Abstract
The bioenergetics of cancer cells is characterized by a high rate of aerobic glycolysis and suppression of mitochondrial metabolism (Warburg phenomenon). Mitochondrial metabolism requires inward and outward flux of hydrophilic metabolites, including ATP, ADP and respiratory substrates, through voltage-dependent anion channels (VDACs) in the mitochondrial outer membrane. Although VDACs were once considered to be constitutively open, closure of the VDAC is emerging as an adjustable limiter (governator) of mitochondrial metabolism. Studies of VDACs reconstituted into planar lipid bilayers show that tubulin at nanomolar concentrations decreases VDAC conductance. In tumor cell lines, microtubule-destabilizing agents increase cytoplasmic free tubulin and decrease mitochondrial membrane potential (ΔΨm), whereas microtubule stabilization increases ΔΨm. Tubulin-dependent suppression of ΔΨm is further potentiated by protein kinase A activation and glycogen synthase kinase-3β inhibition. Knockdown of different VDAC isoforms, especially of the least abundant isoform, VDAC3, also decreases ΔΨm, cellular ATP, and NADH/NAD+, suggesting that VDAC1 and VDAC2 are most inhibited by free tubulin. The brake on mitochondrial metabolism imposed by the VDAC governator probably is released when spindles form and free tubulin decreases as cells enter mitosis, which better provides for the high ATP demands of chromosome separation and cytokinesis. In conclusion, tubulin-dependent closure of VDACs represents a new mechanism contributing to the suppression of mitochondrial metabolism in the Warburg phenomenon.
Introduction
Seminal work by Otto Warburg in the 1920s on respiration and fermentation (conversion of glucose to lactic acid) in tumors led to his conclusion that cancer cells “ferment” substantially more glucose into lactate than nontumor cells even in the presence of physiological levels of oxygen (Warburg et al., 1927). Warburg (1956) further postulated that mitochondrial respiration and oxidative phosphorylation in cancer cells are “damaged,” leading to a compensatory increase of glycolysis. Aerobic glycolysis and suppression of mitochondrial metabolism, the two principal components of the Warburg phenomenon, remain hallmarks of cancer metabolism (Gatenby and Gillies, 2004; Ward and Thompson, 2012). Although molecular biological approaches have largely dominated cancer research in recent years, a resurgence of interest in the Warburg phenomenon has once again highlighted the importance of adaptations of intermediary metabolism to overall cancer cell biology (Ward and Thompson, 2012). Nonetheless, mechanisms causing suppression of mitochondrial metabolism in the Warburg effect remain poorly understood.
Warburg Phenomenon
Aerobic Glycolysis in Tumor Cells.
Most differentiated, nonproliferating cells aerobically metabolize glucose to pyruvate, which is then oxidized in the mitochondrial matrix by the tricarboxylic acid cycle to yield CO2 and NADH with minimal production of lactate. In general, 95% of total ATP in differentiated cells is produced by mitochondrial oxidative phosphorylation with the remaining 5% generated by aerobic glycolysis. In contrast, in cancer cells glycolytic rates and lactate production are high even in the presence of adequate oxygenation (Gambhir, 2002). The relative contribution of aerobic glycolysis to ATP formation in cancer cells is estimated to be 50 to 70% of total ATP (Bustamante and Pedersen, 1977; Vander Heiden et al., 2009).
Enhancement of Glycolysis in Proliferating Cells.
To support a high rate of aerobic glycolysis, cancer cells up-regulate enzymes and transporters associated with uptake and catabolism of glucose, including plasmalemmal glucose transporters (e.g., glucose transporter-1), hexokinase-II, pyruvate kinase M2, and lactate dehydrogenase (Bustamante et al., 1981; Geschwind et al., 2004; Pedersen, 2007; Christofk et al., 2008; Vander Heiden et al., 2011), but the advantage of aerobic glycolysis for tumor cells remains a matter of conjecture. In terms of ATP generation, one mole of glucose generates ∼36 mol of ATP when oxidized completely in mitochondria, whereas metabolism of one mole of glucose to lactate by glycolysis generates only 2 mol of ATP. However, the lower ATP yield of glycolysis compared with mitochondrial oxidative phosphorylation is compensated at least in part by higher rates of glycolytic flux (Harvey et al., 2002).
