Abstract
Background:
Variations in the pedicle morphology and presence of spinal deformities can make pedicle screw placement challenging. Recently, computerized tomography (CT) guided screw placement has reportedly improved the surgical accuracy of pedicle screw insertion. However, it is time consuming and expensive. We combined single-plane fluoroscopy in AP projection alone with tactile guidance for placing pedicle screws more efficiently and accurately. This report presents our results with this technique.
Materials and Methods:
An Institutional Review Board (IRB) approved retrospective study was carried out on 308 patients who underwent lumbar spinal fusion with 1806 pedicle screws placed using fluoroscopy only in the AP plane. There were 182 patients with two-level fusion, 79 with single-level fusion, 26 with three-level fusion, and 21 with more than three-level fusions. The indications of surgery included spondylolisthesis, adult scoliosis, revision surgery, lumbar canal stenosis, and discogenic pain. Pedicle screws were inserted under fluoroscopic guidance in the AP plane alone with a final lateral image after completion of implant placement. Radiographs were performed postoperatively in all patients and CT scans were obtained on 78 patients with 588 screws.
Results:
Twenty nine (5%) cortical wall perforations were noted amongst the 588 screws that were evaluated with a CT scan and did not result in postoperative vascular or neural complications. Anterior cortical vertebral violation was noted in 14 patients, while in 9 patients the screws penetrated the lateral wall of the pedicle. The medial wall of the pedicle was encroached in six patients with no frank perforations.
Conclusion:
Placement of pedicle screws under fluoroscopic guidance using AP plane imaging alone with tactile guidance is safe, fast, and reliable. However, a good understanding of the radiographic landmarks is a prerequisite.
Keywords: Lumbar spine, pedicle screw, fluoroscopy, AP imaging
INTRODUCTION
Spinal instrumentation using pedicle screws is commonly used for stabilization of the spine. The close proximity of the pedicles to the spinal canal and surrounding vessels may lead to serious complications with misplaced pedicle screws.1,2 Thus, accurate and safe placement of the screw within the confines of the pedicle is of paramount importance for a successful surgery. Individual anatomical variations in the pedicle axis, width and body habitus may result in misplacement of pedicle screws.1,2 Additionally, screw placement in revision surgery where the anatomical landmarks are distorted or covered by a bony fusion mass is both challenging and time consuming. Scoliotic spinal curves also increase the potential risk for significant neurological, vascular, and visceral injury.3 A search for methods to improve the surgical accuracy of pedicle screw insertion resulted in the advent of fluoroscopic and more recently computerized tomography (CT)-guided screw placement.4 The CT-guided techniques require preoperative CT scans integrated with expensive and potentially time-consuming Computer Technology Reference. Apart from limited availability, it lengthens the duration of surgery, which has been correlated to an increased incidence of surgical site infection in procedures involving spinal instrumentation.5,6
Combining the principles of fluoroscopy and tactile guidance, we were able to place pedicle screws in the lumbar spine safely and accurately using fluoroscopy in the anteroposterior (AP) plane alone. This study presents the technique and evaluates the positioning of the screws with intraoperative fluoroscopic images and postoperative radiographs in all patients and CT scan in a select group of patients.
