Abstract
Background:
The extent of tumor may necessitate resection of the complete femur rarely to achieve adequate oncologic clearance in bone sarcomas. We present our experience with reconstruction in such cases using an indigenously manufactured, low-cost, total femoral prosthesis (TFP). We assessed the complications of the procedure, the oncologic and functional outcomes, and implant survival.
Materials and Methods:
Eight patients (four males and four females) with a mean age of 32 years, operated between December 2003 and June 2009, had a TFP implanted. The diagnosis included osteogenic sarcoma (5), Ewing's sarcoma (1), and chondrosarcoma (2). Mean followup was 33 months (9–72 months) for all and 40 months (24–72 months) in survivors. They were evaluated by Musculoskeletal Tumor Society score, implant survival as well as patient survival.
Results:
There was one local recurrence and five of seven patients are currently alive at the time of last followup. The Musculoskeletal Tumor Society score for patients ranged from 21 to 25 with a mean of 24 (80%). The implant survival was 88% at 5 years with only one TFP needing removal because of infection.
Conclusions:
A TFP in appropriately indicated patients with malignant bone tumors is oncologically safe. A locally manufactured, cost-effective implant provided consistent and predictable results after excision of the total femur with good functional outcomes.
Keywords: Limb salvage, megaprosthesis, total femoral prosthesis
INTRODUCTION
The advent of effective chemotherapy has made limb salvage an oncologically safe option for a large majority of bone tumors without compromising long term survival. The femur is the commonest site for primary bone tumors, and rarely, the extent of tumor may necessitate resection of the complete femur to achieve adequate oncologic clearance. These extensive resections are a challenge to reconstruct. Options include total femoral prostheses (TFP), allografts, and rotationplasty.1–6
Few reports in literature address the use of TFP exclusively for bone sarcomas. Most of these describe the functional results with expensive internationally available prostheses.2–5 In a resource challenged population, the cost of prostheses can occasionally be a limiting factor to limb salvage, especially in cases of malignant tumors where the prognosis is guarded.7 We present our experience with indigenously manufactured low cost total femoral prosthesis (TFP) for oncologic outcomes and implant survival after resection and replacement of the total femur.
MATERIALS AND METHODS
Nine patients were operated between December 2003 and June 2009 for resection and TFP implantation. These patients were retrospectively reviewed from a prospectively maintained database. Endoprosthetic reconstruction after resection was achieved with a modular total femur prosthesis using an indigenously manufactured fixed hinge TFP (TMH-NICE / ResTOR, Sushrut-Adler Mediequip Pvt. Ltd., Devrukh, India – www.sushrut.com/restor.htm) in eight cases and an expandable Howmedica Modular Resection System (HMRS) prosthesis in one case.
The eight cases in which the indigenously manufactured TFP was implanted were analyzed in this case series. The medical records, imaging, functional and current disease status were reviewed. There were four males and four females with a mean age of 32 years (range 13–72 years). All except one were done as a limb salvage procedure for a primary or recurrent malignant bone tumor. Case 7 was for revision of a broken proximal femur replacement, originally done for a malignant bone tumor [Table 1]. The diagnosis included osteogenic sarcoma (n=5), Ewing's sarcoma (n=1), and chondrosarcoma (n=2). All the patients were nonmetastatic at time of implantation of the TFP. The patients received chemotherapy as per the existing hospital protocols. None of the patients had radiotherapy.
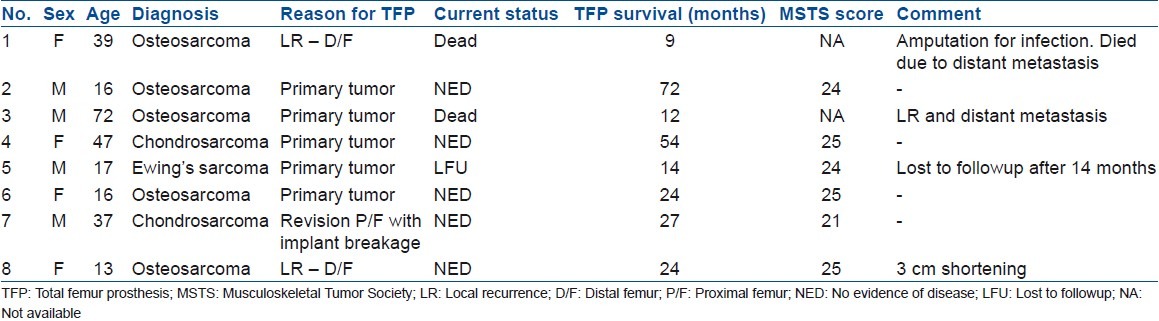
Table 1.