Cell proliferation creates a high demand for amino acids, nucleotides, and lipids needed for biosynthesis of proteins, nucleic acids, and membranes. A possible reason for the switch to aerobic glycolysis by cancer cells is that glucose catabolism generates molecular precursors and NADPH via the pentose phosphate shunt for anabolic metabolism and reductive biosynthesis (Ward and Thompson, 2012). A preference for Warburg metabolism may be universal for rapidly proliferating eukaryotic cells. For example, when glucose and oxygen are both plentiful, growing yeast cultures prefer glucose fermentation (aerobic glycolysis) over oxidative phosphorylation. Only when glucose is no longer available do yeast convert to aerobic mitochondrial metabolism (diauxic shift), but growth rates become slower (Galdieri et al., 2010). Thus, aerobic glycolysis supports more rapid cell proliferation than aerobic oxidative phosphorylation and provides a growth advantage for both yeast and cancer cells.
Suppression of Mitochondrial Metabolism in Tumor Cells.
Warburg metabolism has two major components: increased aerobic glycolysis in the cytosol and suppression of oxidative phosphorylation in mitochondria. Many studies have identified pathways and enzymes up-regulating aerobic glycolysis, but the basis for suppression of mitochondrial function remains unclear, although some evidence suggests that mutations of mitochondrial DNA and enzymes of the tricarboxylic acid cycle contribute to the Warburg phenomenon (Chandra and Singh, 2011). Nonetheless, mitochondria isolated from tumor cells are fully functional to generate ATP and maintain a mitochondrial membrane potential (ΔΨm) (Pedersen, 2007). Thus, the question is how mitochondrial metabolism is suppressed in situ in cancer cells.
Voltage-Dependent Anion Channels
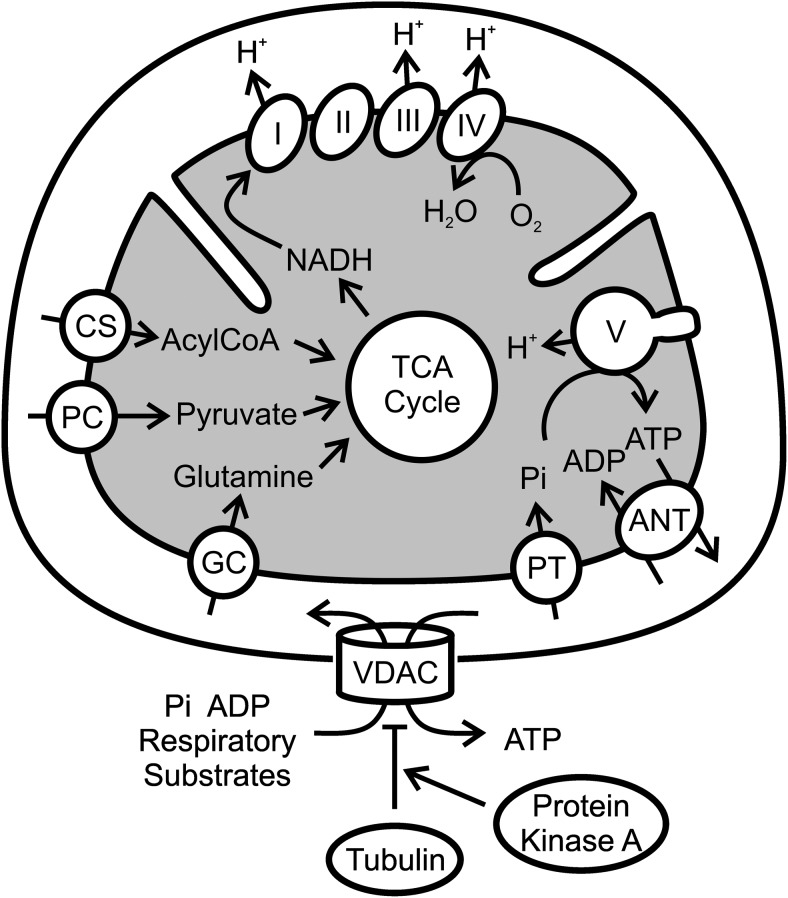
Mitochondrial metabolism requires inward and outward flux of hydrophilic, mostly anionic, metabolites, including ATP, ADP, Pi, and respiratory substrates such as pyruvate and fatty acyl-CoA. In the mitochondrial inner membrane (MIM), different specific carriers and shuttles facilitate fluxes of the individual metabolites, whereas in the mitochondrial outer membrane (MOM) movement of hydrophilic metabolites occurs through one known channel, the voltage-dependent anion channel (VDAC) (Fig. 1).