MATERIALS AND METHODS
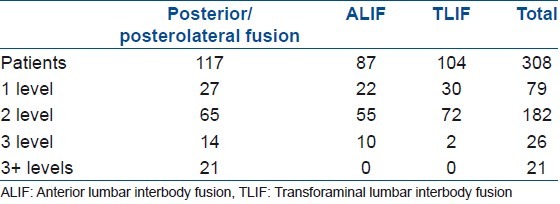
An Institutional Review Board approved retrospective study was carried out on 308 patients who underwent lumbar spinal fusion. Their mean age was 52 years (range 31-79 years) at the time of surgery. This included 186 men and 122 women. Treatment consisted of single or multilevel fusions of the lumbar spine, resulting in 626 fusion levels. A total of 1806 pedicle screws were placed using fluoroscopy only in the AP plane who underwent decompression, posterolateral fusion and instrumentation (n=117); transforaminal lumbar interbody fusion (TLIF) (n=104); and front back 360° fusions (n=87). There were 182 patients with two-level fusion, 79 with single-level fusion, 26 with three-level fusion, and 21 with more than three-level fusions [Table 1]. The indications of surgery included spondylolisthesis, adult scoliosis, revision surgery, lumbar canal stenosis, and discogenic back pain. The Universal Spinal System (USS) Click-X (Synthes Spine, Paoli, USA), or Texas Scottish Rite Hospital (TSRH) (Medtronic, Minneapolis, USA) pedicle screw systems were used for posterior spinal stabilization. Patients who had a front back procedure were stabilized anteriorly with a plate or screw and washer to prevent displacement of the interbody graft. Pedicle screws were inserted under fluoroscopic guidance in the AP plane alone with a final lateral image after completion of implant placement. Radiographs were performed postoperatively in all patients and CT scans were obtained on 78 patients with 588 screws. CT scans were performed only if there was concern for union or patients reported recurrence of back or leg pain. Imaging studies were examined independently by a surgeon and a radiologist to evaluate the position of screws. Screw placement was best evaluated on intraoperative fluoroscopic images as the vertebrae were square during pedicle screw insertion in the posteroanterior (PA) view. During placement of the screw, it was ensured that the screw tip remained within the elliptical density of the pedicle. If a small part of the screw breached the medial wall of the ellipse, it was acceptable since by this time the screw had passed the pedicle and was in the vertebral body. If any part of the screw lay lateral to the lateral wall of the ellipse, it was considered a violation of the lateral wall. The lateral images determined anterior vertebral wall integrity and also the caudal-cephalic orientation of the screw. Acceptable position of the screw was recorded if the pedicle screw lay within the superior and inferior borders of the pedicle and did not violate the anterior cortex. CT scan images were classified according to the Learch7 and Wiesner.8 In this classification, there are four main categories for screw misplacement:
Table 1.
Fusion levels and types (n=308)
Encroachment if the pedicle cortex could not be visualized.
Minor penetration when the screw trajectory was <3 mm outside the pedicular boundaries.
Moderate penetration when the screw trajectory was 3–6mm outside the pedicular boundaries.
Severe penetration when the screw trajectory was >6mm outside the pedicular boundaries.
Operative procedure
Patients were placed prone on a Jackson spinal table with a prone view device to position the head. A Kambin frame allowed the abdomen to hang freely in its valley. Following a standard surgical exposure with posterior midline incision and exposure to the tips of the transverse processes bilaterally, a C-arm was used to obtain a true AP image of the pedicles. The images were determined to be true AP if the superior end plate of the vertebral body appeared sharp and the spinous process was in the midline [Figure 1]. This occurred once the superior endplate was parallel to the image intensifier's beam. Now the pedicles presented as two identical elliptical densities on either side of the spinous processes. The entry point of each pedicle screw on the fluoroscopic image started at the most lateral aspect of the elliptical density at its center in the cranial–caudal plane [Figure 2]. A 3.2 mm drill was used to drill a starting point directed medially with an obliquity equal to that of the C-arm required to obtain a true AP view. At this time, the ellipse was seen to be bisected by the drill, signifying that drill trajectory was correct. Each pedicle was then pre-drilled, and a ball-tipped straight probe was used to assess for cortical violation. C-arm images were obtained at the starting point and at completion of drilling while the surgeon stepped away from the field in the latter instance. The key point of the procedure was to be able to repeatedly get the proper AP image of each vertebra which our radiology technicians picked up fairly quickly. One also needs to advance the probe anteromedially with a force enough to penetrate the vertebral cancellous bone but not the anterior cortex. No further pressure was applied on the probe once hard anterior cortical bone was felt. Following measurement of depth, a suitable pedicle screw was then placed. Sacral screws were placed with a bicortical purchase. While probing the sacrum, a point of anterior give way was felt when the probe transited from a bony canal into the soft anterior sacral structures and determined the screw length. By staying in the ellipse, there is no danger of straying superiorly or inferiorly.
Figure 1.
