Abstract
Objective
Parent and teacher ratings of core attention-deficit/hyperactivity disorder (ADHD) symptoms, as well as behavioral and emotional problems commonly comorbid with ADHD, were compared in children with autism spectrum disorders (ASD).
Method
Participants were 86 children (66 boys; mean: age=9.3 years, intelligence quotient [IQ]=84) who met American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) criteria for an ASD on the Autism Diagnostic Interview–Revised (ADI-R) and the Autism Diagnostic Observation Schedule (ADOS). Parent and teacher behavioral ratings were compared on the Conners' Parent and Teacher Rating Scales (CPRS-R; CTRS-R). The degree to which age, ASD subtype, severity of autistic symptomatology, and medication status mediated this relationship was also examined.
Results
Significant positive correlations between parent and teacher ratings suggest that a child's core ADHD symptoms—as well as closely related externalizing symptoms—are perceived similarly by parents and teachers. With the exception of oppositional behavior, there was no significant effect of age, gender, ASD subtype, or autism severity on the relationship between parent and teacher ratings. In general, parents rated children as having more severe symptomatology than did teachers. Patterns of parent and teacher ratings were highly correlated, both for children who were receiving medication, and for children who were not.
Conclusions
Parents and teachers perceived core symptoms of ADHD and closely-related externalizing problems in a similar manner, but there is less agreement on ratings of internalizing problems (e.g., anxiety). The clinical implication of these findings is that both parents and teachers provide important behavioral information about children with ASD. However, when a clinician is unable to access teacher ratings (e.g., during school vacations), parent ratings can provide a reasonable estimate of the child's functioning in these domains in school. As such, parent ratings can be reliably used to make initial diagnostic and treatment decisions (e.g., medication treatment) regarding ADHD symptoms in children with ASDs.
Introduction
Significant psychiatric comorbidities are common in children with autism spectrum disorders (ASD). Compared with typically-developing peers without an ASD, children and adolescents with an ASD have a higher prevalence of a number of behavioral and emotional concerns, including affective, psychotic, and disruptive behavior disorders (Gadow et al. 2004; Lecavalier 2006; Leyfer et al. 2006; Pearson et al. 2006; Lecavalier et al. 2009; Simonoff et al. 2009). For example, Simonoff and colleagues (2009) noted that 70% of children with ASDs in their population-based sample met American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) criteria for one comorbid psychiatric disorder, and 41% had multiple DSM-IV disorders.
Attention-deficit/hyperactivity disorder (ADHD) symptoms in ASD
Symptoms of ADHD are a significant concern seen in many children with ASDs. Although DSM-IV does not allow the formal diagnosis of ADHD in a child with an ASD, recent findings suggest that significant ADHD symptomatology (i.e., inattention, hyperactivity, and impulsivity) may be present in up to 78% of children and adolescents with ASDs (Gadow et al. 2006; Lee and Ousley 2006; Reiersen et al. 2007; Guerts et al. 2008; Reiersen et al. 2008; Sinzig et al. 2008). Comorbid symptomatology such as ADHD can seriously undermine educational and social functioning in children with ASDs, and by late elementary school, may rival the core symptoms of autism itself in terms of impairment (Loveland et al. 2005; Pearson et al. 2006).
ADHD behavioral ratings in children with and without ASDs
An important step in addressing ADHD symptoms in children with ASD is to evaluate their pervasiveness across home and school settings. A key issue in this assessment is the congruence between informants providing information about the child's functioning. Although positive correlations between parent and professional ratings have been noted with regard to developmental status (Dinnebeil and Rule 1994), other studies have revealed informant discrepancies in reports of behavioral and emotional functioning (Achenbach et al. 1987; Mitsis et al. 2000; De Los Reyes and Kazdin 2005; Rowland et al. 2008).
A number of factors contribute to these discrepancies, including the child's age, the type of behavioral or emotional problem, and differing contexts between home and school. Parents and teachers of elementary school age children have been found to have higher agreement regarding behavioral functioning than do parents and teachers of either preschoolers or older adolescents, perhaps reflecting the fact that elementary school age children spend more time with both sets of these informants than do younger or older children (Achenbach et al. 1987; Szatmari et al. 1994). Discrepancies between parents and teachers have been noted in both internalizing and externalizing symptoms (Tassé and Lecavalier 2000). However, parent–teacher agreement has been found to be particularly discordant when estimating internalizing symptomatology (e.g., anxiety) as compared with externalizing symptomatology (e.g., oppositional behavior) (Achenbach et al. 1987; Stanger and Lewis 1993; Kanne et al. 2009).
Some studies have linked parent–teacher discrepancies to divergent informant perspectives, and to discontinuity in context across settings (Achenbach et al. 1987; Szatmari et al. 1994; Tassé and Lecavalier 2000; Hartman et al. 2007). Szatmari et al. (1994) noted that classrooms are often more structured and have more resources for managing behavior (e.g., aides). Hartman et al. (2007) suggested that teachers may also have more opportunity to observe ADHD symptoms, given the more stringent demands of a classroom. A closely related factor potentially contributing to these disparities is informant bias (Szatmari et al. 1994). For example, maternal depression may influence parent ratings, and teacher ratings may be less influenced by the developmental history of the child (Szatmari et al. 1994). Teachers also have a larger potential normative group against which to rate a child (Tassé and Lecavalier 2000; Hartman et al. 2007). Such disparities support the inclusion of multiple informants as part of the diagnostic process (Dinnebeil and Rule 1994; Mitsis et al. 2000; Tassé and Lecavalier 2000; Sullivan and Riccio 2007).
Informant concordance and medication treatment
Interestingly, some investigators suggest that informant discrepancies can depend upon treatment response. Faraone et al. (2005) found that when a child shows stimulant-related improvements in ADHD symptoms, both the parents and teachers are likely to confirm each other's reports of a therapeutic improvement. Because they provide essentially overlapping information, both sets of informants may not be needed in this situation. However, when one informant did not report behavioral improvement (or even a decline in behavior) in response to treatment, there was far less concordance between the informants' assessments of treatment response. In the latter situation, multiple respondents provided non-redundant information.
