Abstract
Hypoparathyroidism can present with neurological complaints like seizures, parasthesias, depression, psychosis, extrapyramidal manifestations and features of raised intracranial pressure. Hypoparathyroidism and pseudohypoparathyroidism are the most common causes of pathological basal ganglia calcification. A 50 year male presented with generalized seizures and extrapyramidal features like tremors and rigidity. Investigations revealed that he had hypocalcemia, hyperphosphatemia and very low PTH levels, CT scan of head showed calcification of bilateral basal ganglia, cerebellum and subcortical white matter of frontal and parietal lobes. He showed remarkable recovery on restoration of normal serum calcium levels. Hypoparathyroidism should be kept in the differential diagnosis of patients presenting with seizures and extrapyramidal features.
Keywords: Basal ganglia calcification, Extrapyramidal features, Hypoparathyroidism, Seizures
Introduction
Hypoparathyroidism can present with neurological complaints like seizures, parasthesias, depression, psychosis, extrapyramidal manifestations and features of raised intracranial pressure. Hypoparathyroidism and pseudohypoparathyroidism are the most common causes of pathological basal ganglia calcification. We present a case of hypoparathyroidism with seizures, extrapyramidal features and basal ganglia calcification. This case highlights the importance of serum calcium estimation in patients of seizure disorder.
Case Report
A 50 year old male presented with abnormal movements in the form of jerky movements of all four limbs associated with tongue bite and urinary incontinence. These abnormal movements were episodic and each episode lasted for 3-4 minutes and was followed by clouding of consciousness for few minutes. The patient started to experience these seizure episodes when he was 25 years of age, the frequency of seizures was initially one to two episodes in 5-6 months. But since last one month the frequency had markedly increased and patient was having convulsions on almost daily basis. Patient was prescribed phenytoin tablets by local practitioner in dose of 300 mg/day but the seizures were not controlled. Patient also developed tremors of both the hands since last 2 months, tremors were more in the left hand as compared to right and they were more prominent at rest.
On examination there was painful spasm of hand on inflating sphygmomanometer cuff above systolic blood pressure (i.e. Trousseau's sign was positive), he was fully conscious well oriented, appearance and behavior were normal, there were no hallucination and delusions and his memory and speech were normal, all the cranial nerves were intact, coarse pill rolling type of tremors were present at rest in both the hands but more in left hand as compared to right hand. Cog wheel rigidity was present in both the upper limbs, power was normal in all four limbs and sensations were intact.
No scar on the neck to suggest any previous neck surgery was seen, there was no candidiasis or vitiligo neither there was any hearing loss. However cataracts were present in both the eyes.
On investigation his haemoglobin was 13.2 gm/dl, total leucocyte count 9400/μL, differential leucocyte count showed 76% neutrophils and 24% lymphocytes. Blood sugar 90 mg%, blood urea 27 mg% and serum creatinine 0.8 mg%. Alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase and serum bilirubin were all with in normal range. His serum albumin was 4.0 gm/dl. Serum electrolytes were sodium 136 meq/L, potassium 4.2 meq/L, calcium 6.11 mg/dl (normal range 8.0-10.4 mg/dl), ionized calcium 3.0 mg/dl (normal range 4.6-5.4 mg/dl), serum phosphate 5.7 mg/dl (normal range 2.5-4.5 mg/ dl) and serum magnesium was 2.12 mg/dl (normal range 1.3-2.5 mg/dl). His parathormone level was 3.6 pg/ml (normal range 15-68 pg/ml). CT scan of the brain revealed bilaterally symmetrical hyperdense lesions with CT value of calcification in basal ganglia, thalami, white matter of cerebellar hemispheres and subcortical white matter of bilateral frontal and parietal lobes [Figures 1 and 2].
Figure 1.