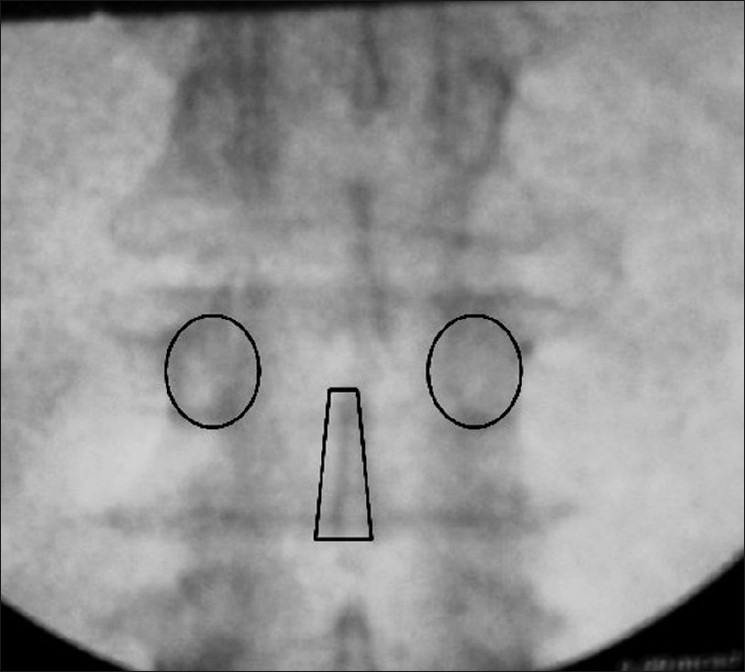
True AP fluoroscopic image showing sharp superior end plate of the vertebral body and midline spinous process
Figure 2.
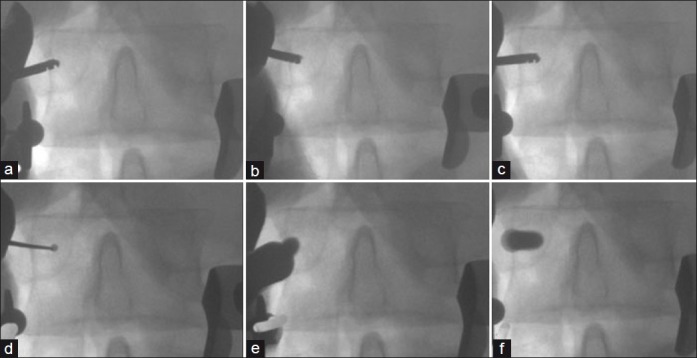
Fluoroscopic true AP Images showing (a) Starting point of drill on the lateral edge of the pedicle ellipse. (b, c) Progress of drill medially. (d) Blunt-tipped probe for penetration of cancellous bone in vertebral body. (e) Starting point of pedicle screw. (f) Final screw placement
In patients with scoliosis, the preoperative magnetic resonance imaging (MRI) or CT scan was reviewed to determine vertebral morphology. In many adult scoliosis patients, the vertebrae are not dysmorphic and are simply rotated and angulated. In these patients, the AP view can be obtained by rotating the C-arm in the axial and coronal planes. We have found this technique to be especially useful in these patients [Figure 3].
Figure 3.