Despite these issues, a number of studies have explored the comparison of ADHD behavior across home and school settings in children in the general school-age population. Many of these studies have found evidence of moderate relationships between parent and teacher ratings of ADHD symptomatology (Hartman et al. 2007; Sullivan and Riccio 2007). In some studies, parents reported more severe ADHD behaviors than did teachers (e.g., Sullivan and Riccio 2007), whereas in others, teachers reported more severe symptoms (e.g., Amador-Campus et al. 2006). Interestingly, there is sometimes greater agreement between parents and teachers regarding specific symptoms of ADHD than there is for ADHD subtype (Mitsis et al. 2000; Rowland et al. 2008). Mitsis et al. (2000) also noted greater parent–teacher agreement for hyperactive/impulsive symptoms than for inattentive symptoms.
To date, little is known about the concordance of parental and teacher ratings of behavioral adjustment in children with autism because few studies have examined this issue. Szatmari et al. (1994) noted that although parents and teachers had high levels of agreement with regard to adaptive function, there was little agreement with regard to ratings of autistic symptomatology. However, other investigators (e.g., Constantino et al. 2007; Kanne et al. 2009) have found more evidence of parent–teacher agreement with regard to autistic severity. In their examination of problem behaviors, Kanne et al. (2009) also found greater parent–teacher concordance for externalizing than for internalizing symptoms, although they noted that even for externalizing symptoms, the correlations of parent–teacher behavioral ratings were only moderate.
Although previous investigations suggested that assessment using both parent and teacher behavioral ratings is ideal (Stanger and Lewis, 1993; Mitsis et al. 2000; Tassé and Lecavalier 2000; De Los Reyes and Kazdin, 2005), there are circumstances in which important decisions regarding a child's care must be made with only one of these important sources of information available to the clinician. Examples of such circumstances are titrating medication response during the summer months, when it is often not possible to obtain teacher ratings, and making decisions regarding a child's psychosocial treatment in conjunction with a move to a new school and/or city. There are also circumstances in which there may be concerns regarding the reliability of either the parent or teacher rater. Reliability of teacher reports can be compromised by their heavy workloads. Another factor can be decreasing familiarity with the child starting in middle school, when multiple teachers are involved instead of one (Faraone et al. 2005). In addition, it is important to know if there are some subgroups of children (e.g., younger/older, less/more severe ASD symptomatology) on the autism spectrum for whom it is especially critical to have both sets of ratings to make these important decisions.
The primary purpose of this study was to examine the relationship between parent and teacher behavior ratings of children with ASD with regard to core ADHD symptoms (i.e., inattention, hyperactivity, and impulsivity) and with regard to externalizing symptoms (e.g., oppositional behavior) and internalizing symptoms (e.g., anxiety) that are commonly comorbid with ADHD. A secondary goal was to assess whether age, autism spectrum subtype, severity of autistic symptomatology, and medication status influenced the relationship between parent and teacher ratings.
Methods
Participants
Characteristics of the children are listed in Table 1. Intelligence quotient (IQ) was derived from the Stanford-Binet Intelligence Scale, 5th edition (Roid 2003). Participants were 86 children (66 boys; mean age=9.3 yrs; mean Full Scale IQ=84.1) who met American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, 4th ed., Text Revision (DSM-IV-TR) criteria for an ASD. They were assessed using the Autism Diagnostic Interview–Revised (ADI-R) (Rutter et al. 2003), the Autism Diagnostic Observation Schedule (ADOS) (Lord et al. 2001), a clinical interview, clinic observation, and a record review by two licensed psychologists (Drs. Pearson and Loveland) who are both highly experienced in the assessment and diagnosis of ASDs, and who are certified as meeting research reliability on both the ADI-R and the ADOS. Clinical diagnoses of ASD subtype were determined by clinical interview, clinic observation of the child, and independent case review (by Drs. Pearson and Loveland). Clinical diagnoses for these children were autistic disorder (n=50), pervasive developmental disorder-not otherwise specified (PDD-NOS) (n=20), and Asperger's disorder (n=16). The racial and ethnic breakdown of the entire sample was 49 (57%) Caucasian (non-Hispanic), 19 (22%) Hispanic, 12 (14%) African-American, 5 (6%) Asian, and 1 (1%) multi-racial/unknown. Among the 86 children who participated in this study, 41 (or 47%) were being treated with psychoactive medication at entry, including psychostimulants (n=29), antipsychotics (n=16), antidepressants (n=13), a norepinephrine reuptake inhibitor (atomoxetine) (n=4), antihypertensives (n=4), a mood stabilizer (n=1), and an anxiolytic (n=1). Eighteen children (21%) were taking two medications, and six children (7%) were receiving three or more.
Table 1.
