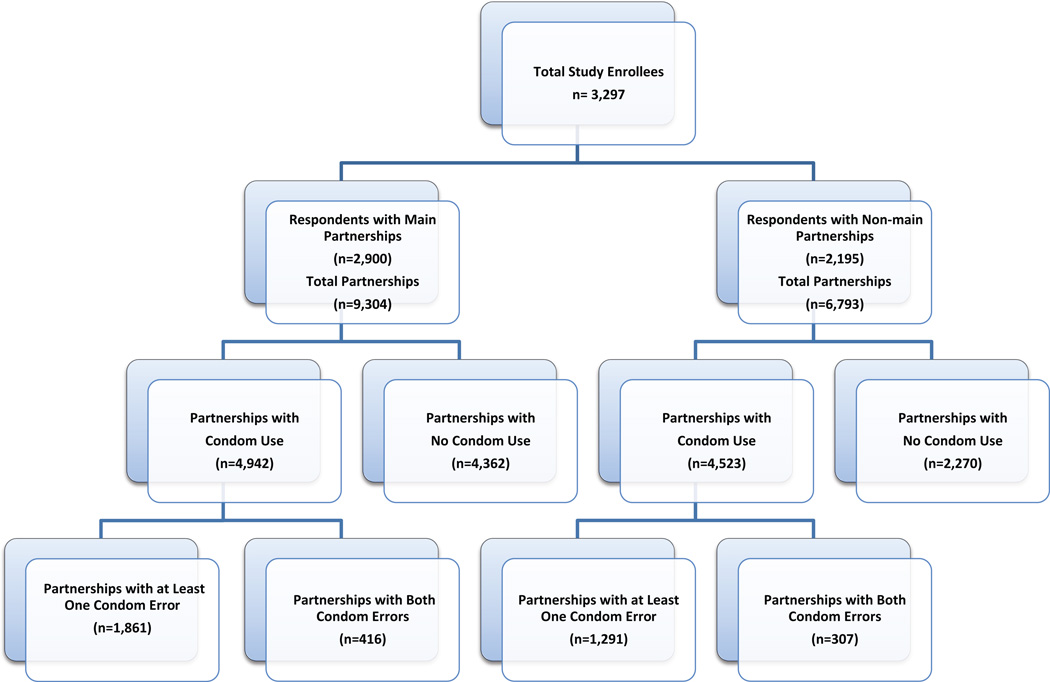
Statistical analysis was conducted among partnerships with valid information where condoms were used for vaginal sex, (n=9,465 sexual partnerships). (Figure 1). Chi-squared tests were conducted to determine individual level predictors associated separately with breakage/slippage and partial use. Proportions of main and non-main partnerships ever experiencing breakage/slippage, partial use, both use problems, and at least one use problem were compared using a z-test for equality of proportions. For all bivariate analyses, we used a more stringent statistical criterion to indicate significance (p ≤ 0.005) due to a large sample size.
Figure 1.
Analytic Sample Description: Partnerships Reported in at Least One
3-month Interval with Complete Condom Use Data
Eight models were fitted, modeling the probability of any episode of breakage/slippage and/or partial use, stratified by both sex and type of partnership. The models were developed using the generalized estimating equations (GEE) approach to account for possible correlations among multiple partnerships of each participant, multiple condom uses among participants, and multiple time intervals. Proc genmod in SAS® version 9.2 was employed for fitting the models, and only significant individual predictor variables were retained in final models in accordance with the backward elimination method.
RESULTS
Respondents who reported vaginal sex in the prior 3 months with a main sexual partner in at least one interview during the study (n= 2,900) were represented equally by men and women, had a median age of 24, and a majority had not obtained a high school education (65.5%). African Americans comprised the largest group of respondents (52.3%) followed by Whites (20.6%), Latinos (18.0%) and other or multiracial (9.1%). Those who reported vaginal sex in the prior 3 months with at least one non-main partner (n=2,195) were more likely to be male (57.4%) but otherwise were similar to the sample reporting main partnerships.
Frequency of Total Condom Use Problems Experienced
A total of 65,234 condoms were used by all respondents; condom breakage/slippage occurred with 3,940 condoms used (6.0%), and partial use occurred with 8,163 condoms used (12.5%). The per-use rate of condom breakage/slippage and partial use among main partnerships were 5.1% and 12.8% respectively. The per-use rate of condom breakage/slippage and partial use among non-main partnerships were 9.4% and 11.5% respectively (Table 1). All the compared rates were significantly different with p<0.0001.