Entry point of pedicle screw on the fluoroscopic image
RESULTS
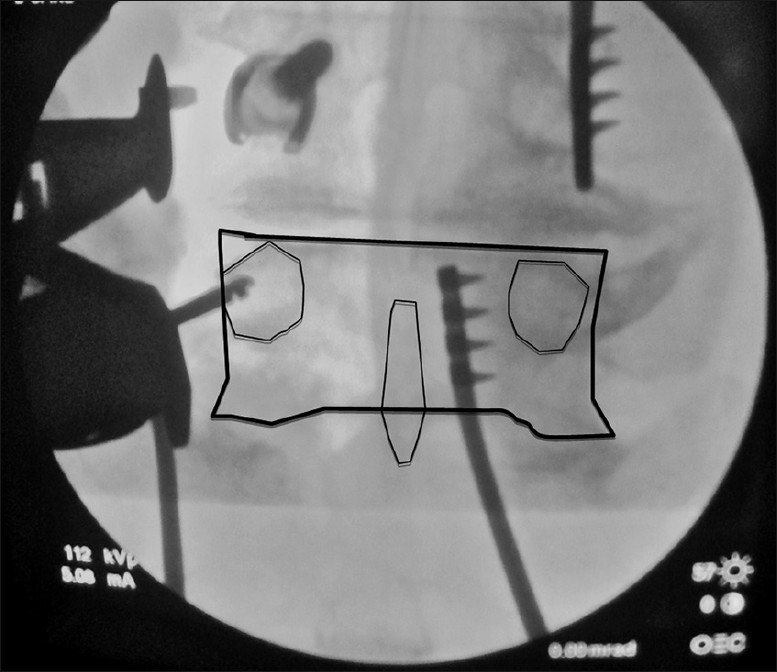
A total of 1806 screws were placed from L1 to S1 and evaluated for accuracy of placement. Although AP and lateral radiographs were performed on all patients postoperatively [Figure 4], accuracy of screw placement was determined based on CT scan images only performed on 78 patients. There were 29 (5%) cortical wall perforations noted in 588 screws, which did not result in any postoperative vascular or neural complications. Anterior cortical vertebral violation was noted in 14 patients and graded as minor (n=9) and moderate (n=5), while in another 9, the screws penetrated the lateral wall of the pedicle. The lateral wall violations were graded as six minor and three moderate. The medial wall of the pedicle was encroached in six patients with no frank perforations. Further, there were no severe penetrations and none of the screws had to be revised due to screw malposition. Additionally, none of the screws violated the disc space and were misplaced in the cephalo-caudal direction. At their latest followup, no patients displayed delayed neurological complications.
Figure 4.
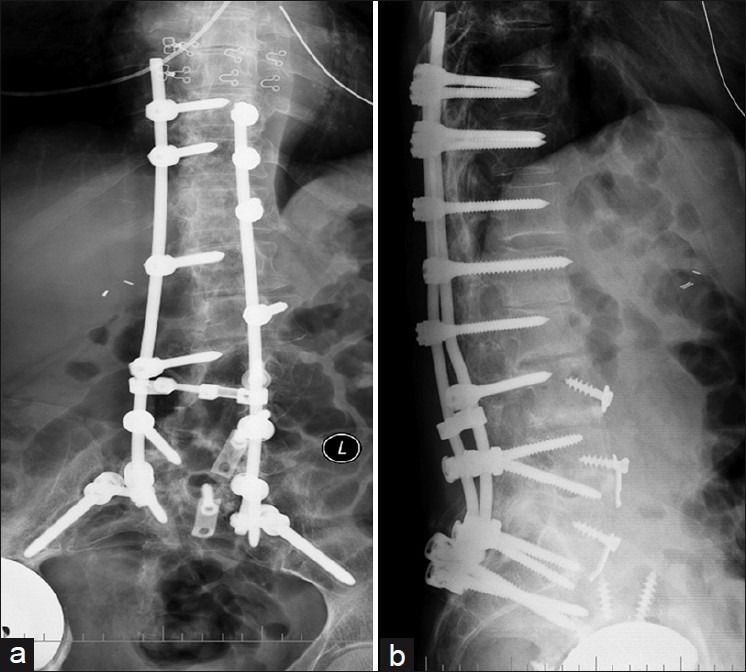
X-ray (Anteroposterior (a) and lateral (b) view) lumbosacral spine in an adult degenerative scoliosis showing multilevel instrumentation
DISCUSSION
The aim of this study was to evaluate the efficacy of pedicle screw placement with the use of fluoroscopy in the AP plane only. Currently, the rate of misplaced screws has been variably reported in literature as ranging from 10 to 15%, with some reports showing as high as 40%.2,9 In the present series of 1806 pedicle screws, frank penetration was noted in 23 screws, of which 8 screws penetrated by more than 2mm. Six screws encroached the medial wall of the pedicle and none displayed frank penetration. Further, none of the patients with misplaced screws showed features of neural, vascular, or visceral injuries. Researchers have observed that a 4 mm “safe zone” exists adjacent to the pedicle in the lumbar spine since no clinical neurologic complications were observed for the screws violating the pedicle by 0–4 mm.10 Most surgeons consider 2 mm to be the safe penetration that may not result in neural complications.2
The most important step to prevent complications is confirmation of an accurate pedicle screw starting point within the confines of the pedicle. Placement of screws in the presence of a previous fusion mass is both challenging and time consuming since the normal anatomy is obliterated and bony landmarks that guide screw placement are not visualized. However, radiographically, the pedicles may be visualized and a suitable starting point identified. Further, as described in the technique, the end point of screw insertion may be recognized with both radiographic and tactile guidance. The benefits of this technique were also clear in patients undergoing long spinal fusions. As screws are placed more efficiently, surgical time and surgeon exhaustion may potentially be minimized allowing the procedure to be performed more effectively. This may not be significant when single-level procedures are performed, but has a summation effect in multilevel surgery.
