Abstract
The increasing number of total hip replacements in the younger clique has added to the demand for revision procedures. Revision situations are often encountered with infection, loss of bone stock and bone defects. There are various methods of reconstruction of acetabular defects. The management options of type 3B Paprosky acetabular defects are limited with allograft and conventional cages. Trabecular metal technology has evolved to address these bone defects. Trabecular metal acetabular revision system (TMARS) cup-cage construct is a new technique to address massive acetabular defects. We describe a case of failed hip reconstruction done for a Giant cell tumour of proximal femur managed by a two stage procedure, initial debridement and second stage reconstruction of acetabulum with TMARS cup-cage construct and femur with allograft prosthesis composite.
Keywords: Allograft, cup-cage, revision, total hip arthroplasty, trabecular metal acetabular revision system
INTRODUCTION
The number of primary hip arthroplasties performed in the younger age patients escalates the demand for revision procedures. Revision procedures almost always pose the surgeon strife due to their complexity and level of competence needed. The crucial determinants in selection of a surgical procedure are the remnant bone stock and the nature of defect. We present the new technique of Trabecular Metal Acetabular Revision System (TMARS) cup-cage construct to accomplish the massive acetabular bone defect in our case.
CASE REPORT
A 29 year old male, college lecturer by profession, presented with pain in the left hip and inability to bear weight on left lower limb for 2 years, along with an active discharging sinus over the thigh. He was operated for giant cell tumor of the proximal femur 8 years back by excision and reconstruction by a custom made total hip replacement (THR) prosthesis. He developed infection following reconstruction and underwent multiple surgeries for the control of infection. Routine blood investigations revealed elevated total leukocyte count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels. Radiographs revealed protrusion of the acetabular and femoral components into the pelvis through a breach in the acetabulum and loosening of prostheses, zones of lysis with extensive periosteal reaction in the remnant femur [Figure 1].
Figure 1.
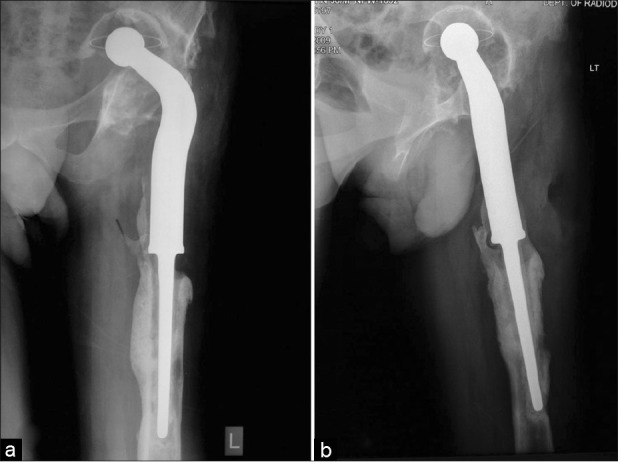
Preoperative radiographs of left hip and thigh anteroposterior (a) and lateral views (b), showing a Paprosky type 3b acetabular defect along with intrapelvic migration of acetabular and femoral component and areas of loosening
All the investigations put together were suggestive of possible pelvic discontinuity and septic loosening of the prosthesis. He was planned for revision reconstruction surgery by a two stage procedure.
The first stage consisted of removal of the prosthesis, debridement, and placement of an antibiotic cement spacer. Antibiotic cement was prepared by amalgamation of Vancomycin powder (4 g in 40 g packet of cement) in Gentamicin precontained cement (Palacos R+G). A cement spacer in the shape of a sphere was made for the acetabulum and the femoral aspect was taken care by an antibiotic cement coated Kuntscher nail inserted into the canal [Figure 2a and b]. Routine bacterial cultures did not grow any organism. He was put on intravenous Amikacin (750 mg once a day for first 5 days) and Magnamycin (2 g twice a day) for 6 weeks and then switched over to oral cefuroxime (500 mg twice a day) for another 6 weeks. The followup ESR and CRP showed a downward trend at 6 weeks and returned to normal by 3 months. Then, the patient was planned for final reconstruction with proximal femoral allograft prosthesis composite for the femoral defect and trabecular metal shell (TM, Zimmer, Warsaw, IN, USA) with cage for the acetabulum. Cup-cage construct was chosen to address the pelvic discontinuity.
