Abstract
Objective
Rheumatoid arthritis often results in deformities at the metacarpophalangeal (MCP) joint. Patients with severe deformities can be treated by silicone metacarpophalangeal joint arthroplasty (SMPA). The objective of the study is to prospectively compare long-term outcomes for a SMPA surgical and a non-surgical cohort of rheumatoid arthritis patients.
Methods
A total of 67 surgical and 95 nonsurgical patients with severe subluxation and/or ulnar drift of the fingers at the MCP joints were recruited from 2004-2008 in this multi-center prospective cohort study. Patients could elect to undergo SMPA or not. Outcomes included the Michigan Hand Outcomes Questionnaire (MHQ), Arthritis Impact Measurement Scales (AIMS2), grip/pinch strength, Jebson-Taylor test and ulnar deviation, extensor lag and arc of motion measurements at the MCP joints.
Results
There was no significant difference in the mean age, race, education, and income at baseline between the two groups. Surgical subjects had worse MHQ function and functional measurements at baseline. At 3 years, the mean overall MHQ score and the MHQ function, activities of daily living, aesthetics and satisfaction scores showed significant improvement in the surgical group compared to the non-surgical group. Ulnar deviation, extensor lag and arc of motion in the MCP and PIP joints also improved significantly in the surgical group. No improvement was seen in the mean AIMS2 scores and grip/pinch strength. Complications were minimal with a fracture rate of 9.5%.
Conclusion
RA patients with poor baseline functioning showed long term improvement in hand function and appearance following treatment with SMPA compared to non-surgical controls.
Keywords: Rheumatoid arthritis, Silicone Metacarpophalangeal Joint Arthroplasty
Inflammation that leads to progressive damage to joints is a hallmark of rheumatoid arthritis (RA). The joints most often affected are the metacarpophalangeal joints (MCPJ) causing dislocation of the MCPJs and ulnar deviation of the fingers. This deformity often results in disability because of the inability to extend the fingers to grasp objects. Treatment for RA almost always requires medications to halt or slow the progression of joint damage. Surgical management for RA, which includes joint arthroplasty and arthrodesis, is recommended as a last resort.
Silicone implants have been used for many years to replace destroyed MCPJs in the rheumatoid hand. Historically, much of the evidence regarding the effectiveness of silicone metacarpophalangeal arthroplasty (SMPA) has relied on low (level 3-4) evidence from retrospective cohorts or case series.1-13 Prospective studies offered higher evidence (level 2) but these studies were hampered by small study sample sizes (N ranged from 12-21 patients).14-17 More recently, high level of evidence (level 1) has come from two randomized controlled trials (RCTs) that compared SMPA to other implants.18,19 The sample sizes for these RCTs were small, ranging from 33 to 52 patients, whereas the retrospective studies ranged from 28 to 264 patients. Follow-up time varied by study type with retrospective studies having longer follow-up (average range 2 and 14 years) whereas prospective studies (average range 1-3 years) and RCT’s (range 1-2 years) had shorter follow-up. None of the studies used a control group consisting of patients who were managed medically without SMPA. The majority of studies focused on physical measurements such as finger arc of motion and degree of ulnar drift to assess outcomes. Overall, the results from these studies report that SMPA improves function of the rheumatoid hand.12 The degree of ulnar drift, extensor lag and the arc of motion in finger joints show improvement after SMPA but grip and pinch strength do not.1,2,8,10,16 Many of studies evaluated health related quality of life (HRQL) using subjective assessments by surgeons or unvalidated questionnaires. Based on these measures, favorable outcomes were reported in hand function, activities of daily living (ADL), pain, aesthetics, and patient satisfaction.1,2,4-10,13,16
The disparity between the results from functional measurements such as grip and pinch strength and patient reported function fuels the ongoing debate regarding the true effectiveness of SMPA. For example, previous studies have found that rheumatologists and hand surgeons disagree on the effectiveness of hand surgery for RA patients.20,21 In a national survey of these two specialties, 34% of rheumatologists compared to 83% of hand surgeons believe SMPA improves hand function for RA patients. This disagreement in treatment options may partially explain the large variations in the surgical management of the rheumatoid hand in the US.22,23 It has been suggested that patients choose surgery to improve the appearance of the hands rather than improve function or lessen pain. Moreover, satisfaction with surgery has been found to be closely correlated with hand appearance.24,25 Finally, although these implants have been used for over 4 decades, the true complication rate of these implants is still unknown.
To better understand outcomes following SMPA, we conducted a multicenter prospective cohort study comparing RA patients with severe MCPJ deformities who elect to undergo SMPA versus those who do not undergo SMPA. The inclusion of the non-surgical control group was one of several unique aspects of this study. Outcome measures included both validated HRQL questionnaires and standardized hand function tests. Lastly, this study achieved the unusual collaboration of rheumatologists and hand surgeons. The specific aim of the study is to assess the effectiveness of SMPA in RA patients with MCPJ deformity in order to provide high level evidence for or against the procedure and to determine the long-term benefit of SMPA. This paper presents the results from the 3 year follow-up after surgery or enrollment.
Patients and Methods
The institutional review boards (IRB) of all three study sites approved the protocol for this study. All subjects enrolled in the study were informed about the study requirements and signed consent forms. A detailed description of the study methods has been previously published.26
Study Sample
Rheumatoid arthritis patients were referred by their rheumatologists to hand surgeons at one of the three study sites: University of Michigan (Ann Arbor, MI), Curtis National Hand Center (Baltimore, MD) and Pulvertaft Hand Centre (Derby, England). All of the study sites are comprehensive centers dedicated to the treatment of upper extremity disorders and have a large rheumatology program, which enhanced patient accrual for this study. In addition, the heterogeneous racial composition from the three study sites ensures that minority groups are represented in this study. Inclusion criteria were (1) diagnosis with RA by a rheumatologist; (2) 18 years of age or older; (3) ability to complete questionnaires in English; and (4) severe deformity at the MCPJ as determined by the sum of the average ulnar deviation and average extensor lag of the four fingers. The sum of these two measurements had to be ≥ 50°. This cutoff was determined by an expert panel to be the minimum level of deformity that would be needed before surgery would be considered. Exclusion criteria were (1) severe medical conditions precluding surgery (e.g., severe coronary artery disease, uncontrolled diabetes mellitus, chronic renal failure), (2) concomitant extensor tendon ruptures and MCP joint disease, (3) Swan-neck or Boutonniere’s deformities that require surgical correction, (4) patients who have undergone previous MCP joint replacement on the study hand, and (5) patients who have begun taking Disease Modifying Anti-Rheumatic Drugs (DMARDs) in the past 3 months.