Fig. 1.
Scheme of the role of the voltage-dependent anion channel in tubulin-dependent suppression of mitochondrial metabolism. Respiratory substrates (e.g., fatty acids, pyruvate, and glutamine), ADP, and Pi move from the cytosol across the MOM into the intermembrane space (IMS) via the VDAC and across the MIM into the matrix via numerous individual transporters, including the adenine nucleotide transporter (ANT), the acylcarnitine transporter of the carnitine shuttle (CS), the pyruvate carrier (PC), the glutamine carrier (GC), and the phosphate transporter (PT). Respiratory substrates feed into the tricarboxylic acid (TCA) cycle, which generates mostly NADH. Transfer of reducing equivalents (electrons) from NADH to oxygen by complexes I to IV produces electrogenic proton translocation from the matrix into the IMS, generating a proton electrochemical gradient. Return of protons into the matrix drives ATP synthesis from ADP and Pi by the F1F0-ATP synthase (complex V). ATP then exchanges for ADP via ANT and subsequently moves through the VDAC into the cytosol. We propose that high free tubulin levels in proliferating cancer cells act to inhibit VDAC and cause global suppression of mitochondrial metabolism in the Warburg phenomenon. PKA through phosphorylation of VDAC sensitizes to inhibition by tubulin.
Originally discovered in mitochondrial membrane fractions from Paramecium aurelia, VDAC is a highly conserved protein found in the MOM from all eukaryotes studied (Sampson et al., 1997). In mice and humans, the VDAC has three isoforms, VDAC1, VDAC2, and VDAC3, of approximately 30 kDa. Each VDAC forms a barrel in the membrane with staves comprised of β-strands (Colombini, 2004). VDAC refolded from inclusion bodies forms 19-stranded β-barrels as analyzed by NMR and X-ray crystallography, although another model proposes that this three-dimensional structure is non-native and functional VDAC forms 13-stranded barrels (Bayrhuber et al., 2008; Hiller et al., 2008; Ujwal et al., 2008; Colombini, 2009).
Beyond discrepancies concerning the number of strands, the VDAC β-barrel encloses an aqueous channel of ∼2.5 nm in internal diameter surrounded by a wall of 1 nm. In the open state, the VDAC is permeable to nonelectrolyte solutes of molecular mass up to 5 kDa (Colombini, 1980; Colombini et al., 1987). Charged species of similar molecular mass, however, may face a greater energy barrier than uncharged molecules and be less permeant (Rostovtseva and Colombini, 1997; Rostovtseva et al., 2002; Colombini, 2004). Typical anionic metabolites involved in oxidative phosphorylation, most notably ATP and ADP, easily enter and exit mitochondria crossing the MOM through open VDACs.
In the open state at low positive or negative voltages (<10 mV), the VDAC favors anions over cations, but the selectivity is weak. At voltages more positive or negative than ± 40 mV, the VDAC decreases its permeability to anionic solutes. In this closed state, the VDAC becomes a cation selective pore of 1.8 nm in diameter, but closed VDAC still conducts small anionic electrolytes such as Cl− (Tan and Colombini, 2007). Because in the closed state the VDAC remains conductive to small electrolytes that collapse MOM potential, whether ΔΨm is a physiological regulator of the VDAC remains a matter of conjecture. A possibility is that Donnan potentials gate VDAC (Tan and Colombini, 2007). Donnan potentials form when impermeant charged species, mostly proteins, are asymetrically distributed across a membrane. The issue is controversial because charged macromolecules reside on both sides of the MOM, and high ionic strength of the intracellular milieu decreases the magnitude of any Donnan potentials forming. However, ΔpH measured across the outer membrane supports the existence of a Donnan potential of approximately −40 mV, which may be large enough to gate the VDAC (Porcelli et al., 2005). A variety of other factors also modulate VDAC conductance, including protein kinase A (PKA), hexokinase-I/II, bcl2 family members, glycogen synthase 3β (GSK3β), NADH, acetaldehyde, and free tubulin (Lee et al., 1994; Vander Heiden et al., 2000, 2001; Azoulay-Zohar et al., 2004; Rostovtseva et al., 2004; Das et al., 2008; Holmuhamedov et al., 2012). Regardless of mechanism, if VDAC closure were to occur, then inward and outward flux of anionic metabolites would be curbed, leading to overall suppression of mitochondrial metabolism (Fig. 1).