Figure 2.
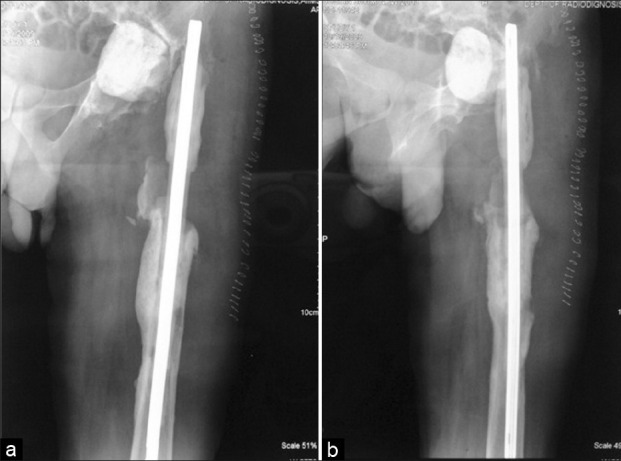
Postoperative radiographs anteroposterior (a) and lateral views (b) following the initial debridement depicting the cement spacer in acetabulum and antibiotic cement coated K nail in the femoral canal
Operative procedure
The hip joint was exposed by a standard posterior approach. The cement spacer in the acetabulum was removed, thoroughly debrided, and acetabulum was assessed for size and type of defect. The native bone was present only in posterosuperior and inferomedial portions, constituting around 30% of the true acetabulum with conspicuous pelvic discontinuity. A Homan retractor was placed in the obturator foramen which represents the level of inferior extent of the true acetabulum. The future hip center was identified by horizontal and vertical distances from this point as determined preoperatively from radiographs by comparison with the normal side. The acetabulum was prepared by graduated reaming until the appearance of bleeding bone and sized for the TM shell. The acetabular floor was filled with morselized allograft and prepared by reverse reaming. The TM shell of the size of last reamer was impacted into the prepared acetabulum and then held in place by screws drilled into the posterosuperior portion of the cup. The cup was then assessed for stability with a Kocher's clamp and it was not found to be satisfactory. Thus, the need of a cup-cage construct, which was suspected preoperatively by virtue of pelvic discontinuity, was corroborated by intraoperative assessment. A cup-cage construct using TMARS cage (Zimmer) was fashioned to secure the TM shell in place till osteointegration. The ischium was exposed and a slot was prepared by an osteotome for placement of inferior flange of the cage. The ilium in the posterosuperior portion of the acetabulum was also adequately exposed to receive the superior flange of the cage. The appropriate sized TMARS cage was selected and flanges were contoured to seat on the patient's ilium and ischium. The cage was embedded onto the TM shell and held in place by inferior flange in the slot in ischium and screws were drilled into the ilium in the superior flange. Best press fit, maximum contact with the host bone, and adequate stability of the cage dictated the ultimate orientation of the construct, i.e. in a more vertical position and relative retroversion. An appropriate sized liner was selected and cemented in position over the cup-cage construct with pressure in desired 45° abduction and 20° anteversion for maximum joint stability.
Femoral reconstruction was done by allograft prosthesis composite after the removal of K nail [Figure 3]. The wound was closed over a drain. The drain was removed on the second postoperative day. Intravenous antibiotic cefotaxime (1 g every 12 h) was administered for the first 5 days and then switched over to oral cefuroxime for another 10 days. Patient was mobilized non weight bearing with walker for the first 6 weeks and then partial weight bearing with crutches till the signs of radiographic union appeared, i.e. at 3 months. Hip abductor strengthening exercises were started from 8 weeks and he was allowed full weight bearing from 3 months.