Study design
This study applied a prospective cohort design. Patients were not randomized due to strong patient preferences regarding their choice for having surgery. A pilot study at 2 of the 3 sites was completed before the start of the study to determine if patients would agree to be randomized. Most patients would not consent to randomization because they have an inherent preference whether to have or not to have surgery. Therefore, patients chose whether or not to have surgery. If both hands were affected, patients chose which hand to have surgery. Surgical subjects had SMPA performed on all four fingers. The non-surgical group chose which hand was the study hand. Subjects in the non-surgical group could cross over to the surgical group after 1 year of enrollment in the study. Additionally, surgical subjects could elect to have surgery on their other affected hand 1 year after having surgery on the first hand. In addition to the time of enrollment, patients were assessed at 6 months, 1 year, 2 years and 3 years post-surgery or enrollment. All outcomes were assessed at each follow-up visit. Patients were contacted by phone and/or mail for follow-up visits and were considered loss to follow-up if there was no response after numerous attempts.
Outcome Measures
Outcomes were assessed at enrollment and 6 months, 1, 2 and 3 years after the surgery date for the surgical cohort or the enrollment date for the non-surgical cohort. All functional measurements were performed on both hands but the results presented are for the surgical or study hand. A certified hand therapist conducted the functional assessments that included: grip strength, lateral pinch, two-point pinch and three-point pinch, and range of motion measurements for all the joints in each finger and for the wrist. The motion measurements included the degree of ulnar drift (angle of the fingers at the MCPJ), extensor lag (degree to which fingers lag when fully extended), and arc of motion (difference in degrees at joints when fingers are extended and flexed). The research coordinator administered the Jebson-Taylor test which simulates activities of daily living (ADL).27 Subjects performed various everyday type activities including (1) turning over 3 by 5 inch cards, (2) picking up small objects and placing them in a container, (3) stacking checkers, (4) simulated eating, (5) moving large, empty cans, and (6) moving large, weighted cans. The writing portion of the test was excluded and the time to complete the tasks is measured in seconds. Two questionnaires were used: the Michigan Hand Outcomes Questionnaire28,29 (MHQ) and the Arthritis Impact Measurement Scales 230 (AIMS2). The MHQ is hand specific questionnaire whereas the AIMS2 measures overall health status in RA patients. The MHQ contains six domains (function, ADL, work, pain, aesthetics, and satisfaction) and scores range from 0 to 100 with higher scores indicating better performance, with the exception of the pain scale. For the pain scale, a higher score indicates more pain. The satisfaction domain asks about satisfaction with the overall performance of the hand and wrist. The MHQ queries subjects about both hands but only the results for the surgical or study hand were analyzed. The AIMS2 contains 4 domains (physical, affect, symptom, social interaction) and domain scores range from 1 to 10 with lower scores indicating better health status. Both questionnaires are validated for rheumatoid arthritis.
Complications
Subjects were assessed for complications such as infections and deformities/fractures of the implants at follow-up visits. The integrity of the MCPJ implants in surgery subjects was assessed using radiographs at 6 months and 3 years after surgery. Each implant was categorized using the protocol by Bass et al.31 as intact, definitely fractured, or severely deformed. Radiographs were reviewed by two of the hand surgeons who were blinded to the study subjects and the subjects’ study site. When the surgeons disagreed on their assessments, they worked together to achieve consensus. When consensus could not be reached, a third hand surgeon made the decision regarding fractures and/or deformities. Deaths were reported to the institutional review boards for each site.
Data analysis
The distribution of demographic variables and other baseline variables were compared between the surgical and non-surgical group using the two-sample t-tests for continuous variables, and chi-square tests for categorical variables. Because non-surgical group subjects were allowed to cross over their treatment groups, all outcome data were censored beyond the time the study hand of the non-surgical group patient was treated by SMPA. Baseline data including demographic and baseline values of the outcome variables were assessed for missing data. Baseline characteristics were also compared between those who were lost to follow-up versus those who were not.
For all outcome measures of interest, means and 95% confidence intervals (CI) at each follow-up time were calculated by the study group. Unadjusted mean changes from baseline in various outcome measures between the surgical versus non-surgical group at three year follow-up time were calculated. Random-effects regression models were used to estimate and compare the 3 year outcomes between the two groups. For each outcome variable, the model used the baseline and three year outcome values as the dependent variable and an indicator for the surgical group, an indicator for 3 year time, and an interaction term of indicators of 3 year time by surgical group. Because of the baseline differences between the two groups, the models were also adjusted for the baseline values of the outcome variable, age, baseline severity (dichotomized as severe or not based on degree of deformity), education (high school and lower versus higher), income (>50K vs. lower), gender and study site. All unadjusted and adjusted mean differences were calculated so the positive values corresponded to greater improvement in the surgical group relative to non-surgical group. We also obtained the propensity stratified estimates of the between group differences in three year outcomes.32 Propensities were estimated using a logistic regression model with receipt of SMPA as the dependent variable, and with all baseline covariates and baseline values of the outcome variables as predictors. For baseline variables with missing values such as education and income, the variable was encoded for an extra level corresponding to those patients who are missing the covariates, and squared terms for continuous variables and appropriate interactions terms were also included.
