Abstract
Atypical Lipomatous Tumor/Well Differentiated Liposarcoma (ALT/WDLS) is a soft tissue sarcoma of intermediate malignant behavior, most frequently affecting the retroperitoneum and lower extremities. Oral liposarcomas are very rare neoplasms, the most common histological subtype being ALT/WDLS. In this study, three additional cases of ALT/WDLS located on the tongue (2 cases) and the lower lip (1 case), respectively, are described. Analysis of the salient clinicopathologic features of 63 oral ALT/WDLS cases previously reported in the English language literature, as well as of the 3 cases presented in this study, indicates that the indolent biologic behavior of this tumor justifies its designation as a locally spreading malignant neoplasm, affording a rather conservative surgical approach.
Keywords: Atypical lipoma, Liposarcoma, Oral neoplasms, Soft tissue sarcoma
Introduction
Liposarcoma accounts for approximately 20% of all soft tissue malignancies, representing the most common type of sarcoma in adults [1, 2]. It usually involves the deep soft tissues of the trunk and lower extremities, in particular the retroperitoneum, thighs, and buttocks [2]. Liposarcomas are classified into several subtypes including: Atypical Lipomatous Tumor/Well-Differentiated Liposarcoma (ALT/WDLS), which is further subdivided morphologically into lipoma-like, sclerosing, inflammatory, and spindle cell variants; Dedifferentiated; Myxoid/Round-cell; Pleomorphic; and Mixed-type liposarcoma [3]. ALT/WDLS is the most common subtype of liposarcoma (40-45% of cases), arising usually in the retroperitoneum and thighs of middle-aged adults [3].
The concept of ALT was first introduced by Evans et al. [4] in 1979, who suggested that well differentiated liposarcomas of the subcutis and extremities show a more favorable clinical and biologic behavior compared to their retroperitoneal counterparts, and should be designated accordingly as atypical lipomas and atypical intramuscular lipomas. As the authors emphasized, although these tumors share a great tendency for local recurrence they do not metastasize unless dedifferentiation with development of a high-grade sarcomatous component occurs, thus radical surgical treatment should be avoided. The term atypical lipomatous tumor (ALT) was also advocated by Evans [5] in 1988, to describe both atypical lipomas and retroperitoneal tumors without lipoblasts. Subsequently, the term has been applied to lipomatous neoplasms with minimal nuclear atypia and few or no lipoblasts, regardless of location [1], while in the latest WHO classification (2002) the combined term ALT/WDLS is reserved for liposarcomas arising in surgically amenable locations, that despite their infiltrative growth pattern and locally aggressive behavior they do not tend to recur after complete surgical removal [3].
Clinical, morphological, and cytogenetic findings provide adequate evidence that ALT and WDLS are identical and both terms should be used synonymously [1, 6]. The theory of ALT/WDLS has gained acceptance, although issues like variations in diagnostic microscopic features and the relationship of the neoplasm to spindle-cell and pleomorphic lipoma have not been settled [1].
Liposarcomas of the head and neck are rare, representing 2–8% of all sarcomas in this region [7]. Oral liposarcomas show a much lower incidence, as relevant reviews have reported a limited number of documented cases [8–11]. In a review of head and neck liposarcomas between 1911 and 2005, approximately 46% of cases (36/78) were localized in the oral mucosa [11], while oral and salivary gland liposarcomas accounted for only 0.3% (18/5,435) of all liposarcomas diagnosed in the Armed Forces Institute of Pathology between 1970 and 2000 [8].
Although ALT/WDLS is the most common type of liposarcoma of the oral mucosa [1, 8–10, 12], pertinent data are limited because most relevant publications have been in the form of either single case reports or small case series. In this study, three additional cases of oral ALT/WDLS are described and a review of the reported oral ALT/WDLS cases in the English language literature is also presented.
Case Reports
Case 1
A 62-year-old female patient presented with an asymptomatic, slowly enlarging tongue lesion, first noticed approximately 1 year ago. Her medical history was non-contributory.
Clinical examination revealed a submucosal swelling covered by normal mucosa at the left dorso-lateral border of the tongue. The lesion measured approximately 1 × 1 cm and on palpation was firm, circumscribed and painless. The rest of the oral mucosa was normal and no palpable neck lymph nodes were found. The differential diagnosis included benign tumors of mesenchymal origin, e.g. lipoma, neurofibroma, granular cell tumor, and surgical excision under local anesthesia was performed. The post-operative course of the patient was uneventful with no sign of recurrence 5 years after the excision.
