Abstract
Background:
Under-five in Nigeria are the most vulnerable group that are often challenged by emergency health conditions.
Aim:
The study was to describe the magnitude of under-five emergencies in a resource-poor environment of a rural hospital in eastern Nigeria.
Materials and Methods:
A descriptive cross-sectional hospital-based study of 282 under-five patients with emergency health conditions at a rural Hospital in Imo state, eastern Nigeria. Data extracted included bio-data and diagnosis.
Results:
A total of 282 under-five emergencies were studied. The ages of the patients ranged from 12 days to 58 months with mean age of 34 ± 9.4 months. There were 153 (54.3%) males and 129 (45.7%) females with male to female ratio of 1.2: 1. The three most common causes of under-five emergencies were acute uncomplicated malaria (29.1%), severe malaria anemia (24.5%), and acute respiratory infections (22.7%). The predominant outcome of emergency admission was discharged home (83.0%). The preeminent cause of death was severe malaria anemia (81.8%). All deaths occurred within 24 hours of hospitalization.
Conclusion:
The three most common under-five emergencies were infectious medical emergencies and the preeminent cause of death was malaria-related. Strengthening the quality of the Roll Back Malaria Initiative, household and community-integrated management of childhood illnesses will help to reduce these preventable medical emergencies and deaths.
Keywords: Emergencies, Hospital, Nigeria, Outcome, Pattern, Rural, Under-five
Introduction
The under-five children's health status is one of the vital indices of societal development.[1] The morbidity and mortality among this special group of the population therefore exerts socio-economic and medical burden on families, communities, and the nation. It has been generalized that about 70% of the under-five Nigerian children reside in the rural areas of the country. Similarly, rural residence has also been described as one of the risk factors for under-five morbidity and mortality.[2,3] Moreover, there is concentration of emergency medical facilities and personnel in the urban areas of the country. This urban bias in the location of emergency medical services is usually strengthened by the class structure largely skewed toward meeting the emergency medical demands of the better-off sections of the population in the urban Nigeria than the needs of the poor rural Nigerians.
The under-five children's disease states are influenced by the process of growth and development and age is epidemiologically recognized as a constitutional risk factor for some medical conditions during childhood especially infectious diseases.[4] This might be due to bio-physiological changes associated with growth and development. The under-five children are therefore the most vulnerable group that bears the burden of diseases to a large extent in Nigeria. Several factors have been identified as important contributors to under-five morbidity and mortality.[3] These factors are broadly classified into child care-givers-related, health workers-related, and government-related factors. Previous reports have shown that under-five morbidity and mortality in rural[5] and urban[6,7] communities in Nigeria were not only due to tropical diseases but were also caused by preventable medical conditions. The under-five patients are therefore high risk patients under emergency health conditions and this can pose a management challenge to the attending health worker.
Studies have shown that infectious diseases have continued to plague under-five Nigerians[5–7] and constituted the most common cause of emergency medical admissions in Enugu, south-eastern Nigeria,[8] Abuja, capital territory of Nigeria,[9] and Jos, north central Nigeria.[10] Moreover, infectious diseases were reportedly predominant cause of mortality following emergency admissions in Enugu,[8] Abuja,[9] Jos,[10] Lagos,[11] and Ilorin.[12] Surprisingly, most of these infectious diseases can be either prevented or treated with minimum input of health resources. In fact, most of the developed nations of the world have overcome many of these problems by such measures as practice of preventive and promotional medicine alongside the improvement in the standard of living.
