Abstract
Despite advances in biomaterials and dialyzer design, thrombin generation occurs in the dialysis circuit because of platelet and leukocyte activation. As such, anticoagulation is required by the majority of children for successful dialysis to prevent clotting in the venous air detector and the capillary dialyzer, particularly for small children with slower blood flow rates. For many years unfractionated heparin has been the standard anticoagulant of choice, but is now being challenged by low-molecular-weight heparins (LMWHs) because they are simple to administer and reliable, particularly as the cost differential has been eroded. Alternative, nonheparin anticoagulants are more frequently available, but are often restricted to special circumstances: patients at high risk of hemorrhage; heparin allergy; or heparin-induced thrombocytopenia. These nonheparin alternatives are significantly more expensive than heparins, and may add a degree of complexity, such as citrate, which is a regional anticoagulant, although citrate-containing dialysate may permit short anticoagulant-free dialysis sessions. Systemic anticoagulants required for immune-mediated, heparin-induced thrombocytopenia are expensive and either have short half-lives, and therefore require continuous infusions, or prolonged half-lives, which, although allowing simple bolus administration, increases the risk of drug accumulation, over-dosage and hemorrhage.
Keywords: Heparin, Argatroban, Lepirudin, Citrate, Prostacyclin, Low molecular weight heparin, Dialysis
Introduction
The introduction of unfractionated heparin (UFH) to prevent clotting in the hemodialysis circuit was one of the major technological advances that allowed the development of dialysis. UFH predominantly acts by binding to antithrombin (formerly called antithrombin III), which inhibits thrombin (factor IIa) generation from prothrombin (factor II). However, initiation of thrombin generation is not primarily due to activation of the intrinsic (or contact) coagulation pathway, but rather by activation of platelets and leukocytes by the hemodialysis circuit [1]. In pediatric practice the narrower internal diameter venous access catheters [2] and dialysis needles required in infants and smaller children generate greater turbulent flows, with increased mechanical activation of platelets and leukocytes, resulting in the release of blebs of surface membrane, which act as a source of tissue factor, rapidly initiating thrombin generation, typically on platelet surfaces, which then stimulates further activation of the coagulation cascades with deposition of fibrin and platelet microparticles on the capillary dialyzer membrane surface [3].
Why change clinical practice?
Over the last few decades advances in polymer chemistry have resulted in changes in the biomaterials used in the manufacture of hemodialysis dialyzers and blood lines and, coupled with the introduction of nanotechnology into capillary dialyzer manufacture, have reduced the bio-incompatibility of the extracorporeal circuit [4, 5] resulting in reduced anticoagulation requirements [6].
Unfractionated heparin is inexpensive and most centers have a wealth of clinical experience, such that many no longer regularly monitor UFH dosages by laboratory-activated partial thromboplastin ratio (aPTTr) or bedside-activated clotting times (ACT). Clinical practice divides into those centers that give a bolus dose of UFH followed by an infusion, with some empirically giving a 500-IU bolus followed by 1,000 IU/h for larger children, a 250-IU bolus with an infusion of 500 IU/h for smaller children, and a 250-IU bolus for babies followed by an infusion of 300 IU/h, whereas others initially dose UFH according to body weight, bolus 50 IU/kg followed by 25 IU/kg/h, and those centers that simply give two boluses, one larger (50 IU/kg) at the start of dialysis and a smaller (25 IU/kg) second dose half way through the treatment session) [7]. Thereafter, dosages and the time to stop the UFH infusion are usually adjusted according to visual clot score in the venous air detector, dialyzer and needle site bleeding times. Thus, in practice most centers either stop the UFH infusion some 20–30 min prior to the end of the dialysis session or slow the infusion down to prevent excessive bleeding from fistula needle puncture sites. A minority adjust UFH dosing regimens to achieve an ACT 180–220 s, or aPTTr of 1.5–2.0.
Even so, UFH adds a degree of complexity by either requiring a UFH infusion to be made, or the nurses remembering to give a second bolus, thus potentially risking inadequate anticoagulation followed by over-anticoagulation.
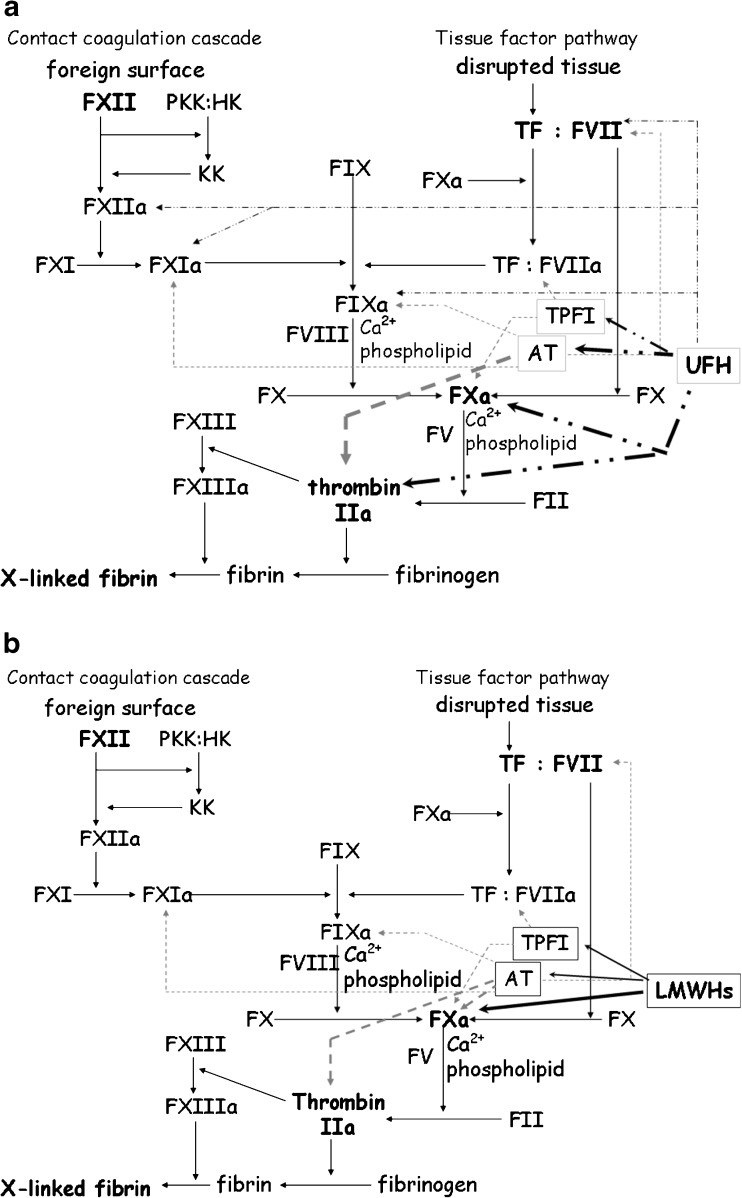
As UFH is not a single molecule, but a series of different sized glycosaminoglycans, quality assurance is simply based on negative charge content, and as such pharmacological activity may vary between different batches, as not all UFH molecules contain the key pentasaccharide motif that binds to antithrombin (AT; Fig. 1a).