Sample Characteristics
| Variable | Mean | SD | Range |
|---|---|---|---|
| Chronological age (years) | 9.3 | 1.9 | 6.7–13.5 |
| Stanford–Binet Intelligence Scale, 5th Ed. | |||
| Verbal IQ | 82.8 | 21.8 | 47–127 |
| Nonverbal IQ | 86.9 | 18.0 | 50–127 |
| Full scale IQ | 84.1 | 19.6 | 46–128 |
| Verbal age equivalent | 8.3 | 6.8 | 2.8–55 |
| Nonverbal age equivalent | 8.1 | 2.9 | 3.4–21 |
| Full scale age equivalent | 7.9 | 3.2 | 3.1–21 |
| Vineland Adaptive Behavior Scales–II | |||
| Communication Domain | 76.2 | 8.6 | 59–97 |
| Daily Living Skills Domain | 78.6 | 9.9 | 55–112 |
| Socialization Domain | 75.6 | 8.1 | 57–104 |
| Vineland Composite | 75.2 | 7.8 | 57–95 |
| Social Communication Questionnaire | 22.5 | 5.5 | 12–36 |
| ADI–R Summary Score | 47.7 | 11.0 | 23–66 |
| Hollingshead 4 Factor Social Class | 1.9 | 1.0 | 1–5 |
| Hollingshead 4 Factor SES Score | 50.3 | 12.9 | 11–66 |
| Educational level (# years) | |||
| Father | 16.1 | 3.0 | 9–25 |
| Mother | 15.7 | 2.3 | 12–21 |
| Gender | |||
| Male | 66 | ||
| Female | 20 | ||
| Primary educational placement | |||
| Regular education class with no modifications | 15 | ||
| Regular education/inclusion class with modifications | 9 | ||
| Regular education/inclusion class with an aide | 5 | ||
| Resource class | 24 | ||
| Self-contained class | 23 | ||
| Private school for autism spectrum disorder | 10 | ||
| Autism spectrum disorder subtype | |||
| Autistic disorder | 50 | ||
| PDD-NOS | 20 | ||
| Asperger's disorder | 16 | ||
SD=standard deviation; IQ=intelligence quotient; ADI–R=Autism Diagnostic Interview–Revised; SES=socioeconomic status; PDD-NOS=pervasive developmental disorder–not otherwise specified.
Exclusion criteria were sensory limitations (e.g., blindness), motor limitations severe enough to prevent adequate testing, and English not being the child's first language. Children were referred from the special education classrooms of a large metropolitan school district, from community agencies/clinics, and from parent advocacy groups (e.g., The Arc of Greater Houston, Houston Families for Effective Autism Treatment). All of the children were living with their families. Written informed consent was obtained from parents and from participants aged 12–13 years, and assent was obtained from the younger children. This study was approved by the Committee for the Protection of Human Subjects at the University of Texas Health Science Center at Houston.
Instruments
Behavioral functioning was assessed using the Conners' Parent Rating Scale-Revised (CPRS-R) and Conners' Teacher Rating Scale-Revised (CTRS-R) (Conners 1997). These widely used questionnaires assess ADHD symptomatology (i.e., inattention, hyperactivity, impulsivity), and comorbid behaviors commonly associated with ADHD, including both externalizing (e.g., oppositional behavior) and internalizing (e.g., anxiety) symptoms. They are also used extensively to assess medication treatment response in children.
The long forms of the CPRS-R (80 items) and the CTRS-R (59 items) were used. The CPRS-R includes seven symptom-specific subscales (Oppositional, Cognitive Problems/Inattention, Hyperactivity, Anxious-Shy, Perfectionism, Social Problems, Psychosomatic), four index scales (ADHD Index, Conners' Global Index: Restless-Impulsive, Conners' Global Index: Emotional Lability, Conners' Global Index: Total), and three DSM-IV subscales for ADHD (Inattentive, Hyperactive-Impulsive, Total ADHD). The CTRS-R has parallel subscale construction, with the exception of the Psychosomatic subscale. Both versions are normed for children and adolescents 3–17 years old. Estimates of symptom severity were obtained using T-scores (mean=50, SD=10); higher T-scores reflected greater psychopathology.
Procedure
Each child's primary caregiver completed the CPRS-R at home as part of our screening procedure. Teachers were sent the CTRS-R at their classrooms, and were instructed to mail them directly back to the clinic. For children who were taking medication (particularly stimulants), both parents and teachers were instructed, to the extent possible, to complete their questionnaires by rating the child's behavior when he or she was not taking medication.
Results
Statistical approach
The data were analyzed using correlational and multivariate techniques with SPSS-PC (Version 19.0) and SAS JMP 8 for Macintosh. Type III sums of squares were used to test all effects in which there were two or more predictor variables. To assess the relationship between parent and teacher ratings, we computed Pearson correlations between the comparable CPRS-R and CTRS-R subscales (e.g., CPRS-R Hyperactivity subscale and CTRS-R Hyperactivity subscale). To determine if the relationship between parent and teacher ratings was affected by age, ASD subtype, or severity of autistic symptomatology, we used a linear regression model in which each of the CPRS-R subscale scores (e.g., CPRS-R Hyperactivity T-scores) was predicted by the corresponding CTRS-R subscale score (e.g., CTRS-R Hyperactivity T-scores), age, gender, autism subtype (autistic disorder, PDD-NOS, Asperger's disorder), autism severity (Social Communication Questionnaire [SCQ], ADI-R scores), race/ethnicity, parental education, and socioeconomic status as well as all two-way interactions among these variables. For the one rating scale in which there was an interaction with autism subtype (Oppositional), correlations were computed separately as a function of the levels of the interacting variable. To address the effects of medication status on parent and teacher correlations, we compared the correlations of parent–teacher behavioral ratings for children who were taking medication versus those who were not, using multivariate techniques.
To assess possible differences between parents and teachers in their ratings of symptom severity, differences between parent and teacher T-scores on each subtest were computed for each child (e.g., CPRS-R Hyperactivity versus CTRS-R Hyperactivity). A multivariate test (Wilks λ) of these difference scores was then conducted, along with follow-up univariate tests to assess the main effect of rater on each individual subtest. Multivariate analyses of variance were also conducted to assess whether or not ASD subtype or medication status influenced the difference between parent and teacher perceptions of behavioral severity in children with ASD.
Relationship of parent–teacher ratings
ADHD/externalizing behavior
As shown in Table 2, parent and teacher ratings of ADHD and externalizing behaviors had moderate-to-high correlations (e.g., Inattention [r=0.63, p<0.0001], Hyperactivity [r=0.46, p<0.0001], and Social Problems [r=0.35, p=0.001]). With only one exception (discussed later), there were no significant effects of age, gender, ASD subtype, autism severity, parental education, or socioeconomic status on these relationships between parent and teacher ratings. Therefore, for the most part, it would appear that these findings of similar parent and teacher ratings of ADHD/externalizing ratings were consistent across 1) the age range of children in this sample, 2) boys and girls, 3) ASD subtype, and 4) autistic symptom severity.
