Abstract
Background:
Enhanced recovery program (ERP) was implemented to optimize the hospital stay in total hip arthroplasty. This study assessed the effects of optimizing preoperative and perioperative care using enhanced recovery (ER) on patients undergoing Total hip arthroplasty.
Materials and Methods:
We compared a prospective group of 64 patients on the ER program with a historic cohort of 63 patients that received conventional care (non ER).
Results:
ER patients were discharged earliest from hospital [mean length of stay (LOS) 5.3 days, median 4; P < 0.001] as compared to a mean of 8.3 days among non ER patients. Comparison based on American Association of Anesthesiologists (ASA) grades, preoperative hemoglobin, and body mass index (BMI) revealed that patients with ASA grade 3, preoperative hemoglobin of <14 g/dl, and BMI >30 on ER program spent shorter time in hospital as compared to the non ER's conventionally treated patients with more favorable physiological parameters of ASA grade 1 and 2, preoperative hemoglobin of >14 g/dl, and BMI <30.
Conclusion:
The ER protocol is universally beneficial and confers an advantage regardless of the patients’ preoperative condition.
Keywords: Enhanced recovery program, length of stay, total hip arthroplasty
INTRODUCTION
Enhanced recovery (ER) programs have been implemented in general surgery and have helped optimize preoperative, perioperative, and postoperative factors to reduce the physiological and psychological stress of surgery.1 Several factors are responsible for functional deterioration and increased risk of morbidity after major surgical procedures, and include the surgical stress response, increased cardiac demand, impairment of pulmonary function, changes in coagulation and fibrinolysis, catabolism and loss of muscle mass, sleep disturbance, and paralytic ileus.2
The ER program begins with preoperative care and detailed patient education prior to admission to hospital. Strictly defined discharge criteria and a prescheduled discharge plan are implemented.3 Postoperative care includes early introduction of oral nutrition supplements, early mobilization, and restricted opiate use to minimize nausea and ileus.4 The multimodal rehabilitation program has enabled early restoration of gastrointestinal function, reduction of fatigue, and improved physical performance in some general surgical procedures.5 Such protocols have also reduced length of hospital stay (LOS).6,7
With approval from the department of clinical governance at our hospital, we implemented an ER program for patients undergoing elective total hip arthroplasty (THA) and compared the results with a similar patient population who had undergone hip replacement surgery prior to the advent of the ER program.
MATERIALS AND METHODS
Between November 2006 and January 2008, 64 consecutive patients underwent total hip arthroplasty on an ER program. The control group consisted of 63 consecutive patients who underwent THA between November 2004 and October 2006 prior to the ER program (non ER). The non ER data were obtained retrospectively from patient records. All patients were treated under the care of the senior author (PP). ER data were collected prospectively and analyzed.
There was no difference in the age of patients. The mean age for the ER patients was 70.5 years (range 48–89 years) and for the non ER group was 72.5 years (range 56–91 years, P=0.9). There were 27 men and 37 women in the ER group and 22 men and 41 women in the non ER group.
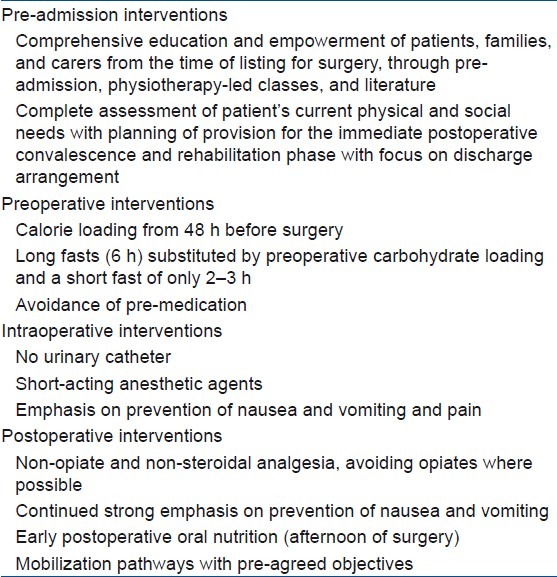
The ER program incorporates a multidisciplinary team composed of surgeons, nurses, physiotherapists, and occupational therapists, and includes the patient as an active participant. The program is followed clearly in a stepwise manner to maximize efficiency of the care pathway [Table 1].