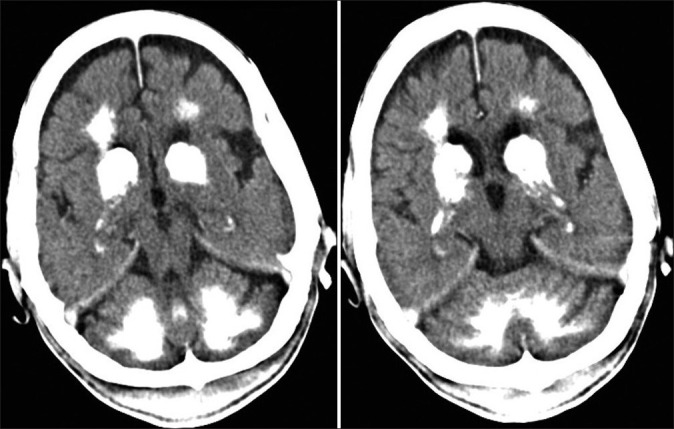
Non-contrast enhanced CT scan at the level of mid-brain showing multiple bilaterally symmetrical hyperdense lesions with CT value of calcification in basal ganglia, thalami and white matter of cerebellar hemispheres
Figure 2.
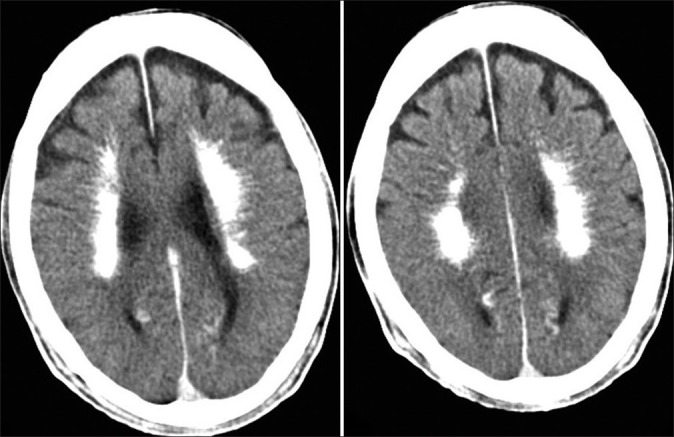
Non-contrast enhanced CT scan at the level of roof of lateral ventricle showing bilaterally symmetrical hyperdense lesions with CT value of calcification in subcortical white matter of bilateral frontal and parietal lobes
On the basis of seizures, extrapyramidal features, bilateral cataracts, positive Trousseau's sign, hypocalcemia, high phosphate levels and low PTH levels our patient was diagnosed as a case of hypoparathyroidism with extrapyramidal features and seizures due to hypocalcemia.
Calcitriol 0.5 μg/day and calcium 1 gm/day was started. Patient's calcium levels returned to normal range with this treatment. Although antiepileptic drugs were not indicated in this patient but we put him on sodium valproate 500 mg twice daily with the aim to withdraw the drug slowly, this was done as the patient was taking phenytoin tablets for a very long duration. With the normalization of serum calcium patient became seizure free and the parkinsonian features (tremors and cog wheel rigidity) also improved remarkably, patient was not prescribed any anti-parkinsonian drug for control of extrapyramidal features. Patient is in follow up for the last four months and did not have even a single seizure episode.
Discussion
Hypoparathyroidism can occur due to acquired or hereditary causes.[1] Acquired hypoparathyroidism is usually due to inadvertent removal of parathyroid gland during neck surgeries for hyperthyroidism, or it can result due to removal of too much parathyroid gland during surgery for hyperparathyroidism.[1] Other rare causes of acquired hypoparathyroidism include radiation induced damage subsequent to radio iodine therapy, sarcoidosis, haemochromatosis, haemosiderosis, Wilson's disease and metastatic infiltration of parathyroid gland.[1,2] Hereditary hypoparathyroidism can occur as an isolated defect without other endocrine or dermatological manifestations (then it is referred to as idiopathic hypoparathyroidism) but more typically hereditary hypoparathyroidism occur along with other developmental anomalies such as defective development of thymus or failure of adrenals, thyroid or ovaries along with mucocutaneous candidiasis, alopecia and vitiligo.[1] Idiopathic and hereditary forms of hypoparathyroidism usually manifest with in the first decade of life, although they can present later.[1] The patient in the above presentation does not underwent any neck surgery, neither there was any feature suggestive of other systemic diseases or developmental anomalies as mentioned above therefore he was most probably suffering from idiopathic hypoparathyroidism.