Case 2
A 36-year-old otherwise healthy female was referred for management of an asymptomatic nodule located on her lower lip. The lesion had emerged 2 months previously after “a bite” in the area, as reported by the patient. Her medical history was non-contributory.
Clinically, a well-circumscribed submucosal mass measuring approximately 0.8 × 0.5 cm was present on her lower left lip. On palpation, the lesion was elastic and non-tender, while the overlying mucosa was normal. No cervical lymphadenopathy was found. With a provisional diagnosis of an “organized mucocele” the patient underwent complete surgical removal. The post surgical course was uneventful with no evidence of recurrence 2 years after the excision.
Case 3
A 70-year-old female patient presented with a slowly growing tongue tumor of 4-years duration. The patient was under treatment for osteoporosis, hypothyroidism, and hypercholesterolemia.
Clinically, a 1.5 × 1.5 cm, asymptomatic, firm, submucosal mass covered by normal mucosa was present on the right side of the anterior third of the tongue. The rest of the oral mucosa was normal and no regional lymphadenopathy was noted. The differential diagnosis included benign mesenchymal tumors and an excisional biopsy was performed. Upon histopathologic examination, infiltration of the surgical margins by neoplastic adipocytes was noted and a re-excision with a 0.5 cm wide clear resection margin was performed. Healing was uneventful and there has been no recurrence 18 months after surgery.
Pathologic Description
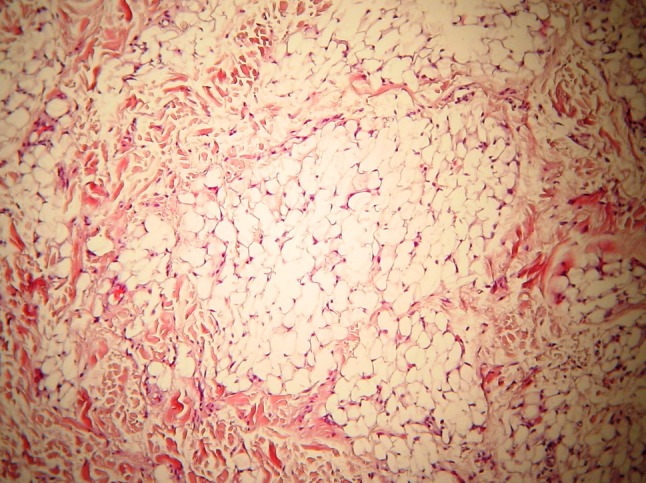
Microscopic examination of formalin-fixed, paraffin-embedded tissue sections showed in all 3 cases an unencapsulated but circumscribed neoplasm with lobules separated by thin fibrous septae (Fig. 1). It was composed of mature adipocytes of variable size and shape (Fig. 2), intermixed with cytologically bland spindle cells (Fig. 3). Numerous multivacuolated lipoblasts with pleomorphic or hyperchromatic nuclei (Fig. 4a), some with a signet-ring appearance (Fig. 4b), were present. In Case 1, rare mitoses (<1 per 10 high power microscopic fields) were recognized (Fig. 4c). Focal infiltration of adjacent small vessels and nerves (Fig. 5), or muscle fibers (Fig. 6) was noted, but necrosis or hemorrhage were absent. Immunohistochemically, neoplastic adipocytes reacted positively with S-100 protein and vimentin. Histopathogic features were consistent with the diagnosis of lipoma-like ALT/WDLS in all cases. The surgical margins in Cases 1 and 2, and the re-excision in Case 3, were negative for tumor.
Fig. 1.
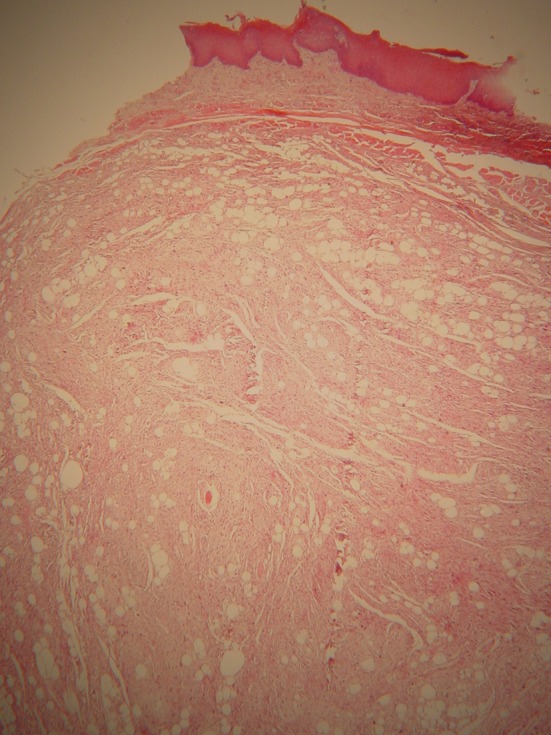
Case 1. An unencapsulated but circumscribed cellular mass (hematoxylin-eosin, original magnification ×25)
Fig. 2.