Table 1.
Enhanced orthopedic recovery in summary
The program was outlined to each patient being admitted for a primary joint replacement. A patient information leaflet was supplied at the initial clinic visit and a mini pre-assessment check carried out at that stage. This identifies those patients who need to see an anesthetist prior to surgery.
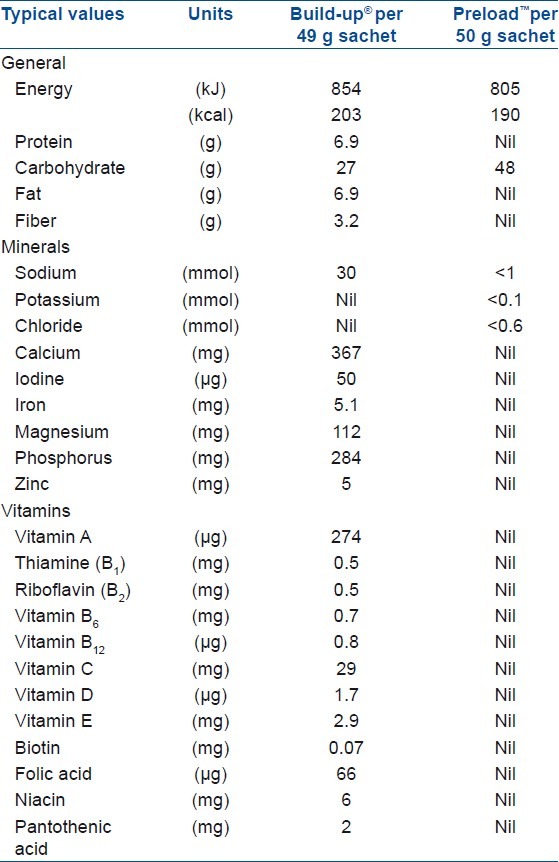
The key aspects of ER were explained again at the pre-assessment clinic prior to admission. At the pre-assessment clinic, each patient undergoes the routine protocol for pre-assessment. The ER program was emphasized again and patients were supplied with supplement drinks (Build-up® by Nestle Nutrition) [Table 2] to be taken 2 days before hospital admission in the morning. Patients were asked to take three sachets of Build-up dissolved in 150 ml of water 2 days before surgery and two sachets 1 day before surgery.
Table 2.
Food values and calorie content of supplemental drinks
All patients attended a pre-admission joint replacement class run by the physiotherapists and occupational therapists and were encouraged to bring a member of their family or a friend for support. This class lasts for approximately 1 h. The ER program was discussed in detail again. Patients were usually admitted on the eve of surgery.
On the day of admission, which is a day before the operation, the patient was given high carbohydrate drink of two sachets of preload™ (by Vitaflo) [Table 2 dissolved in 400 ml of water at 8 p.m. in the evening. A further high carbohydrate drink with one sachet dissolved in 400 ml of water was given 3 h before surgery. This minimizes the adverse metabolic effects of starvation. All patients were given the high energy drink irrespective of any comorbidities, e.g. diabetes or high body mass index (BMI). The high energy drink helps reduce The risk of anesthetic and starvation-induced diabetes, and helps maintain higher energy levels following the operation.
The physiological benefits of managing the metabolic insult of a prolonged starvation period followed by the traumatic insult of surgery are central to our intervention8 and, we believe, are new to orthopedics. Traditional patient starvation regimes (nil by mouth for 6 h) are based on the premise that this will reduce the incidence of pulmonary aspiration. A recent review, however, has provided no scientific support for this practice.9 Recommendations now suggest clear fluids up until 2 h before the initiation of anesthesia and a 6 h solid food fast. This reduces preoperative thirst, hunger, and anxiety, and significantly reduces postoperative insulin resistance.10 Preoperative oral carbohydrates also reduce postoperative nausea and vomiting, which can prevent the rapid postoperative recovery of the patient.11
All patients were given spinal or epidural anesthesia and propofol was used for sedation and maintenance of light general anesthesia which helps reduce postoperative nausea and vomiting. Shortacting opiates decrease the incidence of opiate toxicity, and accurate fluid resuscitation avoids iatrogenic hyperchloremic acidosis and fluid overload.