Fig. 1.
a Cartoon showing the action of unfractionated heparin (UFH) on the traditional coagulation cascades, the width of the black dotted arrow denotes the strength of action. The action of natural inhibitors AT and TFPI are indicated by gray dotted arrows. The width of the arrow denotes the strength of action. a activated factor, AT antithrombin III, F factor, HMWK high-molecular-weight kallikrein, KK kallikrein, LMWH low-molecular-weight heparin, PKK prekallikrein, TF tissue factor, TFPI tissue factor plasma inhibitor. b Cartoon showing the action of low molecular weight heparin (LMWH) on the traditional coagulation cascades, the width of the black arrow denotes the strength of action. The action of natural inhibitors AT and TFPI are indicated by gray dotted arrows. The width of the arrow denotes the strength of action. a activated factor, AT antithrombin III, F factor, HMWK high-molecular-weight kallikrein, KK kallikrein, LMWH low-molecular-weight heparin, PKK prekallikrein, TF tissue factor, TFPI tissue factor plasma inhibitor
Although UFH has a rapid action onset time of ∼3–5 min, the half-life varies between 0.5 h and 2.0 h in patients receiving dialysis, despite being metabolized in a dose-dependent fashion by hepatic and vascular endothelial heparinases [8]. The disparity in half-life is greatest at the extremes of weight, particularly in pediatric practice in infants < 10 kg. In addition, as UFH is a series of large charged molecules, metabolism is also affected by nonspecific electrostatic binding to the endothelium, leukocytes and plasma proteins, and also binding to plastic tubing and dialyzer capillary membrane surfaces in the extracorporeal circuit [9]. Because of the variability of biological activity and nonspecific binding, studies using pharmacokinetic algorithms to predict UFH dosages failed to significantly improve anticoagulation regimes, due to UFH batch, and inter- and intra-patient variability [10, 11].
Although the most widely used anticoagulant for hemodialysis worldwide, UFH is not without adverse effects. Some patients are allergic to heparin, typically reacting to porcine products, and rarely heparin-induced thrombocytopenia can develop, particularly with bovine heparins [12]. In the longer term heparin exposure can lead to osteoporosis and increase the risk of hyperkalemia.
Low-molecular-weight heparin
To improve the predictability of the anticoagulant effects of UFH, low-molecular-weight-heparins (LMWHs) were produced by cleavage of UFH. As LMWHs are smaller molecules, typically around 5 kDa, they are not long enough to bind both AT and thrombin, and as such lose some anti-thrombin activity, while retaining anti-Xa activity (Fig. 1b). However, LMWHs also have a greater effect than UFH on the release of tissue plasma factor inhibitor (TPFI), the natural inhibitor of the extrinsic coagulation cascade (Fig. 1b). LMWHs are not a single entity, as some are made by chemical cleavage and others enzymatic digestion, so they differ in length, molecular weight, and charge [13], and vary biologically in their relative effects on inhibiting factor IIa and Xa (Table 1) [14]. The LMWHs enoxaparin and tinzaparin represent the ends of the spectrum of LMWHs in terms of half-life and the relative ratio of anti-Xa to anti-IIa activity, with enoxaparin having the longest half-life just over 24 hours, whereas tinzaparin has the shortest, as it is degraded by endothelial heparinases [15]. Tinzaparin has the lowest ratio of anti-IIa/Xa activity and so bleeding due to over-anticoagulation can potentially be reversed by protamine, whereas protamine is much less likely to be effective with enoxaparin, which has the highest anti-IIa/Xa ratio (Table 1).
Table 1.
Comparison of currently available low molecular weight heparins (LMWH). Dosage recommendations refer to a standard 4-h dialysis session. Adult single bolus dosages for patients 50–100 kg in IU unless otherwise specified. Pediatric dosages for a 50-kg or heavier child/adolescent, unless otherwise specified [13–19]. Average molecular weight (MWt) kDa, ratio of inhibitory activity to factor IIa (thrombin) to activated factor X (Xa). Average half-life given; note that half-lives vary with residual renal function
| LMWH | MWt kDa | Half-life (h) | IIa/Xa | Adult dose | Pediatric dose |
|---|---|---|---|---|---|
| Tinzaparin | 5.0 | 4.5 | 1.9 | 1,500–3,500 | 50 IU/kg |
| Dalteparin | 6.0 | 5.0 | 2.7 | 5,000 | 40 IU/kg |
| < 15 kg 1,500 | |||||
| 15-30 kg 2,500 | |||||
| 30–50 kg 5,000 | |||||
| Reviparin | 4.0 | 5.0 | 3.5 | 85 IU/kg | 85 IU/kg |
| Nadroparin | 4.5 | 5.0 | 3.6 | 3,800–5,700 | 114 IU/kg |
| 70 IU/kg | < 50 kg 3,000 | ||||
| Enoxaparin | 4.2 | 27.7 | 3.8 | 0.5–0.7 mg/kg | 24–36 mg/m2 |
| 0.5–1.0 mg/kg |
Low molecular weight heparins (LMWHs) are now typically administered as a single bolus, thus requiring less nurse time and complexity, as they have higher bioavailability, because of less nonspecific binding to the endothelium, plasma proteins, and platelets, and the surfaces of the dialysis circuit. Thus, LMWHs have a more rapid onset of action and cause less platelet and leukocyte activation and less fibrin deposition on dialyzer membrane surfaces than UFH [1]. In addition, heparin-induced immune-mediated thrombocytopenia is less common with LMWHs than UFH [16]. When first introduced LMWHs were much more expensive than UFH; however, with the passage of time, and introduction of newer LMWHs, the price differential has been eroded, and indeed in some countries LMWHs are similarly priced to UFH.
LMHWs for extended dialysis and more frequent dialysis
The half-lives of LMWHs are prolonged, as they are predominantly renally cleared—as such they are not suited to very short dialysis sessions of 90–120 min [17]. There have been reports of enoxaparin, which has the longest half-life, accumulating in patients attending for daily dialysis, but not the other LMHWs [15]. However, because of their smaller size, some of the initial bolus when administered predialyzer can be lost before the membrane becomes protein-coated [18]. As such enoxaparin has not been observed to accumulate in children undergoing frequent pre-dilutional hemodiafiltration (M. Fischbach, personal communication, November 14, 2011). Alteration of the dialyzer surface by coating with vitamin E reduces LMWH losses, leading to dose reduction [5].
Although LMWHs have longer half-lives, a single bolus may not always provide adequate anticoagulation for overnight dialysis [19]. If a single bolus, for example, dalteparin 100 IU/kg, or enoxaparin 1 mg/kg [20], does not provide adequate anticoagulation, then either two boluses can be tried, or an initial bolus followed by an infusion, for example, dalteparin infusion of 10–15 IU/h, nadroparin 380 IU/h or enoxaparin 3 mg/h [21, 22].