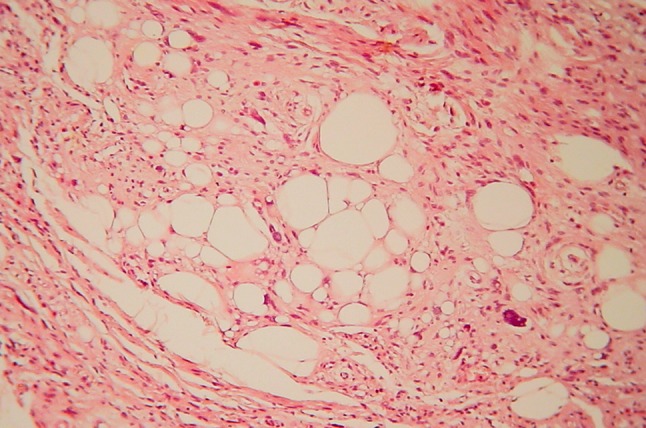
Case 1. Mature adipocytes of variable size and shape in a fibrous stroma (hematoxylin-eosin, original magnification ×100)
Fig. 3.
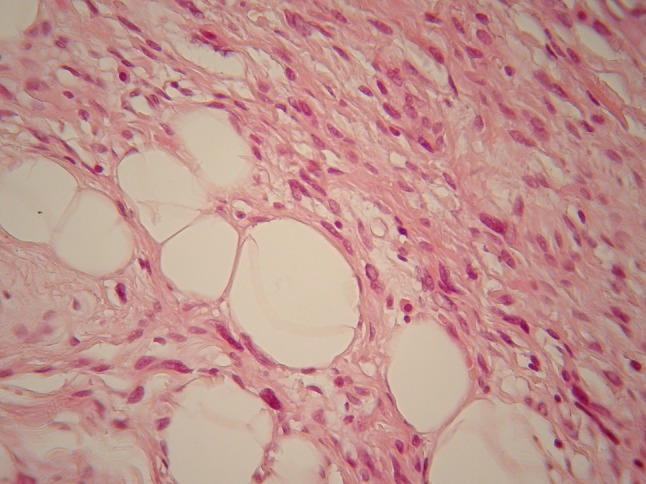
Case 1. Adipocytes intermixed with cytologically bland spindle cells (hematoxylin-eosin, original magnification ×100)
Fig. 4.
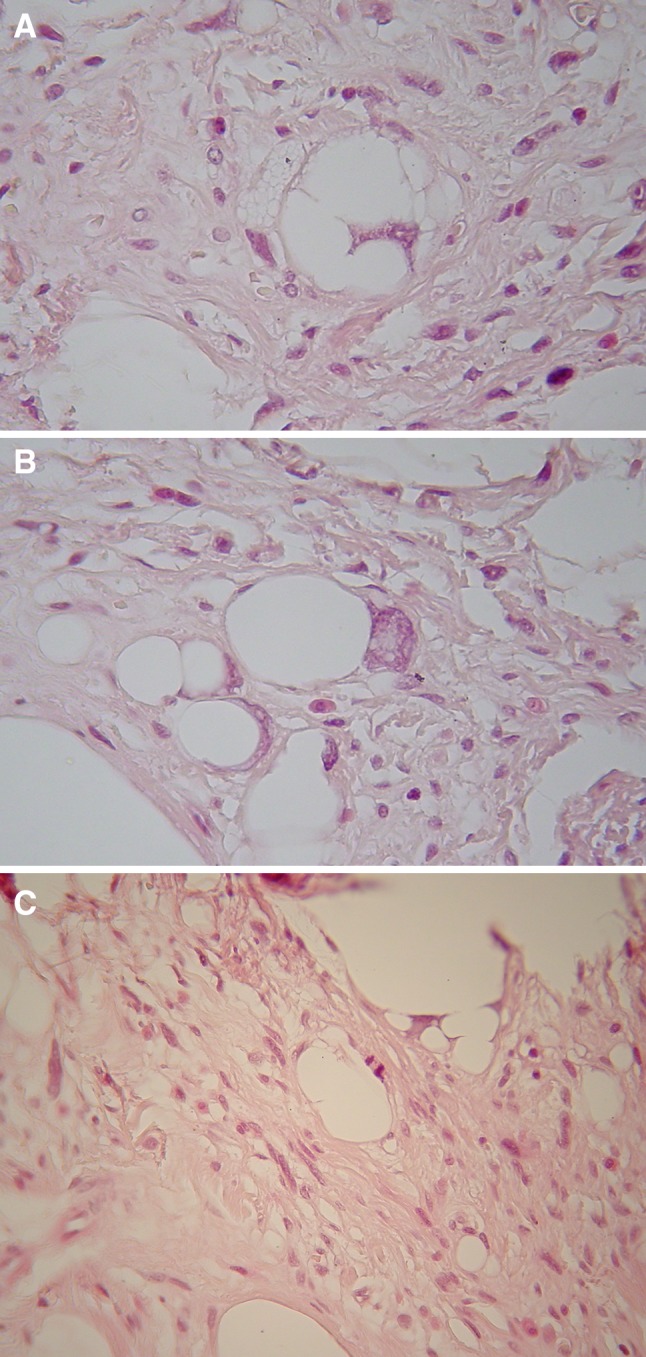
a Case 3. Lipoblasts with marked nuclear pleomorphism and vacuolated cytoplasm. b Case 3. Signet-ring cells. c Case 1. A rare mitotic figure (hematoxylin-eosin, original magnification ×400)
Fig. 5.
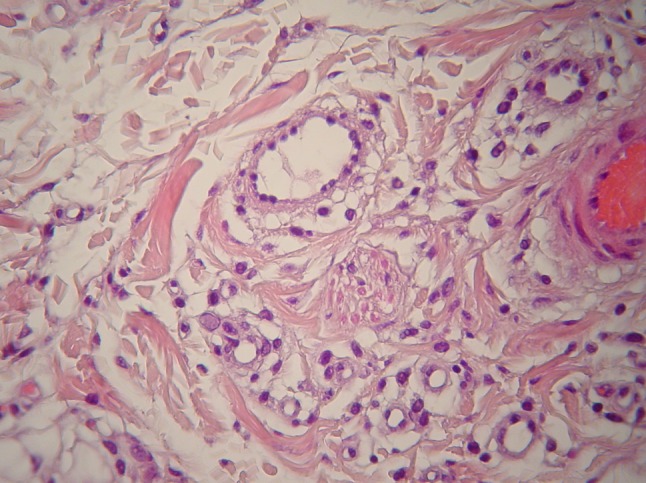
Case 2. Small vessel and nerve infiltration by neoplastic adipocytes (hematoxylin-eosin, original magnification ×100)
Fig. 6.
Case 3. Infiltration of adjacent muscle fibers by neoplastic adipocytes (hematoxylin-eosin, original magnification ×100)
Discussion
A Pubmed search of the English language literature up to July 2011 disclosed 63 cases of ALT/WDLS with a definite oral location. Age, gender, tumor size and location, histologic subtype, treatment modalities, and follow-up data of these 63 cases as well as of the 3 cases presented herein, comprising a total of 66 cases, are summarized in Table 1 [8–10, 12–39]. Five cases described previously as myxoid WDLS were excluded, since they most probably represented myxoid liposarcomas [40]. Case 4 of Nascimento et al. [12] and case 1 of Allon et al. [36] had been previously reported by other authors [10, 12] and as such they were only counted once. Additionally, case 1 of Minic [41] was excluded because it is more consistent with an extraoral location, as were the two cases (1 buccal and 1 lip) from the series of Davis et al. [7], since pertinent information was not given. Four cases described as ALT with dedifferentiation [12] were analyzed separately (Table 2), in order to compare their characteristics with those of the typical ALT.
Table 1.