Postoperatively, the patient was sat up in bed in the recovery room and oral fluids were commenced. Pneumatic intermittent calf compression was instituted to minimize the risk of deep vein thrombosis.
In the ward, the patient was encouraged to sit up, eat, and drink almost immediately. There was an emphasis on oral intake with protein and carbohydrate-rich drinks, rather than reliance on intravenous fluid administration. They were given two sachets of Build-up drink on the evening after surgery and three sachets for 3 days thereafter. The strategy aims to maintain the gut flora, preserve immune function, and optimize wound healing and recovery.12 The multimodal approach to perioperative nutrition is cumulative in its benefits. Dedicated joint replacement physiotherapy started on the evening of the operation and patients were encouraged to sit out of bed in the chair. Enoxaparin (40 mg) was administered subcutaneously in the evening following surgery and for the duration of the in-patient stay only. However, the antithrombotic effects of early mobilization have been shown to reduce the incidence of thromboembolic events after lower limb joint replacement surgery.13
Wound drains were removed on the first postoperative day. Patients were mobilized with the assistance of the physiotherapist. Urinary catheterization was avoided, if at all possible. Mobilization was “goal-oriented.” The patient was encouraged to reach a white board at the end of the ward and to sign it on reaching that target. Discharge plans were again confirmed.
At discharge, patients were escorted to the hospital exit by a physiotherapist or nurse and shown how to get in and out of a car safely. Following discharge, wound care was undertaken either by a district nurse or practise nurse in the community. All patients were reviewed by a physiotherapist between 1 and 3 weeks following discharge, but they could contact the hospital ward should they have any concerns.
All patients were scored according to the American Association of Anesthesiologists (ASA) physical status classification system, preoperative hemoglobin (Hb), and BMI. The LOS (defined as the number of nights spent in hospital) was recorded.
Ethics
We obtained approval from the Department of Clinical Governance at our hospital and followed ethical standards on human experimentation. We performed the procedure in accordance with the Helsinki Declaration of 1975, as revised in 2000, to implement an ER program for patients undergoing elective total hip arthroplasty.
RESULTS
The two groups were similar in size (non ER=63, ER=64). The average age of the ER group was 70.1 years (range 48–89 years, SD=8.79). The average age of the non ER group was 72.5 years (range 56–91 years, SD=8.72). This difference was not statistically significant (P=0.9). However, the BMI of the ER group was significantly higher than the non ER group (29.4 vs. 27.9, P=0.1). The ER patients spent a significantly shorters time in hospital at an average 5.3 days (median 4 days) as against an average 8.3 days (median 7 days) spent by the non ER group (P < 0.001).
We looked at the effect of preoperative Hb, ASA grade, and BMI to determine if they had any influence on LOS. We divided the ER and non ER groups into two subgroups depending on preoperative Hb levels (<14 g/dl and ≥14 g/dl, respectively). It was observed that patients in the ER group with a preoperative Hb of ≥14 g/ dl spent a significantly shorter time in hospital (4.37 days) compared to 6.60 days spent by the non ER group (P < 0.01) [Figure 1]. In the group with an Hb level <14 g/dl, it was found that though the hospital stay was longer for both groups, the non ER group had a significantly longer period of hospitalization (9.16 days) than the ER group (6.02 days, P < 0.01).
Figure 1.