Table 2.
Conners' Parent and Teacher Behavioral Ratings: Means, Correlations, and Univariate Tests
| |
Conners' Parent Rating Scale (CPRS–R) T-scores |
Conners' Teacher Rating Scale (CTRS–R) T-scores |
Correlation: CPRS–R with CTRS–R |
Univariate tests: Main effect of rater (CPRS–R versus CTRS–R) |
||||
|---|---|---|---|---|---|---|---|---|
| Subscale | Mean | SD | Mean | SD | r | p | F | p |
| Oppositional | 60.27 | 13.98 | 62.22 | 16.34 | 0.470 | ≤0.0001 | 0.14 | 0.711 |
| Inattention | 70.13 | 11.76 | 60.37 | 10.19 | 0.633 | ≤0.0001 | 67.42 | <0.0001 |
| Hyperactivity | 72.21 | 14.67 | 63.27 | 12.47 | 0.461 | ≤0.0001 | 27.05 | <0.0001 |
| Anxious/Shy | 62.50 | 14.77 | 65.73 | 13.83 | 0.069 | 0.53 | 3.59 | 0.062 |
| Perfectionism | 62.14 | 12.51 | 60.55 | 14.67 | 0.150 | 0.17 | 0.43 | 0.514 |
| Social Problems | 77.12 | 13.35 | 67.47 | 12.92 | 0.350 | 0.001 | 23.81 | <0.0001 |
| ADHD Index | 71.88 | 11.41 | 66.06 | 11.24 | 0.559 | ≤0.0001 | 19.15 | <0.0001 |
| Global Index: Restless/Impulsivity | 71.15 | 13.30 | 65.63 | 11.05 | 0.508 | ≤0.0001 | 16.20 | <0.0001 |
| Global Index: Emotional Liability | 60.88 | 13.85 | 66.24 | 16.42 | 0.435 | ≤0.0001 | 6.60 | 0.012 |
| Global Index: Total | 69.36 | 13.67 | 67.70 | 11.92 | 0.457 | ≤0.0001 | 2.00 | 0.161 |
| DSM-IV: Inattentive | 70.90 | 11.38 | 63.57 | 10.92 | 0.567 | ≤0.0001 | 32.38 | <0.0001 |
| DSM-IV: Hyperactive-Impulsive | 72.45 | 13.34 | 62.20 | 12.63 | 0.433 | <0.0001 | 35.94 | <0.0001 |
| DSM IV: Total | 73.21 | 11.68 | 64.15 | 11.11 | 0.537 | ≤0.0001 | 45.53 | <0.0001 |
n=86.
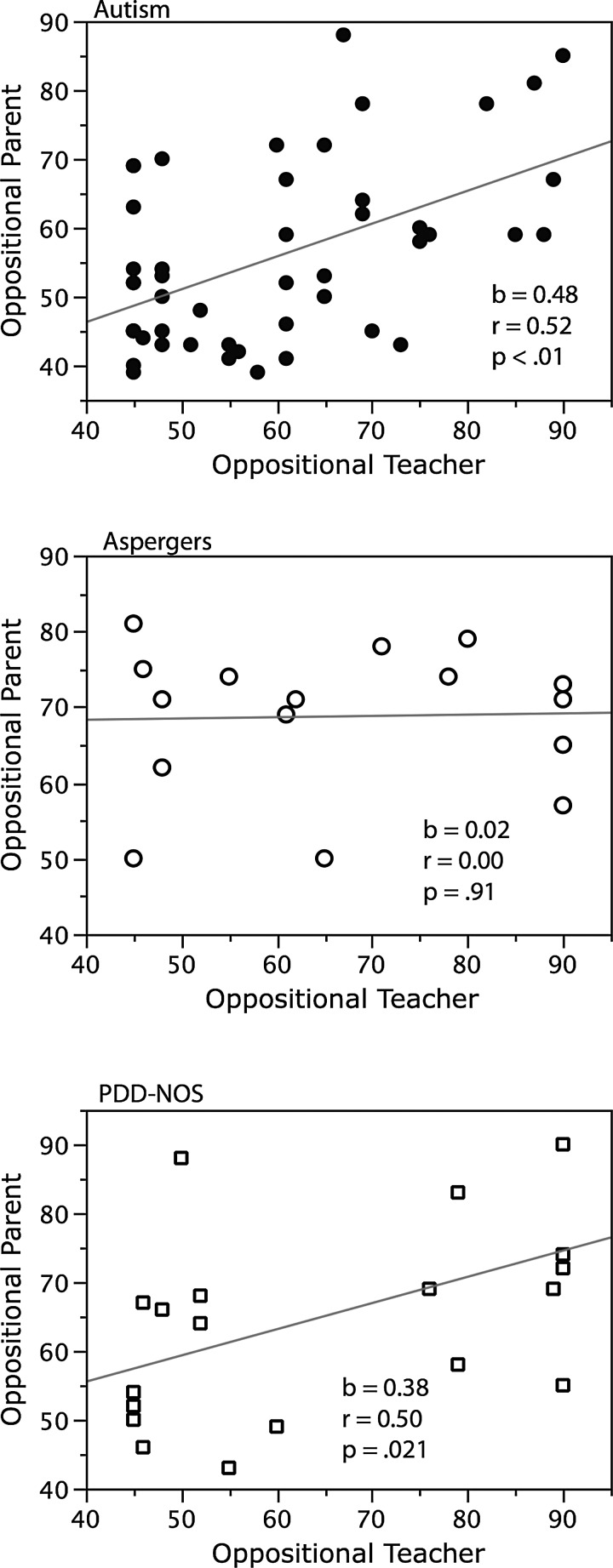
The only exception to this agreement between parent and teacher ratings occurred on the Oppositional subscale for the Asperger subgroup. As can be seen in Figure 1, parent and teacher ratings of oppositional behaviors were highly concordant for children with autism (r=0.52, p<0.01) and for children with PDD-NOS (r=0.50, p=0.02), but were not at all concordant for children in the Asperger subsample (r=0.00, p=0.91). Whereas the slope of the relationship between parent and teacher ratings of oppositional behavior differed by autism subtype in a manner paralleling these correlations, F (2,77)=3.36, p=0.04, there was no significant effect of age, gender, or severity of autistic symptomatology on the slope of this relationship. Although not a prime focus of this study, it is interesting to note that the mean parent and teacher T-scores of oppositional behavior for children in the autism group (parent=55.5; teacher=59.4) were somewhat lower than those of children in the PDD-NOS group (parent=65.4; teacher=65.9) and the Asperger's group (parent=68.8; teacher=66.5).