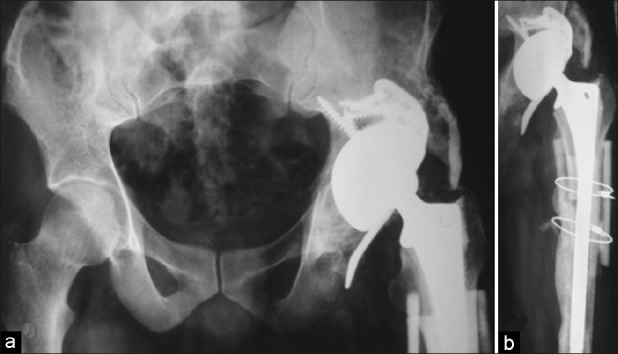
Figure 3.

Immediate postoperative radiograph of pelvis with bilateral hips anteroposterior view following the second stage reconstruction illustrating a well-constructed acetabular and femoral defect with cup-cage construct and allograft prosthesis composite, anatomic restoration of the hip center, and equalization of limb length. The inferior flange of the cage had cut through the ischium
Followup radiographs at 30 months showed solid union of the allograft with the native bone on the femoral side and good consolidation on the acetabular aspect with no zones of radiolucency [Figure 4a and b]. The patient is walking unaided and has a Harris hip score of 90.
Figure 4.
Followup radiographs of pelvis with bilateral hips anteroposterior view (a) and left thigh (b) at 30 months showing good osteointegration on the acetabular aspect and solid graft host bone union on the femoral side with no displacement of constructs
DISCUSSION
The management of an infected THR with a bone defect is almost always an arduous mission to the treating surgeon. The problems confronted in these cases would be infection on precedence, followed by the bone defect.
We resorted to two stage procedure is the gold standard of care with promising results to affray infection.1–3 Comparable results have been proclaimed even with single stage revision.4,5 We resorted to two stage procedure due to non availability of special incubation techniques for impregnation of antibiotics into the allograft and lack of clinical experience with the same. The option of allograft prosthesis for the proximal femoral defect was straightforward and driven by the evidence in literature.6,7
Anatomic restoration of the hip center and stability are the prime factors which govern the outcome in any hip replacement surgery. The situation gets complicated in the presence of massive acetabular bone defects. Proper placement of an acetabular component close to native hip center in these settings could be possible only with use of cages and allograft, i.e. by procurement of an enduring bony substratum which can guard the new acetabular component. However, there have been many controversies regarding the ideal treatment for the acetabular bone defects encountered in revision situations. Situations in which there is >50% available bone stock can be managed by uncemented cups and morselized allografts with good outcomes.8–10 Conflict arises in the setting of acetabular bone defect more than 50%. Traditionally in the past, rings and cages had been used in combination with allograft to address these bone defects. Literature unveils mediocre results with the use of cages and failure rates reaching up to 25% at 5–7 years.11,12 Rings and cages provide only initial stability and do not have a surface that permits osteointegration. So, the allograft should unite with the host bone and osteointegration should take place by the time the cage loses its initial strength. This contention gets complicated in the midst of infection, graft collapse, and resorption, which are more common with allograft.13,14 The use of allograft provides an advantage of restoration of the bone stock even in the case where future revision is necessary.
The advent of TM shell technology has changed the face of revision arthroplasty. The porous tantalum is used in this technology and it is the only material which simulates the native bone. The properties of high porosity (80%), coefficient of friction, and intrinsic strength provide greater stability and an environment conducive for bone in growth.15 TM cups have bestowed excellent short to mid term results. Unger et al. have reported a failure rate of 2% at a mean followup of 42 months with the use of TM cups in contained and segmental defects.16 Lakstein et al. advocated the use of TM cups in contained defects with <50% host bone contact, with their results of success rate being 96% at a mean followup of 4 years.17 The indications of TM cups have broadened to address even the massive uncontained defects with augments and cup-cage constructs.