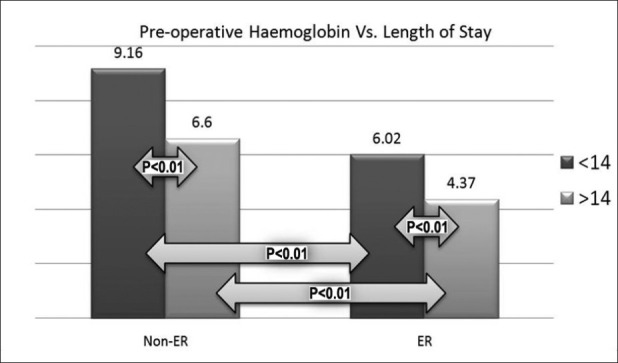
Bar graph showing stay in the two groups (pre-op Hb <14 gm% and >14 gm%) within each cohort. Those with a higher pre-op Hb had significantly shorter stay in days when compared with their lower Hb counterparts in each cohort (ER and non ER), and there was a significant difference between similar groups in each cohort
The non ER patients with an Hb of <14 g/dl spent an average 3.14 days more in hospital than the similar ER group. The patients in the non ER group with an Hb of ≥14 g/dl spent longer in hospital (an average 2.23 days more) than the similar ER group. The ER patients with an Hb of <14 g/dl spent a shorter period (0.58 days less) in hospital compared with non ER patients with an Hb of >14 g/dl, although this was not statistically significant (P = 0.45).
Analysis of the ASA scores showed that the non ER subgroup of ASA 1 and 2 patients spent an average 7.86 days in hospital [Figure 2] compared to 9.46 days spent by ASA 3 patients. However, this difference between the two groups was not statistically significant (P=0.33). In the ER group, however, patients with ASA 1 and 2 had significantly shorter hospital stay (4.72 days) compared to ASA 3 patients who spent an average of 6.79 days in hospital (P=0.01). ASA 3 patients in the ER group spent an average 1.07 days less than the ASA 1 and 2 patients of the non ER group (P=0.08). The patients with ASA 1 and 2 in the ER group spent a significantly shorter time of 4.72 days in the hospital compared to 7.86 days spent by the ASA 1 and 2 patients in the non ER group (P < 0.01).
Figure 2.
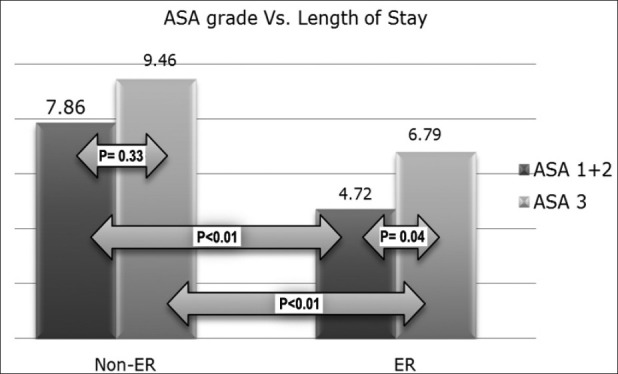
Bar graph showing hospital stay in days for the two groups (ASA 1+2 and ASA 3) within each cohort. Those with ASA 3 rating had a longer stay in both cohorts. Both groups had significantly shorter stay in the ER cohort
The patients were split into two further subgroups of BMI (<30 and ≥30). Those in the ER group with a BMI <30 spent significantly less time in hospital (4.80 days) compared to the patients in the non ER group (8.60 days, P < 0.01) [Figure 3]. ER patients with a BMI >30 spent 6.3 days in the hospital compared to 7.7 days spent by non ER patients (P < 0.01). There was no significant difference in hospital stay between the two non ER subgroups (P=0.5). In the ER group, there was a significant difference between these two cohorts. Patients with a BMI of <30 had an average LOS of 4.8 days, compared to an average of 6.3 days for those with BMI of >30 (P=0.04). It was again observed that ER patients with a BMI of >30 spent an average 2.3 days less in hospital as against those of the non ER group with BMI of <30. Overall, both the groups had significantly shorter stays in the ER cohort.
Figure 3.