Table 1.
Percent of Condom Uses Affected by Different Types of Condom Use Problems by Partnership Type
| Main (% of total condoms used, 95% CI) |
Non-main (% of total condoms used, 95% CI) |
Total (% of total condoms used, 95% CI) |
|
|---|---|---|---|
| Condom Breakage/Slippage† | 2643 (5.1, 4.9–5.3) | 1297 (9.4, 8.9–9.9) | 3940 (6.0, 5.8–6.2) |
| Condom Partial Use† | 6574 (12.8, 12.5–13.1) | 1589 (11.5, 11.0–12.1) | 8163 (12.5,12.2–12.8) |
| Total condoms used | 51454 | 13780 | 65234 |
Rates are statistically significantly different for main and non-main partnerships (p<0.0001).
Respondents reported 9,304 total main partnerships, 53.1% (n=4,942) in which condoms were used at least once (Figure 1). Among main partnerships in which condoms were used during the last 3 months, 39.1% (n=1861) experienced at least one type of condom use problem (breakage/slippage or partial use); 22.5% (n=1,091) breakage/slippage, 21.8% (n=1,062) partial use, and 8.7% (n=416) both types of use problems (Table 2). Respondents reported 6,793 total non-main partnerships, 66.6% (n=4,523) in which condoms were used at least once (Figure 1). Among non-main partnerships in which condoms were used, 29.9% (n=1,291) experienced at least one type of condom problem; 19.0% (n=839) breakage/slippage, 18.7% (n=823) partial use, and 7.1% (n=307) both types of use problems (Table 2). All the compared percentages were significantly different with p<0.001 or p<0.005.
Table 2.
Percentages of Partnerships Experiencing Different Types of Condom Use Problems by Partnership Type
| Main Partnerships | Non-main Partnerships | |||||
|---|---|---|---|---|---|---|
| Type of Error | Valid Total* |
No. with Condom Errors |
Percentage with Condom Errors (95% CI) |
Valid Total* |
No. with Condom Errors |
Percentage with Condom Errors (95% CI) |
| Condom Breakage/Slippage† | 4839 | 1091 | 22.5 (21.4–23.7) | 4423 | 839 | 19.0 (17.8–20.1) |
| Condom Partial Use† | 4866 | 1062 | 21.8 (20.7–23.0) | 4412 | 823 | 18.7 (17.5–19.8) |
| Both Condom Problems‡ | 4763 | 416 | 8.7 (7.9–9.5) | 4315 | 307 | 7.1 (6.3–7.9) |
| At Least One Condom Problem† | 4763 | 1861 | 39.1 (37.7–40.5) | 4315 | 1291 | 29.9 (28.6–31.3) |
Some respondents had missing data for one or both condom use problems.
Percentages are statistically significantly different for main and non-main partnerships (p<0.001).
Percentages are statistically significantly different for main and non-main partnerships (p<0.005).
Multivariable Results
Main Partners: Breakage/Slippage
For men in main partnerships, increased odds for any breakage/slippage problem were associated with: knowing one’s partner less than one month, less education, and having a partner who recently experienced STI-related symptoms. For women, factors included: experiencing past 3-month STI-related symptoms, and talking with sex partner about STIs or condoms. Both men and women had increased odds for any condom breakage/slippage when they had sex while high with drugs/alcohol, and when they had a higher number of condom uses (Table 3).
Table 3.
