Abstract
Objective
The identification of patients most likely to benefit from care management programs case finding – is a crucial determinant of their effectiveness regarding improved health outcomes and reduced costs. Until now, research has mainly focused on claims data-based case finding. This study aimed to explore how primary care physicians (PCPs) select patients for practice-based care management and how risk prediction may complement their case finding.
Study design
Qualitative study
Methods
We performed 12 semi-structured interviews with PCPs from 10 small- to middle-sized primary care practices in Germany. The interviews focused on their criteria for selecting patients as potential participants of an on-site care management program and how PCPs evaluate claims data-based risk prediction as a case finding tool. All interviews were transcribed verbatim. We performed qualitative content analysis using the ATLAS.ti software.
Results
Three major categories emerged from the physicians interviewed: 1) the physicians’ interpretation of the program’s eligibility criteria, 2) physician-related criteria and 3) patient-related criteria. The physician-related criteria included “sympathy/aversion” and “knowing the patient”. Patient-related criteria concerned care sensitivity in terms of “willingness to participate”, “ability to participate” (e.g. sufficient language skills, cognitive status) and “manageable care needs”. PCPs believed that their case finding can be supported by additional information from claims-data based risk prediction.
Conclusions
Case finding for care management programs in primary care may benefit from a structured approach combining clinical judgement by PCPs and claims-data based risk modelling. However, further research is needed to identify the optimal case finding strategy for practice-based care management.
Keywords: Care management, case management, primary health care, case finding, care sensitivity
Introduction
Since decades, numerous care management (CM) programs have evolved in the US and elsewhere aimed at improving quality of care and/or reducing healthcare costs. Despite these CM programs’ diversity in terms of intervention targets and designs, the identification of patients most likely to benefit commonly called case finding – is essential for both their effectiveness and cost-efficiency1, 2. Therefore, particular attention has been drawn on the development and evaluation of practical tools to screen patient populations for potentially eligible participants3. Because a relatively small percentage of the population generates a disproportionate share of healthcare needs and healthcare spending,4, 5 these tools mainly focus on the identification of current or future high cost individuals.
Screening questionnaires like “Probability of Repeat Admissions” (Pra and Pra Plus)6 or “Identification of Seniors at Risk” (ISAR)7 have been empirically tested as case finding tools and have been proved to identify high risk individuals with manageable health needs. However, their use is limited by survey response rates, potential bias arising from self-report and respondent burden.
Since the 1980s, several “predictive models” have been developed to predict future health care utilization and costs8. These models are based on data about diagnostic information, prior health care utilization and costs, which can be obtained from health insurance claims data. Predictive modelling (PM) can be used to identify individuals at high risk of future health care utilization as potential participants of CM programs9,10. However, concerns have risen about which identified potential participants may actually participate in and benefit from these programs. A significant proportion of high risk patients could not be enrolled in CM interventions due to being unable or unwilling to participate10, 11.
Apart from screening questionnaires and PM, physician referral is another case finding approach. Compared to PMs primary care physicians (PCPs) select patients at lower risk of future health care utilization but with higher probability of actually participating in CM programs11. Combining both approaches can help to identify patients at high risk of future health care utilization who are willing and able to participate in CM programs. Until now, there is little evidence about the criteria PCPs use to identify potential CM participants. Eligibility criteria for referral may differ between vendor-supported and on-site primary care practice-based CM programs12. Most recently, the concept of Accountable Care Organizations (ACOs) has evolved in order to accelerate Medicare’s three-part-aim of better care, better health and slower growth in costs13. An ACO will assume responsibility for the care of a defined population of Medicare beneficiaries and may share Medicare savings if it succeeds with the three-part-aim. Primary care group practices could act as medical homes within an ACO and may adopt on-site CM for patients at high risk for future health care utilization as a key strategy to achieve the three-part-aim. Therefore, this study aimed to explore how PCPs select patients for on-site CM programs, how they experience PM-based case finding, and how it may be beneficial to complement risk-based modelling with physician input.