Patient details
The primary goal of surgery was limb preservation with complete excision of the tumor while retaining adequate muscle for satisfactory residual function. Surgery involved disarticulation of the hip and knee with enbloc excision of the entire femur and surrounding muscles involved with the tumor while preserving the neurovascular bundle. The indigenously manufactured modular total femur system comprises a trochanteric component, a central resection segment, and a distal femoral component, designed to lock into each other with a customized self-locking taper. The central resection segments are available in various sizes to match the length of the patient's femur. The trochanteric component couples with a bipolar cup assembly at the proximal end. Restoration of length was based on preoperative radiological assessment and reconfirmed intraoperatively by measurement of the resected specimen [Figure 1].
Figure 1.
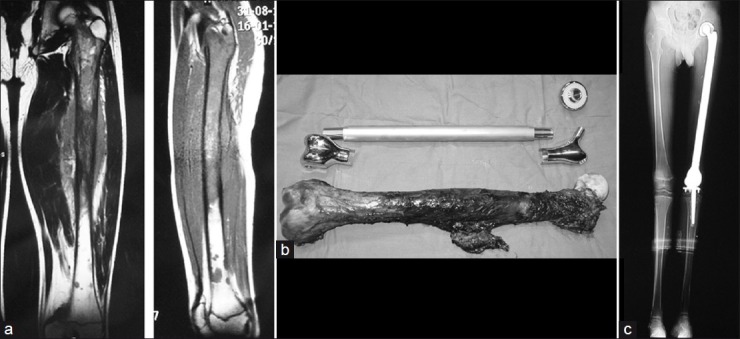
(a) Preoperative T1-weighted MRI showing involvement of the entire femur in a case of Ewing's sarcoma. (b) Intraoperative confirmation of prosthesis length compared to the resected specimen. (c) Radiograph demonstrating restoration of limb length after total femur prosthesis
To further reinforce hip stability and prevent dislocation, the residual hip capsule was sutured around the neck of the prosthesis. In cases where the capsule was deficient, it was reinforced with a polypropylene mesh (Prolene™ – Johnson and Johnson, Ethicon division, Aurangabad, India) that was anchored to the acetabulum and extended to form a sleeve around the proximal part of the prosthesis.8 Only glutei were either sutured directly to the prosthesis and/or sutured to the polypropylene mesh.
Postoperatively, patients used an abduction brace while recumbent for the first 6 weeks. Progressive mobilization using a walker or crutches was started within the first few postoperative days and patients gradually progressed to ambulation without the use of supports. Patients were instructed to restrict hip flexion to 60° for the first 6 weeks while encouraging active quadriceps exercises to regain knee extension.
Patients were asked to followup every 3 months for the first 2 years and six monthly subsequently. Seven patients were available for followup. Functional status was assessed at the time of last followup using the Musculoskeletal Tumor Society (MSTS) scoring system.9 This was based on the analysis of six factors (pain, use of supports for ambulation, walking ability, functional activities, gait, and emotional acceptance). For each of the six factors, values of 0–5 were assigned based on established criteria. The result was expressed as a sum total with a maximum score of 30 and as a percentage of the expected normal function for the patient.
A Kaplan–Meier survival curve was plotted for implant survival. Survival of the implant was analyzed with the starting point defined as the date of implantation of the endoprosthesis and the endpoint being removal (whatever the cause). Patients were censored for statistical analysis (observation stopped before the event occurred) if removal had not occurred at the time the patient was last assessed.
RESULTS
The mean followup was 33 months (9–72 months) for all patients (n=8) and 40 months (24–72 months) in survivors (n= 5). 8 patients analysed, 1 lost to follow up, 2 dead , 5 alive and were available for followup.
Complications
There was one case of infection which developed after 7 months in a patient who had the TFP implanted after excision of a recurrence around an earlier distal femoral prosthesis. Repeated wound lavage failed to control the infection and a hip disarticulation was finally performed (case 1).
Local recurrence and oncologic outcome
All resection margins were histologically free of disease. There was one local recurrence. It occurred in a 72-year-old male who had a large open biopsy elsewhere. His biopsy diagnosis was chondrosarcoma which was revised to chondroblastic osteosarcoma after evaluation of the excised femur. The patient refused adjuvant chemotherapy. He developed simultaneous local and distant recurrences and died at 12 months. Another patient (case 1) who had the TFP implanted after excision of a recurrence around an earlier distal femoral prosthesis eventually succumbed to distant metastasis. Thus, five of the seven patients available for follow up are currently alive.