Mitochondrial Metabolism in Cancer Cells
Mitochondrial Membrane Potential and Free Tubulin.
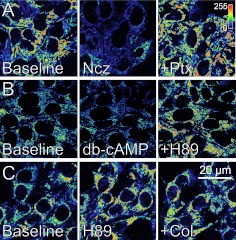
In tumor cells, both mitochondrial respiration and mitochondrial hydrolysis of ATP derived from glycolysis can maintain ΔΨm across the MIM (Maldonado et al., 2010). Respiration and mitochondrial hydrolysis of glycolytic ATP require flux of metabolites into mitochondria through the VDAC. In human tumor cells loaded with tetramethylrhodamine methylester (TMRM) to monitor ΔΨm, microtubule destabilizers such as rotenone (also a complex I inhibitor), colchicine, and nocodazole increase free tubulin and decrease ΔΨm (Fig. 2A). In contrast, microtubule stabilization with paclitaxel decreases free tubulin and increases ΔΨm (Maldonado et al., 2010) (Fig. 2B). Because electrophysiological studies show that heterodimeric free tubulin at nanomolar concentrations closes VDACs reconstituted into planar phospholipid bilayers (Rostovtseva et al., 2008), in situ studies showing the effects of microtubule polymerization and depolymerization on ΔΨm suggest strongly that free tubulin is promoting VDAC closure in living cancer cells as well (Fig. 1). Free tubulin also inhibits mitochondrial metabolism in isolated brain mitochondria and permeabilized synaptosomes and cardiac myocytes, which is consistent with tubulin-dependent inhibition of VDAC activity (Timohhina et al., 2009).
Fig. 2.
Effect of free tubulin and protein kinase A on mitochondrial membrane potential in HepG2 cells. A, nocodazole (Ncz; 10 μM), a microtubule-depolymerizing agent that increases free tubulin, decreased ΔΨm in HepG2 human hepatoma cells, as shown by decreased fluorescence (visualized in pseudocolor) of the ΔΨm indicator TMRM. Paclitaxel (Ptx; 10 μM), a microtubule stabilizer that decreases free tubulin, blocked depolarization induced by nocodazole and instead promoted hyperpolarization (increase of TMRM fluorescence). B, activation of PKA with dibutyryl-cAMP (db-cAMP, 2 mM) decreased ΔΨm, as shown by decreased TMRM fluorescence. Subsequent addition of H89 (1 μM), a PKA inhibitor, reversed the depolarizing effect of db-cAMP and promoted mitochondrial hyperpolarization. C, PKA inhibition with H89 hyperpolarized mitochondria and prevented tubulin-induced depolarization after colchicine (Col; 10 μM), another microtubule-destabilizing agent. Additions in B and C were approximately 20 min apart.