Monitoring of LMWHs
As LMWHs predominantly have anti-Xa activity, but only a modest effect on thrombin, they only minimally affect the aPTTr, and require anti-Xa activity assays [22]. Although bedside tests have been developed, these are not widely used, with most centers relying on laboratory testing. When LMWHs were first trialed, dosages were titrated to achieve a peak anti-Xa activity of 0.4–0.6 IU/ml, and <0.2 IU/ml at the end of dialysis [23]. However, as the anticoagulant effect of LMWHs is more predictable than that of UFH, most centers do not formally monitor anti-Xa activity [24], but simply adjust the initial bolus dose according to visual inspection of clotting in the venous air detector and dialyzer, and the time needed for needle puncture sites to stop bleeding [14].
Anticoagulation-free dialysis circuits
As platelets play a key role in initiating clotting in the dialysis circuit, anticoagulation is rarely required in thrombocytopenic patients, whereas anticoagulation is typically required in children prescribed warfarin, unless the international normalized ratio is ≥3.0. Children with higher hematocrits have greater heparin requirements [25], and circuit clotting is more common with babies. The traditional approach to reducing clotting and performing anticoagulant-free dialysis has been to use regular predialyzer saline boluses [8]. In addition, some centers circulate heparinized saline (UFH 5,000–20,000 IU) for up to an hour prior to dialysis, to allow UFH binding to the dialyzer and circuit, and then the heparinized solution is rinsed out before dialysis is started [26]. Higher blood pump speeds (> 300 ml/min) and cooled dialysate (at 20°C) also reduce the risk of clotting [27], whereas the risk of clotting is increased in infants < 10 kg with slower blood flows [28].
Heparin-coated dialyzers and heparin-bonded circuits
Heparin bonding of cardiopulmonary and extracorporeal oxygenation circuits reduces UFH requirements and the risk of hemorrhage. Alteration of the polyacrylonitrile dialyzer surface increased heparin binding, which led to the commercialization of heparin-bonded dialyzers. These have been reported to permit heparin-free short dialysis sessions [29], and reduce heparin requirements for routine outpatient hemodialysis [30]. Heparin-coated and bonded dialysis circuits have also been reported to allow heparin-free dialysis, but this is not currently commercially available [31].
Regional anticoagulants
Unfractionated heparin and LMHW are systemic anticoagulants and thus increase the risk of hemorrhage with overdosage and also in susceptible groups of patients, including those postoperatively and also neonates with their increased susceptibility to intracranial hemorrhage. As such, regional anticoagulants offer the potential to anticoagulate the dialysis circuit, but not the patient, thus reducing the risk of bleeding. Citrate is the most commonly used regional anticoagulant and its effect is reversed in the dialysis circuit, whereas prostanoids and nafamostat are regional anticoagulants because of their very short systemic half-lives.
Citrate anticoagulation
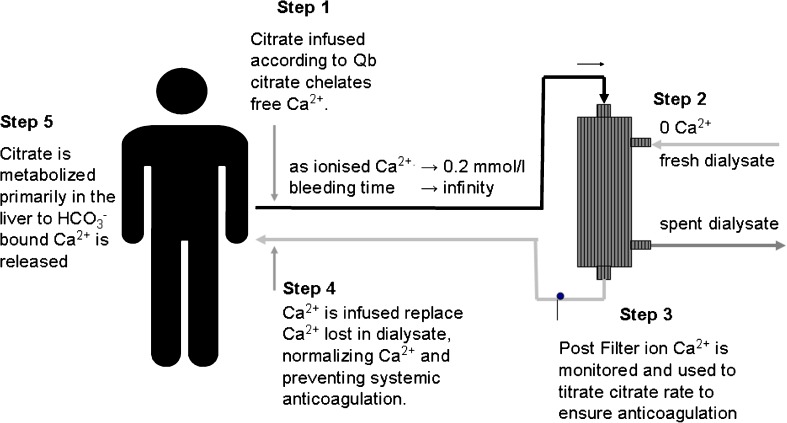
Citrate is an effective regional anticoagulant [1], which acts by binding ionized calcium. Thus, typically a specialized dialysate with no calcium, low or zero magnesium, and reduced or no bicarbonate is required [32, 33]. The citrate infusion must be adjusted with the blood flow to achieve an ionized calcium concentration of 0.2–0.3 mmol/l to prevent clotting within the circuit, which equates to a predialyzer citrate concentration around 4 mmol/l [33]. Although most centers use hypertonic trisodium citrate (TCA 4% citrate), others use 3% acid citrate dextrose (acid citrate dextrose A solution contains 22.0 g/l sodium citrate with a citrate concentration of 0.112 mmol/ml, 8.0 g/l citric acid monohydrate and 24.5 g/l glucose) [34]. For example, for a blood flow of 100 ml/min this equates to an infusion of 175 ml/min for 4% TCA or 210 ml/min for ACD-A.
Citrate chelates calcium and magnesium, with losses into the dialysate [33]; thus, to maintain a normal ionized plasma concentration, calcium is infused centrally or into the venous line (Fig. 2). As the half-life of calcium-citrate is 2–3 min, citrate acts as a regional anticoagulant, allowing successful dialysis of patients at high risk of bleeding [32].
Fig. 2.
Cartoon depicting the five steps of regional citrate anticoagulation for hemodialysis. Ca2+ ionized calcium
Although the activated clotting time (ACT) can be used to monitor the anticoagulant effect of citrate (160–200 s postcitrate infusion and 80–120 s postdialyzer), most centers simply adjust the citrate infusion to achieve a postdialyzer ionized calcium concentration of 0.25–0.35 mmol/l [35]. Although citrate may appear to be a complex treatment, Kreuzer recently suggested a simplified starting algorithm for intermittent hemodialysis, using 3% commercially available citrate (ACD-A) infused at 8X ml/h with a blood flow of 4X ml/min, and 10% calcium gluconate started at X ml/h using a zero calcium dialysate with a lowered sodium level of 134 mmol/l and a bicarbonate level of 26–30 mmol/l [34]. For example, with a blood flow of 200 ml/min, then the starting ACD-A infusion would be 400 ml/h, and the calcium infusion 50 ml/h. Thereafter, the citrate flow is adjusted to maintain postdialyzer ionized calcium at ≤0.30 mmol/l and the calcium gluconate adjusted to maintain the ionized calcium within the normal physiological range (1.00–1.30 mmol/l). Other models for prescribing citrate dialysis with trisodium citrate are similarly available [35].
Citrate dialysis can potentially lead to citrate intoxication, if citrate is not adequately metabolized, in cases of severe hepatic failure, muscle hypo-perfusion and rhabdomyolysis and also during isolated ultrafiltration, when citrate is not being dialyzed out [33]. Accumulation of calcium–citrate complexes increases total serum calcium, but reduces the ionized fraction, often termed the “calcium gap,” and increases the ratio of total calcium to ionized calcium, and citrate accumulation considered with ratios of > 2.5 [33]. As the total calcium increases it is important to realize that this is due to failure to adequately clear citrate and as such the citrate infusion should be reduced, or even stopped. Increasing the dialysate flow can also increase citrate clearance.
