Abstract
Fear of scar rupture is one of risks involved in a post caesarean pregnancy. This had led to an increased rate of repeat cesarean delivery in today's times. Closure of the uterine incision is a key step in cesarean section, and it is imperative that an optimal surgical technique be employed for closing a uterine scar. This technique should be able to withstand the stress of subsequent labor. In the existing techniques of uterine closure, single or double layer, correct approximation of the cut margins, that is, decidua-to-decidua, myometrium to myometrium, serosa to serosa is not guaranteed. Also, there are high chances of inter surgeon variability. It was felt that if a suturing technique which ensures correct approximation of all the layers mentioned above with nil or minimal possibility of inter operator variability existed, there will not be any thinning of lower segment caesarean section (LSCS). Further, a scarred uterus repaired in this manner will be able to withstand the stress of labor in future. We hereby report a new technique for uterine closure devised by us, which incorporates a continuous modified mattress suture technique as a modification of the existing surgical technique of uterine closure.
Keywords: Cesarean section, Continuous modified mattress suture, Uterine closure, Vaginal birth after caesarean
Introduction
Caesarean section is one of the oldest procedures performed in the history of surgery. Since the first documented caesarean delivery in 1020 AD, various modifications have been made in the technique. It was surgery performed as a last resort, mostly peri- or post-portem.[1] Initially, the uterine wound developed in cesarean section was not sutured as it was opined that the contraction and relaxation of the uterus would make the placement of uterine sutures ineffective.[2] It was Lebas who, in 1769, first advocated closure of uterine incision.[2,3] Non-absorbable sutures of those days were left protruding from the wound for later removal. This greatly increased chances of maternal mortality from sepsis. In 1876, Eduardo Porro started performing a subtotal hysterectomy after cesarean section[4] so as to save the mother's life; however, this was at the cost of her future fertility. It was Max Sanger who in 1882 insisted that suturing of the uterus was essential,[5] and he introduced a silver suture that produced minimal tissue reaction.
Much changed in the subsequent centuries, and, presently, cesarean section is the most common surgical procedure performed on women and has become a much safer procedure. However, it confers an increased risk of complications in present as well as future pregnancies. One specific risk factor involved in a post caesarean pregnancy is the fear of scar rupture. Closure of the uterine incision is a key step in cesarean section, particularly given the increasing awareness of future scar dehiscence. It is imperative therefore, that the optimal surgical technique be employed to minimize the morbidity in both the present case and in any future deliveries. Despite this, there is no universally accepted technique for performing cesarean section,[6] and every step in this surgical procedure differs from surgeon to surgeon. In 2005, Berghella et al.[7] and five years later in 2010, Walsh[8] did a comprehensive review of the reported literature on cesarean techniques. Every single step of cesarean section was analyzed based on good quality evidence published.
A Cochrane review[9] of techniques for uterine closure in cesarean section was also published in 2008. It was brought out that single-layer closure was associated with significant reductions in blood loss, operative time and postoperative pain. Hamar et al.[10] randomized 30 women to one or two-layer closure and followed them up with ultrasonographic assessment of the scar remodeling at the 2nd and 6th post-operative weeks. They reported equivalent scar thickness irrespective of the method of closure. Although these data support the use of single-layer closure, effect on future childbearing needs to be kept into consideration. A few retrospective studies[11,12] have brought out higher rates of subsequent uterine rupture in women who had a single layer uterine closure in previous cesarean. Although not consistent across all studies, there remains sufficient concern of a conflict between minimizing short-term complications with the use of single layer closure without adversely affecting subsequent pregnancy outcome. It would seem prudent to consider a woman's reproductive ambitions in determining the correct uterine closure approach. However, if a technique can combine the short-term advantages of single layer and can provide perceived long-term strength to the uterine scar provided by a double layer technique, it would become an ideal suturing technique for uterine closure. Probably an anatomically proper closure of the incision on the uterus would prevent the uterine scar dehiscence in future pregnancies.
In the existing techniques of uterine closure, correct approximation of the cut margins: decidua-to-decidua, myometrium to myometrium, serosa to serosa, are not guaranteed. This may be possibly due to edges getting overlapped; and, after remodeling and the process of the healing, thickness of the site of lower segment caesarean section (LSCS) is significantly reduced. There is also a very high possibility of inter surgeon variability. It was felt that if there is a suturing technique which ensures correct approximation of all the layers mentioned above with nil or minimal possibility of inter operator variability, there will not be any thinning of LSCS site, and scarred uterus repaired in this manner will be able to withstand the stress of labor in future.