GEE Logistic Regression Models: Condom Breakage/Slippage among Those Who Had Vaginal Sex with a Main Partner (4,839 partnerships) and Non-Main Partner (4,420 partnerships)
| Predictors | MAIN PARTNERS | NON-MAIN PARTNERS | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males (2,299 partnerships) | Females (2,540 partnerships) | Males (2,785 partnerships) | Females (1,635 partnerships) | ||||||||||||||
| Odds Ratio |
P* | [95% CI] | Odds Ratio |
P* | [95% CI] | Odds Ratio |
P* | [95% Cl] | Odds Ratio |
P* | [95% Cl] | ||||||
| RESPONDENT | |||||||||||||||||
| Education | <HS | 1.35 | 0.0174 | 1.05 | 1.73 | 1.21 | 0.1080 | 0.96 | 1.54 | 1.36 | 0.0129 | 1.07 | 1.74 | 1.39 | 0.0287 | 1.04 | 1.88 |
| HS grad + | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |
| Respondent had sex while high | |||||||||||||||||
| Ever | 1.30 | 0.0287 | 1.03 | 1.64 | 1.50 | 0.0005 | 1.19 | 1.88 | 1.82 | <0.0001 | 1.46 | 2.27 | 1.26 | 0.0925 | 0.96 | 1.66 | |
| Never | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |
| Respondent had STI symptoms prior 3 months | |||||||||||||||||
| Yes | 1.12 | 0.4279 | 0.85 | 1.49 | 1.31 | 0.0210 | 1.04 | 1.64 | |||||||||
| No or not known | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| PARTNER | |||||||||||||||||
| Partner had STI prior 3 months | |||||||||||||||||
| Yes | 2.42 | 0.0042 | 1.32 | 4.44 | 1.65 | 0.2203 | 0.74 | 3.66 | |||||||||
| No or not known | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| Partner had STI symptoms prior 3 months | |||||||||||||||||
| Yes | 1.36 | 0.0297 | 1.03 | 1.80 | 1.23 | 0.1838 | 0.90 | 1.68 | |||||||||
| No or not known | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| Perceived partner STI risk | |||||||||||||||||
| Very likely, likely, or unlikely | 1.29 | 0.0424 | 1.01 | 1.64 | 1.63 | 0.0008 | 1.22 | 2.17 | |||||||||
| Very unlikely | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| PARTNERSHIP | |||||||||||||||||
| How long partners knew each other before initiating sex | |||||||||||||||||
| Less than 1 month | 1.27 | 0.0439 | 1.01 | 1.60 | 1.06 | 0.6419 | 0.84 | 1.33 | 1.26 | 0.0292 | 1.02 | 1.56 | 0.93 | 0.5908 | 0.71 | 1.21 | |
| 1 month or longer | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |
| Discussed condoms with partner | |||||||||||||||||
| Ever | 1.23 | 0.2116 | 0.89 | 1.71 | 1.42 | 0.0444 | 1.01 | 2.00 | |||||||||
| Never or not known | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| Discussed STI with partner | |||||||||||||||||
| Ever | 1.17 | 0.1594 | 0.94 | 1.46 | 1.24 | 0.0378 | 1.01 | 1.53 | 1.35 | 0.0059 | 1.09 | 1.68 | 1.66 | <0.0001 | 1.28 | 2.14 | |
| Never or not known | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |
| Number of protected vaginal sex acts | 1.01 | 0.0288 | 1.00 | 1.01 | 1.01 | <0.0001 | 1.01 | 1.02 | 1.03 | 0.0046 | 1.01 | 1.05 | 1.03 | 0.0934 | 1.00 | 1.06 | |
| Percent protected vaginal sex acts | |||||||||||||||||
| 1%–99% condom use | 1.05 | 0.6840 | 0.83 | 1.32 | 0.95 | 0.6025 | 0.76 | 1.17 | 1.21 | 0.0969 | 0.97 | 1.52 | 1.07 | 0.66 | 0.79 | 1.44 | |
| 100% condom use | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |
| Length of sexual partnership | |||||||||||||||||
| 1 month or longer | 0.77 | 0.0221 | 0.62 | 0.96 | 0.91 | 0.4878 | 0.70 | 1.18 | |||||||||
| < 1 month | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
Main Partners: Partial Use
For men in main partnerships, the following characteristics were associated with an increased risk for partial use: having a sexual partner who recently experienced STI symptoms. For women, factors were: being in a sexual partnership for one month or longer, and having a partner with a history of injection drug use. Characteristics for both men and women included having sex while high, less education, and using condoms less than 100% of the time (Table 4).
Table 4.