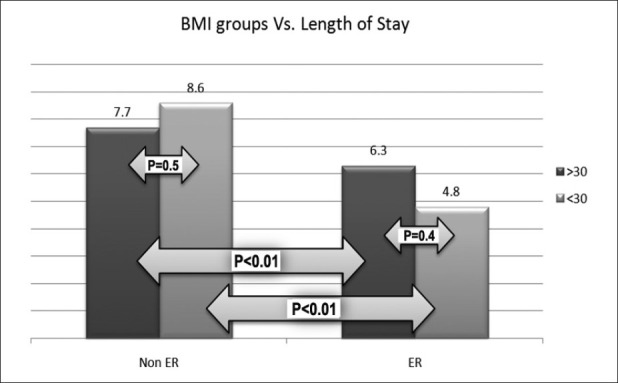
Bar graph showing hospital stay in days in the two groups (BMI <30 and >30) within each cohort. Within the non ER cohort, there was no significant difference between the two groups; however, those with lower BMI had significantly shorter stay in the ER cohort. Overall, both groups had significantly shorter stay in the ER cohort
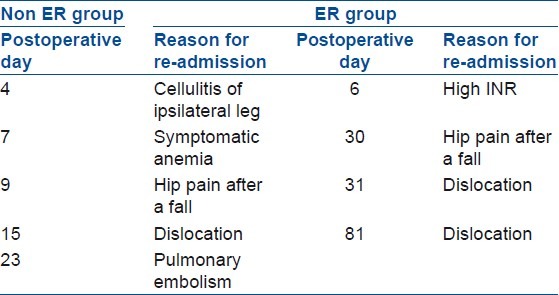
The readmission and complication rates were similar in both the groups and are summarized in Table 3. There was no statistical difference (P=0.57) in the rate of dislocations, with two in the ER group as compared to one in the non ER group.
Table 3.
Complications and re-admissions
DISCUSSION
Discharge planning is a routine feature of health systems in many countries. The aim is to reduce hospital length of stay and unplanned readmission to hospital, and improve the coordination of services following discharge from hospital, thereby bridging the gap between hospital and place of discharge.14 Furthermore, the risk and morbidity associated with surgical procedures has been steadily decreasing in recent decades, primarily because of improvements in patient preparation for surgery and anesthetic and surgical techniques.2 Within the setting of inpatient recovery following major joint replacement, increased length of stay is often attributed to patient factors such as BMI, existing co-morbidities, and age.15 Our two cohorts (ER and non ER) had the same profile with respect to these factors. We compared preoperative Hb, ASA grade, and BMI to length of stay, between our two matched groups. Further subdivision of the groups was made to separate out the so-called “healthier” patients that would be expected to have a shorter LOS. However, we found that despite subdivision of each cohort (ER and non ER) into groups, ER patient groups still demonstrated a significantly reduced hospital stay. Conlon et al. (2008) in study looking at Hb levels on discharge and change in quality of life scores from preoperative to postoperative in patients over 65 years of age who had undergone primary hip arthroplasty has shown that patients with lower Hb on discharge consistently reported less improvement.16
In our study group, every attempt was made to minimize the intraoperative blood loss, and therefore a higher preoperative Hb was advantageous for postoperative recovery and this was reflected in the early discharge of ER patients with an Hb of >14 g/dl (average 4.37 days). The non ER patients with preoperative Hb of >14 g/dl spent slightly longer in hospital than the ER patients with a preoperative Hb of <14 g/dl, suggesting that the ER program aided postoperative recovery and enabled earlier discharge. This shows the effectiveness of the ER program in both Hb subgroups.
The ASA score is a rating given to each patient by the anesthetist before anesthesia. It was designed originally as a standardized way to convey information about the patient's overall health status and allow outcomes to be stratified by a global assessment of their severity of illness. The ASA score is used to estimate operative risk and it correlates well with surgical and anesthetic mortality and morbidity.15,17–21 Our study confirms that ER patients with ASA scores of 1 or 2 and ASA 3 patients spent 39.9% and 28.2% less time, respectively, in the hospital. It is also of note that with the implementation of the ER program, the postoperative LOS of ASA 3 patients was reduced by 13.6% when compared with ASA 1 and 2 patients in the non ER group.