Methods
This qualitative study was part of a set of exploratory studies undertaken to inform the development of a primary care-based CM intervention in Germany14. The planned intervention comprises comprehensive needs assessments, self-management support and regular telephone-based follow up by specially trained health care assistants who work on-site together with the PCPs.
A commercial PM of the likelihood of hospitalization within the next 12 months (LOH) was used (CSSG 0.6, Verisk Health, Munich Germany) to identify high risk beneficiaries of the German General Regional Health Fund (AOK) suffering from any of the following inclusion criteria, which were a diagnosis of any of four index conditions: type 2 diabetes mellitus, chronic obstructive pulmonary disease, chronic heart failure or late-life depression (aged 60 years and above). The following exclusion criteria were applied: minors (age less than 18 years), dementia, palliative care or permanent nursing home residency, active cancer disease, and dialysis. The PM based on inpatient and ambulatory diagnostic codes, age, gender, medication and population density markers. Blinded to the results of PM-based case finding, PCPs were asked to screen a list of all their AOK beneficiaries in order to select up to 30 patients likely to benefit from the planned CM intervention. PCPs and PM used identical diagnostic codes (International Classification of Diseases - ICD10GM) for inclusion and exclusion conditions to select patients (coded at least once in the preceding year). Details on the planned intervention were given to PCPs but they received no specified selection criteria beside the abovementioned inclusion and exclusion criteria.
After submitting their list of selected patients, PCPs received the results of the PM-based case finding algorithm (selecting all eligible beneficiaries with LOH scores above the 90th percentile). Details of the study design are described elsewhere14. The study protocol was approved by the institutional review board of the University Hospital Heidelberg, Germany. We report our results in line with recommended standards for publishing qualitative research15.
Study participants
We invited all 14 PCPs from 10 small- to middle-sized primary care clinics who were involved in the case finding study11 by telephone to take part in a semi-structured interview. Two PCPs declined participation due to time constraints. Prior to beginning the interviews, all participants gave written informed consent into audio-recording, transcription, analysis, and depersonalized publication of the results. Socio-demographic and practice characteristics of participating PCPs and clinics are displayed in Table 1.
Table 1.
Socio demographic and practice characteristics of primary care physician and clinics
| Participating primary care physicians (n=12) | |
|
| |
| Age, mean y (range) | 54 (41–67) |
|
| |
| Female, n (%) | 3 (25) |
|
| |
| Working experience, mean y (range) | 18 (3–31) |
|
| |
| Medical specialty, n (%) | |
| Family physician | 6 (50) |
| General internist | 6 (50) |
|
| |
| Primary care clinics (n=10) | |
|
| |
| Single handed | 5 (50) |
|
| |
| Location, n (%) | |
| Urban | 7 (70) |
| Rural | 3 (30) |
|
| |
| Patient contacts per quarter, n (%) | |
| 500–1,000 | 1 (10) |
| 1,001–1,500 | 3 (30) |
| > 1,500 | 6 (60) |
|
| |
| Number of AOK beneficiaries per clinic, mean (SD) | 603 (313) |
Data collection
The interviews were semi-structured, using an interview guide composed of open-ended questions with additional prompts. A multi-professional team of a family physician (FPK), a nursing scientist (CM) and a health services researcher (TF) developed the interview guide on the basis of the existing concepts of case finding reported above. It was refined based on a pilot interview. All interviews were carried out face-to-face in the primary care clinics by an experienced interviewer (TF) using the abovementioned interview guide which was read verbatim and included additional prompts. Field notices were taken by a research assistant (SG) who was the only person additionally accompanying the interviews. Interviews lasted 67 minutes on average (36–100 minutes), were audio-taped and transcribed verbatim (SG).
The results presented in this manuscript refer to the following two questions:
What were your criteria to select patients for the care management program?
How did you experience case finding based on predictive modelling?