GEE Logistic Regression Models: Partial Condom Use among Those Who Had Vaginal Sex with a Main Partner (4,865 partnerships) and a Non-Main Partner (4,408 partnerships)
| Predictors | MAIN PARTNERS | NON-MAIN PARTNERS | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males (2,304 partnerships) | Females (2,561 partnerships) | Males (2,776 partnerships) | Females (1,632 partnerships) | ||||||||||||||
| Odds Ratio | P* | [95% CI] | Odds Ratio | P* | [95% CI] | Odds Ratio | P* | [95% CI] | Odds Ratio | P* | [95% CI] | ||||||
| RESPONDENT | |||||||||||||||||
| Education | <HS | 0.75 | 0.0144 | 0.59 | 0.94 | 0.70 | 0.0041 | 0.56 | 0.89 | ||||||||
| HS Grad + | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| Respondent had sex while high | |||||||||||||||||
| Ever | 1.62 | <0.0001 | 1.30 | 2.00 | 1.34 | 0.0112 | 1.07 | 1.67 | 1.44 | 0.0012 | 1.15 | 1.79 | 0.98 | .08715 | 0.75 | 1.28 | |
| Never | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | N/A | Ref | N/A | N/A | |
| PARTNER | |||||||||||||||||
| Partner had STI symptoms prior 3 months | |||||||||||||||||
| Yes | 1.70 | 0.0001 | 1.30 | 2.22 | 1.03 | 0.8555 | 0.75 | 1.42 | |||||||||
| No or not known | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| Partner was IDU | |||||||||||||||||
| Ever | 0.95 | 0.8876 | 0.45 | 1.98 | 1.83 | 0.0090 | 1.16 | 2.89 | |||||||||
| Never | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| PARTNERSHIP | |||||||||||||||||
| Length of the sexual partnership | |||||||||||||||||
| 1 month or longer | 1.08 | 0.5667 | 0.84 | 1.38 | 1.27 | 0.0490 | 1.00 | 1.62 | |||||||||
| < 1 month | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| Number of protected vaginal sex acts | 1.00 | 0.0654 | 0.9997 | 1.01 | 1.00 | 0.5861 | 0.9972 | 1.01 | 1.01 | 0.1433 | 0.9959 | 1.03 | 0.99 | 0.7097 | 0.96 | 1.04 | |
| Percent protected vaginal sex acts | |||||||||||||||||
| 1%–99% condom use | 2.10 | <0.0001 | 1.67 | 2.64 | 1.84 | <0.0001 | 1.47 | 2.30 | 1.71 | <0.0001 | 1.37 | 2.14 | 2.37 | <0.0001 | 1.83 | 3.08 | |
| 100% condom use | Ref | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | ||
| How long partners knew each other before initiating sex | |||||||||||||||||
| Less than 1 month | 1.30 | 0.0084 | 1.07 | 1.58 | 1.06 | 0.6813 | 0.81 | 1.39 | |||||||||
| 1 month or longer | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
| Discussed condoms with partner | |||||||||||||||||
| Ever | 1.31 | 0.0243 | 1.04 | 1.66 | 1.37 | 0.0819 | 0.96 | 1.95 | |||||||||
| Never or not known | Ref | N/A | N/A | N/A | Ref | N/A | N/A | N/A | |||||||||
Non-Main Partners: Breakage/Slippage
For men in non-main partnerships, the following characteristics were associated with an increased risk for any breakage/slippage: engaging in sex while high, an increased number of protected vaginal sex acts, a partner who had an STI in the prior 3 months, being in a sexual partnership for less than one month, and knowing one’s partner for less than one month prior to initiating sex. Characteristics for both men and women included the perception that one’s partner had STI risk, less education, and having discussed STIs with one’s partner (Table 3).
Non-Main Partners: Partial Use
Men in non-main partnerships had higher odds for partial condom use if they reported recently having sex while drunk or high, knew one’s partner for less than one month before initiating sex, or had previously talked with one’s partner about using condoms. The single common predictor associated with partial use for women and men was less than 100% condom use (Table 4).
Discussion: Implications for Future STI/HIV Prevention and Research Efforts
Condom use problems were prevalent among this large sample of urban STD clinic attendees in the U.S.; more than 1 in 3 partnerships where condoms were used experienced condom use problems over the last 3 months. The per-use rates of condom breakage/slippage (1 of 16 condoms used overall) are slightly higher than estimates from other U.S. studies.5,16,17,19–21 The per-use rate of partial condom use (1 of 8 condoms used overall) was even higher than breakage/slippage.
We anticipated our finding that partial condom use occurs more frequently in main partnerships where users may be primarily concerned with preventing pregnancy (and not disease); this distinction is important for STI prevention purposes since partial use is likely more amenable to behavioral interventions and partnership communication. Factors associated with early condom removal in other studies include erection loss and difficulties reaching orgasm due to reduced sensation,22 while delayed application of condoms may be due to mistaken beliefs that condoms are only important for STI or pregnancy prevention during ejaculation.22,23 The high partial use rates found in this study underscores that that STI/HIV prevention interventions should stress the importance of using condoms from start to finish,7,22 and also provide and encourage the use of different types of condoms to assist the user in finding the types that may allow for the greatest level of sensitivity.