FIG. 1.
The relationship between parent and teacher ratings of oppositional behaviors in children with autism, children with Asperger's, and children with pervasive developmental disorder–not otherwise specified (PDD-NOS).
Internalizing behaviors
Parent and teacher ratings of internalizing symptomatology were far less concordant, as indicated by low and non-significant correlations on subscales tapping anxiety (r=0.07, p=0.53) and perfectionism (r=0.15, p=0.17). This pattern of lower correlation between parent and teacher ratings of internalizing symptoms was similar for all ASD subtypes. Similar to our findings on externalizing symptomatology, there was no significant effect of age, gender, or severity of autistic symptomatology on the slope of the relationship between parent and teacher ratings.
Effect of medications on parent–teacher correlations
Although parents and teachers were asked to rate the children off medication, teachers may have had less opportunity than parents to see the children off medications. If true, it may have led to lower parent–teacher agreement for children who were on medications, as compared with those who were not. For this reason, we compared the correlations of parent–teacher behavioral ratings for children who were taking medication versus those who were not. Interestingly, there was no evidence that the correlation between parent and teacher ratings differed as a function of psychotropic medication status. The 12 differences between parent and teacher correlations ranged from −0.26 to 0.33, and none of these differences approached significance. The largest difference was found for the Anxiety-Shy subscale, on which the parent–teacher correlation for children not taking and taking psychotropic medication were 0.22 and 0.10, respectively (Z=1.47, p=0.141). Comparable results were obtained when comparing parent–teacher correlations between children who were taking psychostimulant medications to those who were not. In this instance, the 12 differences between parent and teacher correlations ranged from −0.35 to 0.24, and again none of these correlations approached significance. The largest difference was found for the Inattention subscale, for which the correlation for those not taking stimulant medication was 0.58 and the correlation for those on stimulant medication was 0.77 (Z=−1.48, p=0.139). These findings would suggest that parent and teacher agreement regarding a child's behavioral functioning is similar, regardless of whether they are taking psychoactive medication.
Parent–teacher differences in severity of behavioral ratings
The initial multivariate test of the overall difference between parent and teacher behavioral ratings was significant, F (12, 72)=10.60, p<0.001, indicating that parents and teachers differ in the severity of their behavioral ratings.
ADHD/externalizing symptoms
As seen in Table 2, univariate follow-up analyses revealed that parents gave higher (more severe) ratings than did teachers on the core ADHD symptoms, i.e., inattention, F (1,83)=67.42; p<0.0001; hyperactivity, F (1,83)=27.05, p<0.0001; as well as on closely related comorbid symptoms (social problems F [1,83]=23.81, p<0.0001). Therefore, even though there was a high correlation between the parent and teacher ratings (i.e., parents and teachers tended to give high ratings to the same children and low ratings to the same children), the teachers tended to rate the child's behavior as being less problematic than did the parents. None of the individual subscales showed evidence that the differences in severity between parent and teacher ratings differed as a function of ASD subtype (p>0.40 in all cases).
Internalizing symptoms
Interestingly, in contrast to the pattern found between parent and teacher ratings of severity of core ADHD and externalizing symptoms, the overall means of parent and teacher internalizing scores were similar and did not differ significantly (e.g., anxiety, F [1,83]=3.59, p=0.062, and perfectionism, F [1,83]=0.43, p=0.514). The only exception to this finding was in the area of emotional lability, on which teachers provided more severe ratings than did parents (F [1,83]=6.60, p=0.012). None of the subscales scores for internalizing symptoms differed between parent and teacher as a function of ASD subtype.
Effects of ASD subtype and medication treatment on differences in parent–teacher ratings of symptom severity
A multivariate analysis of variance was conducted using ASD subtype as the independent variable and the difference scores (between parent and teacher T-scores) as the dependent variables. There was no evidence of an effect of ASD subtype on the overall difference between parent and teacher ratings (Wilks λ=0.802, F [24, 144]=0.70, p=0.844). The patterns of parent–teacher rating differences were similar in children who were being treated with psychoactive medication and in children who were not taking medication, and did not differ significantly (F [12,73]=1.09, p=0.379); they were also similar and not significantly different for children who were, or were not, taking psychostimulants (F [12,73]=0.357, p=0.97).
Discussion
These findings suggest that for the most part, parents and teachers of children with ASDs perceive core symptoms of ADHD, and externalizing symptoms such as oppositional behavior, in a similar manner. These findings are consistent with previous findings of greater agreement between parents and teachers regarding ratings of externalizing behavior in samples of elementary school age children who are typically developing (Achenbach et al. 1987). Externalizing behaviors are more observable and more likely to cause management problems, making them more salient to external observers (Stanger and Lewis, 1993). Consistent with previous studies (Szatmari et al. 1994; Gadow et al. 2006), no effect of gender was found—although as in these earlier studies, our sample size did not allow extensive analyses of a sex effect. Future studies that oversample girls with ASDs are needed to address this question more conclusively.