In an earlier study, we had determined that obesity adversely affects the rate of intraoperative complications associated with lumbar fusion surgery.11 Surgical procedures are required to be performed in a deeper plane with limited visualization and illumination. Unlike other reports, in the present study, we noted that the rate of misplaced screws in the obese was not affected by the body mass index (BMI) of the patient.12 We attribute this to the use of the SynFrame Access and Retractor System (Synthes Inc., West Chester, PA, USA).
Another relevant factor for screw misplacement is pedicle convergent angle. Morphometric anatomic studies have determined that pedicles flare out laterally from the upper to lower lumbar spine.13 Transverse pedicle angles of the lower lumbar spine range from 8.0°–23.5° at L3 (mean 14.4°) to 19.0°–44.0° at L5 (mean 29.8°).14 Several authors have reported more discrepancy between the pedicle convergent angle and the screw trajectory angle in the lower lumbar spine.12 The lumbar pedicles are wider than their thoracic counterparts, allowing some play in the trajectory of screw insertion. The pedicle screws may be placed either along the midpedicular axis, requiring longer incisions, or in a straighter trajectory with their tips ending in the lateral vertebral body. The insertion of the pedicle screws in a straight fashion does not require extensive dissection, retraction, or excision of paraspinal musculature, while placement along the transverse pedicle angles can range up to 38° from the midline. We had earlier reported that straight screw insertion results in a pedicle screw construct that has a better fatigue performance.13 Based on this study, we place our screws straighter in obese patients, resulting in smaller incisions with no increase in failure rate.
This study differs from the others as the technique relies only on the PA image for screw insertion and utilizes the lateral image as a confirmatory image, which could potentially decrease the amount of fluoroscopic time used during surgery. We noted that an assessment of screw placement could be carried out more accurately using fluoroscopic images since the vertebral bodies during screw insertion were square with the beam of the C-arm being parallel to the vertebral body. In contrast, postoperative AP radiographs included the entire lumbar spine and were unable to neutralize the vertebral angle, especially in the lower lumbar spine and sacrum, giving an erroneous assessment of screw position due to the presence of a parallax. Lateral radiographs were able to determine anterior cortical violation if the screws penetrated close to the center of the vertebral body. Pedicle screws that violated the anterior cortex more laterally also appeared accurately positioned due to the circular shape of the anterior vertebra and superimposition of the central anterior cortex. For this reason, we have used only CT images to evaluate the accuracy of pedicle screw placement.
As reported earlier, the gold standard for assessment of pedicle screw position is postoperative CT scans. Previous reports looking at the use of CT scans in detecting pedicle wall breaches show an accuracy rate of 87 ± 3% for titanium screws.15 The results and conclusions of this study are based on CT images available on 78/308 patients (25%), and it may be of concern that all patients did not undergo this imaging study. However, CT scans were performed only in patients with a suspicion of nonunion or with complaints of recurrence of back or leg pain. These patients thus represent the group with inferior results in the cohort. It is our premise that if CT scans were performed on all patients, the screw perforation rate may be the same or even less since all remaining patients had an uneventful recovery and noted improved outcomes following surgery. Additionally, this technique has a learning curve since it depends on tactile sensation. Though experienced hands may find it fairly easy, to the uninitiated surgeon this may be a challenge.