In HepG2 human hepatoma cells, PKA activation with dibutyryl-cAMP decreases ΔΨm, whereas the PKA inhibitor N-[2-[[3-(4-bromophenyl)-2-propenyl]amino]ethyl]-5-isoquinolinesulfonamide dihydrate dihydrochloride (H89) increases ΔΨm (Maldonado et al., 2010) (Fig. 2B). Conversely, inhibitors of GSK3β decrease ΔΨm, and VDAC2 phosphorylation by GSK3β seems to promote channel opening. PKA and GSK3β are serine/threonine kinases shown to phosphorylate the VDAC in vitro (Bera et al., 1995; Pastorino et al., 2002; Das et al., 2008). Phosphorylation also increases the sensitivity of VDACs reconstituted into planar lipid bilayers to inhibition by tubulin. VDAC phosphorylation increases the on rate of tubulin binding by up to two orders of magnitude without affecting other properties of the VDAC, including single-channel conductance and selectivity (Sheldon et al., 2011). In HepG2 cells, PKA inhibition both blocks and reverses depolarization induced by colchicine, showing that the inhibitory effect of free tubulin on ΔΨm is enhanced by PKA-mediated phosphorylation (Sheldon et al., 2011) (Fig. 2C). Future studies are needed to determine the precise sites of VDAC phosphorylation by PKA in situ that enhance tubulin binding.
These observations show that free tubulin dynamically regulates mitochondrial function in cancer cells, because ΔΨm is responsive to both increases and decreases of free tubulin. In contrast, in cultured hepatocytes ΔΨm decreases after microtubule depolymerization but does not increase after microtubule stabilization. Such results are consistent with the conclusion that free tubulin is an endogenous regulator of VDAC conductance and mitochondrial metabolism in cancer cells but not in nonproliferating differentiated cells such as aerobic hepatocytes. Thus, in cancer cells free tubulin may be acting as a brake to suppress mitochondrial metabolism by closing the VDAC, which contributes to the Warburg effect.
Role of Individual VDAC Isoforms in Regulating Mitochondrial Metabolism of Cancer Cells.
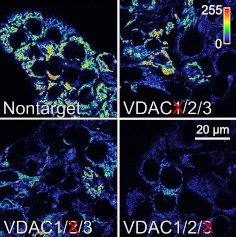
HepG2 cells express all three VDAC isoforms. Based on mRNA, the relative abundance of VDAC isoforms is VDAC2 ≈ VDAC1 > VDAC3 (Maldonado et al., 2011). To assess the role of individual VDAC isoforms in mitochondrial metabolism, HepG2 cells were treated with siRNAs against each VDAC isoform. Each siRNA decreased mRNA and protein expression for the corresponding isoform by 90% without affecting the remaining isoforms. Knockdown of VDAC1, VDAC2, and VDAC3 for 48 h also decreased ΔΨm by 42, 59, and 79%, respectively, compared with cells transfected with nontarget siRNA (Fig. 3). The drop of ΔΨm occurring after knocking down each isoform shows that all of the VDAC isoforms contribute to ΔΨm formation. It is noteworthy that knockdown of the least abundant isoform, VDAC3, caused the greatest drop in ΔΨm (Fig. 3). Thus, VDACs, especially VDAC3, are limiting for formation of ΔΨm. Indeed, VDAC3 knockdown, but not VDAC1 or VDAC2 knockdown, caused cellular ATP to decrease by 48%. Overall, these findings show that VDAC, especially VDAC3, contributes importantly to the control of mitochondrial metabolism in cancer cells (Maldonado et al., 2011).
Fig. 3.
VDAC knockdown decreases ΔΨm. siRNA knockdowns were performed against each of the three VDAC isoforms in HepG2 cells. ΔΨm assessed by TMRM fluorescence decreased after knockdown of each isoform. Knockdown of VDAC3 produced the greatest decrease of ΔΨm.
Why Tubulin?
If the VDAC is limiting oxidative phosphorylation in proliferating cells, why should tubulin have evolved to inhibit VDAC conductance and induce Warburg metabolism? Because rapidly dividing cells must prepare for spindle formation at mitosis, free tubulin is maintained at high levels during interphase compared with nonproliferating cells. HepG2 cells, for example, have a more than five times greater free-to-polymerized tubulin ratio than hepatocytes (Maldonado et al., 2010). In this respect, high free tubulin is a signature of cell proliferation. However, as spindle formation occurs during cell division, free tubulin will decrease. If free tubulin is inhibiting the VDAC, the decreased free tubulin will lead to VDAC opening and enhancement of mitochondrial metabolism. In this way, mitochondrial metabolism becomes activated to meet the high energy demand of chromosome separation and cytokinesis, but as cell division is completed and the spindle apparatus disappears, free tubulin should again increase to block the VDAC and favor the aerobic glycolysis of the Warburg phenomenon. In this way, naturally occurring fluctuations of free tubulin modulate in an appropriate way the bioenergetic metabolism of proliferating cells: during interphase, high free tubulin inhibits the VDAC and suppresses mitochondrial respiration to promote aerobic glycolysis and a maximal rate of biomass formation, whereas during cell division a decrease of free tubulin leads to the VDAC opening, activation of oxidative phosphorylation, and maximal generation of ATP just as it is most needed for chromosome movement and cytoplasmic division. However, empirical confirmation for this hypothetical chain of events during the cell cycle is still needed.