We used multiple imputation method to account for missing covariates as well as missing outcomes.33 Five imputed data sets were created using all available baseline covariates we suspected or found to be relevant to missing data mechanism, including rheumatoid medication types used (DMARDs, biologics, or anti-inflammatories), whether the study hand was a dominant hand or not, number of comorbid medical conditions as well as demographic variables. The imputations also used all longitudinally measured outcome data and accounted for the correlation between a patient’s longitudinally measured outcome data. Any imputed values outside of plausible range were truncated with the proper values. For the non-surgical group patients who later received SMPA on their study hand, their outcome data after their receipt of SMPA were imputed based on all data prior to the time of receipt of their SMPA. Across the imputed datasets, covariate adjusted between-group mean differences were estimated using the random-effects model, and the estimates were combined using Rubin’s combining rules.34 All analyses including multiple imputations were performed using Stata 11.2 (StataCorp LP, College Station, TX)
Results
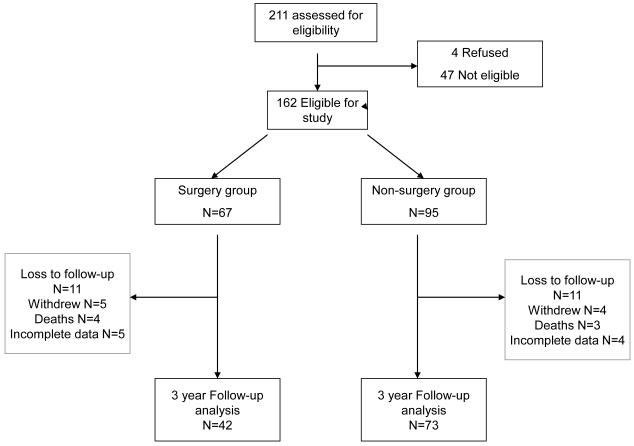
A total of 162 subjects (67 surgical and 95 nonsurgical) were enrolled in the study. Two control subjects chose to have surgery on the study hand after 1 year, and 10 surgical subjects elected to have surgery on their other affected hand 1 year after having the initial SMPA on the study hand. The 1 year results have been presented previously.26 Due to withdrawals (n= 9), deaths (n=7), losses to follow-up (n=22) and missing data (n=9), three year data were available in 42 surgical (58%) and 73 (78%) nonsurgical subjects (including 2 subjects who had surgery on their study hand prior to their three year follow-up time) (Figure 1).
Figure 1.
Study flow chart
Baseline demographic information by surgical status is shown in Table 1. Baseline data were missing for 5 percent or less patients except for income (8% had missing income). The two study groups were not significantly different at baseline in terms of age, race, education and income. The surgical group had a lower percentage of men compared to the nonsurgical group. Those who were missing versus not missing 3 year outcome data were not different with respect to various demographic variables, but the missingness depended on the baseline values of the outcomes and the magnitude of the change in the outcome values. Specifically, in both non-surgical and surgical group, those who were missing the three year MHQ data tended to have more severe baseline symptoms than those not missing the three year follow-up data (p = 0.02 based on baseline MHQ). In addition, in surgical group, greater improvement in MHQ values from baseline to two years were associated with greater likelihood of missing the 3 year MHQ outcome data (p = 0.03), and thus the completers only analysis (e.g., analysis of crude change) was expected to give a smaller effect associated with surgical group.
Table 1. Comparison of Demographic Values for Surgical vs. Non-Surgical Subjects.
| Demographic variables | SMPA (N=67) |
Non-SMPA (N=95) |
P- value |
|---|---|---|---|
| Age, mean (SD) | 60 (8) | 62 (11 ) | 0.24 |
| Male, No. (%) | 12 (18) | 32 (35) | 0.03 |
| Race, White, No. (%)a | 58 (94) | 79 (86) | 0.14 |
| Education, ≤ High School Degree, No. (%)a | 35 (56) | 38 (41) | 0.07 |
| Income, ≤ $50,000, No. (%)a | 47 (77) | 60 (68) | 0.24 |
Eight (5%) participants are missing race and education data and 13 (8%) are missing income data.
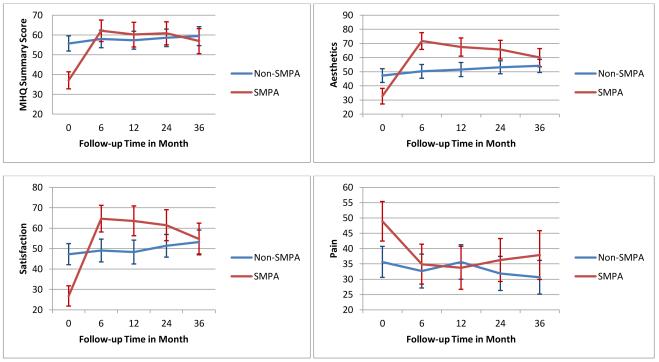
Surgical subjects were significantly different from nonsurgical subjects for the majority of baseline measurements (Table 2). In particular, surgical subjects had worse hand functioning as measured with the MHQ; mean overall MHQ score was 37 in the surgical group and 56 in the non-surgery group. Figure 2 plots the mean overall MHQ scores, Aesthetics, Satisfaction and Pain domain scores over time by the study groups. In general, hand outcomes of the surgical patients improved from their initial state to a level similar to the control group by six months, and this improvement was maintained to 3 years. In the Aesthetics and Satisfaction domains, the surgical patients improved to substantially higher levels than those of the non-surgical patients at 6 months, but the domain scores slowly decreased after 1 year. AIMS2 subscales all showed significantly worse health in surgical than nonsurgical patients at baseline, and over the 3 years of follow-up, the surgical group did not show better outcomes than the nonsurgical group.