Trisodium citrate introduces a sodium load, and as each citrate is eventually metabolized to three bicarbonates, risks alkalosis, and as such dialysates are typically adjusted with reduced sodium and bicarbonate concentrations. As magnesium is also lost with citrate, some centers choose to add magnesium to the dialysate [36]. Calcium and magnesium-containing dialysates have been used with citrate anticoagulation, and although they reduce complexity by dispensing with the venous calcium infusion, they increase the risk of circuit clotting [37].
Citrate-containing dialysates
Dialysates typically contain a small amount of acetate to reduce calcium deposition within the dialysis machine circuit. Replacing some of the acetate with citrate (Citrasate®; Advanced Renal Technologies, Bellevue, WA, USA; containing 1.5 mmol/l calcium and 0.8 mmol/l citrate) has been reported to improve dialyzer clearances and allow heparin-free dialysis, although many centers have found that additional, but reduced dosages of systemic anticoagulants are often required [38, 39].
Serine protease inhibitors
Nafamostat mesilate is a serine protease inhibitor with a half-life of 5–8 min, acts predominantly as a regional anticoagulant by inhibiting thrombin, factor Xa and factor XIIa, but also has effects on the kinin system, fibrinolysis, and platelet activation [40].
Most clinical experience with nafamostat for intermittent hemodialysis emanates from Japan, with a bolus of 20 mg for adults combined with an infusion rate of 40 mg/h, which is then adjusted to achieve a target aPTTr of 1.5–2.0, or activated coagulation time of 140–180 s [40, 41]. The infusion rates reported for children have varied between 0.1 and 1 mg/kg/h. Depending upon the dialyzer, some 40% of nafamostat can be removed during dialysis with high flux membranes. There have been occasional reports of myalgia, arthralgia, eosinophilia, and rarely anaphylactoid reactions and agranulocytosis with nafamostat.
Prostacyclin and other prostanoids
Prostacyclin (PGI2) is the most potent of the prostanoids, which are naturally occurring anticoagulants produced by endothelial cells from arachidonic acid, and has a very short half-life of 2–3 min [25]. Naturally occurring prostanoids, including PGI2 and its synthetic analogue epoprostenol, block platelet cyclic AMP, reducing platelet activation and dialyzer membrane fouling. Prostanoids, particularly PGI2 are also potent pulmonary and systemic vasodilators and thus may induce symptomatic hypotension, and as such should not be considered in hypotensive children. If hypotension should develop then this can usually be readily reversed by stopping the infusion, because of the short half-life. The risk of hypotension can be reduced by slowly increasing the dose, starting at 0.5 ng/kg/min, and steadily increasing to the standard infusion rate for hemodialysis of 5 ng/kg/min [8]. Other prostanoids, such as prostaglandin E1 (PGE1 also known as alprostadil) and prostaglandin D, also have anti-platelet effects and can similarly be used as extracorporeal anticoagulants. PGE1 and PGD are not as potent as prostacyclin, so do not cause as much hypotension, but also require higher infusion rates of 5–20 ng/kg/min to achieve adequate extracorporeal anticoagulation [25].
As PGI2 and other prostanoids primarily block platelet activation they do not have any measurable effect on standard laboratory coagulation assays. As such, their anticoagulant effect cannot be readily measured to allow adjustment of infusion rates. As PGI2, other natural prostanoids, and their synthetic analogs are essentially regional anticoagulants, they have been successfully used to dialyze patients at high risk of hemorrhage.
Systemic anticoagulants as alternatives to the heparins
Naturally occurring proteoglycans and heparinoids
Proteoglycans are naturally occurring anticoagulants, produced by mammalian endothelium, but also by many other species including algae. They can also have anti-inflammatory actions, for example, by inhibiting the classical complement pathway. Dermatan sulfate was one of the first proteoglycans to be used as an anticoagulant for hemodialysis using either a single bolus dose of 6 mg/kg, or a combination of a smaller initial bolus dose of 4 mg/kg with a continuous infusion of 0.65 mg/kg/h [41]. Proteoglycans, similar to heparin, are negatively charged molecules, but of lower molecular weight, which can bind to antithrombin and other plasma proteins by electrostatic charge, although dermatan sulfate can also bind to heparin cofactor II to inhibit thrombin, and both chondroitin sulfate and heparan sulfate have been reported to contain the key pentasaccharide motif that binds to antithrombin. Other proteoglycans that have been used occasionally as anticoagulants for hemodialysis include sulodexide (80% iduroylglycos-aminoglycan sulfate and 20% dermatan sulfate) and mesoglycan, which is composed of varying amounts (25–60%) of dermatan sulfate and 3–15% of chondroitin sulfate. As these proteoglycans are lower molecular weight compounds they are subject to clearance during predilational hemodiafiltration and high flux dialysis.
In current clinical practice danaparoid, a mixture of 84% heparan sulfate, 12% dermatan sulfate and 4% chondroitin sulfate, with a molecular weight of 5.5 kD, is the most commonly used proteoglycan for extracorporeal anticoagulation. Danaparoid is a naturally occurring proteoglycan obtained from porcine intestinal mucosa. Danaparoid, as with other proteoglycans, predominantly has anticoagulant activity against factor Xa, but also has some activity against factor thrombin due to interaction with AT. Danaparoid is expensive, and therefore tends to be restricted for anti-coagulating patients with immune-mediated heparin thrombocytopenia (HIT) [42]. Compared with other anticoagulants for treating patients with HIT, danaparoid has been reported to be more effective in preventing thrombosis by not only reducing the binding of platelet factor 4 to platelets, but also disrupting immune complexes that contain platelet factor 4. Hence, danaparoid can prevent activation of platelets by heparin-induced thrombocytopenia antibodies. However, prior to initiating danaparoid therapy laboratory testing for in vitro cross-reactivity should be checked, as danaparoid may be contaminated with small amounts of heparin, although there are no reports suggesting that this is clinically relevant.
As with other proteoglycans, danaparoid has a prolonged half-life depending upon residual renal function of up to 30 h in dialysis patients [43], and is therefore given by a single bolus at the start of dialysis. As the half-life is so prolonged, monitoring and dose adjustment is based on the anti-Xa activity prior to the start of the following dialysis session to prevent accumulation. In clinical practice, providing the patient has no additional hemorrhagic risk, then one pragmatic dosing schedule would be to give a higher initial single bolus with the first hemodialysis (3,750 IU if weight > 55 kg, 2,500 IU in patients <55 kg) and then reduced prior to the second dialysis (2,500 IU if weight > 55 kg and 2,000 IU if weight < 55 kg) [43]. An alternative strategy is to give a bolus of 1,000 IU plus 30 IU/kg for children aged < 10 years; and 1,500 U plus 30 U/kg for older children 10–17 years [17], and thereafter danaparoid bolus doses adjusted on the basis of the anti-Xa activity before dialysis, aiming for a value of <0.3 IU/ml and no visible signs of clotting in the circuit with an intradialytic anti-Xa activity of 0.4–0.6 IU/ml. Subsequently, no change in bolus dose if anti-Xa activity <0.3 U/ml, reduced dose by 250 IU if anti-Xa activity 0.3–0.5 U/ml, or withdrawn if anti-Xa activity >0.5 IU/ml (Table 2) [17].