Conclusions and Future Prospects
The findings reviewed here support the conclusion that the VDAC is an adjustable limiter (governator) of mitochondrial metabolism whose partial closure acts as a brake suppressing mitochondrial metabolism so that proliferating cancer cells can use glucose optimally to generate biomass, namely formation of proteins, nucleic acids, and membranes. Tubulin and protein kinases, especially PKA activation, act to inhibit VDAC conductance and may account in large part for suppression of mitochondrial oxidative phosphorylation in the Warburg phenomenon. However, the brake on mitochondrial metabolism imposed by the VDAC governator probably is released when free tubulin decreases as cells enter mitosis to better provide for the high energy needs for chromosome separation and cytokinesis. If our view is correct, then the VDAC governator acts to turn mitochondrial metabolism on and off to match the varying metabolic needs of proliferating cells as cell growth advances to cell division. The VDAC governator hypothesis also has implications for the development of new chemotherapeutic agents, and drugs disrupting VDAC-tubulin interactions might antagonize Warburg metabolism and promote a nonproliferative cellular phenotype. Identification of such drugs is a goal of ongoing studies.
This work was supported, in part, by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases [Grants DK073336, DK37034]. E.N.M. is a recipient of a Specialized Program of Research Excellence Career Development Award [Grant P50 CA058187]. Imaging facilities for this research were supported, in part, by the Hollings Cancer Center, Medical University of South Carolina [Grant P30 CA138313].
Article, publication date, and citation information can be found at http://jpet.aspetjournals.org.
- ΔΨm
- mitochondrial membrane potential
- MIM
- mitochondrial inner membrane
- MOM
- mitochondrial outer membrane
- VDAC
- voltage-dependent anion channel
- PKA
- protein kinase A
- GSK3β
- glycogen synthase kinase-3β
- TMRM
- tetramethylrhodamine methylester
- siRNA
- short interfering RNA
- ANT
- adenine nucleotide transporter
- db-cAMP
- dibutyryl-cAMP
- H89
- N-[2-[[3-(4-bromophenyl)-2-propenyl]amino]ethyl]-5-isoquinolinesulfonamide dihydrate dihydrochloride.
Authorship Contributions
Wrote or contributed to the writing of the manuscript: Maldonado and Lemasters.
References
- Azoulay-Zohar H, Israelson A, Abu-Hamad S, Shoshan-Barmatz V. (2004) In self-defence: hexokinase promotes voltage-dependent anion channel closure and prevents mitochondria-mediated apoptotic cell death. Biochem J 377:347–355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayrhuber M, Meins T, Habeck M, Becker S, Giller K, Villinger S, Vonrhein C, Griesinger C, Zweckstetter M, Zeth K. (2008) Structure of the human voltage-dependent anion channel. Proc Natl Acad Sci U S A 105:15370–15375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bera AK, Ghosh S, Das S. (1995) Mitochondrial VDAC can be phosphorylated by cyclic AMP-dependent protein kinase. Biochem Biophys Res Commun 209:213–217 [DOI] [PubMed] [Google Scholar]
- Bustamante E, Morris HP, Pedersen PL. (1981) Energy metabolism of tumor cells. Requirement for a form of hexokinase with a propensity for mitochondrial binding. J Biol Chem 256:8699–8704 [PubMed] [Google Scholar]
- Bustamante E, Pedersen PL. (1977) High aerobic glycolysis of rat hepatoma cells in culture: role of mitochondrial hexokinase. Proc Natl Acad Sci U S A 74:3735–3739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra D, Singh KK. (2011) Genetic insights into OXPHOS defect and its role in cancer. Biochim Biophys Acta 1807:620–625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christofk HR, Vander Heiden MG, Harris MH, Ramanathan A, Gerszten RE, Wei R, Fleming MD, Schreiber SL, Cantley LC. (2008) The M2 splice isoform of pyruvate kinase is important for cancer metabolism and tumour growth. Nature 452:230–233 [DOI] [PubMed] [Google Scholar]