Access to health services and the quality of care administered at the primary health care level of health care delivery system have been considered by the world health organization (WHO) as one of the central determinants of health outcome.[13] In addition, health outcome can also be influenced by the illness practices[14] and health-seeking behavior of the under-five children care givers.[15,16] The WHO posits that seeking prompt and appropriate care could reduce child deaths from curable and preventable medical conditions. In a bid to attain the fourth millennium development goal (MDG) aimed at reducing child mortality by two-thirds by the year 2015, the Federal Government of Nigeria has adopted several strategies toward prevention of under-five morbidity and mortality. These interventional strategies have been elucidated for more than a decade and include Baby friendly hospital initiatives (BFHI), national program on immunization (NPI), oral rehydration therapy (ORT), roll back malaria initiatives (RBMI), among others. The recently introduce integrated management of childhood illnesses (IMCI) is an approached aimed at promoting key household practices (household-IMCI), promoting key community practices (community-IMCI), improving health workers skills to manage childhood illnesses holistically, improving health systems to support IMCI implementation and changes in care givers behavior toward adopting recommended practices. The overall goal is to improve the survival, healthy growth, and development of the under-five child. In order to provide necessary under-five emergency health services in any community, health care providers should identify prevailing under-five emergencies, determine their priority rather than continue to provide prototype health services. It is only by taking cognizance of the pattern and outcome of the under-five emergencies that the country plans for effective interventions aimed at reducing preventable emergency admissions among this special group of Nigerians. This will therefore guide institutional and diverse authorities in designing appropriate and dedicated strategies that are family friendly and community-oriented to address the predispositional and enabling factors that promote under-five emergency health facility admissions with its attendant risk of death. It is against this background that the researchers were motivated to study the pattern and outcome of under-five emergencies in a resource-poor environment of a rural hospital in south-eastern Nigeria for preliminary assessment of emergency health needs of the under-five children in the study area.
Materials and Methods
A descriptive cross-sectional hospital-based study of 282 under-five patients who presented between June 2008 and June 2011 with emergency health conditions at St Vincent De Paul hospital, Amurie-Omanze, a rural Mission General Hospital in Imo State, south-eastern Nigeria. The hospital renders 24 hours service daily including public holidays to the community and its environs.
The clinical records of the under-five patients who presented each day to the hospital with emergency health conditions were collected and entered into a data collection schedule sheet. The under-five patients who needed highly specialized diagnostic investigations and critical care were referred out and excluded from the study. Sample size estimation was determined using the formula[17] for estimating minimum sample size for descriptive studies when studying proportions with entire population size < 10,000 using estimated population size of 500 under-five patients based on the previous annual under-five patients hospital attendance records.[5] The estimated minimum sample size assuming 50% expected variance in estimating the proportion of the under-five patients attending the hospital gave final minimum sample size estimate of 217 under-five patients. However, the selected sample size of 282 under-five patients was used based on the duration of the study. Relevant laboratory and radio-diagnostic investigative studies that were not available in the study centre were done at Federal Medical Centre, Owerri, Imo State University Teaching Hospital, Orlu, and Hi-tech Laboratory, Owerri. Data extracted for analysis included bio-data such as age, sex, and diagnosis.
The authors defined under-five patients as a period of childhood from 0 to 59 months. An emergency medical condition refers to medical or surgical condition that requires immediate care on an unscheduled basis. These patients were admitted to the in-patients services of the hospital for management or referred to tertiary hospitals in the state after resuscitations. The outcome of admission was categorized as discharged home, referred to tertiary hospital, left against medical advice, and death.
Statistics
The results generated were analyzed using Statistical Package for Social Sciences (SPSS) software version 13.0, Microsoft coperation, Inc. Chicago, IL, USA for the calculations of mean, frequencies and percentages.
Results
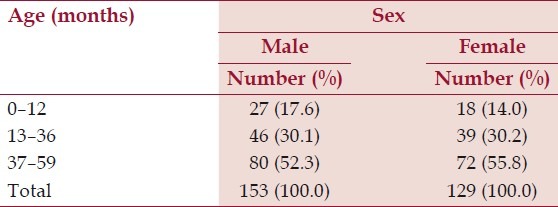
A total of 282 under-five emergencies were seen during the study period. The ages of the patients ranged from 12 days to 58 months with mean age of 34 ± 9.4 months. There were 153 (54.3%) males and 129 (45.7%) females with a male to female ratio of 1.2 [Table 1].
Table 1.
Age and sex distribution of the study population
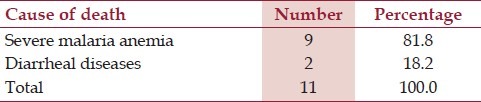
The three most common causes of under-five emergencies were acute uncomplicated malaria (29.1%), severe malaria anemia (24.5%), and acute respiratory infections (22.7%) [Table 2]. The most common outcome of emergency admission was discharged home (83.0%), others included referral to tertiary hospitals (10.3%), dead (3.9%), and signed against medical advice (2.8%) [Table 3]. The predominant cause of death was severe malaria anemia (81.8%) [Table 4]. All deaths occurred within 24 hours of presentation to the hospital.