Clinicopathological features of 66 cases of oral ALT/WDLS
| Author | No | Age/gender | Size (greatest dimension in cm) | Location | Diagnosis | Follow-up (in months) |
|---|---|---|---|---|---|---|
| Henefer et al. [34] | 1 | 39/M | 7.5 | Buccal mucosa | WDLS | 18 NED |
| Larson et al. [35] | 2 | 42/F | 1.5 | Tongue (ventral) | WDLS | N/A |
| Saunders et al. [36] | 3 | 31/M | 5 | Soft palate | WDLS, sclerosing | 18 NED |
| Yamada et al. (31) | 4 | 51/F | 12 | Buccal mucosa | WDLS | 12 |
| Sadeghi and Sauk [18] | 5 | 42/F | 5.2 | Buccal mucosa | WDLS | – |
| Suzuki et al. [37] | 6 | 0.5/M | 4.5 | Buccal mucosa | WDLS | 36 NED |
| Charnock et al. [38] | 7 | 63/M | 3 | Buccal mucosa | WDLS | 24 NED |
| Ruacan et al. [39] | 8 | 32/M | 3 | Buccal mucosa | WDLS | 10 NED |
| Nakahara et al. [40] | 9 | 48/F | 2.2 | Floor of the mouth | WDLS with a myxoid variant | 12 NED |
| Lucas et al. [41] | 10 | −/− | – | Buccal mucosa | WDLS | N/A |
| Kacker and Taskin [42] | 11 | 78/M | 6.0 | Tongue (lateral) | Atypical lipoma | N/A |
| Saddik et al. [32] | 12 | 76/M | 2.5 | Tongue (base/tonsillar fossa) | WDLS | 4 recurrences in 23 years |
| Senyuva et al. [43] | 13 | 71/M | 7.9 | Buccal mucosa | WDLS, sclerosing | 12 NED |
| Kamikaidou et al. [23] | 14 | 60/F | 5 | Buccal mucosa | WDLS | 1 recurrence at 9 months as myxoid liposarcoma |
| Nelson et al. [25] | 15 | 37/M | 3.0 | Tongue (anterior dorsolateral/ventral) | WDLS or atypical lipoma | 18 NED |
| Orita et al. [33] | 16 | 70/M | 3.5 | Tongue (lateral) | WDLS, lipoma-like | 8 NED |
| Gagari et al. [10] | 17 | 73/M | 2.0 | Tongue (anterior dorsolateral) | WDLS, lipoma-like | LFU |
| Nikitakis et al. [11] | 18 | 28/M | 4 | Buccal mucosa | WDLS | 17 NED |
| Moore et al. [44] | 19 | 43/M | 0.8 | Tongue (anterior dorsolateral) | Atypical lipoma | 10 NED |
| Nunes et al. [45] | 20 | 65/M | 1.0 | Tongue (anterior dorsal) | WDLS | 18 NED |
| Nascimento et al. [12] | 21 | 36/M | 0.6 | Tongue | WDLS, adipocytic (ALT) | 108 NED |
| 22 | 48/F | 3 | n/a | WDLS, adipocytic (ALT) | N/A | |
| 23 | 50/M | 1.2 | Tongue | WDLS, adipocytic (ALT) | 48 NED | |
| 24 | 47/F | 2.2 | Tongue | WDLS, adipocytic (ALT) | 16 NED | |
| 25 | 74/M | – | Tongue | WDLS, adipocytic (ALT) | 4 recurrences in 17 months | |
| 26 | 77/F | 0.6 | Tongue | WDLS, adipocytic (ALT) | 20 NED | |
| 27 | 43/M | 1.0 | Tongue | WDLS, adipocytic (ALT) | 11 NED | |
| 28 | 45/M | 1.5 | Gingiva | WDLS, adipocytic (ALT) | 24 NED | |
| 29 | 72/M | 0.7 | Tongue | WDLS, adipocytic with heterologous cartilage (ALT) | 24 NED | |
| 30 | −/− | – | Buccal mucosa | WDLS, adipocytic with spindle cell features (ALT) | N/A | |
| 31 | 80/M | 1.0 | Tongue | WDLS, adipocytic with spindle cell features (ALT) | 2 NED, then LFU | |
| 32 | 35/F | 4 | Floor of the mouth | WDLS, adipocytic with spindle cell features (ALT) | 25 NED | |
| 33 | 49/F | 3 | Buccal mucosa | WDLS, adipocytic with spindle cell features (ALT) | 24 NED | |
| 34 | 51/F | 0.9 | Lip | WDLS, adipocytic with spindle cell features (ALT) | 3 NED, then LFU | |
| 35 | 53/M | 0.8 | Tongue | WDLS, adipocytic with spindle cell features (ALT) | 2 NED, then LFU | |
| 36 | 47/M | 6 | Buccal mucosa | WDLS, adipocytic with spindle cell features (ALT) | Multiple recurrences in 7 years | |
| 37 | 28/F | 2 | Lip | WDLS, adipocytic with spindle cell features (ALT) | 9 NED, then LFU | |
| 38 | 55/F | 1 | Soft palate | WDLS, adipocytic with spindle cell features (ALT) | N/A | |
| Fanburg-Smith et al. [9] | 39 | 36/F | 6 | Palate | WDLS, slerosing | LFU |