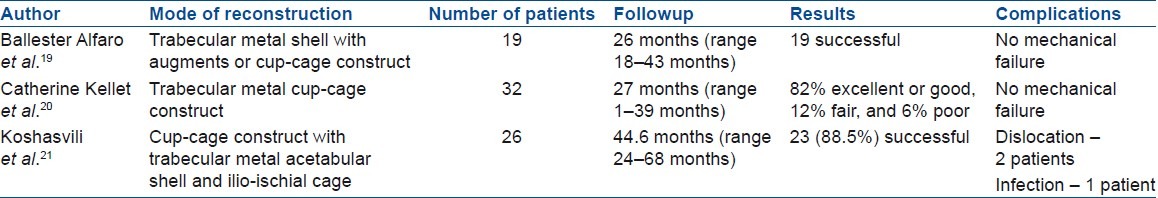
Cup-cage construct was first described by Hanssen and Lawellan.18 This employs an ilio-ischial cage which allows for permanent anchorage by bone in growth and provides a good support for the TM cup till osteointegration. The stresses are relieved from cage after the osteointegration of the cup, and thus may defeat the cage failures. Table 1 illustrates the results of various reports on this technique.
Table 1.
Summary of reports which employed the trabecular metal cup-cage construct
There are many constraints in a developing country like India, which may limit the appositeness of the above principles in all cases of failed hip replacements. They include high costs of surgery and nonavailability of the suitable implant and allograft. The TMARS cage was imported from Australia in our case. However, a routinely available, less expensive Burch Schneider cage might serve the purpose of provision of initial stability for the TM cup and substitute the role of a TMARS cage. Burch Schneider cage is also made of pure titanium (Protasul-Ti) like TMARS cage and is rough-blasted on the side facing bone. TMARS cage caters the advantage by its modularity, flexibility, and design. However, there is not yet any published study elucidating the use of Burch Schneider cage in cup-cage construct.
The cup-cage construct carries the theoretical advantages in comparison to the allograft for the reconstruction of massive acetabular bone defects. This new technique has come up with encouraging short term results [Table 1] and invokes comparative trials with long term followup. Thus, the cup-cage construct may mitigate the need of allografts for reconstruction of acetabulum in future.21
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Lai KA, Shen WJ, Yang CY, Lin RM, Lin CJ, Jou IM. Two-stage cementless revision THR after infection. 5 recurrences in 40 cases followed 2.5-7 years. Acta Orthop Scand. 1996;67:325–8. doi: 10.3109/17453679609002324. [DOI] [PubMed] [Google Scholar]
- 2.Younger A, Duncan C, Masri B. Treatment of infection associated with segmental bone loss in the proximal part of the femur in two stages with use of an antibiotic-loaded interval prosthesis. J Bone Joint Surg Am. 1998;80:60–9. doi: 10.2106/00004623-199801000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Stockley I, Mockford BJ, Hoad-Reddick A, Norman P. The use of two-stage exchange arthroplasty with depot antibiotics in the absence of long-term antibiotic therapy in infected total hip replacement. J Bone Joint Surg Br. 2008;90:145–8. doi: 10.1302/0301-620X.90B2.19855. [DOI] [PubMed] [Google Scholar]
- 4.Winkler H, Kaudela K, Stoiber A, Menschik F. Bone grafts impregnated with antibiotics as a tool for treating infected implants in orthopedic surgery - one stage revision results. Cell Tissue Bank. 2006;7:319–23. doi: 10.1007/s10561-006-9010-3. [DOI] [PubMed] [Google Scholar]
- 5.Winkler H, Stoiber A, Kaudela K, Winter F, Menschik F. One stage uncemented revision of infected total hip replacement using cancellous allograft bone impregnated with antibiotics. J Bone Joint Surg Br. 2008;90:1580–4. doi: 10.1302/0301-620X.90B12.20742. [DOI] [PubMed] [Google Scholar]
- 6.Anract P, Coste J, Vastel L, Jeanrot C, Mascard E, Tomeno B. Proximal femoral reconstruction with megaprosthesis versus allograft prosthesis composite: A comparative study of functional results, complications and longevity in 41 cases. [In French] Rev Chir Orthop Reparatrice Appar Mot. 2000;86:278–88. [PubMed] [Google Scholar]