Table 2.
*Top 10 under-five emergencies
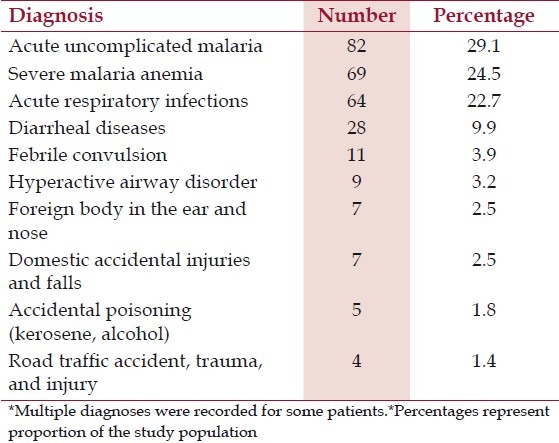
Table 3.
Outcome of under-five emergencies
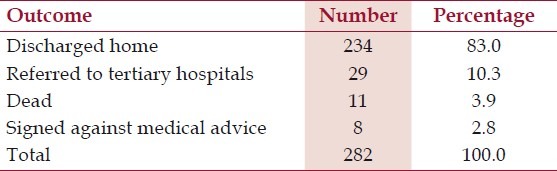
Table 4.
Causes of under-five death
Discussion
This study has showcased the three most common under-five emergencies among the study population. These were medical emergencies resulting from infectious medical conditions such as acute uncomplicated malaria, severe malaria anemia, and acute respiratory infections. This pattern of under-five medical emergency is related to the general trend of morbidity from infectious diseases reported in Nigeria in rural[5] and urban Nigerian communities.[6] This pattern is also similar but varies in reported proportions to the common pediatric emergencies reported from Enugu, south-eastern Nigeria,[8] Abuja, capital territory of Nigeria,[9] Jos, north central Nigeria,[10] and Lagos, south-western Nigeria.[11] The finding of this study has demonstrated that infectious medical conditions are important contributors to under-five children emergencies in Nigeria. The prospects of curtailing these common under-five medical emergencies depend on clear understanding of these emergencies by the health care givers and health care providers attending to under-five children in Nigeria since the under-five population is a special group of people whose diseases are influenced by the process of growth and development.[4] The under-five children are therefore a high risk group for infectious diseases due to the waning of transplacentally acquired immunity and transitional period of development of their own immunity. When these important medical contributors to under-five medical emergencies are not adequately prevented or treated, they may constitute an obstacle to the attainment of MDGs among under-five Nigerians particularly those who are living in resource-poor rural Nigerian communities. The causes of the under-five medical emergencies in Nigeria are factors that are eminently treatable and preventable. The finding of this study is therefore a clarion call to improve on the various programs established by the WHO and Federal Government of Nigeria to prevent morbidity and mortality from infectious diseases. These interventional programs are primarily targeted at the under-five children aimed at reducing preventable deaths among this special population in Nigeria.
This study has shown that the most common cause of under-five emergency was acute uncomplicated malaria infection. This finding is similar to previous reports from Nigeria[8,9] but differ in varying magnitude. According to these reports, malaria is the most common cause of medical emergency from infectious disease in the country. However, the under-five children in holoendemic malaria communities such as the study area are most vulnerable to malaria infection since age is a surrogate marker of acquired immunity for malaria.[18,19] Malaria therefore causes variations in under-five children's health which may result in the impairment of their functional capacities or otherwise pose a threat to their wellness through progression of uncomplicated malaria infection to severe malaria disease. The RBMI is aimed at building human and institutional resources and support to fight the scourge of malaria infection; health care givers who attend to under-five children in rural Nigeria are important recipients of health information and sources of motivation for the family and community members concerning health matters such as appropriate family practices for malaria involving early recognition of the illness and seeking prompt and appropriate health facility-based treatment, prevention of malaria infection and avoidance of ineffective and harmful treatment. The under-five children health care givers education on malaria disease should therefore be an important part of under-five malaria management consultations especially in holoendemic malaria rural communities.