Of note, in our sample of children with ASDs, parents tended to report higher levels of core ADHD symptom severity than did teachers. Neither ASD subtype nor the presence/absence of psychoactive medication treatment affected this tendency. Although some studies of children in the general school-age population have found that teachers produce higher ADHD ratings (Mitsis et al. 2000; Amador-Campos et al. 2006), studies of children with developmental disorders such as intellectual disabilities (ID) and autism have found that teachers report less severe symptoms of ADHD (Tassé and Lecavalier 2000). Perhaps teachers who work with children with developmental disabilities are accustomed to the higher levels of ADHD symptoms seen in children with intellectual and developmental disabilities (Pearson et al. 1997), and rate their students against this higher-baseline-ADHD comparison group. If this is the case, it may contribute to a tendency by teachers of children with ASDs or ID to rate their students as not being as severe in ADHD symptomatology relative to other raters (e.g., teachers in mainstream classrooms, parents). Therefore, although teachers in mainstream classrooms have a “calibration advantage” over parents in having many typically developing children of the same age and sex to compare with, it may be the case that some teachers of special classes may develop a mirror-image “calibration disadvantage” induced by consistent exposure to special needs students such that their impression of the norm becomes somewhat biased.
Additionally, the behavior of children with ASDs may actually have been better in school than at home, given that they are typically served in special education classrooms with a high staff–student ratio or in a mainstream classroom with an individual aide, and that their day was highly structured with an Individualized Education Program (IEP) to avoid frustration. This situation would be the opposite of that for typically developing children, most of whom do not have these supports and who may face more challenges in the classroom than at home.
Despite the instructions to parents and teachers to rate children in their unmedicated state, another factor that might have had played a role in the less-severe ratings given by teachers was that teachers sometimes have fewer opportunities to see children off medications than do parents—especially in this era of long-acting formulations of medicines. Although this may have been the case for some (medicated) children in this study, no significant effect of medications was found on the relationship between parent and teacher ratings. Given that many children with ASDs are being treated with psychoactive medications (Aman et al. 2005), our findings suggest that: 1) parent and teacher ratings are highly correlated, at least with regard to core ADHD symptomatology and comorbid disruptive behaviors, and 2) parents tend to provide more severe behavioral ratings whether or not a particular child is taking psychotropic medication.
Interestingly, although parents and teachers were largely concordant with regard to ADHD and externalizing symptomatology, their perceptions of internalizing symptoms (e.g., anxiety) appeared to be less concordant. These findings are very consistent with the finding of lower parent–teacher agreement for internalizing symptoms than for externalizing symptoms, both in the general school-age population (Achenbach et al. 1987) and in children with autism spectrum disorders (Kanne et al. 2009). These findings would suggest that both parent and teacher input are particularly important when assessing internalizing symptoms in children with autism. As noted by others (Achenbach et al. 1987; Tassé and Lecavalier 2000), the effect of the different contexts may also contribute to the divergence in behavioral ratings, particularly with regard to internalizing symptomatology. Another potential contributing factor to the divergence between parent and teacher ratings of internalizing behavior may be that the subscale items on the CPRS-R and CTRS-R are not entirely identical. Although differences between subscale items on the CPRS-R and CTRS-R reflect contextual differences (e.g., in the way anxiety is expressed in these different settings), this aspect may have influenced parent–teacher agreement on the internalizing subscales. However, the same can be said about the externalizing subscales.
Although not a prime focus of this investigation, our findings were suggestive of considerable parent–teacher agreement for Conners' subscales targeting both individual symptoms (e.g., inattention, hyperactivity) and for subscales tapping overall DSM-IV subscale symptomatology (e.g., DSM-IV Inattention, DSM-IV Hyperactivity/Impulsivity, DSM-IV Total). This finding differs from some others who found less agreement for DSM-IV subtypes, but it is very important to note that previous investigations (Mitsis et al. 2000) relied on categorical rankings afforded by interview techniques, rather than continuous scores provided by questionnaires. The possible greater emphasis on dimensional assessment of ADHD in American Psychiatric Association Association Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (DSM-V) may lead to greater alignment between parent and teacher ratings. For example, Mitsis et al. (2000) noted that much of the discrepancy in parent–teacher agreement regarding ADHD subtype was the result of differences of opinion between informants regarding a single symptom (e.g., a score of six symptoms in a domain yields an endorsement of serious ADHD symptomatology within that domain, whereas a score of five does not.) A possible greater emphasis on dimensional measurement of symptoms in DSM-5 may avoid this problem.
A notable exception to our general finding of high agreement between parents and teachers regarding externalizing symptoms was that there was essentially no relationship between parent and teacher ratings of oppositional behavior in children with a clinical diagnosis of Asperger's. This finding is intriguing, given that it mirrors the finding in the general elementary school-age population that ratings of oppositional defiant disorder (ODD) may be highly dependent on the rater of those behaviors (Drabick et al. 2007). Guttmann-Steinmetz et al. (2009) suggested that an ASD may significantly alter the ODD phenotype. Interestingly, Gadow et al. (2004) noted that preschoolers with Asperger's were rated by both parents and teachers as being more oppositional than were preschoolers with either autism or PDD-NOS. Our finding of greater disagreement between parents and teachers of children with Asperger's with regard to oppositional symptoms should be interpreted with caution, given that multiple statistical interactions were explored, and given that the Asperger's subsample had a total sample size of only 16. Although the DSM-5 may eliminate the current Asperger's diagnostic category, these findings suggest that clinicians should be particularly careful to obtain parent and teacher ratings for high-functioning children on the autism spectrum for whom oppositional behavior is a significant concern. This issue clearly warrants further investigation, given that disruptive behavior problems appear to elevate parental stress in children with ASDs, and that this relationship between behavioral problems and stress is exacerbated over time (Lecavalier et al. 2006).
Limitations
Finally, we note some limitations of this study. The children in this study were relatively high functioning, with a mean IQ of 84. The relationship between parent and teacher ratings may be different in children who were lower functioning. The sample size was relatively small, reflecting a clinic-based study rather than an epidemiological sample. Therefore, although we found no evidence that parent–teacher ratings differed as a function of ASD subtype or treatment with psychoactive medication, it is always possible that some differences existed that were not detected by this study. The sample was recruited for a study of ADHD symptoms in children with ASDs. Although children both with and without significant symptoms of ADHD were recruited for this project, it may be that parents who were most concerned by their child's ADHD symptoms were particularly motivated to participate. If this was true, it may have contributed to the more severe parent ratings of ADHD symptomatology. However, even with this caveat, the findings of this study would arguably be most pertinent to precisely this subset of families—that is, families who are very concerned about their child's symptoms of ADHD.