Table 2. Mean Scores for Surgical (SMPA) vs. Non-Surgical Subjects.
| Preoperative | 2-Year | 3-Year | ||||
|---|---|---|---|---|---|---|
| SMPA | Non- SMPA |
SMPA | Non- SMPA |
SMPA | Non- SMPA |
|
|
| ||||||
| MHQ1 | N = 63 | N = 93 | N = 48 | N = 79 | N = 40 | N = 71 |
|
| ||||||
| Function | 37 (22) | 58 (19)** | 62 (19) | 58 (22) | 59 (19) | 58 (21) |
| ADL | 34 (26) | 59 (24)** | 58 (29) | 61 (25) | 55 (27) | 61 (27) |
| Work | 41 (22) | 59 (23)** | 54 (27) | 61 (26) | 51 (28) | 61 (27) |
| Pain | 49 (26) | 36 (25)* | 36 (25) | 32 (25) | 38 (26) | 31 (24) |
| Aesthetics | 33 (22) | 47 (24)** | 66 (23) | 53 (21) | 60 (21) | 54 (20) |
| Satisfaction | 27 (20) | 47 (25)** | 61 (27) | 51 (25) | 55 (25) | 53 (25) |
| Overall | 37 (17) | 56 (19)** | 61 (21) | 59 (20) | 57 (20) | 59 (21) |
|
| ||||||
| AIMS22 | N = 63 | N = 93 | N = 48 | N = 79 | N = 40 | N = 71 |
|
| ||||||
| Physical | 4.0 (2.4) | 2.5 (1.9)** | 3.3 (2.2) | 2.5 (2.0) | 3.4 (2.3) | 2.6 (2.2) |
| Affect | 4.2 (1.9) | 3.1 (1.8)** | 3.7 (1.8) | 2.9 (1.7) | 3.7 (2.3) | 2.7 (1.6) |
| Symptom | 5.7 (2.8) | 4.3 (2.4)* | 4.6 (2.4) | 3.9 (2.3) | 5.0 (2.3) | 4.0 (2.5) |
| Social interaction | 4.1 (2.0) | 3.6 (1.4)* | 4.1 (2.1) | 3.7 (1.3) | 4.1 (2.1) | 3.5 (1.6) |
|
| ||||||
|
Objective Measurements |
N = 67 | N = 95 | N = 45 | N = 74 | N = 39 | N = 66 |
|
| ||||||
|
Grip Strength (kg) |
5.4 (5.2) | 8.6 (7.4)* | 6.1 (4.4) | 10.6 (7.5) | 6.0 (4.2) | 9.7 (5.9) |
|
Key (lateral) pinch (kg) |
3.5 (2.2) | 4.0 (1.8) | 3.2 (1.9) | 3.7 (1.9) | 3.0 (2.0) | 3.4 (1.8) |
|
2-point (tip) pinch (kg) |
2.5 (1.6) | 3.1 (1.5)* | 2.4 (1.5) | 2.9 (1.5) | 2.2 (1.4) | 2.7 (1.3) |
|
3-jaw (palmar) pinch (kg) |
2.5 (1.5) | 3.2 (1.4)* | 2.5 (1.4) | 3.2 (1.5) | 2.4 (1.5) | 2.7 (1.2) |
|
Jebson-Taylor (s)3 |
55 (27) | 43 (12)** | 43 (11) | 39 (10) | 44 (13) | 40 (12) |
| Ulnar Drift3 | 37 (15) | 35 (15) | 14 (9) | 33 (16) | 14 (11) | 34 (17) |
| Extensor Lag3 | 65 (23) | 47 (18)** | 25 (14) | 48 (23) | 29 (15) | 53 (21) |
|
MCP Arc of Motion |
20 (15) | 37 (18)** | 33 (17) | 33 (20) | 30 (14) | 29 (16) |
|
PIP Arc of Motion |
56 (27) | 70 (22)** | 66 (25) | 67 (22) | 64 (26) | 67 (21) |
Abbreviations: AIMS2, Arthritis Impact Measurement Scales 2, ADL, activities of daily living; SMPA, Silicone Metacarpophalangeal Joint Arthroplasty, MCP, Metacarpophalangeal Joint, PIP, Proximal Interphalangeal Joint.
Cell values are means (SD).
All MHQ domain scores and overall score can range from 0 to 100, and higher scores correspond to better outcomes, except for pain where higher scores correspond to greater pain.
All AIMS2 subscales can range from 0 to 10, and, higher scores correspond to worse outcome.
Higher values correspond to worse outcomes.
P < 0.05
P < 0.001 for between group difference at baseline.
Figure 2.
Means and 95% confidence intervals from baseline to 3 years for select MHQ scores:Surgical vs. non-surgical subjects
The degree of ulnar drift and lateral pinch strength were similar at baseline between the two study groups but grip and tip and palmar pinch strength were worse in surgical patients compared to nonsurgical patients. Standard functional measurements of grip strength, pinch strength, and ulnar drift and extensor lag showed different responses to treatment. For example, grip strength showed some improvement over time in both groups but the surgical group still showed less strength compared to nonsurgical subjects over time. No improvement was seen for all three types of of pinch strength (key, two point, and three point) over the entire time period. The most dramatic results were seen for degree of ulnar drift, extensor lag, and arc of motion where the surgical group showed significant improvement after SMPA, which remained through 3 years, whereas the nonsurgical group showed little change.
At three years, the surgical group showed significant improvement from baseline in MHQ scores, whereas the nonsurgical group showed minimal to no improvement (Table 3). The between group difference at 3 years from baseline was highly significant for the overall MHQ score as well as the function, ADL, aesthetics, and satisfaction domains, all showing greater improvement in hand outcomes in the SMPA group than in the non-surgical group. The between group difference estimated using the imputed data gave similar findings, although only ADL was highly significant. For the propensity stratified estimates, the propensity model had an area under the receiver operating curve of 0.91. The propensities were trimmed for non-overlapping ranges, which led to a much reduced sample size of 88 patients, and of those, only 59 patients provided 3 year MHQ data. Despite the much smaller sample size, the propensity stratified estimate of the between-group difference of the 3 year MHQ overall summary score was 14.8 (p = 0.002). Similarly, the propensity stratified estimates were 17.6 (p = 0.002) for function, 15.7 (p = 0.001) for ADL, 7.1 (p = 0.27) for work, 6.2 (p = 0.37) for pain, 21.1 (p = 0.001) for aesthetics and 21.2 (p = 0.003) for satisfaction domain of the MHQ.