- Colombini M. (1980) Structure and mode of action of a voltage dependent anion-selective channel (VDAC) located in the outer mitochondrial membrane. Ann NY Acad Sci 341:552–563 [DOI] [PubMed] [Google Scholar]
- Colombini M. (2004) VDAC: the channel at the interface between mitochondria and the cytosol. Mol Cell Biochem 256–257:107–115 [DOI] [PubMed] [Google Scholar]
- Colombini M. (2009) The published 3D structure of the VDAC channel: native or not? Trends Biochem Sci 34:382–389 [DOI] [PubMed] [Google Scholar]
- Colombini M, Yeung CL, Tung J, König T. (1987) The mitochondrial outer membrane channel, VDAC, is regulated by a synthetic polyanion. Biochim Biophys Acta 905:279–286 [DOI] [PubMed] [Google Scholar]
- Das S, Wong R, Rajapakse N, Murphy E, Steenbergen C. (2008) Glycogen synthase kinase 3 inhibition slows mitochondrial adenine nucleotide transport and regulates voltage-dependent anion channel phosphorylation. Circ Res 103:983–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galdieri L, Mehrotra S, Yu S, Vancura A. (2010) Transcriptional regulation in yeast during diauxic shift and stationary phase. OMICS 14:629–638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambhir SS. (2002) Molecular imaging of cancer with positron emission tomography. Nat Rev Cancer 2:683–693 [DOI] [PubMed] [Google Scholar]
- Gatenby RA, Gillies RJ. (2004) Why do cancers have high aerobic glycolysis? Nat Rev Cancer 4:891–899 [DOI] [PubMed] [Google Scholar]
- Geschwind JF, Georgiades CS, Ko YH, Pedersen PL. (2004) Recently elucidated energy catabolism pathways provide opportunities for novel treatments in hepatocellular carcinoma. Expert Rev Anticancer Ther 4:449–457 [DOI] [PubMed] [Google Scholar]
- Harvey AJ, Kind KL, Thompson JG. (2002) REDOX regulation of early embryo development. Reproduction 123:479–486 [DOI] [PubMed] [Google Scholar]
- Hiller S, Garces RG, Malia TJ, Orekhov VY, Colombini M, Wagner G. (2008) Solution structure of the integral human membrane protein VDAC-1 in detergent micelles. Science 321:1206–1210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmuhamedov EL, Czerny C, Beeson CC, Lemasters JJ. (2012) Ethanol suppresses ureagenesis in rat hepatocytes: role of acetaldehyde. J Biol Chem 287:7692–7700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee AC, Zizi M, Colombini M. (1994) β-NADH decreases the permeability of the mitochondrial outer membrane to ADP by a factor of 6. J Biol Chem 269:30974–30980 [PubMed] [Google Scholar]
- Maldonado EN, DeHart DN, Patnaik JR, Lemasters JJ. (2011) The voltage-dependent anion channel regulates mitochondrial function in HepG2 cells. Hepatology 54:763A [Google Scholar]
- Maldonado EN, Patnaik J, Mullins MR, Lemasters JJ. (2010) Free tubulin modulates mitochondrial membrane potential in cancer cells. Cancer Res 70:10192–10201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pastorino JG, Shulga N, Hoek JB. (2002) Mitochondrial binding of hexokinase II inhibits Bax-induced cytochrome c release and apoptosis. J Biol Chem 277:7610–7618 [DOI] [PubMed] [Google Scholar]
- Pedersen PL. (2007) Warburg, me and Hexokinase 2: Multiple discoveries of key molecular events underlying one of cancers' most common phenotypes, the “Warburg Effect”, i.e., elevated glycolysis in the presence of oxygen. J Bioenerg Biomembr 39:211–222 [DOI] [PubMed] [Google Scholar]