| 40 | 41/M | – | Buccal mucosa | WDLS | 276 NED | |
| 41 | 43/F | 2.0 | Tongue (lateral) | WDLS | 24 NED | |
| 42 | 52/M | 5.5 | Mandibular soft tissues | WDLS | 192 NED | |
| 43 | 64/F | 1.5 | Tongue | WDLS | 192 NED | |
| 44 | 67/F | 6 | Buccal mucosa | WDLS | 180 NED, 2 recurrences at 4 and 5 years | |
| 45 | 69/M | – | Buccal mucosa | WDLS, focal myxoid features | LFU | |
| 46 | 70/M | 2.1 | Buccal mucosa | Atypical lipoma, sclerosing | 144 NED | |
| Hattori [46] | 47 | 81/M | 1.2 | Lower lip | ALT/WDLS | LFU |
| Capodiferro et al. [47] | 48 | 58/F | 2.5 | Tongue (lateral) | WDLS | 24 NED |
| Angeles et al. [48] | 49 | 86/M | 0.5 | Tongue (anterior/middle lateral) | ALT | N/A |
| Allon et al. [18] | 50 | 68/F | 1 | Tongue | ALT | 12 NED |
| 51 | 72/M | 0.7 | Tongue | ALT | 12 NED | |
| 52 | 57/M | 2 | Tongue | ALT | 12 NED | |
| Chan et al. [49] | 53 | 58/M | 1 | Anterior mandibular alveolus | WDLS, lipoma like | 12 NED |
| DeWitt et al. [21] | 54 | 58/F | 0.6 | Tongue (lateral) | WDLS/ALT | 18 NED |
| 55 | 62/F | 0.7 | Tongue (lateral) | WDLS/ALT | 12 NED | |
| Paragis Sanchez et al. [50] | 56 | 36/F | – | Tongue | WDLS/ALT | N/A |
| Laco et al. [24] | 57 | 78/F | 1.1 | Tongue (lateral) | ALT, lipoma like | 63 NED |
| 58 | 27/F | 0,7 | Tongue (lateral) | ALT, lipoma like | 58 NED | |
| 59 | 65/M | 2 | Tongue (multiple nodules, bilaterally) | ALT, lipoma like | Recurrence at 59 months | |
| 60 | 11/M | 0,8 | Tongue (lateral) | ALT, sclerosing | N/A | |
| 61 | 75/M | 1 | Tongue (lateral) | ALT, sclerosing | 159 NED | |
| 62 | 50/F | 1.2 | Tongue (lateral) | ALT, lipoma like | 4 NED | |
| Moritani [51] | 63 | 68/M | 1.3 | Tongue (lateral) | ALT | 36 NED |
| Present report | 64 | 62/F | 1.0 | Tongue (anterior lateral) | ALT-lipoma like | 60 NED |
| 65 | 36/F | 0.8 | Lower lip | ALT-lipoma like | 24 NED | |
| 66 | 70/F | 1.5 | Tongue (anterior lateral) | ALT-lipoma like | 18 NED |
F female, M male, N/A not available, NED no evidence of disease, LFU lost to follow-up
Table 2.
Clinicopathological features of 4 cases of oral ALT/WDLS with dedifferentiation reported in the English literature
| Author | No | Age/gender | Size (greatest dimension in cm) | Location | Diagnosis | Follow-up (in months) |
|---|---|---|---|---|---|---|
| Da Cuhna et al. [26] | 1 | 42/F | 1 | Gingival sulcus | WDLS with angiosarcomatous dedifferentiation | 12 NED |
| Nascimento et al. [12] | 2 | 29/M | 5 | Buccal mucosa | WDLS, adipocytic (ALT), “incipient” dedifferentiation | 5 NED, then LFU |
| Nascimento et al. [12] | 3 | 83/F | 2.5 | Tongue | WDLS, adipocytic with dedifferentiation (non-lipogenic, round cells) | N/A |
| Nascimento et al. [12] | 4 | 49/F | 8 | Floor of the mouth | WDLS, adipocytic with spindle cell features (ALT), “incipient” dedifferentiation | 66 NED |
F female, M male, N/A not available, NED no evidence of disease, LFU lost to follow-up
According to available data in 64/66 cases, 37 patients (57.8%) were males and 27 females (male-to-female ratio approximately 1.37:1). As has been shown in previous studies, head and neck liposarcomas [7, 12] and intraoral liposarcomas [8–10] show a male predominance, in contrast to the reported female predilection for ALT/WDLS’s of various locations [1, 6, 42]. The mean age of 64 patients with available information was 54.05 ± 17.84 years (age range 6 months to 86 years; median 54 years), with 78.1% of patients (50/64) being ≥40 years-old. This finding is in accordance with the previously reported mean age at diagnosis for intraoral liposarcomas, regardless of histologic subtype [9, 38].