Table 3. Crude and adjusteda changes from baseline to 3 years for MHQ and AIMS2 Scales.
| Crude change | Adjusted Change | Adjusted Differenced With Imputatione |
||||
|---|---|---|---|---|---|---|
| SMPA | Non-SMPA | SMPA | Non-SMPA | |||
|
| ||||||
| MHQb | N = 40 | N = 71 | N = 40 | N = 71 | N = 111 | N = 162 |
|
| ||||||
| Overall | 18 (12, 24) | 2 (−.4, 5) | 19 (15, 22) | 3 (−.1, 5) | 16** (12, 21) | 14 (−1, 30) |
| Function | 21 (13, 28) | −2 (−5, 1) | 21(17, 26) | −1 (−5, 2) | 22** (17, 28) | 18 (0, 36)* |
| ADLf | 17 (12, 23) | 2 (−2, 5) | 18 (14, 22) | 2 (−1, 5) | 16** (11, 21) | 21 (11, 32) ** |
| Work | 8 (1, 14) | 2 (−2, 7) | 8 (3, 13) | 3 (−1, 7) | 6 (−1, 12) | 10 (−12, 33) |
| Pain | 9 (−.8, 18) | 3 (−2, 7) | 10 (4, 15) | 3 (−1, 8) | 6 (−1, 13) | 8 (−14, 30) |
| Aesthetics | 28 (19, 37) | 5 (.6, 9) | 28 (23, 33) | 5 (1, 9) | 23** (16, 29) | 20 (4, 37)* |
| Satisfaction | 28 (19, 36) | 4 (−.5, 9) | 28 (22, 33) | 4 (−.0, 9) | 24** (17, 31) | 19 (4, 33)* |
|
| ||||||
| AIMS2c | N = 40 | N = 71 | N = 40 | N = 71 | N = 111 | N = 162 |
|
| ||||||
| Physical | .1 (−.2, .5) | −.0 (−.3, .2) | .2 (−.1, .5) | −.0 (−.3, .2) | .2 (−.1, .6) | .7 (−1.1, 2.5) |
| Affect | .3 (−.3, .8) | .2 (−.1, .5) | .3 (−.1, .6) | .2 (−.1, .5) | .1 (−.4, .5) | .3 (−1.1, 1.8) |
| Symptom | .7 (.1, 1.3) | .1 (−.4, .5) | .7 (.2, 1.2) | .1 (−.3, .5) | .6 (−.0, 1.2) | .2 (−1.3, 1.8) |
|
Social Interaction |
.1 (−.4, .6) | −.0 (−.3, .3) | .1 (−.3, .4) | −.0 (−.3, .3) | .1 (−.3, .6) | .2 (−1.0, 1.5) |
Cell values are means (95% confidence interval).
Using random effects model with baseline and year 3 outcome values as dependent variable and adjusted for baseline values of the outcome variable, age, gender, baseline severity stage, education level, income level, study site, 3 year indicator, SMPA group indicator and SMPA group by 3 year time interaction.
Positive values reflect improvement; calculated as 3 year minus baseline values for all scales, except pain where it is baseline minus 3 year values.
Changes are calculated as baseline minus 3 year values so that positive values reflect improvement
Between group differences at three years; positive scores reflect better outcomes in SMPA group relative to non-surgical group
Based on five imputations
Activities of daily living
P < 0.05
P < 0.001.
The AIMS2 score changes were minimal with no significant between group differences (Table 3). Objective measures such as grip and pinch strength did not show greater improvement for surgical group compared to nonsurgical group, except for Jebsen-Taylor test (Table 4). For each of ulnar drift, extensor lag, MCP arc of motion and PIP arc of motion, significant improvements were seen in SMPA group, whereas worsening was seen in nonsurgical groups in general, and the adjusted between group differences were significant at three years, using both all available data and multiply imputed data.
Table 4. Crude and adjusteda from baseline to 3 years for objective measures.
| Crude change | Adjusted Change | Adjusted Differenceb |
Adjusted Differenceb With Imputatione |
|||
|---|---|---|---|---|---|---|
| SMPA | Non-SMPA | SMPA | Non-SMPA | |||
|
| ||||||
|
Objective Measures |
N = 39 | N = 66 | N = 39 | N = 66 | N = 105 | N = 162 |
|
| ||||||
|
Grip Strengthc |
.5 (−1.5, 2.5) | 1.5 (.3, 2.6) | .9 (−.4, 2.2) | 1.5 (.6, 2.5) | −.6 (−2.2, 1.0) | .3 (−2.0, 2.6) |
|
Jebsen- Taylord Test |
6.5 (2.0, 11.1) | 2.6 (−.0, 5.1) | 6.7 (3.8, 9.6) | 2.5 (.2, 4.7) | 4.2 (.5, 7.9)* | 9.7 (−32.7, 13.3) |
|
Two Point Pinchc |
−.1 (−0.5, 0.2) | −.2 (−.5, 0.3) | −.2 (−.4, .1) | −.2 (−.5, −.0) | .1 (−.2, .4) | .1 (−.4, .6) |
|
Three Point Pinchc |
−.0 (−.4, 0.4) | −.3 (−.6, −0.1) | −.0 (−.3, .3) | −.3 (−.5, −.1) | .3 (−.0, .7) | .3 (−.2, .8) |
| Key Pinchc | −.2 (−.7, .2) | −.4 (−.8, −.1) | −.2 (−.6, .1) | −.4 (−.7, −.2) | .2 (−.2, .7) | .7 (−.6, 2.0) |
|
Average Ulnar Driftd |
20.6 (16.0, 25.3) | −.9 (−4.5, 2.6) | 21.2 (17.8, 24.6) | −1.1 (−3.8, 1.6) | 22.3 (17.9, 26.6)** | 19.8 (12.0, 27.6)** |
|
Average Extensor Lagd |
30.4 (22.7, 38.1) | −7.9 (−11.5, −4.4) | 31.7 (27.1, 36.2) | −7.7 (−11.2, −4.1) | 39.3 (33.6, 45.1)** | 38.9 (27.5, 50.4)** |
|
MCPf Arc of Motionc |
9.2 (3.1, 15.3) | −9.5 (−13.2, −5.8) | 10.1 (6.2, 14.0) | −9.2 (−12.3, −6.2) | 19.3 (14.4, 24.3)** | 19.0 (12.3, 25.7)** |
|
PIPg Arc of Motionc |
6.9 (1.4, 12.4) | −2.6 (−5.2, 0.0) | 7.5 (4.2, 10.9) | −2.6 (−5.2, 0.1) | 10.1 (5.8, 14.3)** | 10.4 (−4.3, 25.2)** |
Cell values are means (95% confidence interval).