Severe malaria anemia is the second most common under-five emergency in this study. This finding has corroborated the reports that the clinical manifestation of severe malaria infection in under-five children in Nigeria[8,9,11,20] and in other African countries such as Uganda[21] is characterized by the predominant outcome of severe anemia. According to these reports from Nigeria, severe malaria anemia has become a clinical and public health problem in Nigeria and a major cause of under-five medical emergency. Although, malaria may be recognized by care givers in rural Nigeria, but majority of the care givers have not realized that severe malaria is a life threatening medical condition. Pathobiophysiologically, severe malaria anemia may not have an abrupt onset[22] and studies have shown that the severe malaria outcome in under-five children is influenced by interplay of epidemiological[23,24] and immunological factors.[18,19] The health seeking behavior[15,16] and illness-related practices[14,25] are key epidemiological factors that impacts on progression from uncomplicated malaria to severe malaria leading to emergency presentation with its attendant risk of death.
The most common cause of mortality from the emergency medical condition in this study was severe malaria anemia. This finding is similar to the most common cause of under-five mortality reported in Enugu,[8] Ilorin,[12] and in other African countries such as Uganda[21] and Burkina Faso.[26] However, the most common cause of death in this study is at disparity with the reports from Abuja,[9] Jos,[10] and Lagos[11] where malnutrition, diarrheal diseases and respiratory infections were the preeminent causes of death. According to the finding of this study and reports from Enugu,[8] Ilorin,[12] Uganda,[21] and Burkina Faso[26] presentation with severe anemia was associated with most of the deaths from severe malaria. The finding of this study could be a mirror of the late recognition of symptoms of severe malaria anemia complication by under-five children's care givers and a proxy indicator of poor knowledge of early symptoms of severe anemia related complication of severe malaria such as anemic heart failure. This could also be a reflection of poor state of primary health care facilities in the study area since all the patients who died from severe malaria anemia received treatment from first level formal health care delivery system and even concurrent treatment from traditional homes, patent medicine dealers and vendors in the study area. The finding of this study has negated one of the pillars of RBMI on prompt and effective treatment of malaria infection[27] as well as quality of care administered to the sick under-five children at first level of formal health care in the study area.[13] Of great concern in the study area is the inappropriate intervention practices on the sick under-five children especially upper abdominal wall scarification by traditional practitioners for treatment of malaria hepatomegaly and splenomegaly with its attendant disastrous consequences.[5] These traditional interventional practices might have contributed to higher mortality from malaria anemia resulting from blood loss from the scarification. The scarification practices may also have caused delay in seeking and obtaining prompt and effective treatment for malaria infection. There is therefore urgent need for effective methods to enlighten under-five child care givers especially mothers on appropriate child health practices that are safe, timely, effective, efficient, and child health friendly and centered.
Regrettably, all the deaths from severe malaria anemia and diarrheal disease occurred within 24 hours of presentation to the study centre. This finding is similar to previous reports from Nigeria[8,12] and other African countries such as Uganda.[21] This finding has also corroborated previous reports[9,21] and the documentation by WHO[22] that most children dying from malaria do so within 3 days of onset of severe symptoms. This may be attributed to the pathogenesis of severe malaria and has underscored that the speed at which malaria is diagnosed and treated among the under-five children is critical in reducing its mortality. Since severe malaria develops rapidly from uncomplicated malaria disease, the interventional strategies of access to appropriate health facility, administration of effective antimalarial drugs within 24 hours to avert disease progression should therefore be emphasized in the study area. Apparently, despite the achievement of RBMI and laudable advances in the IMCI, mortality from severe malaria disease occurs within 24 hours of presentation to the study centre. There is therefore the need for wider and more dedicated campaign on household and community-based IMCI. The IMCI is aimed at promoting key household practices (household-IMCI), promoting key community practices (community-IMCI), improving health workers skills to manage childhood illnesses holistically, improving health systems to support IMCI implementation, and changes in care givers behavior toward adopting recommended practices with the ultimate goal of reducing morbidity and mortality among the under-fives. This is probably one of the ways the under-five children will benefit from the life saving tenets of RBMI and IMCI. Equipping the care givers and primary health care providers to identify under-five medical emergencies represent one of the largest resources for under-five medical emergencies in the study area. This study therefore beckons for care givers health seeking decision making such as early presentation to appropriate health facility. This should be the focus of intensive mass media campaign in rural Nigeria where there are constraints of accessibility and availability of high quality under-five emergency medical services.