Data analysis
We conducted a computer-assisted content analysis according to Mayring16 using ATLAS.ti software, version 5.2 (ATLAS.ti GmbH, Berlin, Germany). All transcripts were read and open-coded independently by two authors (TF, SG). Codes were created independently by both authors as a first level of abstraction. In an iterative process, content-related codes were further collapsed into sub-categories and major categories. Each sub-category was defined by anchor citations which we report in the result section of this article. During consensus meetings, major categories and subcategories were discussed until mutual agreement was reached. One author (TF) recoded the material according to the final categories.
Results
Three major categories emerged from the physicians interviewed: 1) the physicians’ interpretation of the program’s eligibility criteria, 2) physician-related criteria and 3) patient-related criteria. Regarding their experience with PM-based case finding, two major categories emerged from the interviews: feasibility and usefulness of the software output.
Case finding criteria
Eligibility criteria of the program
Selection criteria due to eligibility for the program fell into three subcategories. Firstly, PCPs named the predefined inclusion and exclusion criteria of the program as case finding criteria (e.g. presence of at least one index condition). Secondly, PCPs’ own assessment of a patient’s risk for future hospitalization (which was not an explicit inclusion criterion) was mentioned by half of the PCPs. Patients’ ability to fill out a questionnaire was named as additional case finding criterion by some of the PCPs as both the case finding study as well as the planned CM program included the requests for participants to fill out paper-based questionnaires.
Physician-related criteria
Two different factors relating to the PCP emerged from the interviews. First, some PCPs reported case finding to be influenced by sympathy or aversion:
“Well, there are patients, I mean with many patients I have an almost personal, warm-hearted relationship, and these patients I would really like to get into the program” [PCP02]
“Some are unlikeable, I am just discouraged to convince them to participate [in the program]” [PCP04]
Knowing patients as being their treating PCP was an important case finding criterion for nearly all of the interviewees.
“As I saw that screening list, I started considering: Who do I know? Whose face is popping up?” [PCP06]
Patient-related criteria
Patient-related case finding criteria fell into three subcategories: patients’ willingness to participate, patients’ ability to participate, and care needs manageable for the planned intervention.
Patients’ willingness to participate in a CM program was given serious consideration by the PCPs. As many PCPs had known their patients for several years, they were able to rate their “likelihood of active participation” in CM.
“[I selected] those who at least are prepared to take their medicine, to collaborate with the practice team, with the physician” [PCP08]
If neither patients nor their care givers were seen to be likely to be engaged in the program, PCPs did not select them from the list.
“Many were excluded because I am pretty sure that both the patient and his care givers did not like these things.” [PCP04]
PCPs rated patients’ ability to participate in CM in terms of sufficient language skills and cognitive status.
“I would mean that it is crucial to include patients, who are able to participate actively, especially in terms of their cognitive status and as we started screening, we selected patients, who are able to participate” [PCP07]
To some PCPs the social situation of patients appeared to be an opportunity to overcome patients’ inability to participate.
“Well, patients’ situation at home is very important! How is he or she cared for at home? Does a caregiver exist? If so, there is somebody who could call help if things start going worse. Then I may be able to help before it is too late.” [PCP09]
In terms of manageable care needs, PCPs preferred to select patients with high clinical complexity and high risk of future deterioration.
“I selected the patients, who are most vulnerable, either because of the severity of the diseases they have or because of having multiple chronic diseases, so multimorbid patients.” [PCP08]
“Their medical history was quite important to me. How likely will the clinical status of the patient deteriorate in the near future? I based my rating mostly on the frequency of deteriorations in the past.” [PCP09]
Some of the PCPs stated that patients in need for highly frequent follow-up should be in the program. Whereas a complete lack of motivation to engage in managing their disease could lead to exclusion of patients, non-compliance was also seen as a potentially manageable care need and relevant inclusion criterion for the program.
“I had in mind that for some patients, improving compliance could be a goal of this structured program.” [PCP10]
Risk prediction
When PCPs were asked to evaluate the list of potentially eligible patients for the CM program based on predicted LOH, feasibility and usefulness of this case finding approach emerged as evaluation criteria from the qualitative analysis.