The common clinical features of hypoparathyroidism are mainly due to hypocalcaemia and include circumoral numbness, parasthesias, spasms of carpal and pedal muscles, laryngeal spasm, tetany and seizures.[2] Important signs on physical examination include Chovstek's sign (twitching of upper lip on tapping the cheek along the course of facial nerve) and Trousseau's sign (painful carpal spasm elicited by inflating sphygmomanometer cuff 20 mm Hg above systolic blood pressure for 3 minutes). Neurological manifestations apart from seizures include raised intracranial tension, papillioedema, irritability, depression, psychosis, extrapyramidal and cerebellar manifestations.[1,3–8] Other features include chronic changes in finger nails and hairs, extra osseous calcification and lenticular cataracts, heart failure and QT prolongation.[1] our patient had seizures and extrapyramidal manifestations like rigidity and tremors. Tonic clonic seizures occurring with hypoparathyroidism have been reported previously, Glaser et al. described 4 patients of hypoparathyroidism and pseudohypoparathyroidism with seizures,[9] Bindu et al. described 2 cases of tonic clonic seizures occurring with hypoparathyroidism,[10] Armelisasso et al. also described occurrence of tonic clonic seizure in a 36 year old male with hypoparathyroidism,[11] Garg et al. reported tonic clonic seizures in a female patient with hypoparathyroidism,[7] Gupta et al. also described a patient with recurrent seizures and altered mental status who was later diagnosed as a case of hypoparathyroidism.[6]
Laboratory evaluation to diagnose hypoparathyroidism should include serum calcium (total as well as ionized), phosphorous, serum albumin, creatinine, magnesium, intact PTH and 25-hydroxyvitamin D levels.[2] Serum calcium levels are low, phosphate levels are high and intact PTH level are inappropriately low in hypoparathyroidism. Patients with pseudohypoparathyroidism also have low calcium, high phosphorus but high PTH levels.[2] Measurement of 25-hydroxyvitamin D levels is important to rule out vitamin D deficiency as a cause of hypocalcemia. Measurement of magnesium is also important as magnesium depletion or excess can also cause hypocalcaemia by inducing functional hypoparathyroidism.[12] Hypoparathyroidism was diagnosed in our patient on the basis of low serum calcium (ionized and total), high phosphate and very low PTH levels in face of normal Magnesium levels.
Electro encephalo gram (EEG) in the presence of hypocalcemia can show evolution from alpha through theta and delta dominance, generalized spikes and sharp-waves burst of delta activity with sharp components.[13] Unfortunately facility of EEG was not available at our center.
Radiological feature of hypoparathyroidism include intracranial calcification most commonly involving bilateral basal ganglia.[14] Calcification can also occur in cerebellum, sub cortical white matter, corona radiata and thalamus.
Intracranial calcification can also be physiological in 0.3-1.5% of subjects.[15] Most common pathological causes of basal ganglia calcification are hypoparathyroidism and pseudohypoparathyroidism. Other causes of basal ganglia calcification are Fahr's syndrome, tuberous sclerosis, Cockayne's syndrome, mitochondrial disease, familial idiopathic basal ganglia calcification, diffuse neurofibrillary tangles with calcification, Down's syndrome and post infectious.