Functional status
The MSTS score for patients evaluated at their last followup ranged from 21 to 25 with a mean of 24 (80%). All the patients were independent ambulators and none of them required a support for walking.
Implant survival
The Kaplan–Meier survival curve is shown in Figure 2. Only one TFP needed removal and that was because of infection. The survival of the implant was 88% at 5 years.
Figure 2.
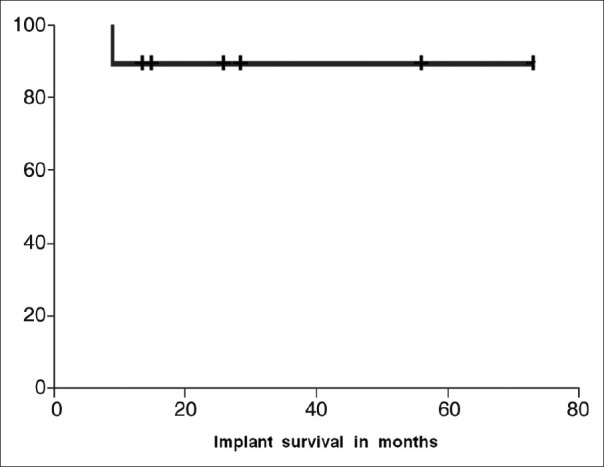
The Kaplan–Meier curve showing implant survival
DISCUSSION
Reconstructing large defects after resection of a tumor has always been challenging. In the past, most patients with extended sarcomas of the femur had an amputation with poor function.3 The advent of better imaging modalities, effective chemotherapy, better understanding of anatomy with continuous refinement in surgical techniques, and advances in prosthesis design and materials have all played a part in increasing the incidence of limb salvage surgery. Limb salvage should not compromise patient survival while ensuring that patients are able to resume near-normal function as soon as possible.5 The prostheses used must also demonstrate good long term survival. When evaluating a reconstruction technique, various factors need to be considered including its complications, functional outcome, and durability. In resource-challenged populations, cost too often plays a role in the decision making.10
In most cases of tumors involving the femur, adequate resection may be possible with retention of enough bone either proximally or distally to seat an intramedullary stem for a distal femoral or proximal femoral prosthesis. Occasionally, for oncologic reasons, entire femoral resection may be necessary or the residual bone stump after proximal/distal femoral resection may be too short to adequately seat a stable intramedullary stem. These are the cases where a TFP is indicated.
Hip dislocation is a common complication reported after total femur replacement.2,4–6,11 A combination of various factors can contribute to this. These include lack of functional abductor musculature, resection of the joint capsule, acetabular resurfacing, and use of a rotating hinge design at the knee since rotation at the knee can lead to hip dislocation.2,5 In our series, we did not have any dislocation. This can be attributed to the use of a fixed hinge prosthesis, using a bipolar head in all cases, and reinforcing the residual hip capsule with a polypropylene mesh in cases where the capsule was deficient.
The incidence of local recurrence is a reflection of adequate oncologic clearance and the effectiveness of chemotherapy.12 We had one local recurrence occurring in a case of osteosarcoma, who had an open biopsy at a non oncology center and received no chemotherapy. Having identified definite adverse contributing factors in this case, we believe that limb salvage with a TFP is an oncologically sound procedure in appropriately selected cases. Local control rates are similar to those described for limb salvage procedures at other sites.7
The survival of the implant was 88%, with removal as the endpoint. Only one implant was removed in a patient who had an amputation for infection.
The average functional score (80%) in our study as evaluated by the MSTS scoring system is encouraging when compared with other series describing the use of TFP [Table 2].2,4–6 One case (case 8) currently has 3 cm shortening and is managing with a shoe raise. Patients reported very good psychological acceptance after limb salvage with the TFP despite having a poor gait which is primarily due to the lack of good abductor muscle attachment. All the patients preferred the limb salvage option. This is significant as the prostheses used for limb salvage were low-cost, locally manufactured devices costing approximately US $ 2000 (international prosthesis costs approximately US $ 18,000). We currently do not use a locally manufactured expandable prosthesis. Thus, due to cost constraints, we are unable to offer conventional limb salvage to some young children requiring total femur excision and do a rotationplasty instead.13
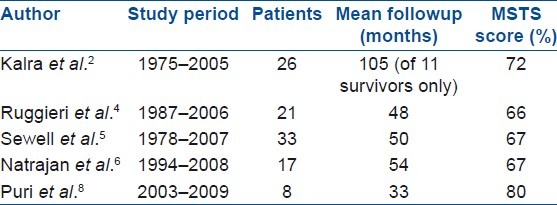
Table 2.