We hereby report a new technique for uterine closure (proposed to be called as Babu and Magon's uterine closure technique) devised by us, as a modification of the existing surgical technique of uterine closure. We first performed this new technique in a patient who was a known case of fibroid uterus and had a post LSCS pregnancy. Unwilling for a trial of labor (TOL) for vaginal birth after caesarean (VBAC), she underwent a repeat pre-labor cesarean. Intraoperatively, the previous uterine scar was very thin. The tinned out margins were excised and sutured by the new technique. The approximation and homeostasis was excellent. The patient underwent hysterectomy at a later stage because of the symptomatic fibroids at our institute itself. This provided us with an opportunity to assess the site of the uterine scar repaired by the new technique. There was no thinning at the site of uterine repair. We also compared it with another post-cesarean uterus (uterine rent sutured with conventional double layer technique) taken out at hysterectomy. Thinning was observed at the uterine rent repair site in the latter [Figures 1–3]. It was believed that if the uterus is closed by this new proposed technique at the time of primary LSCS, it could give a good scar, which can withstand the stress of labor or abortion in the future. We do not use the thickness of scar site as the final predictor of uterine scar strength, and to correlate its ability to withstand future stress of labor; however, it cannot be ignored that the perfect approximation of uterine layers by the new technique, and scar formation without any thinning, definitely open up avenues of further trials using this technique vis-à-vis previous techniques for uterine closure following cesarean section.
Figure 1.

Appearance of the lower segment of unscarred uterus at hysterectomy. Note there is no thinning
Figure 3.
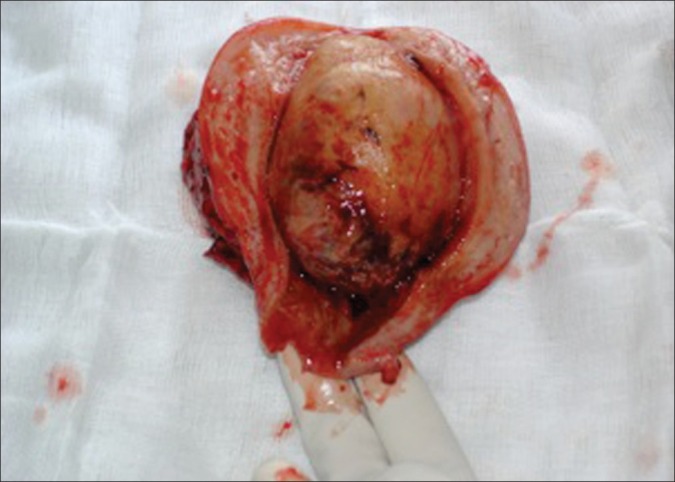
Specimen of uterus removed by hysterectomy of our first patient in which the uterine closure was done by our new technique. Note there is no thinning anywhere in lower segment
Figure 2.

Specimen of the uterus removed by hysterectomy where the lady had undergone a lower segment caesarean section 12 years back and uterus was closed by conventional double layer technique. Note the significant thinning at lower segment, which probably is the site of uterine rent
Our Technique
The existing suturing techniques of uterine closure include: double layer where continuous interlocking is followed by an imbricating second layer; and, single layer where continuous interlocking or non-interlocking sutures are used. In the new technique, the uterus is closed with delayed absorbable suture polyglactin 910 (0) or PGA (0), by continuous modified mattress suture technique in a single layer excluding the decidual layer. The aim of using this method is to ensure the correct anatomical approximation of the deciduas to deciduas, myometrium to myometrium and serosa to serosa layers.
Step 1
After securing the angle of the incision, a full thickness needle bite is taken starting 1 cm away from the margin of the incision and coming out at the junction of the myometrium and decidua of the lower edge of the incision. We then enter at the junction of the myometrium and decidua of the upper edge of the incision, and come out 1 cm away from the margin of the upper edge. This ensures good approximation of the deciduas without overlapping of the decidual margins. The assistant will maintain the traction at this stage.
Step 2
Without changing the direction of the needle, a superficial bite is taken encircling the outer margins, sub peritoneal fascia and outer myometrium from the lower edge and followed by the upper edge, and then the needle bite as described in the first step is started [Figure 4].
Figure 4.