Treatment of hypoparathyroidism involves replacement with vitamin D or 1,25 (OH)2D3 (calcitriol) along with high dose of calcium. For most of the patients vitamin D in a dose of 40,000-120,000 U/day (1-3 mg/day) with elemental calcium in a dose of ≥1 gm/day are usually satisfactory.[1] Oral calcium and vitamin D restore the overall calcium-phosphate balance but do not reverse hypercalcuria seen in hypoparathyroidism, therefore after vitamin D and calcium replacement excessive urinary calcium excretion can lead to kidney stone formation. Thiazides diuretics can lower urinary calcium excretion in such patients.[1]
Subcutaneous synthetic human parathyroid hormone (PTH 1-34) is also being used now a days in treatment of hypoparathyroidism.[16]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Potts JT. Diseases of the parathyroid gland and other hyper and hypocalcemic disorders. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, et al., editors. Harrison's principles of internal medicine. 17th ed. New York: McGraw Hills; 2008. pp. 2377–96. [Google Scholar]
- 2.Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391–403. doi: 10.1056/NEJMcp0803050. [DOI] [PubMed] [Google Scholar]
- 3.Pleet AB, David JS. Neurological aspects of endocrine disturbance. In: Baker AB, Baker LH, editors. Clinical neurology. Philadelphia: JB Lippincott company; 1993. p. 24. [Google Scholar]
- 4.Abe S, Tojo K, Ichida K, Shigematsu T, Hasegawa T, Morita M, et al. A rare case of idiopathic hypoparathyroidism with varied neurological manifestations. Intern Med. 1996;35:129–34. doi: 10.2169/internalmedicine.35.129. [DOI] [PubMed] [Google Scholar]
- 5.Fonseca OA, Calverley JR. Neurological manifestation of hypoparathyroidism. Arch Intern Med. 1967;120:202–6. [PubMed] [Google Scholar]
- 6.Idiopathic hypoparathyroidism: An unusual cause of acute encephalopathy. BMJ Case Reports. 2011. [Accessed March 24, 2012]. at http://casereports.bmj.com/content/2011/bcr.12.2010.3593.full . [DOI] [PMC free article] [PubMed]
- 7.Garg RK, Garg N, Tandon N, Khurana ML, Ammini AC. Idiopathic hypoparathyroidism presenting as epilepsy in a 40 years female. Neurol India. 1999;47:244–5. [PubMed] [Google Scholar]
- 8.Hossain M. Neurological and psychiatric manifestations in idiopathic hypoparathyroidism: Response to treatment. J Neurol Neurosurg Psychiatry. 1970;33:153–6. doi: 10.1136/jnnp.33.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glaser GH, Levy L. Seizures and idiopathic hypoparathyroidism.A clinical-electroencephalographic study. Epilepsia. 1960;1:454–65. doi: 10.1111/j.1528-1157.1959.tb04280.x. [DOI] [PubMed] [Google Scholar]
- 10.Bindu M, Harinarayana CV. Hypoparathyroidism: A rare treatable cause of epilepsy - report of two cases. Eur J Neurol. 2006;13:786–8. doi: 10.1111/j.1468-1331.2006.01287.x. [DOI] [PubMed] [Google Scholar]
- 11.Armelisasso C, Vaccario ML, Pontecorvi A, Mazza S. Tonic-clonic seizures in a patient with primary hypoparathyroidism: A case report. Clin EEG Neurosci. 2004;35:97–9. doi: 10.1177/155005940403500209. [DOI] [PubMed] [Google Scholar]
- 12.Tong GM, Rude RK. Magnesium deficiency in critical illness. J Intensive Care Med. 2005;20:3–17. doi: 10.1177/0885066604271539. [DOI] [PubMed] [Google Scholar]
- 13.Castilla-Guerra L, del Carmen Fernández-Moreno M, López-Chozas JM, Fernández-Bolaños R. Electrolytes disturbances and seizures. Epilepsia. 2006;47:1990–8. doi: 10.1111/j.1528-1167.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- 14.Fulop M, Zeifer B. Case report: Extensive brain calcification in hypoparathyroidism. Am J Med Sci. 1991;302:292–5. doi: 10.1097/00000441-199111000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Verulashvili IV, Glonti LSh, Miminoshvili DK, Maniia MN, Mdivani KS. Basal ganglia calcification: Clinical manifestations and diagnostic evaluation. Georgian Med News. 2006;140:39–43. [PubMed] [Google Scholar]
- 16.Winer KK, Ko CW, Reynolds JC, Dowdy K, Keil M, Peterson D, et al. Long-term treatment of hypoparathyroidism: A randomized controlled study comparing parathyroid hormone-(1-34) versus calcitriol and calcium. J Clin Endocrinol Metab. 2003;88:4214–20. doi: 10.1210/jc.2002-021736. [DOI] [PubMed] [Google Scholar]