Table 2.
Alternative options to heparin for cases of heparin-induced thrombocytopenia (argatroban, lepirudin, and danaparoid) and regional anticoagulants for patients at risk of hemorrhage. Activated partial thromboplastin time ratio (aPTTr), anti-factor Xa activity (antiXa). *Possible actions if clot appears in the dialysis circuit
| Loading dose | Maintenance dose | Monitoring | Dose adjustment | |
|---|---|---|---|---|
| Argatroban | Nil | 0.7 μg/kg.min (Liver disease 0.2 μg/kg/min) | aPTTr target 2.0–2.5 check after 2 h | Adjust if required by 0.25 μg/kg/min and recheck aPTTR |
| Lepirudin | 0.2–0.5 mg/kg 5–30 mg | None | Hirudin 0.5–0.8 μg/ml aPTTr 1.5–2.0 | Adjust dose for subsequent dialysis |
| Danaparoid | 1,000 + 30 IU/kg if aged < 10 years or 1,500 +30 IU/kg aged >10 years | None | Predialysis antiXa <0.30 IU/l | Reduce dose by 250 IU if predialysis anti-Xa >0.3 <0.5 and stop if >0.5 IU/l |
| Citrate infusion | None | Adjusted to blood flow | Postdialyzer ionized calcium 0.2–0.3 mmol/land normal systemic calcium | Increasing systemic calcium suspect citrate toxicity—reduce infusion or increase dialysate flow |
| Citrate dialysate | None | Fixed amount of citrate in dialysate | None | *Consider increasing dialysate flow |
| Prostacyclin | None | 5–10 ng/kg/min | None | * Increase infusion if blood pressure permits |
Synthetic heparinoids
Neither fondaparinux nor idraparinux is currently licensed as an anticoagulant for intermittent hemodialysis. However, patients may be prescribed these systemic anticoagulants for other medical conditions that also require dialysis [44]. The normal half-life of fondaparinux of 12–17 h is markedly increased in patients receiving dialysis such that even reduced dosages (normal dose 5 mg daily for patients 50–75 kg, 7.5 mg for patients 75–100 kg) and 0.0125 to 0.05 mg/kg or 2.5-mg boluses with alternate-day hemodialysis can lead to accumulation and inter-dialytic systemic anticoagulation with low-flux dialyzers [45]. However, high-flux dialysis and hemodiafiltration lead to increased intradialytic losses and coupled with daily treatments might then require larger boluses or daily administration to sustain systemic anticoagulation [12]. Idraparinux, has an even longer half-life than fondaparinux.
Direct thrombin inhibitors
Irreversible direct thrombin inhibitors
Lepirudin, a recombinant form of the natural anticoagulant hirudin, is renally excreted; thus, it has a prolonged half-life in dialysis patients of >35 h, with reports of >100 h in anephric patients. As such, lepirudin is given as a single bolus, with centers giving varying doses from 0.2–0.5 mg/kg (5–30 mg) [8, 46]. As lepirudin is a small peptide (molecular weight 6.9 kD) it can be cleared by low-flux dialysis depending upon dialyzer choice, with greater clearance during high-flux hemodialysis and hemodiafiltration [47].
Lepirudin is typically used for anticoagulated patients with immune-mediated heparin-induced thrombocytopenia, and paradoxically antibodies to hirudin have been variously reported to develop in 10–50% of patients continuously treated with hirudin. These antibodies reduce clearance, but do not affect anticoagulant activity, thereby risking accumulation of an irreversible direct thrombin inhibitor and bleeding [46]. In these cases with anti-hirudin antibodies, only plasma exchange can remove the complexes.
As hirudin has such a prolonged half-life, dose adjustments are made by monitoring anticoagulation or plasma hirudin concentration prior to the following hemodialysis session until a steady state is achieved; even so, regular checking is warranted to detect lepirudin accumulation due to antibody formation. Lepirudin was initially monitored with aPTTr, aiming for a value <1.5 prior to dialysis to prevent lepirudin accumulation, and 1.5–2.0 during dialysis. However, the relationship between plasma lepirudin concentration and aPTTr is not linear; thus, what may appear to be small increases in aPTTr may reflect major increases in plasma lepirudin concentration, with risk of hemorrhage [47]. Thus, most centers recommend further testing by measuring either the ecarin clotting tests (a laboratory test of direct thrombin activation based on snake venom) or plasma hirudin concentration, when the aPTTr is > 1.5. There are a number of ecarin clotting tests now commercially available, but there is currently no standardization or reference range, as target ranges vary between assays [42]. As such, many centers have turned to measuring plasma hirudin, aiming for a therapeutic target of 0.5–0.8 μg/ml [42].
Accumulation and overdosage of lepirudin significantly increase the risk of bleeding, as lepirudin is an irreversible thrombin inhibitor. There is no simple antidote, and management centers correct the coagulation defect by administering fresh frozen plasma and activated factor VII concentrates, similar to the management of treating bleeding due to other antithrombin agents and heparinoids. In addition, lepirudin can be cleared by hemodiafiltration, or, in cases of lepirudin accumulation due to the formation of anti-lepirudin antibodies, plasma exchange [47]. Other reported serious complications with lepirudin include anaphylactoid reactions, which are more common following repeated administration, and further administration is contraindicated.
Reversible direct thrombin inhibitors
Argatroban is a synthetic peptide derived from arginine, with a molecular weight of 527 Da, and acts as a reversible direct thrombin inhibitor by binding to the catalytic site of thrombin. Argatroban is licensed by the FDA for treatment of immune-mediated heparin-induced thrombocytopenia in children in the USA, but is not currently licensed for children in Europe. As argatroban is used as a systemic anticoagulant for treating cases of immune-mediated heparin-induced thrombocytopenia, patients are treated with a continuous infusion. Although argatroban is predominantly metabolized in the liver, the half-life is increased in patients with renal failure [48]; thus, the doses reported for children requiring dialysis are lower than for those with normal renal function. Thus, whereas the standard dose for initiating argatroban is 2.0 μg/kg/min, those used for dialysis-dependent patients have ranged from 0.3 to 12 μg/kg/min [49], with a recommended starting dose of 0.75 μg/kg/min for children with normal hepatic function, reduced for those with liver disease or elevated serum bilirubin to 0.2 μg/kg/min [48]. As argatroban has a prompt action, then the aPPTr should be checked 2 h after starting the infusion, and the infusion dose increased or decreased by 0.25 μg/kg/min to achieve an aPTTr of 2.0–2.5, and then rechecked every 2–4 h until a steady state is achieved. Argatroban is not significantly removed by dialysis owing to protein binding, and consideration should be given to reducing the dose 20–30 min prior to the end of a dialysis session to prevent excessive bleeding from fistula needle puncture sites.