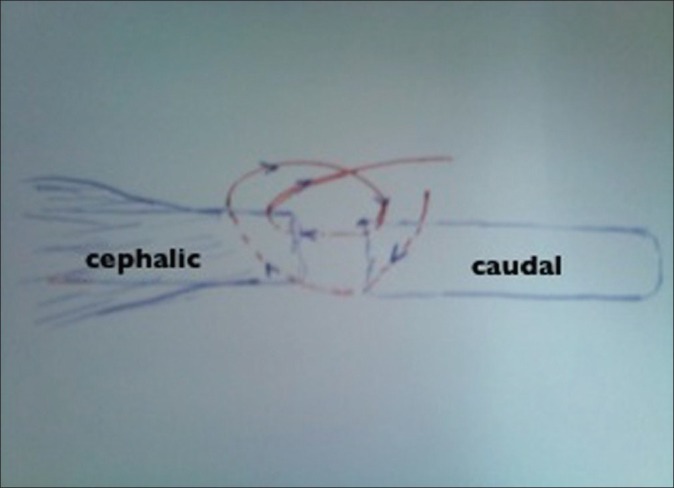
Diagrammatic representation of continuous modified mattress suture of uterine wall used in our study
Step 3
At this stage, two loose loops are formed at the cranial and caudal ends. Surgeon will pull the caudal loop, and the cranial loop gets tightened once the assistant leaves the traction. The surgeon now tightens the caudal loop by pulling the thread. Both the deep and superficial bites are tightened and the assistant maintains the traction of the thread and the surgeon continues the same process for the next bite. This technique will ensure full thickness decidua-to-decidua, myometrium-to-myometrium and serosa-to-serosa approximation of the uterine cut margins and good homeostasis.
Discussion
The immediate requirement of the uterine closure at the time of cesarean is closure of the rent on the uterus and good homeostasis. The conventional double layer or single layer suturing achieves this. However, the remote requirement of a good scar by full thickness healing of the cut margins, which can withstand the stress of labor in future, may not be achieved in the conventional double layers or single layer method due to the nature of the lower segment and difficulty in identifying the cut margins of the uterus due to the process of labor. This leads to poor healing of the uterine wall and results in thinned out scars. The aim of searching for a different technique was to achieve the full thickness approximation of the cut margins, and hence full thickness healing of the uterine incision.
Williams[13] believed that the uterus heals by regeneration of the muscular fibers and not by the scar tissue. Inspection of unopened uterus at repeat cesarean revealed no trace of previous scar, and at the most, an almost invisible linear scar. Schwarz[14] concluded that if the cut surfaces are closely apposed, the proliferation of the connective tissue is minimal, and the normal relation of the smooth muscle to connective tissue in gradually reestablished. This indicates that the approximation of the cut edges is one of the important factors in the healing of the wound on the puerperal uterus. Correct approximation of the cut margins can be achieved and ensured by the new method, that is, the continuous modified mattress suture. Bujold et al.[15] recently evaluated the effects of a prior single-layer closure compared with the double-layer closure on the risk of uterine rupture, and published that prior single-layer closure carries more than twice the risk of uterine rupture compared with the double-layer closure. Authors further advocated that the single-layer closure should be avoided in women who could contemplate future VBAC. More recently, Roberge et al.[16] evaluated the available evidence regarding the association between single-layer closure and uterine rupture. They reviewed nine studies, which included a total of 5810 women. Overall, the risk of uterine rupture during TOL after a single-layer closure was not found to be significantly different from that after a double-layer closure: however, the authors brought out an interesting finding that locked, and not unlocked single-layer closures were associated with a higher uterine rupture risk than the double-layer closure, in women attempting a TOL.
The safe cut off thickness of scar in post LSCS uterus varies from 1.5 to 3.5 mm, and though not a criteria for VBAC, the thinning of the site is the cause of worry. After suturing uterine rent with the new technique, 50 cases were evaluated by trans vaginal sonography (TVS), after 6 months of LSCS and there was no observable thinning of the anterior lower uterine segment. Hence it is assumed that these uteri can withstand the stress of labor. The quantitative analysis of the scar site can be done by postnatal ultra sonography (USG) preferably by TVS or Magnetic resonance imaging (MRI) of the uterus after six months. Involution and remodeling of the LSCS scar site takes more than the normal six weeks; and may be because of the reaction to the suture material while closing the uterus. However, the qualitative assessment of the scar is possible only if the patient delivers without rupturing the uterus. The authors feel that the technique described here has the potential to be the technique of choice for closure for uterus at LSCS in cases where the future reproductive choices of women need be preserved. We call upon the international community to conduct larger randomized controlled trials to assess the strength of uterus closed by this new technique in withstanding TOL. In case this technique withstands the rigors of evidence-based medicine, it can effectively bring down the increasing rates of cesarean delivery throughout the world.