BMI for an individual is their weight in kilograms (kg) divided by their height in meters squared (m2). This correlates with their total body fat.22 Obesity is defined as23 a BMI >30 kg/m2 and we divided our patients into two groups of BMI greater or less than 30 kg/m2 to determine the effect on the LOS. Sadr Azodi et al,24 reported a mean increase in hospital stay in patients with a BMI of <24.9 undergoing total hip arthroplasty surgery, when compared to patients with a BMI ≥25 (from 9 to 10 days). Dall et al,25 reported an increase from 7.9 to 8.2 days amongst their patients with BMI of <30 and ≥30, respectively. Our study clearly demonstrates the benefit of the ER program with patients in the ER group having a BMI <30 spending nearly half as much time in hospital (4.8 days) compared to 7.9 and 9 days reported in the above studies. The results in these studies are similar to the results of the non ER patients. The ER patients in the more favorable subgroups (Hb > 14, BMI < 30, and ASA 1and2) had a significantly reduced LOS when compared to other ER patients in less favorable subgroups (Hb < 14, BMI > 30, and ASA 3). It was also observed that patients with favorable parameters in the non ER group took longer to be discharged from the hospital when compared with patients with less favorable parameters in the ER group.
This study clearly demonstrates the advantages of the ER program. This program resulted in an overall 36.5% reduction in LOS in patients undergoing total hip arthroplasty surgery. The ER protocol confers an advantage for recovery even in less healthy or obese patients without affecting the complication or readmissions.
To conclude this program to be effective, it is imperative that the patient is actively involved throughout the pre- and perioperative period. It requires a motivated group of health care providers committed to the program. This program has brought about significant benefits for both the hospital and the patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.King PM, Blazeby JM, Ewings P, Franks PJ, Longman RJ, Kendrick AH, et al. Randomized clinical trial comparing laparoscopic and open colorectal cancer within an enhanced recovery program. Br J Surg. 2006;93:300–8. doi: 10.1002/bjs.5216. [DOI] [PubMed] [Google Scholar]
- 2.Kehlet H. Multimodal approach to control postoperative pathophysiology abd rehabilitation. Br J Anaesth. 1997;78:606–17. doi: 10.1093/bja/78.5.606. [DOI] [PubMed] [Google Scholar]
- 3.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630–41. doi: 10.1016/s0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- 4.Kehlet H, Dahl JB. Anesthesia, surgery and challenges in postoperative recovery. Lancet. 2003;362:1187–92. doi: 10.1016/S0140-6736(03)14966-5. [DOI] [PubMed] [Google Scholar]
- 5.Basse L, Raskov HH, Hjort Jakobsen D, Sonne E, Billesbølle P, Hendel HW, et al. Accelerated postoperative recovery program after colonic resection improves physical performance, pulmonary function and body composition. Br J Surg. 2002;89:446–53. doi: 10.1046/j.0007-1323.2001.02044.x. [DOI] [PubMed] [Google Scholar]
- 6.Delaney CP, Zutshi M, Senagore AJ, Remzi FH, Hammel J, Fazio VW. Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum. 2003;46:851–9. doi: 10.1007/s10350-004-6672-4. [DOI] [PubMed] [Google Scholar]
- 7.Basse L, Thorbøl JE, Løssl K, Kehlet H. Colonic surgery with accelerated rehabilitation or conventional care. Dis Colon Rectum. 2004;47:271–7. doi: 10.1007/s10350-003-0055-0. [DOI] [PubMed] [Google Scholar]
- 8.Fearon KC, Luff R. The nutritional management of surgical patients: enhanced recovery after surgery. Proc Nutr Soc. 2003;62:807–11. doi: 10.1079/PNS2003299. [DOI] [PubMed] [Google Scholar]
- 9.Ljungqvist O, Søreide E. Preoperative fasting. Br J Surg. 2003;90:400–6. doi: 10.1002/bjs.4066. [DOI] [PubMed] [Google Scholar]