CONCLUSIONS
The preliminary results of this study suggest that placement of pedicle screws with fluoroscopic guidance using AP plane imaging alone is safe, fast, and reliable for an operator with good understanding of the radiographic landmarks. The greatest benefits of this technique are in long spinal fusions, revison surgery, and in obese patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Park Y, Ha JW, Lee YT, Sung NY. Percutaneous placement of pedicle screws in overweight and obese patients. Spine J. 2011;11:919–24. doi: 10.1016/j.spinee.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 2.Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, et al. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2011;21:247–55. doi: 10.1007/s00586-011-2011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang KW, Wang YF, Zhang GZ, Cheng CW, Chen HY, Leng X, et al. Tai Chi. Pedicle screw placement for severe scoliosis. JSpinal Disord Tech. 2011;25:E67–73. doi: 10.1097/BSD.0b013e31823db498. [DOI] [PubMed] [Google Scholar]
- 4.Wood M, Mannion R. A comparison of CT-based navigation techniques for minimally invasive lumbar pedicle screw placement. J Spinal Disord Tech. 2011;24:E1–5. doi: 10.1097/BSD.0b013e3181d534b8. [DOI] [PubMed] [Google Scholar]
- 5.Silbermann J, Riese F, Allam Y, Reichert T, Koeppert H, Gutberlet M. Computer tomography assessment of pedicle screw placement in lumbar and sacral spine: Comparison between free-hand and O-arm based navigation techniques. Eur Spine J. 2011;20:875–81. doi: 10.1007/s00586-010-1683-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desai S, Sethi A, Ninh CC, Bartol S, Vaidya R. Pedicle screw fixation of the C7 vertebra using an anteroposterior fluoroscopic imaging technique. Eur Spine J. 2010;19:1953–9. doi: 10.1007/s00586-010-1513-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Learch TJ, Massie JB, Pathria MN, Ahlgren BA, Garfin SR. Assessment of pedicle screw placement utilizing conventional radiography and computed tomography: a proposed systematic approach to improve accuracy of interpretation. Spine (Phila Pa 1976) 2004;29:767–73. doi: 10.1097/01.brs.0000112071.69448.a1. [DOI] [PubMed] [Google Scholar]
- 8.Wiesner L, Kothe R, Rüther W. Anatomic evaluation of two different techniques for the percutaneous insertion of pedicle screws in the lumbar spine. Spine (Phila Pa 1976) 1999;24:1599–603. doi: 10.1097/00007632-199908010-00015. [DOI] [PubMed] [Google Scholar]
- 9.Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine (Phila Pa 1976) 1996;21:1320–4. doi: 10.1097/00007632-199606010-00008. [DOI] [PubMed] [Google Scholar]
- 10.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15:11–4. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A. Lumbar spine fusion in obese and morbidly obese patients. Spine (Phila Pa 1976) 2009;34:495–500. doi: 10.1097/BRS.0b013e318198c5f2. [DOI] [PubMed] [Google Scholar]
- 12.Kim MC, Chung HT, Cho JL, Kim DJ, Chung NS. Factors affecting the accurate placement of percutaneous pedicle screws during minimally invasive transforaminal lumbar interbody fusion. EurSpine J. 2011;20:1635–43. doi: 10.1007/s00586-011-1892-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sterba W, Kim DG, Fyhrie DP, Yeni YN, Vaidya R. Biomechanical analysis of differing pedicle screw insertion angles. Clin Biomech (Bristol, Avon) 2007;22:385–91. doi: 10.1016/j.clinbiomech.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976) 1987;12:160–6. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Yoo JU, Ghanayem A, Petersilge C, Lewin J. Accuracy of using computed tomography to identify pedicle screw placement in cadaveric human lumbar spine. Spine (Phila Pa 1976) 1997;22:2668–71. doi: 10.1097/00007632-199711150-00016. [DOI] [PubMed] [Google Scholar]