Study implications
The burden of under-five emergencies due to preventable medical conditions is common in resource-poor rural Nigerian communities. If the under-five health status is affected and afflicted by emergency medical conditions, they will probably have shorter expectations of life. Knowledge of common under-five medical emergencies can be a useful tool to the clinicians attending to under-five children in rural Nigeria especially in secondary health care facilities. Generally, the under-five children cannot express themselves verbally like adults. The under-five emergency medical conditions when not properly managed can predispose them to preventable deaths. Prioritizing the emergency medical problems of the under-five children would provide sustainable solution to reduce the health problems of this special group of children in the community. Improving the under-five children's health is therefore important for clinical and public health practice aimed toward an effective under-five health care service delivery. It is only by studying these under-five medical emergencies that the dream of achieving the fourth MDGs as regards child health by the year 2015 will be achieved.
Conclusion
This study has shown that the three most common under-five emergencies were medical emergencies (acute uncomplicated malaria, severe malaria anemia, and acute respiratory infections). The predominant cause of mortality was severe malaria anemia. All deaths occur within 24 hours of presentation to the hospital. Strengthening the pillars of RBMI and improving the quality of the household and community IMCI will help in reduction of these preventable medical emergencies and deaths.
Acknowledgement
The authors are grateful to Rev. Sister Francisca Eya of St. Vincent de Paul Hospital, Amurie-Omanze for permission for the study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Murray CJ, Shibuya K. Can we achieve Millennium Development Goal 4? New analyses of counting trends and forecast of under-five mortality to 2015. Lancet. 2007;370:1040–54. doi: 10.1016/S0140-6736(07)61478-0. [DOI] [PubMed] [Google Scholar]
- 2.Goldman N, Heuveline P. Health-seeking behaviour for child illness in Guatemela. Trop Med Int Health. 2000;5:145–55. doi: 10.1046/j.1365-3156.2000.00527.x. [DOI] [PubMed] [Google Scholar]
- 3.Lawoyin TO. Risk factors for infant mortality in a rural African community. J R Soc Promot Health. 2000;121:114–8. doi: 10.1177/146642400112100213. [DOI] [PubMed] [Google Scholar]
- 4.Njokanma OF, Nkanginieme KE. Growth and development. In: Azubuike JC, Nkangineme KE, editors. Paediatrics and childhealth in a tropical region. 2nd ed. Owerri: African Educational Services; 2007. pp. 56–9. [Google Scholar]
- 5.Iloh GU, Amadi AN, Nwankwo BO, Ugwu VC. Common under-five morbidity in south-eastern Nigeria: A study of its pattern in a rural mission General Hospital in Imo state. Niger J Med. 2011;22:99–104. [PubMed] [Google Scholar]
- 6.Nwolisa CE, Erinugha AU, Ofoleta SI. Pattern of morbidity among pre-school children attending the children's outpatient clinic of Federal Medical Centre, Owerri, Nigeria. Niger J Med. 2005;14:378–80. doi: 10.4314/njm.v14i4.37191. [DOI] [PubMed] [Google Scholar]
- 7.Omokhodion OF, Oyemade A, Sridhar MK. Morbidity pattern among under-five children of market women in Ibadan. Niger J Paediatr. 2003;30:135–9. [Google Scholar]
- 8.Ibeziako SN, Ibekwe RC. Pattern and outcome of admissions in the children's emergency room of the University of Nigeria Teaching Hospital, Enugu. Niger J Paediatr. 2002;29:103–7. [Google Scholar]