- 10.Thorell A, Efendic S, Gutniak M, Häggmark T, Ljungqvist O. Insulin resistance after abdominal surgery. Br J Surg. 1994;81:59–63. doi: 10.1002/bjs.1800810120. [DOI] [PubMed] [Google Scholar]
- 11.Hausel J, Nygren J, Thorell A, Lagerkranser M, Ljungqvist O. Randomized clinical trial of the effects of oral preoperative carbohydrates on postoperative nausea and vomiting after laparoscopic cholecystectomy. Br J Surg. 2005;92:415–21. doi: 10.1002/bjs.4901. [DOI] [PubMed] [Google Scholar]
- 12.Soop M, Carlson GL, Hopkinson J, Clarke S, Thorell A, Nygren J, et al. Randomized clinical trial of the effects of immediate enteral nutrition on metabolic responses to major colorectal surgery in an enhanced recovery protocol. Br J Surg. 2004;91:1138–45. doi: 10.1002/bjs.4642. [DOI] [PubMed] [Google Scholar]
- 13.Pearse EO, Caldwell BF, Lockwood RJ, Hollard J. Early mobilisation after conventional knee replacement may reduce the risk of postoperative venous thromboembolism. J Bone Joint Surg Br. 2007;89:316–22. doi: 10.1302/0301-620X.89B3.18196. [DOI] [PubMed] [Google Scholar]
- 14.Shepperd S, McClaran J, Phillips CO, Lannin NA, Clemson LM, McCluskey A, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2010;1:CD000313. doi: 10.1002/14651858.CD000313.pub3. [DOI] [PubMed] [Google Scholar]
- 15.Cullen DJ, Apolone G, Greenfield S, Guadagnoli E, Cleary P. ASA physical status and age predict morbidity after three surgical procedures. Ann Surg. 1994;220:3–9. doi: 10.1097/00000658-199407000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conlon NP, Bale EP, Herbison GP, McCarroll M. Postoperative anemia and quality of life after primary hip arthroplasty in patients over 65 years old. Anesth Analg. 2008;106:1056–61. doi: 10.1213/ane.0b013e318164f114. [DOI] [PubMed] [Google Scholar]
- 17.Cullen DJ, Nemeskal AR, Cooper JB, Zaslavsky A, Dwyer MJ. The effect of pulse oximetry, age and ASA physical status on the frequency of patients admitted unexpectedly to a post operative intensive care unit and the severity of their anesthesia related complications. Anesth Analg. 1992;74:181–8. doi: 10.1213/00000539-199202000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Djokovic JL, Hedley-Whyte J. Prediction of outcome of surgery and anesthesia in patients over 80. JAMA. 1979;242:2301–6. [PubMed] [Google Scholar]
- 19.Owens WD, Dykes MH, Gilbert JP, McPeek B, Ettling MB. Development of two indices of postoperative morbidity. Surgery. 1975;77:586–92. [PubMed] [Google Scholar]
- 20.Tiret L, Desmonts JM, Hatton F, Vourc’h G. Complications associated with anesthesia-a prospective study in France. Can Anaesth Soc J. 1986;33:336–44. doi: 10.1007/BF03010747. [DOI] [PubMed] [Google Scholar]
- 21.Vacanti CJ, VanHouten RJ, Hill RC. A statistical analysis of the relationship of physical status to postoperative mortality in 68,388 cases. Anesth Analg. 1970;49:564–6. [PubMed] [Google Scholar]
- 22.Bray GA. Overweight is risking fate: Definition, classification, prevalence and risks. Ann NY Acad Sci. 1987;499:14–28. doi: 10.1111/j.1749-6632.1987.tb36194.x. [DOI] [PubMed] [Google Scholar]
- 23.Spicer DD, Pomeroy DL, Badenhausen WE, Schaper LA, Jr, Curry JI, Suthers KE, et al. Body Mass Index as a predictor of outcome in total knee replacement. Int Orthop. 2001;25:246–9. doi: 10.1007/s002640100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sadr Azodi O, Bellocco R, Eriksson K, Adami J. The impact of tobacco use and body mass index on the length of stay in the hospital and risk of postoperative complications among patients undergoing total hip replacement. J Bone Joint Surg Br. 2006;88:1316–20. doi: 10.1302/0301-620X.88B10.17957. [DOI] [PubMed] [Google Scholar]
- 25.Dall GF, Ohly NE, Ballantyne JA, Brenkel IJ. The influence of preoperative factors on the length of in-patient stay following primary total hip replacement for osteoarthritis. A multivariate analysis of 2302 patients. J Bone Joint Surg Br. 2009;91:434–40. doi: 10.1302/0301-620X.91B4.21505. [DOI] [PubMed] [Google Scholar]