Using random effects model with baseline and year 3 outcome values as dependent variable and adjusted for baseline values of the outcome variable, age, gender, baseline severity stage, education level, income level, study site, 3 year indicator, SMPA group indicator and SMPA group by 3 year time interaction.
Between group differences at three years; positive scores reflect better outcomes in SMPA group relative to non-surgical group
Changes are calculated as 3 year minus baseline values, and positive values reflect improvement
Changes are calculated as baseline minus 3 year values, and positive values reflect improvement
Based on five imputations
Metacarpophalangeal joint
Proximal interphalangeal joint
p<0.05
p<0.001
We analyzed the outcomes of the study hand (surgical) hand and the control (nonsurgical) hand in the SMPA group to determine if we would find comparable results to those found in Tables 3 and 4. The analysis looked at the difference in mean scores from baseline to 3 years for the two hands (Supplement Table 5). The results were similar to the analyses comparing SMPA and nonsurgical subjects; significant differences were found between study and control hands in the change in mean values from baseline to 3 years for arc of motion, ulnar drift, extensor lag and overall MHQ score.
We also compared results by study center. Patients in all centers showed significant improvement in MHQ, but even after adjusting for covariates including the use of biologic, the two U.S. sites showed significantly greater improvement than the non-US site. A previous paper noted the differences between the US and the UK sites which were attributed to differences in the health care systems between countries.35
Adverse events
One patient had an infection from a proximal interphalangeal joint fusion. Two patients required revision SMPA due to ulnar drift and dislocation of the implant respectively. Fractures and deformities of the silicone implant were assessed using radiographs. Of the 69 surgical cases, 42 had radiographs taken at 3 years after surgery. Four (9.5 %) subjects had definite fractures in at least one finger and 7 (16.7%) had at least one severely deformed joint. Seven subjects died prior to the 3 year assessment. None of the deaths were determined to be related to the study.
Discussion
The evidence-based medicine movement stresses the importance of finding the highest available evidence and combining that information with physician experience and patient preferences when determining the course of treatment. There is a substantial amount of high level evidence through randomized controlled trials that medications can slow or stop the progression of rheumatoid arthritis. Surgery, and in particular SMPA, cannot prevent the physical damage of RA, but there is some evidence that it can restore function to the hands of affected RA patients. The results presented in this paper are from the largest collaborative study between hand surgeons and rheumatologists on SMPA.
The results from extended follow-up of this cohort of surgical and nonsurgical subjects showed that the benefits of SMPA continue through 3 years after surgery. The main outcome of the study is hand function as assessed using the MHQ. Surgical patients, when compared to nonsurgical patients, reported significant improvements from the MHQ in hand function, ADL, aesthetics and satisfaction over time. For example, the average scores for these domains increased by 22, 16, 23, and 24 points respectively after adjusting for other variables. The minimal clinical important difference (MCID) calculated for the MHQ function and ADL domains are 13 and 3.36 Our results for these domains are well over this threshold. Previous studies have reported improvements in pain, aesthetics, satisfaction, ADL and function after SMPA. However, these results were not based on validated HRQL questionnaires.
Surgical subjects as compared to nonsurgical subjects show a dramatic improvement in the degree of ulnar drift, extensor lag and arc of motion at the MCPJ. We found an average 20 degree improvement in ulnar drift and 30 degree improvement in extensor lag over 3 years. Previous studies that did compare objective measures before and after surgery had similar results. These studies found ulnar drift to improve from 9 to 30 degrees post-operatively and extensor lag improved from 34 to 47 degrees.1,2,8,10,11,16 Arc of motion in our study increased 9 degrees on average over 3 years whereas other studies have reported from -11 to 34 degrees post-operative improvement.1-5,7,8,10,11,16,17 The lack of improvement in grip strength in this study has been confirmed in previously.8 SMPA allows the patient to open and close their hands more easily, but does not increase the strength of the hand or pinch of the fingers. There is no reference standard for determining hand function but research has shown that patient reported outcomes, such as those reported in the MHQ, are more sensitive patient-oriented measures of outcomes than traditional measures such as grip and pinch strength.37
Complications from SMPA in our cohort were minimal at 3 years. One complication that can arise from SMPA is implant fracture. Previous studies of implant fracture specifically for the silicone implant have found rates ranging from 0-67%.5-8,10,11,14,28,29,31,38-42 Overall, the 3-year fracture rate of 9.5% for this cohort is low.
The most important outcome for rheumatoid patients and hand surgeons considering surgery is improved function. Our 3 year results have demonstrated that the SMPA procedure will improve function and activities of daily living and restore the appearance of severely deformed rheumatoid hands. More importantly, the baseline adjusted difference between SMPA versus non-surgically treated hands remained significant, indicating that at three years after surgery, SMPA treated patients continued to have better hand outcomes than comparable non-surgically treated patients.
Supplementary Material
Significance and Innovation.
The study provides high level long-term evidence on silicone metacarpophalangeal arthroplasty (SMPA) results.
This is a large collaborative study between rheumatologists and hand surgeons.
The study uses a hand specific outcomes questionnaire to measure results.
Surgical subjects are compared to a nonsurgical cohort with similar levels of deformities.