Footnotes
Source of Support: Nil.
Conflict of Interest: The authors declare that no conflicts of interests are associated with this study.
References
- 1.Todman D. A history of caesarean section: From ancient world to the modern era. Aust N Z J Obstet Gynaecol. 2007;47:357–61. doi: 10.1111/j.1479-828X.2007.00757.x. [DOI] [PubMed] [Google Scholar]
- 2.Boley JP. The history of caesarean section. CMAJ. 1991;145:319–22. [PMC free article] [PubMed] [Google Scholar]
- 3.Garrigues HJ. The improved cesarean section. Am J Obstet. 1883;16:33. [Google Scholar]
- 4.Porro E. Della amputazione utero-ovarica come complemento di taglio cesareo. Ann Univ Med Chir (Milan) 1876;237:289–350. [Google Scholar]
- 5.Sanger M. Der Kaiserschnitt. Arch Gynak. 1882;19:370. [Google Scholar]
- 6.Tully L, Gates S, Brocklehurst P, McKenzie-McHarg K, Ayers S. Surgical techniques used during caesarean section operations: Results of a national survey of practice in the UK. Eur J Obstet Gynecol Reprod Biol. 2002;102:120–6. doi: 10.1016/s0301-2115(01)00589-9. [DOI] [PubMed] [Google Scholar]
- 7.Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery. Am J Obstet Gynecol. 2005;193:1607–17. doi: 10.1016/j.ajog.2005.03.063. [DOI] [PubMed] [Google Scholar]
- 8.Walsh AC. Evidence-based cesarean technique. Curr Opin Obstet Gynecol. 2010;22:1105. doi: 10.1097/GCO.0b013e3283372327. [DOI] [PubMed] [Google Scholar]
- 9.Dodd JM, Anderson ER, Gates S. Surgical techniques for uterine incision and uterine closure at the time of caesarean section. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD004732.pub2. CD004732. [DOI] [PubMed] [Google Scholar]
- 10.Hamar BD, Saber SB, Cackovic M, Magloire LK, Pettker CM, Abdel-Razeq SS, et al. Ultrasound evaluation of the uterine scar after cesarean delivery: A randomized controlled trial of one- and twolayer closure. Obstet Gynecol. 2007;110:808–13. doi: 10.1097/01.AOG.0000284628.29796.80. [DOI] [PubMed] [Google Scholar]
- 11.Bujold E, Bujold C, Hamilton EF, Harel F, Gauthier RJ. The impact of a single-layer or double layer closure on uterine rupture. Am J Obstet Gynecol. 2002;186:1326–30. doi: 10.1067/mob.2002.122416. [DOI] [PubMed] [Google Scholar]
- 12.Gyamfi C, Juhasz G, Gyamfi P, Blumenfeld Y, Stone JL. Single-versus double-layer uterine incision closure and uterine rupture. J Matern Fetal Neonatal Med. 2006;19:639–43. doi: 10.1080/14767050600849383. [DOI] [PubMed] [Google Scholar]
- 13.Williams JW. A critical analysis of 21 years experience with cesarean section. Bull Johns Hopkins Hosp. 1921;32:173. [Google Scholar]
- 14.Schwarz O, Paddock R, Bortnic AR. The cesarean scar: An experimental study. Am J Obstet Gynecol. 1938;36:962. [Google Scholar]
- 15.Bujold E, Goyet M, Marcoux S, Brassard N, Cormier B, Hamilton E, et al. The role of uterine closure in the risk of uterine rupture. Obstet Gynecol. 2010;116:43–50. doi: 10.1097/AOG.0b013e3181e41be3. [DOI] [PubMed] [Google Scholar]
- 16.Roberge S, Chaillet N, Boutin A, Moore L, Jastrow N, Brassard N, et al. Single- versus double-layer closure of the hysterotomy incision during cesarean delivery and risk of uterine rupture. Int J Gfynaecol Obstet. 2011;115:5–10. doi: 10.1016/j.ijgo.2011.04.013. [DOI] [PubMed] [Google Scholar]