- 9.Okechukwu AA, Nwalozie C. Morbidity and mortality pattern of admissions into the emergency paediatric unit of University of Abuja Teaching Hospital, Gwagwalada. Niger J Med. 2011;20:109–13. [PubMed] [Google Scholar]
- 10.Ighogboja IS, Angyo I, Okolo AA, Szlachetka R. Morbidity and mortality patterns of paediatric emergencies in Jos. Niger Med Pract. 1995;30:15–8. [Google Scholar]
- 11.Ezeaka VC, Grange AO, Ogunbase AO. Childhood morbidity and mortality at the Lagos University Teaching Hospital (LUTH) Lagos. Niger J Paediatr. 2002;29:91–5. [Google Scholar]
- 12.Adeboye MA, Ojuawo A, Adeniyi A, Fadeyi A, Alisu AT. Pattern of deaths occurring within the first 24 hours of admission between February and July 2001 in the emergency paediatric unit, University of Ilorin Teaching Hospital. Niger J Paediatr. 2001;29:92–5. [Google Scholar]
- 13.Geneva: World Health Organization; 2000. WHO. World Health Report 2000, Health System: Improving performance. [Google Scholar]
- 14.Oladele BA, Kauna K. Illness-related practices for the management of childhood malaria among the Bwatiye people of north-eastern Nigeria. Malar J. 2005;4:1–6. doi: 10.1186/1475-2875-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tumwesigire S, Watson S. Health-seeking behaviour by families of children suspected to have malaria in Kabale, Uganda. Afr Health Sci. 2002;2:94–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Mbagaya GM. Mothers health seeking behaviour during child illness in a rural Western Kenya community. Afr Health Sci. 2005;4:322–7. doi: 10.5555/afhs.2005.5.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Araoye MO. Research Methodology with Statistics for Health and Social Sciences. Ilorin: Nathadex Publishers; 2004. Sample size determination; pp. 115–21. [Google Scholar]
- 18.Anumudu CI, Okafor CM, Ngwumohaike V, Afolabi KA, Nwuba RI, Nwagwu M. Clinical manifestation and immunological response in severe paediatric malaria in Adeoyo hospital, Ibadan. Afr J Med Med Sci. 2004;33:57–63. [PubMed] [Google Scholar]
- 19.Nwuba R, Sodeinde O, Anumudu C, Omosun Y, Odaibo A, Holder A, et al. The human immune response to plasmodium falciparum includes both antibodies that inhibit merozoites surface protein 1 secondary processing and blocking antibodies. Infect Immun. 2002;70:5328–31. doi: 10.1128/IAI.70.9.5328-5331.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Angyo JA, Pam SD, Sziachetka R. Clinical pattern and outcome in children with acute severe falciparum malaria at Jos University Teaching Hospital, Nigeria. East Afr Med J. 1996;72:823–6. [PubMed] [Google Scholar]
- 21.Idro R, Aloyo J. Manifestation and quality of emergency care and outcome of severe malaria in Mulago Hospital, Uganda. Afr Health Sci. 2004;4:50–7. [PMC free article] [PubMed] [Google Scholar]
- 22.WHO. Severe falciparum malaria. Trans R Soc Trop Med Hyg. 2000;94(Suppl 1):1–45. [PubMed] [Google Scholar]
- 23.Anumudu CI, Okafor CM, Ngumohaike V, Afolabi KA, Nwuba RI, Nwagwu M. Epidemiological factors that promote the development of severe malaria anaemia in children in Ibadan. Afr Health Sci. 2007;7:80–5. doi: 10.5555/afhs.2007.7.2.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greenwood BM. The epidemiology of malaria. Ann Trop Med Parasitol. 1997;91:763–9. doi: 10.1080/00034989760518. [DOI] [PubMed] [Google Scholar]
- 25.Baume C, Helitzer D, Kachur SP. Patterns of care for childhood malaria in Zambia. Soc Sci Med. 2000;51:1491–503. doi: 10.1016/s0277-9536(00)00049-6. [DOI] [PubMed] [Google Scholar]
- 26.Modano D, Sirima BS, Sawadogo A, Sanou I, Paré J, Konaté A, et al. Severe malaria in Burkina Faso urban and rural environment. Parassitologia. 1999;41:251–4. [PubMed] [Google Scholar]
- 27.UNICEF. Malaria prevention and treatment. Prescriber. 2000;18:1–16. [Google Scholar]