- Porcelli AM, Ghelli A, Zanna C, Pinton P, Rizzuto R, Rugolo M. (2005) pH difference across the outer mitochondrial membrane measured with a green fluorescent protein mutant. Biochem Biophys Res Commun 326:799–804 [DOI] [PubMed] [Google Scholar]
- Rostovtseva T, Colombini M. (1997) VDAC channels mediate and gate the flow of ATP: implications for the regulation of mitochondrial function. Biophys J 72:1954–1962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rostovtseva TK, Antonsson B, Suzuki M, Youle RJ, Colombini M, Bezrukov SM. (2004) Bid, but not Bax, regulates VDAC channels. J Biol Chem 279:13575–13583 [DOI] [PubMed] [Google Scholar]
- Rostovtseva TK, Komarov A, Bezrukov SM, Colombini M. (2002) VDAC channels differentiate between natural metabolites and synthetic molecules. J Membr Biol 187:147–156 [DOI] [PubMed] [Google Scholar]
- Rostovtseva TK, Sheldon KL, Hassanzadeh E, Monge C, Saks V, Bezrukov SM, Sackett DL. (2008) Tubulin binding blocks mitochondrial voltage-dependent anion channel and regulates respiration. Proc Natl Acad Sci U S A 105:18746–18751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson MJ, Lovell RS, Craigen WJ. (1997) The murine voltage-dependent anion channel gene family. Conserved structure and function. J Biol Chem 272:18966–18973 [DOI] [PubMed] [Google Scholar]
- Sheldon KL, Maldonado EN, Lemasters JJ, Rostovtseva TK, Bezrukov SM. (2011) Phosphorylation of voltage-dependent anion channel by serine/threonine kinases governs its interaction with tubulin. PLoS One 6:e25539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan W, Colombini M. (2007) VDAC closure increases calcium ion flux. Biochim Biophys Acta 1768:2510–2515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timohhina N, Guzun R, Tepp K, Monge C, Varikmaa M, Vija H, Sikk P, Kaambre T, Sackett D, Saks V. (2009) Direct measurement of energy fluxes from mitochondria into cytoplasm in permeabilized cardiac cells in situ: some evidence for mitochondrial interactosome. J Bioenerg Biomembr 41:259–275 [DOI] [PubMed] [Google Scholar]
- Ujwal R, Cascio D, Colletier JP, Faham S, Zhang J, Toro L, Ping P, Abramson J. (2008) The crystal structure of mouse VDAC1 at 2.3 A resolution reveals mechanistic insights into metabolite gating. Proc Natl Acad Sci U S A 105:17742–17747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Heiden MG, Cantley LC, Thompson CB. (2009) Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science 324:1029–1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Heiden MG, Chandel NS, Li XX, Schumacker PT, Colombini M, Thompson CB. (2000) Outer mitochondrial membrane permeability can regulate coupled respiration and cell survival. Proc Natl Acad Sci U S A 97:4666–4671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Heiden MG, Li XX, Gottleib E, Hill RB, Thompson CB, Colombini M. (2001) Bcl-xL promotes the open configuration of the voltage-dependent anion channel and metabolite passage through the outer mitochondrial membrane. J Biol Chem 276:19414–19419 [DOI] [PubMed] [Google Scholar]
- Vander Heiden MG, Lunt SY, Dayton TL, Fiske BP, Israelsen WJ, Mattaini KR, Vokes NI, Stephanopoulos G, Cantley LC, Metallo CM, et al. (2011) Metabolic pathway alterations that support cell proliferation. Cold Spring Harb Symp Quant Biol 76:325–334 [DOI] [PubMed] [Google Scholar]
- Warburg O. (1956) On the origin of cancer cells. Science 123:309–314 [DOI] [PubMed] [Google Scholar]
- Warburg O, Wind F, Negelein E. (1927) The metabolism of tumors in the body. J Gen Physiol 8:519–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward PS, Thompson CB. (2012) Metabolic reprogramming: a cancer hallmark even Warburg did not anticipate. Cancer Cell 21:297–308 [DOI] [PMC free article] [PubMed] [Google Scholar]