This study also highlights the diverse set of factors related to condom use problems at the individual, partner and partnerships levels. For both men and women, our research corroborates findings from other studies noting that exposure to risks of pregnancy and STIs are not necessarily isolated to periods of nonuse for these persons.12 However, even when condoms are used consistently, individuals may use them incorrectly, which has direct implications for STD prevention interventions. For example, men in main partnerships had increased odds for any breakage/slippage when they had a partner who recently experienced STI-related symptoms. Given that men were recruited from STD clinics and had received standard of care counseling following STD treatment, this finding highlights the need for more intensive counseling strategies for these men. For women, risk factors included experiencing past 3-month STI-related symptoms and talking with sex partner about STIs or condoms. Communication with sex partners is one of the most important consistent predictors of condom use in the literature, and most prevention interventions are designed to enhance partner communication about condom use.
Having vaginal sex while under the influence of alcohol/drugs was the single most consistent predictor of condom use problems. This finding complements studies documenting the association between substance use, higher levels of sexual risk-taking and lower levels of condom use.25–27 This appears to be particularly true for non-main partnerships where condom use may be more greatly affected by partner characteristics, perceived self-efficacy for negotiation, and the type of sexual encounter (i.e., first time versus casual) to a greater degree than within established relationships.26,28 Thus, the incorporation of substance use components into sexual risk reduction interventions targeted to partner-specific characteristics and situations may be the most important enhancement to present STI/HIV prevention efforts our study offers.
Our study had several strengths. First, the large number of participants enrolled in RESPECT-2 allowed for comparisons between types of partnerships, specific condom use problems, and by sex. Further, this study improves upon the methodology used in previous studies by collecting detailed condom use problem data from individual partnerships over time.8 Specifically, the measures of breakage/slippage used in this study were designed to ask about use problems occurring during intercourse thereby eliminating reports of condom breakage that may have occurred prior to usage (i.e., when opening the packaging and/or applying the condom), which would not confer pregnancy or STI risk.17
Study limitations include our inability to identify specific partners at each survey because respondents could have reported on the same partnerships multiple times and a partnership could have changed status during the course of the study. This is particularly problematic given the role that partnership status plays in condom use. We were unable to account for additional relationship attributes that may influence condom use frequency and problems, such as communication about overcoming past condom use problems and enhanced proficiency of condom use resulting from using condoms in the same partnership over time. Another caveat is that our dichotomy of main versus non-main partnerships is not necessarily mutually exclusive as many respondents with main partners also had non-main partnerships. Thus, respondents who had both types of partnerships during the course of the study were represented within both samples. As with other studies, this study also relied on self-reported condom use and use problems and not objective biomarkers of unprotected sexual activity, such as prostate-specific antigen and Y chromosome. Finally, the age of the data from RESPECT-2 trial is a potential limitation to the extent that the prevalence of condom use problems and associations with covariates may have changed over time.
Respondents used condoms during less than half of vaginal sexual encounters, and even when condoms were used, problems with use occurred commonly. 5Understanding factors associated with condom breakage and slippage is important as studies have shown these events can be reduced through behavioral counseling.24 Our data support the importance of addressing condom skills to enhance proper use, and recent policy developments may enhance opportunities to do so, especially the endorsement by the US Preventive Services Task Force of high-intensity behavioral counseling as a recommended prevention intervention for adolescents and adults at risk of STD,29 and the decision by the Centers for Medicaid and Medicare Services to provide reimbursement for this prevention service. Additionally, promising new condom technologies are evolving that may improve successful condom application and usage throughout intercourse, and condoms could be further improved to enhance the fit and sensitivity for all users. Additionally, marketing that emphasizes that sexual satisfaction is possible with the use of condoms for both men and women could supplement or replace traditional public health disease avoidance messaging.30,31 Finally, future research should incorporate detailed questions about condom use problems and the contexts and reasons attributed to these problems. Rigorous examination of the relative effectiveness of skill-based training to prevent condom breakage and slippage, communication techniques to avoid partial usage, and the impact of condom use problems on STI acquisition will further enhance understanding of the importance of condom use problems.