Argatroban is typically a short term treatment, until the immune-mediated thrombocytopenia has resolved, and patients are then warfarinized. Argatroban, and to a lesser extent its major metabolite, termed M1, can cause prolongation of the international normalized ratio, and therefore making conversion to warfarin more difficult to judge when patients are fully warfarinzed and argatroban should be withdrawn [39].
In cases of overdosage or bleeding, the infusion should be stopped, and depending upon the severity of the clinical situation fresh frozen plasma and activated factor VII concentrates may be required.
Although bivalirudin is not licensed for hemodialysis, it is a reversible direct thrombin inhibitor used by cardiologists that has a much shorter half-life than hirudin. Preliminary studies where bivalirudin was infused at 1.0–2.5 mg/h (0.009–0.023 mg/kg/h) aiming for a target aPTTr of ∼1.5, reported successful dialysis without circuit clotting.
Summary
Anticoagulation requirements for dialysis have reduced over time because of improvements in circuit design, biomaterials, and the introduction of nanotechnology manufacture, all designed to minimize bio-incompatibility and reduce platelet and leukocyte activation. Although UFH remains the most commonly used anticoagulant worldwide for standard, extended, and more frequent intermittent hemodialysis sessions, it does not effectively prevent platelet microthrombi formation, and carries an increased risk of bleeding. LMWHs not only have quicker onset of action, but also have a more predictable anticoagulant effect and reduce dialyzer fibrin and platelet deposition compared with UFH. As the cost of LMWHs has continued to fall, they are becoming the anticoagulant of choice in an increasing number of centers.
Heparins are systemic anticoagulants; thus, regional anticoagulants are preferred for patients at risk of hemorrhage. Although citrate potentially adds an extra degree of complexity, an increasing number of centers are using citrate in everyday practice as, compared with other regional anticoagulants, citrate does not have the hypotensive effects of the prostanoids, or the costs of nafamostat.
Heparin-induced immune-mediated thrombocytopenia can occur with UFH and to a lesser extent LMWHs. Systemic anticoagulation options reside with either the direct thrombin inhibitors (argatroban and lepirudin) or the heparinoid danaparoid. All are substantially more costly than heparin, with an increased risk of hemorrhage, particularly for lepirudin.
Acknowledgements
I am indebted to Professors Michel Fischbach, Stuart Goldstein, and Drs Patrick Brophy and Deepa Chand.
Competing interests
The author declares no competing interests.
Key summary points
Low molecular weight heparins have a more rapid onset of action, a more predictable anticoagulant effect and a reduced deposition of platelets and thrombin on dialyzer surfaces compared with unfractionated heparin.
Citrate is a potent regional anticoagulant, but adds a degree of complexity requiring a zero calcium dialysate for best results, regulation of citrate infusion by monitoring ionized to total serum calcium, and a central calcium infusion to prevent hypocalcemia.
Danaparoid, argatroban, and lepirudin provide systemic anticoagulation for cases of immune-mediated heparin-induced thrombocytopenia, but availability and licensing for pediatric patients vary between countries. They are expensive, and both lepirudin and argatroban increase the risk of hemorrhage.
Research points
Continued research is required to develop biomaterials for the dialysis circuit that do not activate platelet and leukocytes to permit future anticoagulation free dialysis.
Newer oral anticoagulants that act as thrombin inhibitors or anti-factor Xa antagonists are being developed for clinical practice, and research is required to determine whether patients prescribed these agents require reduced or no additional anticoagulation for dialysis.
As low molecular weight heparins and heparinoids become more readily used in clinical practice, more rapid or bedside tests of anti-Xa activity need to be developed to allow monitoring of hospital patients given low molecular weight heparin prophylaxis or treatment, who then require dialysis.
Development of specific treatments to manage bleeding in patients over-anticoagulated with direct thrombin inhibitors.
Multiple choice questions (Answers are provided following the reference list.)
Low molecular weight heparins:
Have an increased half-life compared with unfractionated heparin
Carry a similar risk to unfractionated heparin of causing immune-mediated thrombocytopenia
Are suitable for short (≤ 2 h) dialysis sessions
Should be monitored by the activated partial thromboplastin time
Citrate is a regional anticoagulant:
ACD-A citrate is a more effective anticoagulant than trisodium citrate
Which must only be used with a special calcium free dialysate
Which may cause hypomagnesemia
Which should be adjusted according to postdialyzer serum calcium
Danaparoid is a naturally occurring heparinoid:
Which has a similar half-life to unfractionated heparin
Can be monitored by measuring the activated partial thromboplastin time
Which is made up of heparan and dermatan sulfate
Which can disrupt heparin-platelet factor 4 antibody complexes
Lepirudin is a recombinant form of hirudin which:
Can be cleared during hemodiafiltration
Reversibly binds to thrombin
Should be administered by continuous infusion
Carries a reduced risk of bleeding compared with unfractionated heparin
Argatroban is a synthetic peptide derived from arginine which:
Is predominantly metabolized by the kidney
Can be monitored by the activated partial thromboplastin time
Interacts with warfarin to prolong the international normalized ratio
Can cause anaphylactoid reactions
Footnotes
Answers
MCQ 1 Answer 2: Have an increased half-life compared with unfractionated heparin
MCQ 2 Answer 3: Which may cause hypomagnesemia
MCQ 3 Answer 4: Which can disrupt heparin-platelet factor 4 antibody complexes
MCQ 4 Answer 1: Can be cleared during hemodiafiltration
MCQ 5 Answer 2: Can be monitored by the activated partial thromboplastin time