Comparative studies
Our study is limited by its small numbers, but the uncommon use of TFP for bone sarcomas would necessitate results from various centers being pooled to reach meaningful conclusions.4 Though late local recurrence is uncommon, the incidence of implant related complications can be expected to increase with a longer followup.12
In spite of these shortcomings, we believe that this study does add to the existing literature on use of massive implants in limb salvage, especially the use of TFP in appropriately indicated patients with malignant bone tumors. The procedure is oncologically safe and patient survival does not appear to be compromised. The successful use of locally manufactured megaprostheses demonstrates that cost constraints need no longer be an insurmountable barrier for the use of limb salvage implants in resource-challenged populations.
ACKNOWLEDGMENT
The authors would like to acknowledge Mr. Ravi Sarangapani of Sushrut-Adler Mediequip Pvt. Ltd. for his inputs on implant design.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Agarwal M, Puri A, Anchan C, Shah M, Jambhekar N. Rotationplasty for bone tumors: is there still a role? Clin Orthop Relat Res. 2007;459:76–81. doi: 10.1097/BLO.0b013e31805470f0. [DOI] [PubMed] [Google Scholar]
- 2.Kalra S, Abudu A, Murata H, Grimer RJ, Tillman RM, Carter SR. Total femur replacement: primary procedure for treatment of malignant tumours of the femur. Eur J Surg Oncol. 2010;36:378–83. doi: 10.1016/j.ejso.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Mankin HJ, Hornicek FJ, Harris M. Total femur replacement procedures in tumor treatment. Clin Orthop Relat Res. 2005;438:60–4. doi: 10.1097/00003086-200509000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Ruggieri P, Bosco G, Pala E, Errani C, Mercuri M. Local recurrence, survival and function after total femur resection and megaprosthetic reconstruction for bone sarcomas. Clin Orthop Relat Res. 2010;468:2860–6. doi: 10.1007/s11999-010-1476-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sewell MD, Spiegelberg BG, Hanna SA, Aston WJ, Bartlett W, Blunn GW, et al. Total femoral endoprosthetic replacement following excision of bone tumours. J Bone Joint Surg Br. 2009;91:1513–20. doi: 10.1302/0301-620X.91B11.21996. [DOI] [PubMed] [Google Scholar]
- 6.Natarajan MV, Balasubramanian N, Jayasankar V, Sameer M. Endoprosthetic reconstruction using total femoral custom mega prosthesis in malignant bone tumours. Int Orthop. 2009;33:1359–63. doi: 10.1007/s00264-009-0737-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agarwal M, Anchan C, Shah M, Puri A, Pai S. Limb salvage surgery for osteosarcoma: effective low-cost treatment. Clin Orthop Relat Res. 2007;459:82–91. doi: 10.1097/BLO.0b013e31805d85c4. [DOI] [PubMed] [Google Scholar]
- 8.Puri A, Agarwal M. Use of polypropylene mesh to stabilize skeletal reconstructions after resection for bone tumors. J Surg Oncol. 2007;95:158–60. doi: 10.1002/jso.20595. [DOI] [PubMed] [Google Scholar]
- 9.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993:241–6. [PubMed] [Google Scholar]
- 10.Kwan MK, Ng ES, Penafort R, Saw A, Sengupta S. Resection arthrodesis for primary bone tumour about the knee. Med J Malaysia. 2005;60(Suppl C):66–71. [PubMed] [Google Scholar]
- 11.Ward WG, Dorey F, Eckardt JJ. Total femoral endoprosthetic reconstruction. Clin Orthop Relat Res. 1995:195–206. [PubMed] [Google Scholar]
- 12.Grimer RJ, Taminiau AM, Cannon SR. Surgical outcomes in osteosarcoma. J Bone Joint Surg Br. 2002;84:395–400. doi: 10.1302/0301-620x.84b3.12019. [DOI] [PubMed] [Google Scholar]
- 13.Agarwal M, Puri A, Anchan C, Shah M, Jambhekar N. Rotationplasty for bone tumors: Is there still a role? Clin Orthop Relat Res. 2007;459:76–81. doi: 10.1097/BLO.0b013e31805470f0. [DOI] [PubMed] [Google Scholar]