- 7.Farid Y, Lin PP, Lewis VO, Yasko AW. Endoprosthetic and allograft-prosthetic composite reconstruction of the proximal femur for bone neoplasms. Clin Orthop Relat Res. 2006;442:223–9. doi: 10.1097/01.blo.0000181491.39048.fe. [DOI] [PubMed] [Google Scholar]
- 8.Della Valle CJ, Shuaipaj T, Berger RA, Rosenberg AG, Shott S, Jacobs JJ, et al. Revision of the acetabular component without cement after total hip arthroplasty. A concise follow-up, at fifteen to nineteen years, of a previous report. J Bone Joint Surg Am. 2005;87:1795–800. doi: 10.2106/JBJS.D.01818. [DOI] [PubMed] [Google Scholar]
- 9.Engh CA, Glassman AH, Griffin WL, Mayer JG. Results of cementless revision for failed cemented total hip arthroplasty. Clin Orthop Relat Res. 1988;235:91–110. [PubMed] [Google Scholar]
- 10.Harris WH. Results of uncemented cups: A critical appraisal at 15 years. Clin Orthop Relat Res. 2003;417:121–5. doi: 10.1097/01.blo.0000096824.67494.aa. [DOI] [PubMed] [Google Scholar]
- 11.Goodman S, Saastamoinen H, Shasha N, Gross A. Complications of ilioischial reconstruction rings in revision total hip arthroplasty. J Arthroplasty. 2004;19:436–46. doi: 10.1016/j.arth.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 12.Gross AE, Goodman S. The current role of structural grafts and cages in revision arthroplasty of the hip. Clin Orthop Relat Res. 2004;429:193–200. doi: 10.1097/01.blo.0000149822.49890.5e. [DOI] [PubMed] [Google Scholar]
- 13.Hooten JP, Jr, Engh CA, Heekin RD, Vinh TN. Structural bulk allografts in acetabular reconstruction: Analysis of two grafts received at post-mortem. J Bone Joint Surg Br. 1996;78:270–5. [PubMed] [Google Scholar]
- 14.Pollock FH, Whiteside LA. The fate of massive allografts in total hip acetabular revision surgery. J Arthroplasty. 1992;7:271–6. doi: 10.1016/0883-5403(92)90048-u. [DOI] [PubMed] [Google Scholar]
- 15.Bobyn JD, Stackpool GJ, Hacking SA, Tanzer M, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999;81:907–14. doi: 10.1302/0301-620x.81b5.9283. [DOI] [PubMed] [Google Scholar]
- 16.Unger AS, Lewis RJ, Gruen T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty: Clinical and radiological results of 60 hips. J Arthroplasty. 2005;20:1002–9. doi: 10.1016/j.arth.2005.01.023. [DOI] [PubMed] [Google Scholar]
- 17.Lakstein D, Backstein D, Safir O, Kosashvili Y, Gross AE. Trabecular Metal™ Cups for acetabular defects with 50% or less host bone contact. Clin Orthop Relat Res. 2009;467:2318–24. doi: 10.1007/s11999-009-0772-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanssen AD, Lewallen DG. Modular acetabular augments: Composite void fillers. Orthopedics. 2005;28:971–2. doi: 10.3928/0147-7447-20050901-29. [DOI] [PubMed] [Google Scholar]
- 19.Ballester Alfaro JJ, Sueiro Fernández J. Trabecular metal buttress augment and the trabecular metal cup-cage construct in revision hip arthroplasty for severe acetabular bone loss and pelvic discontinuity. Hip Int. 2010;20:119–27. doi: 10.1177/11207000100200s720. [DOI] [PubMed] [Google Scholar]
- 20.Kellet Catherine F, Gross Allan E, Backstein David, Safir Oleg. Massive acetabular bone loss: The cup-cage solution. Semin Arthroplast. 2010;21:57–61. [Google Scholar]
- 21.Kosashvili Y, Backstein D, Safir O, Lakstein D, Gross AE. Acetabular revision using an anti-protrusion (ilio-ischial) cage and trabecular metal acetabular component for severe acetabular bone loss associated with pelvic discontinuity. J Bone Joint Surg Br. 2009;91:870–6. doi: 10.1302/0301-620X.91B7.22181. [DOI] [PubMed] [Google Scholar]