References
- 1.Hofbauer R, Moser D, Frass M, Oberbauer R, Kaye AD, Wagner O, Kapiotis S, Druml W. Effect of anticoagulation on blood membrane interactions during haemodialysis. Kidney Int. 1999;56:1578–1583. doi: 10.1046/j.1523-1755.1999.00671.x. [DOI] [PubMed] [Google Scholar]
- 2.Davenport A. Central venous catheters for haemodialysis: how to overcome the problems. Hemodial Int. 2000;4:78–82. doi: 10.1111/hdi.2000.4.1.78. [DOI] [PubMed] [Google Scholar]
- 3.Davenport A. Membrane designs and composition for hemodialysis, hemofiltration and hemodialfiltration: past, present and future. Minerva Urol Nefrol. 2010;62:29–40. [PubMed] [Google Scholar]
- 4.Vernon K, Peasegood J, Riddell A, Davenport A. Dialyzers designed to increase internal filtration do not result in significantly increased platelet activation and thrombin generation. Nephron Clin Pract. 2011;117:c403–c408. doi: 10.1159/000319884. [DOI] [PubMed] [Google Scholar]
- 5.Aoun B, Janssen-Lozinska Y, Ulinski T. Effect of vitamin E coated dialyzers on anticoagulation requirement in hemodialyzed children. Saudi J Kidney Dis Transpl. 2010;21:466–470. [PubMed] [Google Scholar]
- 6.Ouseph R, Ward RA. Anticoagulation for intermittent hemodialysis. Semin Dial. 2000;13:181–187. doi: 10.1046/j.1525-139X.2000.00052.x. [DOI] [PubMed] [Google Scholar]
- 7.Wilhelmsson S, Lins LE. Heparin elimination and hemostasis in hemodialysis. Clin Nephrol. 1984;22:303–306. [PubMed] [Google Scholar]
- 8.Davenport A. Anticoagulation options for pediatric hemodialysis. Hemodial Int. 2003;7:168–176. doi: 10.1046/j.1492-7535.2003.00022.x. [DOI] [PubMed] [Google Scholar]
- 9.Davenport A. Optimization of heparin anticoagulation for hemodialysis. Hemodial Int. 2011;15(Suppl 1):S43–S48. doi: 10.1111/j.1542-4758.2011.00601.x. [DOI] [PubMed] [Google Scholar]
- 10.Ouseph R, Ward RA. Improved dialyzer reuse after use of a population pharmacodynamic model to determine heparin doses. Am J Kidney Dis. 2000;35:89–94. doi: 10.1016/S0272-6386(00)70306-4. [DOI] [PubMed] [Google Scholar]
- 11.Brunet P, Simon N, Opris A, Faure V, Lorec-Penet AM, Portugal H, Dussol B, Berland Y. Pharmacodynamics of unfractionated heparin during and after a hemodialysis session. Am J Kidney Dis. 2008;51:789–795. doi: 10.1053/j.ajkd.2007.12.040. [DOI] [PubMed] [Google Scholar]
- 12.Charif R, Davenport A. Heparin-induced thrombocytopenia: an uncommon but serious complication of heparin use in renal replacement therapy. Hemodial Int. 2006;10:235–240. doi: 10.1111/j.1542-4758.2006.00101.x. [DOI] [PubMed] [Google Scholar]
- 13.Davenport A. Low-molecular-weight heparin as an alternative anticoagulant to unfractionated heparin for routine outpatient haemodialysis treatments. Nephrology. 2009;14:455–461. doi: 10.1111/j.1440-1797.2009.01135.x. [DOI] [PubMed] [Google Scholar]
- 14.Zhang W, Xiaonong Chen X, Chen Y, Chen N. Clinical experience with nadroparin in patients undergoing dialysis for renal impairment. Hemodial Int. 2011;15:379–384. doi: 10.1111/j.1542-4758.2011.00564.x. [DOI] [PubMed] [Google Scholar]
- 15.Davenport A. Low-molecular-weight heparin for routine hemodialysis. Hemodial Int. 2008;12(Suppl. 2):S34–S37. doi: 10.1111/j.1542-4758.2008.00322.x. [DOI] [PubMed] [Google Scholar]
- 16.Neuhaus TJ, Goetschel P, Schmugge M, Leumann E. Heparin-induced thrombocytopenia type II on hemodialysis: switch to danaparoid. Pediatr Nephrol. 2000;14:713–716. doi: 10.1007/PL00013423. [DOI] [PubMed] [Google Scholar]
- 17.Steinbach G, Bosc C, Caraman PL, Azoulay E, Olry L, D'Azemar P, Chopin J. Use in hemodialysis and hemofiltration of CY 216 (Fraxiparine) administered via intravenous bolus in patients with acute and chronic renal insufficiency with and without hemorrhagic risk. Nephrologie. 1990;11:17–21. [PubMed] [Google Scholar]
- 18.Sombolos KI, Fragia TK, Gionanlis LC, Veneti PE, Bamichas GI, Fragidis SK, Georgoulis IE, Natse TA. The anticoagulant activity of enoxaparin sodium during on-line hemodiafiltration and conventional hemodialysis. Hemodial Int. 2009;13:43–47. doi: 10.1111/j.1542-4758.2009.00336.x. [DOI] [PubMed] [Google Scholar]
- 19.Schlegel N, Mascher MA, Hurtaud MF, Maisin A, Bara L, Loirat C. The use of CY216 in paediatric hemodialysis. In: Breddin L, Fareed J, Samama M, editors. Fraxiparine, First International Symposium. Stuttgart New York: Schattauer; 1989. pp. 169–171. [Google Scholar]
- 20.Bianchetti MG, Speck S, Müller R, Oetliker OH. Simple coagulation prophylaxis using low-molecular heparin enoxaparin in pediatric haemodialysis. Schweiz Rundsch Med Prax. 1990;79:730–731. [PubMed] [Google Scholar]
- 21.Joannidis M, Kountchev J, Rauchenzauner M, Schusterschitz N, Ulmer H, Mayr A, Bellmann R. Enoxaparin vs. unfractionated heparin for anticoagulation during continuous veno-venous hemofiltration: a randomized controlled crossover study. Intensive Care Med. 2007;33:1571–1579. doi: 10.1007/s00134-007-0719-7. [DOI] [PubMed] [Google Scholar]
- 22.Greaves M, Control of Anticoagulation Subcommittee of the Scientific and Standardization Committee of the International Society of Thrombosis and Haemostasis Limitations of the laboratory monitoring of heparin therapy. Scientific and Standardization Committee Communications: on behalf of the Control of Anticoagulation Subcommittee of the Scientific and Standardization Committee of the International Society of Thrombosis and Haemostasis. Thromb Haemost. 2002;87:163–164. [PubMed] [Google Scholar]
- 23.Saltissi D, Morgan C, Westhuyzen J, Healy H. Comparison of low-molecular-weight heparin (enoxaparin sodium) and standard fractionated heparin for haemodialysis. Nephrol Dial Transplant. 1999;14:2698–2703. doi: 10.1093/ndt/14.11.2698. [DOI] [PubMed] [Google Scholar]
- 24.Seeherunvong W, Rubio L, Abitbol CL, Montané B, Strauss J, Diaz R, Zilleruelo G. Identification of poor responders to erythropoietin among children undergoing hemodialysis. J Pediatr. 2001;138:710–714. doi: 10.1067/mpd.2001.112246. [DOI] [PubMed] [Google Scholar]
- 25.Davenport A. Anticoagulation options for intermittent haemodialysis. Minerva Urol Nefrol. 2006;58:171–180. [PubMed] [Google Scholar]