Oral liposarcomas have been reported to occur mainly on the buccal mucosa [8–10, 38, 43], but in the largest case series of ALT’s, tongue was the favorite site of involvement [12]. In the present review, 36 out of 65 cases (55.38%) of oral ALT/WDLS were located on the tongue, with exactly 50% of lesions situated on the lateral border (18/36 cases), followed by the buccal mucosa (17 cases), the lips (4 cases), the gingiva/gingival sulcus (3 cases), the palate (3 cases) and the floor of the mouth (2 cases).
Oral ALT/WDLS usually appears as a circumscribed, slowly enlarging, painless, submucosal mass that may be present for several months or even years before being excised. Rare cases of bilateral or multinodular ALT/WDLS of the tongue have also been reported [22, 27, 36]. The tumor is generally asymptomatic and patients usually become aware of its presence, only when it reaches a size large enough to cause cosmetic or functional problems [10]. Superficial location may account for the small size at the time of diagnosis. In 60 lesions, the maximum diameter ranged from 0.5 to 12 cm, with a mean diameter of 3.31 ± 2.64 cm. The indolent growth and small size of the ALT may justify the usual provisional clinical diagnosis of an irritation fibroma or a benign mesenchymal neoplasm [2, 28, 41]. A provisional diagnosis of either a reactive or benign tumor or a cystic lesion was rendered in all three cases of our series.
Microscopically, lipoma-like was the most common histopathologic subtype, while 10 cases showed a spindle cell component, 6 displayed sclerosing areas, 2 focal myxoid changes, and 1 heterologous cartilage formation.
Four cases of ALT with dedifferentiation have been reported in the English literature (Table 2) [12, 44]. The mean age of patients was 50.75 ± 23.04 (age range 29 months to 83 years; median 45.5 years), while 3/4 were females. The tumors were located one each on the tongue, floor of the mouth, buccal mucosa, and gingival sulcus, while their mean diameter was 4.6 ± 3.51 cm (range 1–8 cm). In all 4 cases, dedifferentiation was observed during initial histopathologic diagnosis and in 2/4 cases was described as “incipient”, characterized by small areas of increased cellularity with focal pleomorphism [45]. This finding is possibly consistent with the reported potential of gradual dedifferentiation in some cases of ALT/WDLS’s, although the prognostic significance of small foci of dedifferentiation remains undetermined [46]. The concept of low-grade dedifferentiation, consisting of fibroblastic areas with mild nuclear atypia, as a precursor lesion of high-grade dedifferentiation has also gained acceptance, although no differences regarding the clinical outcome seem to exist between the two grades [46–48]. It is noteworthy that these cases of dedifferentiation reveal a younger median age, female preponderance, and a greater diameter compared to ALT/WDLS’s, although the number of cases is too small for conclusions. Prognostically, for an average of 27.6 months of follow-up, none of these cases was reported to recur or metastasize.
The histopathologic differential diagnosis of ALT/WDLS includes benign adipose tissue lesions, such as: the ordinary lipoma; spindle-cell, pleomorphic or chondroid lipoma; lipogranuloma; lipoblastoma; angiolipoma; fibrolipoma; hibernoma; and intramuscular lipoma [1, 2, 12, 22]. ALT/WDLS is usually well-circumscribed but unencapsulated, similar to an ordinary lipoma, while the presence of muscle infiltration may mimic the features of an intramuscular lipoma. Additionally, mitoses are rare and necrosis or hemorrhage are absent, while sclerosing ALT/WDLS may show extensive fibrosis simulating degenerative changes noted in lipomas. On the other hand, lipoblasts, varying from primitive mesenchymal cells with few, inconspicuous lipid droplets to signet ring cells with laterally displaced or indented nuclei, are only occasionally seen in ALT’s [2]. Interestingly, Fanburg-Smith et al. [8] have noticed that tongue ALT/WDLS contain more lipoblasts, compared to liposarcomas of other oral and extraoral sites. However, lipoblasts are not diagnostic of ALT/WDLS as they may be found in benign adipocytic lesions, such as lipoblastoma, pleomorphic lipoma, and chondroid lipoma [1, 8], while cells mimicking lipoblasts may be seen in spindle cell lipoma (“pseudo-lipoblasts”) [49] and various reactive conditions (“lipoblast-like cells”), such as fat necrosis and granulomatous foreign-body reactions (e.g. silicone granuloma) [50]. Careful inspection and extensive sampling allow the recognition of atypical cells with large, hyperchromatic and bizarre nuclei, as well as a great variation in cell size and shape, which are diagnostic for ALT/WDLS [12]. These findings and the presence of dense rather than wiry collagen fibers separating lobules of neoplastic cells [49] proved useful in Case 1 of the present study, where an abundance of spindle cells was strongly reminiscent of a spindle cell lipoma.