Conclusions
In conclusion, and in agreement with previous studies, our findings suggest that parent and teacher behavioral ratings are both important components in the evaluation of children with ASDs, particularly when assessing internalizing symptoms and perhaps also when evaluating high-functioning children on the autism spectrum. However, when teacher behavioral ratings are unavailable for an elementary school age child with an autism spectrum diagnosis (e.g., during the summer), parent ratings of core ADHD behaviors (e.g., inattention, hyperactivity, and impulsivity) appear to provide a reasonable estimate of the child's functioning in these domains in the school.
Clinical significance
The clinical implication of this study is that when a clinician is unable to access teacher ratings, parent ratings of ADHD symptoms in children with ASD can be reliably used to contribute helpful information in making diagnostic and treatment (e.g., medication titration) decisions for their patients. As always, information from behavioral questionnaires should be interpreted within the context of a comprehensive evaluation that includes clinical interview and observation.
Disclosures
Dr. Pearson and Ms. Mansour have received travel reimbursement from the Forest Research Institute, and research support from Curemark LLC. Dr. Pearson has also served as a consultant to Curemark LLC and to United BioSource Corporation. Michael Aman, Ph.D. has received research contracts, consulted with, or served on advisory boards of Biomarin Pharmaceuticals, Bristol-Myers Squibb, Confluence Pharmaceutica, Forest Research, Hoffman LaRoche, Johnson & Johnson, and Supernus Pharmaceutica. Dr. Arnold has received research funding from CureMark, Lilly, NIMH, and Shire, has consulted to Organon, NIDA, Sigma Tau, and Targacept, and has served on advisory boards for AstraZeneca, Biomarin, Novartis, Noven, and Seaside Therapeutics. Dr. Santos and Ms. Ezzell have received research support from Curemark LLC. Dr. Casat has received research funding from Eli Lilly, Novartis, and Abbott Laboratories. Dr. Jerger has served as a consultant to Pearson Assessments/Psychological Corporation. The other authors report no biomedical financial interests or potential conflicts of interest.
References
- Achenbach TM. McConaughy SH. Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychol Bull. 1987;101:213–232. [PubMed] [Google Scholar]
- Amador–Campos JA. Forns–Santacana M. Guardia–Olmos J. Pero–Cebollero M. DSM-IV attention deficit hyperactivity disorder symptoms: Agreement between informants in prevalence and factor structure at different ages. J Psychopathol Behav Assess. 2006;28:23–32. [Google Scholar]
- Aman MG. Lam KSL. Van Bourgondien ME. Medication patterns in patients with autism: Temporal, regional, and demographic influences. J Child Adolesc Psychopharmacol. 2005;15:116–126. doi: 10.1089/cap.2005.15.116. [DOI] [PubMed] [Google Scholar]
- Conners CK. Conners' Rating Scales–Revised. North Tonawanda, NY: MHS; 1997. [Google Scholar]
- Constantino JN. LaVesser PD. Zhang Y. Abbacchi AM. Gray T. Todd RD. Rapid quantitative assessment of autistic social impairment by classroom teachers. J Am Acad Child Adolesc Psychiatry. 2007;46:1668–1676. doi: 10.1097/chi.0b013e318157cb23. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A. Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychol Bull. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Dinnebeil LA. Rule S. Congruence between parents' and professionals' judgments about the development of young children with disabilities. Topics Early Child Spec Educ. 1994;14:1–25. [Google Scholar]
- Drabick DAG. Gadow KD. Loney J. Source-specific oppositional defiant disorder: Comorbidity and risk factors in referred elementary schoolboys. J Am Acad Child Adolesc Psychiatry. 2007;46:92–101. doi: 10.1097/01.chi.0000242245.00174.90. [DOI] [PubMed] [Google Scholar]
- Faraone SV. Biederman J. Zimmerman B. Correspondence of parent and teacher reports in medication trials. Eur Child Adolesc Psychiatry. 2005;14:20–27. doi: 10.1007/s00787-005-0415-5. [DOI] [PubMed] [Google Scholar]
- Gadow KD. DeVincent CJ. Pomeroy J. ADHD symptom subtypes in children with pervasive developmental disorder. J Autism Dev Disord. 2006;36:271–283. doi: 10.1007/s10803-005-0060-3. [DOI] [PubMed] [Google Scholar]
- Gadow KD. DeVincent CJ. Pomeroy J. Azizian A. Psychiatric symptoms in preschool children with PDD and clinic and comparison samples. J Autism Dev Disord. 2004;34:379–393. doi: 10.1023/b:jadd.0000037415.21458.93. [DOI] [PubMed] [Google Scholar]
- Guerts HM. Grasman RPPP. Verte S. Oosterlaan J. Roevers H. van Kammen S. Sergeant JA. Intra-individual variability in ADHD, autism spectrum disorders and Tourette's syndrome. Neuropsychologia. 2008;46:3030–3041. doi: 10.1016/j.neuropsychologia.2008.06.013. [DOI] [PubMed] [Google Scholar]
- Guttmann–Steinmetz S. Gadow KD. DeVincent CJ. Oppositional defiant and conduct disorder behaviors in boys with autism spectrum disorder with and without attention deficit hyperactivity disorder versus several comparison samples. J Autism Dev Disord. 2009;9:976–985. doi: 10.1007/s10803-009-0706-7. [DOI] [PubMed] [Google Scholar]
- Hartman CA. Rhee SH. Willcutt EG. Pennington BF. Modeling rater disagreement for ADHD: Are parents or teachers biased? J Abnorm Child Psychol. 2007;35:536–542. doi: 10.1007/s10802-007-9110-y. [DOI] [PubMed] [Google Scholar]