- 26.Mujais SK, Chimeh H. Heparin free hemodialysis using heparin coated hemophan. ASAIO J. 1996;42:M538–M541. doi: 10.1097/00002480-199609000-00044. [DOI] [PubMed] [Google Scholar]
- 27.Otte KE, Jensen PB, Svendsen P, Gram J, Starklint H, Jørgensen KA. Heparin-free hypothermal hemodialysis at 20 degrees C improves biocompatibility. Blood Purif. 1997;15:200–207. doi: 10.1159/000170333. [DOI] [PubMed] [Google Scholar]
- 28.Geary DF, Gajaria M, Fryer-Keene S, Willumsen J. Low-dose and heparin-free hemodialysis in children. Pediatr Nephrol. 1991;5:220–224. doi: 10.1007/BF01095957. [DOI] [PubMed] [Google Scholar]
- 29.Evenepoel P, Dejagere T, Verhamme P, Claes K, Kuypers D, Bammens B, Vanrenterghem Y. Heparin-coated polyacrylonitrile membrane versus regional citrate anticoagulation: a prospective randomized study of 2 anticoagulation strategies in patients at risk of bleeding. Am J Kidney Dis. 2007;49:642–649. doi: 10.1053/j.ajkd.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 30.Chanard J, Lavaud S, Maheut H, Kazes I, Vitry F, Rieu P. The clinical evaluation of low-dose heparin in haemodialysis: a prospective study using the heparin-coated AN69 ST membrane. Nephrol Dial Transplant. 2008;23:2003–2009. doi: 10.1093/ndt/gfm888. [DOI] [PubMed] [Google Scholar]
- 31.Frank RD, Müller U, Lanzmich R, Groeger C, Floege J. Anticoagulant-free Genius haemodialysis using low molecular weight heparin-coated circuits. Nephrol Dial Transplant. 2006;21:1013–1018. doi: 10.1093/ndt/gfi293. [DOI] [PubMed] [Google Scholar]
- 32.Evenepoel P, Maes B, Vanwalleghem J, Kuypers D, Messiaen T, Vanrenterghem Y. Regional citrate anticoagulation for hemodialysis using a conventional calcium-containing dialysate. Am J Kidney Dis. 2002;39:315–323. doi: 10.1053/ajkd.2002.30551. [DOI] [PubMed] [Google Scholar]
- 33.Davenport A, Tolwani A. Citrate anticoagulation for continuous renal replacement therapy (CRRT) in patients with acute kidney injury admitted to the intensive care unit. Nephrol Dial Transplant Plus. 2009;2:439–447. doi: 10.1093/ndtplus/sfp136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kreuzer M, Ahlenstiel T, Kanzelmeyer N, Ehrich JH, Pape L. Management of regional citrate anticoagulation in pediatric high-flux dialysis: activated coagulation time versus post-filter ionized calcium. Pediatr Nephrol. 2010;25:1305–1310. doi: 10.1007/s00467-010-1483-4. [DOI] [PubMed] [Google Scholar]
- 35.Thijssen S, Kruse A, Raimann J, Bhalani V, Levin NW, Kotanko P. A mathematical model of regional citrate anticoagulation in hemodialysis. Blood Purif. 2005;29:197–203. doi: 10.1159/000245647. [DOI] [PubMed] [Google Scholar]
- 36.Apsner R, Buchmayer H, Gruber D, Sunder-Plassmann G. Citrate for long-term hemodialysis: prospective study of 1,009 consecutive high-flux treatments in 59 patients. Am J Kidney Dis. 2005;45:557–564. doi: 10.1053/j.ajkd.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 37.Kossman RJ, Gonzales A, Callan R, Ahmad S. Increased efficiency of hemodialysis with citrate dialysate: a prospective controlled study. Clin J Am Soc Nephrol. 2009;4:1459–1464. doi: 10.2215/CJN.02590409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hanevold C, Lu S, Yonekawa K. Utility of citrate dialysate in management of acute kidney injury in children. Hemodial Int. 2011;14(Suppl 1):S2–S6. doi: 10.1111/j.1542-4758.2010.00483.x. [DOI] [PubMed] [Google Scholar]
- 39.Davenport A. What are the options for anticoagulation needs in dialysis for patients with heparin-induced thrombocytopenia? Semin Dial. 2011;24:382–385. doi: 10.1111/j.1525-139X.2011.00916.x. [DOI] [PubMed] [Google Scholar]
- 40.Yang JW, Han BG, Kim BR, Lee YH, Kim YS, Yu JM, Choi SO. Superior outcome of nafamostat mesilate as an anticoagulant in patients undergoing maintenance hemodialysis with intracerebral hemorrhage. Ren Fail. 2009;31:668–675. doi: 10.3109/08860220903180616. [DOI] [PubMed] [Google Scholar]
- 41.Boccardo P, Melacini D, Rota S, Mecca G, Boletta A, Casiraghi F, Gianese F. Individualized anticoagulation with dermatan sulphate for haemodialysis in chronic renal failure. Nephrol Dial Transplant. 1997;12:2349–2354. doi: 10.1093/ndt/12.11.2349. [DOI] [PubMed] [Google Scholar]
- 42.Davenport A. Antibodies to heparin-platelet factor 4 complex: pathogenesis, epidemiology, and management of heparin-induced thrombocytopenia in hemodialysis. Am J Kidney Dis. 2009;54:361–374. doi: 10.1053/j.ajkd.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 43.Polkinghorne KR, McMahon LP, Becker GJ. Pharmacokinetic studies of dalteparin (Fragmin), enoxaparin (Clexane), and danaparoid sodium (Orgaran) in stable chronic hemodialysis patients. Am J Kidney Dis. 2002;40:990–995. doi: 10.1053/ajkd.2002.36331. [DOI] [PubMed] [Google Scholar]
- 44.Nagler M, Haslauer M, Wuillemin WA (2012) Fondaparinux – data on efficacy and safety in special circumstances. Thromb Res. doi:10.10161j.thrombres2011.10.037 [DOI] [PubMed]
- 45.Sharathkumar AA, Crandall C, Lin JJ, Pipe S. Treatment of thrombosis with fondaparinux (Arixtra) in a patient with end-stage renal disease receiving hemodialysis therapy. J Pediatr Hematol Oncol. 2007;29:581–584. doi: 10.1097/MPH.0b013e3181256ba5. [DOI] [PubMed] [Google Scholar]
- 46.Fischer KG. Essentials of anticoagulation in hemodialysis. Hemodial Int. 2007;11:178–189. doi: 10.1111/j.1542-4758.2007.00166.x. [DOI] [PubMed] [Google Scholar]
- 47.Benz K, Nauck MA, Böhler J, Fischer KG. Hemofiltration of recombinant hirudin by different hemodialyzer membranes: implications for clinical use. Clin J Am Soc Nephrol. 2007;2:470–476. doi: 10.2215/CJN.02550706. [DOI] [PubMed] [Google Scholar]
- 48.Hursting MJ, Dubb J, Verme-Gibboney CN. Argatroban anticoagulation in pediatric patients:a literature analysis. J Pediatr Hematol Oncol. 2006;28:4–10. doi: 10.1097/01.mph.0000195296.48319.38. [DOI] [PubMed] [Google Scholar]
- 49.Young G, Boshkov LK, Sullivan JE, Raffini LJ, Cox DS, Boyle DA, Kallender H, Tarka EA, Soffer J, Hursting MJ (2012) Argatroban therapy in pediatric patients requiring nonheparin anticoagulation: An open-label, safety, efficacy and pharmacokinetic study. Pediatr Blood Cancer. doi:10.1002/pbc.22852 [DOI] [PubMed]