Feasibility of prediction-based case finding
In general, most PCPs rated the use of a screening list of patients filtered by prediction software as feasible as it helped them to focus on potential participants for the program.
“In general, it is a valuable approach to provide a physician with a list of pre-selected patients among who he can select participants for the program. This is not bad!” [PCP03]
As all information on the list was de-identified due to legal privacy issues, they rated the process of “de-coding” patients’ names as time consuming thus limiting feasibility of this approach. However, de-coding was necessary in the study setting for research privacy purposes but would not be part of case finding in real practice.
Usefulness of prediction-based case finding
Overall, PCPs rated the approach as a useful tool to identify patients likely to benefit from CM. However, they were concerned about time lags between data analysis and patient recruitment. The list contained some deceased patients and patients who were then living in nursing home residencies. Some of the patients suffered from dementia according to the physicians (without any information on that condition in the insurance claims) whereas others lacked any of the index conditions (although claims suggested that they did). Knowing the patient was one of the most important inclusion criteria as mentioned above. However, matching beneficiaries to their treating PCPs based on claims data was not perfect. PCPs therefore claimed patients on the list, who they hardly knew, as mismatching. Finally, patients selected by PM were neither filtered by their willingness nor their ability to participate in CM. This led to the perception by the PCPs that a significant proportion of pre-selected patients were not willing and/or able to participate.
“Well, this long list contained patients, who I could not get into the program because, I mean, due to their character, they were not really able to cooperate; some had serious language problems, others I know to be not interested in. Based on previous contacts, I would say that they are not interested in their diseases and not willing to engage in actively managing their diseases.” [PCP08]
Discussion
This study provides insights into the criteria PCPs used to select patients as potential participants of a primary care practice-based CM program. Furthermore, it is the first study that explores how PCPs evaluate case finding by PM.
Case finding criteria varied between PCPs, a fact that is already known from literature12, 17. However, PCPs in this study consistently described a combined assessment of risk and “care sensitivity”: They aimed to include patients with complex but manageable care needs who would be able and willing to participate either by themselves or supported by an active care giver. This finding is in line with current literature arguing that there is a shift of focus from the identification of high risk patients to the identification of those who are likely to be impacted by the planned intervention18, 19. Summarizing the results of this study, we propose a three-dimensional structure of care sensitivity, i.e. the likelihood of a patient to respond to care (see figure 1).
Figure 1. The three dimensional concept of care sensitivity.
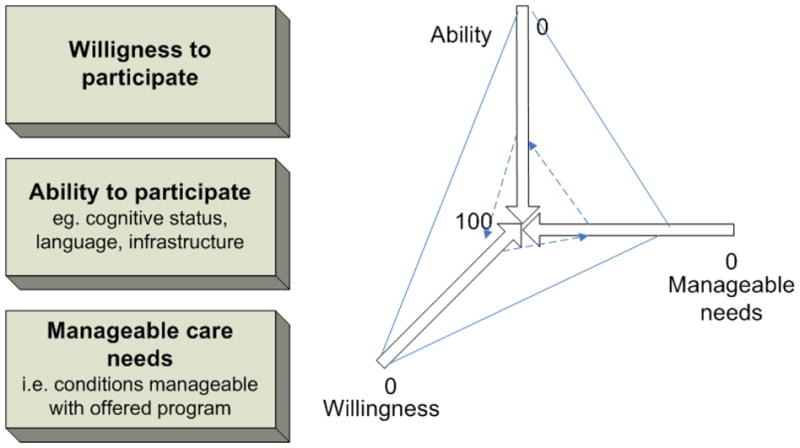
Patients can be characterized by their individual pattern of ability and willingness to participate in a specific program that may or may not manage their needs. If a patient lacks all three dimensions (bold line) care sensitivity has to be rated as low, indicating that he/she is less likely to benefit from the program compared to patients with high ratings on all three care sensitivity dimensions (dotted line).