Acknowledgements
The authors acknowledge the assistance of the following participants of the SMPA Study Group: Sandra V. Kotsis, MPH, (University of Michigan), Lorraine A. Zellers, CRC (Curtis National Hand Center), Marian Regan, MD, Mary J. Bradley, MSc, Melanie Arundell (Pulvertaft Hand Centre) and the referring rheumatologists in Michigan, Derby and Baltimore. The authors also greatly appreciate the assistance of Jeanne M. Riggs, OTR, CHT, Kurt Hiser, OTR, Carole Dodge, OTR, CHT, Jennifer Stowers, OTR, CHT, Cheryl Showerman, OTR, Jo Holmes, OTR, Victoria Jansen, PT and Helen Dear, OTR in taking measurements for the study patients.
Supported in part by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (2R01AR047328 - 06) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung)
Footnotes
Study registered at Clinicaltrials.gov, NCT00124254, http://www.clinicaltrials.gov
References
- 1.Kirschenbaum D, Schneider LH, Adams DC, Cody RP. Arthroplasty of the metacarpophalangeal joints with use of silicone-rubber implants in patients who have rheumatoid arthritis. Long-term results. J Bone Joint Surg Am. 1993 Jan;75(1):3–12. doi: 10.2106/00004623-199301000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Gellman H, Stetson W, Brumfield RH, Jr., Costigan W, Kuschner SH. Silastic metacarpophalangeal joint arthroplasty in patients with rheumatoid arthritis. Clin Orthop Relat Res. 1997 Sep;(342):16–21. [PubMed] [Google Scholar]
- 3.el-Gammal TA, Blair WF. Motion after metacarpophalangeal joint reconstruction in rheumatoid disease. J Hand Surg Am. 1993 May;18(3):504–511. doi: 10.1016/0363-5023(93)90100-H. [DOI] [PubMed] [Google Scholar]
- 4.Jensen CM, Boeckstyns ME, Kristiansen B. Silastic arthroplasty in rheumatoid MCP-joints. Acta Orthop Scand. 1986 Apr;57(2):138–140. doi: 10.3109/17453678609000887. [DOI] [PubMed] [Google Scholar]
- 5.Hansraj KK, Ashworth CR, Ebramzadeh E, et al. Swanson metacarpophalangeal joint arthroplasty in patients with rheumatoid arthritis. Clin Orthop Relat Res. 1997 Sep;(342):11–15. [PubMed] [Google Scholar]
- 6.Beckenbaugh RD, Dobyns JH, Linscheid RL, Bryan RS. Review and analysis of silicone-rubber metacarpophalangeal implants. J Bone Joint Surg. 1976 Jun;58A(4):483–487. [PubMed] [Google Scholar]
- 7.Mannerfelt L, Andersson K. Silastic arthroplasty of the metacarpophalangeal joints in rheumatoid arthritis. J Bone Joint Surg Am. 1975 Jun;57(4):484–489. [PubMed] [Google Scholar]
- 8.Blair WF, Shurr DG, Buckwalter JA. Metacarpophalangeal joint implant arthroplasty with a Silastic spacer. J Bone Joint Surg Am. 1984 Mar;66(3):365–370. [PubMed] [Google Scholar]
- 9.Fleming SG, Hay EL. Metacarpophalangeal joint arthroplasty eleven year follow-up study. J Hand Surg [Br] 1984 Oct;9(3):300–302. doi: 10.1016/0266-7681(84)90047-0. [DOI] [PubMed] [Google Scholar]
- 10.Bieber EJ, Weiland AJ, Volenec-Dowling S. Silicone-rubber implant arthroplasty of the metacarpophalangeal joints for rheumatoid arthritis. J Bone Joint Surg Am. 1986 Feb;68(2):206–209. [PubMed] [Google Scholar]
- 11.Goldfarb CA, Stern PJ. Metacarpophalangeal joint arthroplasty in rheumatoid arthritis. J Bone Joint Surg. 2003;85A:1869–1878. doi: 10.2106/00004623-200310000-00001. 2003. [DOI] [PubMed] [Google Scholar]
- 12.Chung KC, Kowalski CP, Myra Kim H, Kazmers IS. Patient outcomes following Swanson silastic metacarpophalangeal joint arthroplasty in the rheumatoid hand: a systematic overview. J Rheumatol. 2000 Jun;27(6):1395–1402. [PubMed] [Google Scholar]
- 13.Vahvanen V, Viljakka T. Silicone rubber implant arthroplasty of the metacarpophalangeal joint in rheumatoid arthritis: a follow-up study of 32 patients. J Hand Surg [Am] 1986 May;11(3):333–339. doi: 10.1016/s0363-5023(86)80138-1. [DOI] [PubMed] [Google Scholar]
- 14.Swanson AB. Flexible implant arthroplasty for arthritic finger joints: rationale, technique, and results of treatment. J Bone Joint Surg Am. 1972 Apr;54(3):435–455. [PubMed] [Google Scholar]
- 15.Sollerman CJ, Geijer M. Polyurethane versus silicone for endoprosthetic replacement of the metacarpophalangeal joints in rheumatoid arthritis. Scand J Plast Reconstr Surg Hand Surg. 1996 Jun;30(2):145–150. doi: 10.3109/02844319609056397. [DOI] [PubMed] [Google Scholar]
- 16.Rothwell AG, Cragg KJ, O’Neill LB. Hand function following Silastic arthroplasty of the metacarpophalangeal joints in the rheumatoid hand. J Hand Surg [Br] 1997 Feb;22(1):90–93. doi: 10.1016/s0266-7681(97)80027-7. [DOI] [PubMed] [Google Scholar]
- 17.McArthur PA, Milner RH. A prospective randomized comparison of Sutter and Swanson silastic spacers. J Hand Surg [Br] 1998 Oct;23(5):574–577. doi: 10.1016/s0266-7681(98)80004-1. [DOI] [PubMed] [Google Scholar]
- 18.Escott BG, Ronald K, Judd MG, Bogoch ER. NeuFlex and Swanson metacarpophalangeal implants for rheumatoid arthritis: prospective randomized, controlled clinical trial. J Hand Surg Am. 2010 Jan;35(1):44–51. doi: 10.1016/j.jhsa.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 19.Honkanen PB, Tiihonen R, Skytta ET, Ikavalko M, Lehto MU, Konttinen YT. Bioreconstructive poly-L/D-lactide implant compared with Swanson prosthesis in metacarpophalangeal joint arthroplasty in rheumatoid patients: a randomized clinical trial. J Hand Surg Eur Vol. 2010 Nov;35(9):746–753. doi: 10.1177/1753193410375777. [DOI] [PubMed] [Google Scholar]