- Kanne SM. Abbacchi AM. Constantino JN. Multi-informant ratings of psychiatric symptom severity in children with autism spectrum disorders: The importance of environmental context. J Autism Dev Disord. 2009;39:856–864. doi: 10.1007/s10803-009-0694-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecavalier L. Behavioral and emotional problems in young people with pervasive developmental disorders: Relative prevalence, effects of subject characteristics, and empirical classification. J Autism Dev Disord. 2006;36:1101–1114. doi: 10.1007/s10803-006-0147-5. [DOI] [PubMed] [Google Scholar]
- Lecavalier L. Gadow KD. DeVincent CJ. Edwards MC. Validation of DSM-IV model of psychiatric syndromes in children with autism spectrum disorders. J Autism Dev Disord. 2009;3:278–289. doi: 10.1007/s10803-008-0622-2. [DOI] [PubMed] [Google Scholar]
- Lecavalier L. Leone S. Wiltz J. The impact of behavior problems on caregiver stress in young people with autism spectrum disorders. J Intellect Disabil Res. 2006;50:172–183. doi: 10.1111/j.1365-2788.2005.00732.x. [DOI] [PubMed] [Google Scholar]
- Lee DO. Ousley OY. ADHD symptoms in a clinic sample of children and adolescents with pervasive developmental disorders. J Child Adolesc Psychopharmacol. 2006;16:737–746. doi: 10.1089/cap.2006.16.737. [DOI] [PubMed] [Google Scholar]
- Leyfer OT. Folstein SE. Bacalman S. Davis NO. Dinh E. Morgan J. Tager-Flusberg H. Lainhart JE. Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. J Autism Dev Disord. 2006;36:849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Lord C. Rutter M. DiLavore PC. Risi S. Autism Diagnostic Observation Schedule. Los Angeles: Western Psychological Services; 2001. [Google Scholar]
- Loveland KA. Tunali–Kotoski B. The school-aged child with an autistic spectrum disorder. In: Volkmar F., editor; Klin A., editor; Paul R., editor. Handbook of Autism and Pervasive Developmental Disorders. 3rd. New York: Wiley; 2005. pp. 247–287. [Google Scholar]
- Mitsis EM. McKay KE. Schultz KP. Newcorn JH. Halperin JM. Parent–teacher concordance for DSM-IV attention-deficit/hyperactivity disorder in a clinic-referred sample. J Am Acad Child Adolesc Psychiatry. 2000;39:308–313. doi: 10.1097/00004583-200003000-00012. [DOI] [PubMed] [Google Scholar]
- Pearson DA. Loveland KA. Lachar D. Lane DM. Reddoch SL. Mansour R. Cleveland SL. A comparison of behavioral and emotional functioning in children and adolescents with autistic disorder and PDD-NOS. Child Neuropsychol. 2006;12:321–333. doi: 10.1080/09297040600646847. [DOI] [PubMed] [Google Scholar]
- Pearson DA. Norton AM. Farwell EC. ADHD in mental retardation: Nature, treatment of attention deficits. In: Enns J.T., editor; Burack J., editor. Attention, Development, and Psychopathology. New York: Guilford; 1997. pp. 205–229. [Google Scholar]
- Reiersen AM. Constantino JN. Volk HE. Todd RD. Autistic traits in a population-based ADHD twin sample. J Child Psychol Psychiatry. 2007;48:464–472. doi: 10.1111/j.1469-7610.2006.01720.x. [DOI] [PubMed] [Google Scholar]
- Reiersen AM. Neurman RJ. Reich W. Constantino JN. Volk HE. Todd RD. Intersection of autism, ADHD: Evidence for a distinct syndrome influenced by genes, by gene-environment interactions. In: Hudziak J.J., editor; Arlington VA, editor. Developmental Psychopathology and Wellness: Genetic and Environmental Influences. American Psychiatric Publishing; 2008. pp. 191–207. [Google Scholar]
- Roid GH. Stanford–Binet Intelligence Scale. 5th. Itasca, IL: Riverside; 2003. [Google Scholar]
- Rowland AS. Skipper B. Rabiner DL. Umbach DM. Stallone L. Campbell RA. Hough RL. Naftel AJ. Sandler DP. The shifting subtypes of ADHD: Classification depends on how symptom reports are combined. J Abnorm Child Psychol. 2008;36:731–743. doi: 10.1007/s10802-007-9203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. Le Couteur A. Lord C. Autism Diagnostic Interview–Revised. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- Simonoff E. Pickles A. Charman T. Chandler S. Loucas T. Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2009;47:921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Sinzig J. Bruning N. Morsch D. Lehmkuhl G. Attention profiles in autistic children with and without comorbid hyperactivity and attention problems. Acta Neuropsychiatr. 2008;20:207–215. doi: 10.1111/j.1601-5215.2008.00292.x. [DOI] [PubMed] [Google Scholar]
- Stanger C. Lewis M. Agreement among parents, teachers, and children on internalizing and externalizing behavior problems. J Clin Child Adolesc Psychol. 1993;22:107–116. [Google Scholar]
- Sullivan JR. Riccio CA. Diagnostic group differences in parent and teacher ratings on the BRIEF and Conners' Scales. J Atten Disord. 2007;11:398–406. doi: 10.1177/1087054707299399. [DOI] [PubMed] [Google Scholar]
- Szatmari P. Archer L. Fisman S. Streiner DL. Parent and teacher agreement in the assessment of pervasive developmental disorders. J Autism Dev Disord. 1994;24:703–717. doi: 10.1007/BF02172281. [DOI] [PubMed] [Google Scholar]
- Tassé MJ. Lecavalier L. Comparing parent and teacher ratings of social competence and problem behaviors. Am J Ment Retard. 2000;10:252–259. doi: 10.1352/0895-8017(2000)105<0252:CPATRO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]