Depending on different individual patterns of care sensitivity, a patient may be more or less likely to respond to the offered care program. It has to be kept in mind that the shape may be altered on the basis of “manageable care needs” depending on the program offered: e.g. palliative care needs which may be perfectly manageable in a palliative CM program but totally unmanageable in a diabetes CM program. Therefore, referral patterns of PCPs may vary due to the skills and resources of care managers as well as their connection to primary care practices12. This leads to the fundamental question whether case finding should aim to find the patients that fit to a specific CM program or to find the CM program that fits the patient’s needs.
Quantitative data from our related study revealed that PCPs were outperformed by PM in terms of identifying patients at high risk of hospitalization whereas PM was less likely to identify patients supposed to be care sensitive11. Only 5 percent of potential eligible patients were identified by both approaches11. These results were underlined by the PCPs’ experiences with the software output as reported in this study. Conceptually, PM is not focused on patients’ likelihood to be willing or able to participate in CM programs. Additionally, PM faces structural problems: The time lag between claims data input and case selection could result in the identification of patients who had already died, moved away, or been admitted to nursing home residency. These problems have previously been reported from similar software models20 indicating a need to further develop filter mechanisms that may help to increase the validity of the software output and decrease time delays. Despite conceptual and structural limitations of prediction based-case finding, all of the PCPs appreciated the list of pre-selected patients. However, further assessment by PCPs may help to identify patients most likely to benefit by combining predicted risk and care senstitivity11, 20.
PCPs in our study reported “sympathy or aversion” to be a relevant issue for case finding. This finding raises concerns about the equity of access to intensified primary care and should further be explored in quantitative studies (e.g. surveys). If sympathy and aversion, i.e. the doctor-patient relationship, plays a significant role in PCP-based case finding, PM may help to overcome access barriers if PCPs were asked to include pre-selected patients with no regard to their attitude towards these patients. From the perspective of ACOs the results of our study may support the idea of identifying primary care patients at high risk by combining data-driven models or tools and clinical judgment by PCPs. Acceptance for these programs may be higher among both patients and PCPs if case finding involves judgment by PCPs.
A strength of this study is that it is the first to explore how PCPs evaluate case finding based on PM which is an emerging approach in population health management9, 18. Furthermore, this study gives detailed insight into the underlying criteria PCPs use in case finding, which shed further light on our prior quantitative findings11. However, our results focused on a specific primary care practice-based CM program offered in the German health care system. PCPs from other countries, working in different health care systems and CM programs might have other or additional case finding criteria. In addition to that, our findings should be interpreted as a first step to explore PCP-based case finding. The results demand to be validated in quantitative studies. Therefore, further international research is needed to reveal potential universal as well as program- and system-specific case finding criteria. Finally, our study is limited by the fact that we did not explore PCPs’ experiences with case finding by health risk assessment tools, which allow risk modelling-based case finding without relying on insurance claims data.
In summary, German PCPs selected patients for an on-site care management program after assessing their care sensitivity, i.e. the willingness and ability to participate in a program that potentially manages their needs. PCPs experienced case finding based on PM to be supportive although the output had to be filtered for validity and care sensitivity. Further research may help us to understand the complex relationship between risk of future hospitalization and care sensitivity in order to improve our ability to identify and target patients most likely to participate in and benefit from CM programs.
Acknowledgments
Support: The study was funded by the General Regional Health Fund (AOK) Baden-Wurttemberg. The funding agency had no role in the design of the study, analysis of data, or preparation of the manuscript. Dr. Boyd is supported by the Paul Beeson Career Development Award Program (NIA K23 AG032910, AFAR, The John A. Hartford Foundation, The Atlantic Philanthropies, The Starr Foundation and an anonymous donor).
We thank all interviewees for their contribution to this work.
Footnotes
Conflict of interest statement
All authors declare no potential conflicts of interest.