Acknowledgments
RESPECT-2 was funded by the United States Centers for Disease Control and Prevention. The preparation of this manuscript was supported in part by Award Number P20MD003942 from the National Institute on Minority Health and Health Disparities. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, the National Institute on Minority Health and Health Disparities, or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Peterman TA, Tian LH, Warner DL, et al. Condom use in the year following a sexually transmitted disease clinic visit. Int J STD AIDS. 2009;20:9–13. doi: 10.1258/ijsa.2008.008177. [DOI] [PubMed] [Google Scholar]
- 2.Warner L, Newman DR, Austin HD, et al. Condom effectiveness for reducing transmission of gonorrhea and chlamydia: the importance of assessing partner infection status. Am J Epidemiol. 2004;159:242–251. doi: 10.1093/aje/kwh044. [DOI] [PubMed] [Google Scholar]
- 3.Warner L, Macaluso M, Newman D, et al. Condom effectiveness for prevention of C trachomatis infection. Sexually Transmitted Infections. 2006;82:265. doi: 10.1136/sti.2005.018978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rietmeijer CA, Van Bemmelen R, Judson FN, Douglas JM., Jr Incidence and repeat infection rates of Chlamydia trachomatis among male and female patients in an STD clinic: implications for screening and rescreening. Sex Transm Dis. 2002;29:65–72. doi: 10.1097/00007435-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Steiner MJ, Cates W, Jr, Warner L. The real problem with male condoms is nonuse. Sex Transm Dis. 1999;26:459–462. doi: 10.1097/00007435-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 6.White ND, Hill DM, Bodemeier S. Male condoms that break in use do so mostly by a "blunt puncture" mechanism. Contraception. 2008;77:360–365. doi: 10.1016/j.contraception.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 7.Choi KH, Gregorich SE. Assessment of fully and partially condom-protected sex among US women: The potential for overestimating protected sex acts. Sex Transm Dis. 2010 doi: 10.1097/OLQ.0b013e3181ffd73e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Noar SM, Cole C, Carlyle K. Condom use measurement in 56 studies of sexual risk behavior: Review and recommendations. Arch Sex Behav. 2006;35:327–345. doi: 10.1007/s10508-006-9028-4. [DOI] [PubMed] [Google Scholar]
- 9.Paz-Bailey G, Koumans EH, Sternberg M, et al. The effect of correct and consistent condom use on chlamydial and gonococcal infection among urban adolescents. Arch Pediatr Adolesc Med. 2005;159:536–542. doi: 10.1001/archpedi.159.6.536. [DOI] [PubMed] [Google Scholar]
- 10.Warner L, Stone KM, Macaluso M, Buehler JW, Austin HD. Condom use and risk of gonorrhea and Chlamydia: a systematic review of design and measurement factors assessed in epidemiologic studies. Sex Transm Dis. 2006;33:36–51. doi: 10.1097/01.olq.0000187908.42622.fd. [DOI] [PubMed] [Google Scholar]
- 11.Sanders SA, Yarber WL, Kaufman EL, Crosby RA, Graham CA, Milhausen RR. Condom use errors and problems: a global view. Sexual health. 2012;9:81–95. doi: 10.1071/SH11095. [DOI] [PubMed] [Google Scholar]
- 12.Warner L, Newman DR, Kamb ML, et al. Problems with condom use among patients attending sexually transmitted disease clinics: Prevalence, predictors, and relation to incident gonorrhea and chlamydia. Am J Epidemiol. 2008;167:341–349. doi: 10.1093/aje/kwm300. [DOI] [PubMed] [Google Scholar]
- 13.Crosby R, Milhausen R, Sanders SA, Graham CA, Yarber WL. Two heads are better than one: The association between condom decision-making and condom use errors and problems. Sexually Transmitted Infections. 2008;84:198–201. doi: 10.1136/sti.2007.027755. [DOI] [PubMed] [Google Scholar]
- 14.Kalichman SC, Amaral CM, Swetzes C, et al. A simple single-item rating scale to measure medication adherence: further evidence for convergent validity. J Int Assoc Physicians AIDS Care (Chic Ill) 2009;8:367–374. doi: 10.1177/1545109709352884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crosby R, Sanders S, Yarber WL, Graham CA. Condom-use errors and problems: a neglected aspect of studies assessing condom effectiveness. Am J Prev Med. 2003;24:367–370. doi: 10.1016/s0749-3797(03)00015-1. [DOI] [PubMed] [Google Scholar]