- 20.Alderman AK, Chung KC, Kim HM, Fox DA, Ubel PA. Effectiveness of rheumatoid hand surgery: contrasting perceptions of hand surgeons and rheumatologists. J Hand Surg. 2003 Jan;28A(1):3–11. doi: 10.1053/jhsu.2003.50034. [DOI] [PubMed] [Google Scholar]
- 21.Alderman AK, Ubel PA, Kim HM, Fox DA, Chung KC. Surgical management of the rheumatoid hand: consensus and controversy among rheumatologists and hand surgeons. J Rheumatol. 2003 Jul;30(7):1464–1472. [PubMed] [Google Scholar]
- 22.Alderman AK, Chung KC, DeMonner S, Spilson SV, Hayward RA. Large area variations in the surgical management of the rheumatoid hand. Surg Forum. 2001;LII:479–481. 2001. [Google Scholar]
- 23.Alderman AK, Chung KC, Demonner S, Spilson SV, Hayward RA. The rheumatoid hand: a predictable disease with unpredictable surgical practice patterns. Arthritis Rheum. 2002 Oct 15;47(5):537–542. doi: 10.1002/art.10662. [DOI] [PubMed] [Google Scholar]
- 24.Mandl LA, Galvin DH, Bosch JP, et al. Metacarpophalangeal arthroplasty in rheumatoid arthritis: what determines satisfaction with surgery? J Rheumatol. 2002;29:2488–2491. 2002. [PubMed] [Google Scholar]
- 25.Bogoch ER, Judd MGP. The hand: a second face? J Rheumatol. 2002;29:2477–2483. 2002. [PubMed] [Google Scholar]
- 26.Chung KC, Burns PB, Wilgis EF, et al. A multicenter clinical trial in rheumatoid arthritis comparing silicone metacarpophalangeal joint arthroplasty with medical treatment. J Hand Surg Am. 2009 May-Jun;34(5):815–823. doi: 10.1016/j.jhsa.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sharma S, Schumacher HRJ, McLellan AT. Evaluation of the Jebsen hand function test for use in patients with rheumatoid arthritis. Arthritis Care Res. 1994;7:16–19. doi: 10.1002/art.1790070105. 1994. [DOI] [PubMed] [Google Scholar]
- 28.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg. 1998 Jul;23A(4):575–587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 29.Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999 Jun;42(6):619–622. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Meenan RF, Mason JH, Anderson JJ, Guccione AA, Kazis LE. AIMS2. The content and properties of a revised and expanded Arthritis Impact Measurement Scales Health Status Questionnaire. Arthritis Rheum. 1992 Jan;35(1):1–10. doi: 10.1002/art.1780350102. [DOI] [PubMed] [Google Scholar]
- 31.Bass RL, Stern PJ, Nairus JG. High implant fracture incidence with Sutter silicone metacarpophalangeal joint arthroplasty. J Hand Surg [Am] 1996 Sep;21(5):813–818. doi: 10.1016/S0363-5023(96)80197-3. [DOI] [PubMed] [Google Scholar]
- 32.D’Agostino RB., Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998 Oct 15;17(19):2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 33.Little RJA, Rubin DB. Statistical Analysis with Missing Data. Wiley; New York: 1987. [Google Scholar]
- 34.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Wiley; New York: 1987. [Google Scholar]
- 35.Chung KC, Kotsis SV, Fox DA, et al. Differences between the United States and the United Kingdom in the treatment of rheumatoid arthritis: analyses from a hand arthroplasty trial. Clin Rheumatol. 2010 Apr;29(4):363–367. doi: 10.1007/s10067-009-1314-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shauver MJ, Chung KC. The minimal clinically important difference of the Michigan hand outcomes questionnaire. J Hand Surg Am. 2009 Mar;34(3):509–514. doi: 10.1016/j.jhsa.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pincus T, Yazici Y, Bergman MJ. Patient questionnaires in rheumatoid arthritis: advantages and limitations as a quantitative, standardized scientific medical history. Rheum Dis Clin North Am. 2009 Nov;35(4):735–743. vii. doi: 10.1016/j.rdc.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 38.Schmidt K, Willburger RE, Miehlke RK, Witt K. Ten-year follow-up of silicone arthroplasty of the metacarpophalangeal joints in rheumatoid hands. Scand J Plast Reconstr Surg Hand Surg. 1999 Dec;33(4):433–438. doi: 10.1080/02844319950159163. [DOI] [PubMed] [Google Scholar]
- 39.Wilson YG, Sykes PJ, Niranian NS. Long-term follow-up of Swanson’s silastic arthroplasty of the metacarpophalangeal joints in rheumatoid arthritis. J Hand Surg. 1993;18B:81–91. doi: 10.1016/0266-7681(93)90203-r. [DOI] [PubMed] [Google Scholar]
- 40.Hagert CG, Eiken O, Ohlsson NM, Aschan W, Movin A. Metacarpophalangeal joint implants. I. Roentgenographic study on the silastic finger joint implant, swanson design. Scand J Plast Reconstr Surg. 1975;9(2):147–157. doi: 10.3109/02844317509022781. [DOI] [PubMed] [Google Scholar]
- 41.Levack B, Stewart HD, Flierenga H, Helal B. Metacarpo-phalangeal joint replacement with a new prosthesis: description and preliminary results of treatment with the Helal flap joint. J Hand Surg [Br] 1987 Oct;12(3):377–381. doi: 10.1016/0266-7681_87_90193-8. [DOI] [PubMed] [Google Scholar]
- 42.Creighton JJ, Jr., Steichen JB, Strickland JW. Long-term evaluation of Silastic trapezial arthroplasty in patients with osteoarthritis. J Hand Surg [Am] 1991 May;16(3):510–519. doi: 10.1016/0363-5023(91)90024-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.