References
- 1.Bodenheimer T, Berry-Millet R. Care management of patients with complex healthcare needs. 19. Princeton, NJ: The Robert Wood Johnson Foundation; 2009. research synthesis report. [Google Scholar]
- 2.Goetzel RZ, Ozminkowski RJ, Villagra VG, Duffy J. Return on investment in disease management: a review. Healthcare Financ Rev. 2005;26:1–19. [PMC free article] [PubMed] [Google Scholar]
- 3.Bernstein RH. New arrows in the quiver for targeting care management: high-risk versus high-opportunity case identification. J Ambul Care Manage. 2007;30(1):39–51. doi: 10.1097/00004479-200701000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 5.Busse R. Competition in healthcare a health systems’ perspective [German] Z Evid Qual Gesundh wesen. 2009;109:608–620. doi: 10.1016/j.zefq.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 6.Boult C, Pualwan TF, Fox PD, Pacala JT. Identification and assessment of high-risk seniors. Am J Manag Care. 1998;4:1137–1146. [PubMed] [Google Scholar]
- 7.Dendukuri N, McCusker J, Belzile E. The identification of seniors at risk screening tool: further evidence of concurrent and predictive validity. J Am Geriatr Soc. 2004;52:290–296. doi: 10.1111/j.1532-5415.2004.52073.x. [DOI] [PubMed] [Google Scholar]
- 8.Weir S, Aweh G, Clark RE. Case selection for a Medicaid chronic care management program. Health Care Financ Rev. 2008;30:61–74. [PMC free article] [PubMed] [Google Scholar]
- 9.Forrest CB, Lemke KW, Bodycombe DP, Weiner JP. Medication, diagnostic, and cost information as predictors of high-risk patients in need of care management. Am J Manag Care. 2009;15:41–48. [PubMed] [Google Scholar]
- 10.Sylvia ML, Shadmi E, Hsiao CJ, Boyd CM, Schuster AB, Boult C. Clinical features of high-risk older persons identified by predictive modeling. Dis Manag. 2006;9:56–62. doi: 10.1089/dis.2006.9.56. [DOI] [PubMed] [Google Scholar]
- 11.Freund T, Mahler C, Erler A, et al. Identification of patients likely to benefit from care management programs. Am J Manag Care. 2011;17(5):345–352. [PubMed] [Google Scholar]
- 12.Wilcox AB, Dorr DA, Burns L, Jones S, Poll J, Bunker C. Physician perspectives of nurse care management located in primary care clinics. J Case Man. 2007;8(2):58–63. doi: 10.1891/152109807780845573. [DOI] [PubMed] [Google Scholar]
- 13.Berwick DM. Launching accountable care organizations--the proposed rule for the Medicare Shared Savings Program. N Engl J Med. 2011;21;364(16):e32. doi: 10.1056/NEJMp1103602. [DOI] [PubMed] [Google Scholar]
- 14.Freund T, Wensing M, Mahler C, et al. Development of a primary care-based complex care management intervention for chronically ill patients at high risk for hospitalization: a study protocol. Implement Sci. 2010;5:70. doi: 10.1186/1748-5908-5-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 16.Mayring P. Content Analysis. UTB; Berlin: 2007. Qualitative Inhaltsanalyse. [Google Scholar]
- 17.Nutting PA, Gallagher K, Riley K, et al. Care management for depression in primary care practice: findings from the RESPECT-depression trial. Ann Fam Med. 2008;6:30–37. doi: 10.1370/afm.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meek JA. Predictive modelling and proactive care management part 1. Lipp Cas Man. 2003;8:170–174. doi: 10.1097/00129234-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Lewis GH. “Impactability models”: Identifying the subgroup of high-risk patients most amenable to hospital-avoidance programs. Milbank Q. 2010;88(2):240–255. doi: 10.1111/j.1468-0009.2010.00597.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall S, Kulendran M, Sadek AR, Green S, de Lusignan S. Variability in selecting patients to manage in the community: a service evaluation of community matron’s case-finding strategies. Fam Pract. 2011;0:1–8. doi: 10.1093/fampra/cmq095. [DOI] [PubMed] [Google Scholar]