- 16.Gabbay MB, Thomas J, Gibbs A, Hold P. A randomized crossover trial of the impact of additional spermicide on condom failure rates. Sex Transm Dis. 2008;35:862–868. doi: 10.1097/OLQ.0b013e31817fb802. [DOI] [PubMed] [Google Scholar]
- 17.Grady WR, Tanfer K. Condom breakage and slippage among men in the United States. Fam Plann Perspect. 1994;26:107–112. [PubMed] [Google Scholar]
- 18.Metcalf CA, Douglas JM, Jr, Malotte CK, et al. Relative efficacy of prevention counseling with rapid and standard HIV testing: A randomized, controlled trial (RESPECT-2) Sex Transm Dis. 2005;32:130–138. doi: 10.1097/01.olq.0000151421.97004.c0. [DOI] [PubMed] [Google Scholar]
- 19.Macaluso M, Demand MJ, Artz LM, Hook EW., 3rd Partner type and condom use. AIDS. 2000;14:537–546. doi: 10.1097/00002030-200003310-00009. [DOI] [PubMed] [Google Scholar]
- 20.Reece M, Herbenick D, Sanders SA, P M, Temkit M, Yarber WL. Breakage, slippage and acceptability outcomes of a condom fitted to penile dimensions. Sexually Transmitted Infections. 2008;84:143–149. doi: 10.1136/sti.2007.028316. [DOI] [PubMed] [Google Scholar]
- 21.Steiner MJ, Warner DL, Stone KM, Cates W., Jr . Condoms and other barrier methods for prevention of STD/HIV infection and pregnancy. In: Holmes KK, Sparling PF, Stamm WE, et al., editors. Sex Transm Dis. Fourth Edition. New York: McGraw-Hill; 2008. pp. 1821–1830. [Google Scholar]
- 22.Graham CA, Crosby RA, Milhausen RR, Sanders SA, Yarber WL. Incomplete Use of Condoms: The Importance of Sexual Arousal. AIDS Behavior. 2009 doi: 10.1007/s10461-009-9638-7. [DOI] [PubMed] [Google Scholar]
- 23.Warner L, Klausner JD, Rietmeijer CA, et al. Effect of a brief video intervention on incident infection among patients attending sexually transmitted disease clinics. PLoS Medicine. 2008;5 doi: 10.1371/journal.pmed.0050135. 0919-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steiner MJ, Taylor D, Hylton-Kong T, et al. Decreased condom breakage and slippage rates after counseling men at a sexually transmitted infection clinic in Jamaica. Contraception. 2007;75:289–293. doi: 10.1016/j.contraception.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 25.Sly DF, Quadagno D, Harrison DF, Eberstein I, Riehman K. The association between substance use, condom use and sexual risk among low-income women. Fam Plann Perspect. 1997;29:132–136. [PubMed] [Google Scholar]
- 26.Brown JL, Vanable PA. Alcohol use, partner type, and risky sexual behavior among college students: Findings from an event-level study. Addict Behav. 2007;32:2940–2952. doi: 10.1016/j.addbeh.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scott-Sheldon LA, Carey MP, Vanable PA, Senn TE, Coury-Doniger P, Urban MA. Alcohol consumption, drug use, and condom use among STD clinic patients. Journal of Studies on Alcohol and Drugs. 2009;70:762–770. doi: 10.15288/jsad.2009.70.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leigh BC. Alcohol and condom use: a meta-analysis of event-level studies. Sex Transm Dis. 2002;29:476–482. doi: 10.1097/00007435-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Behavioral Counseling to Prevent Sexually Transmitted Infections. [Accessed 2/9/12];2008 at http://www.uspreventiveservicestaskforce.org/uspstf/uspsstds.htm. [PubMed]
- 30.Warner DL, Gallo MF, Macaluso M. Condom use around the globe: How can we fufill the prevention potential of male condoms? Sexual health. 2012 doi: 10.1071/SH11072. In press. [DOI] [PubMed] [Google Scholar]
- 31.Decision Memo for Screening for Sexually Transmitted Infections (STIs) and High Intensity Behavioral Counseling (HIBC) to prevent (STIs) (CAG-00426N) [Accessed 2/9/12];2011 at https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?&NcaName=Screening%20for%20Sexually%20Transmitted%20Infections%20(STIs)%20and%20High-Intensity%20Behavioral%20Counseling%20(HIBC)%20to%20prevent%20(STIs)&bc=ACAAAAAAIAAA&NCAId=250&.