Immunohistochemistry is rather of minimal value in the diagnosis of ALT/WDLS [12]. Lipoblasts may be identified by S-100 protein positivity, while HMB-45 negativity may be of help in the differential diagnosis from angiomyolipoma [3]. CD34 immunostaining is also of limited use in cases of ALT resembling spindle cell lipoma, since CD34 positive ALT/WDLS’s have been reported [12, 49].
The histologic classification, as well as differential diagnosis, of liposarcomas may be facilitated by the recognition of distinct cytogenetic phenotypes [1, 51]. ALT/WDLS features ring or giant marker chromosomes, composed of DNA sequences derived from the 12q14–15 region. Overexpression of MDM2 (murine double minutes) nuclear phosphoprotein, CDK4 (cyclin-dependent kinase 4), and HMGI-C glycoprotein (High-mobility group protein isoform I–C), suggesting loss of control at the G1-S checkpoint, are frequently found in ALT/WDLS, and their prognostic value remains to be decided [42]. Immunohistochemical expression and amplification by FISH analysis of MDM2 and CDK4 have also been described in oral ALT/WDLS [22]. Myxoid and round cell liposarcomas show a characteristic t(12;16) translocation or, more rarely, a t(12;22) translocation, leading to the fusion of the transcription factor gene CHOP on 12q13 with the transcription factors TLS/FUS on chromosome 16p11 or EWS on chromosome 22, respectively. Complex rearrangements have also been identified in pleomorphic liposarcomas.
Wide surgical excision with free margins is usually curative for ALT/WDLS [4] and inadequate excision is considered the main reason for local recurrence, estimated at approximately 30% [1, 10]. Post-operative selective radiation may be of some benefit in certain cases, while the role of adjuvant chemotherapy has not been adequately evaluated [7, 41, 43].
Follow-up, ranging from 2 months to 23 years, was available in 52 out of 66 oral ALT/WDLS. Six tumors recurred (11.53%) within a mean time of 40 months, most of them many times during the follow-up period, but none was reported to metastasize. One tumor recurred as a myxoid liposarcoma [25, 52] while in another case of recurrent tumor situated in the base of the tongue, the diagnosis of ALT/WDLS was established after the last recurrence [25, 52]. As recurrence may develop many years after initial treatment, a continuous and close follow-up is necessary.
A better prognosis for liposarcomas of the head and neck has been associated with the superficial location, small size, and predominance of the ALT/WDLS variant [29, 41]. In general, superficially located liposarcomas behave in a rather benign manner, in contrast to deep-seated lesions, such as retroperitoneal or mesenteric liposarcomas. Most intraoral liposarcomas are usually superficial and well circumscribed, although they lack a true capsule and satellite nodules may be seen infiltrating adjacent tissues [9, 10]. A ≤5.0 cm maximum diameter is considered a favorable prognostic marker for oral liposarcomas [8]. ALT/WDLS and myxoid liposarcomas have a much better prognosis than the other histologic subtypes and they rarely metastasize [7, 10, 12, 43]. In contrast, round-cell, pleomorphic, and dedifferentiated liposarcomas show higher rates of recurrence and metastasis, particularly to the lungs, brain, spine, liver, pleura, and kidney [10, 29]. It should be noted though, that even in the three cases of oral ALT/WDLS with dedifferentiation and available follow-up data, no evidence of local recurrence or metastasis was reported.
In conclusion, most of the hitherto reported oral ALT/WDLS have been small-sized non-metastasizing tumors that have exhibited an excellent outcome after complete excision and a low recurrence rate. The clinicopathologic features, as well as the indolent biological behavior of oral WDLS’s, justify their designation as ALT; thus, conservative surgical excision with close follow-up rather than a radical surgical approach should be preferred and oral surgeons should be informed accordingly by the oral pathologist.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Dei Tos AP. Liposarcoma: new entities and evolving concepts. Ann Diagn Pathol. 2000;4:252–266. doi: 10.1053/adpa.2000.8133. [DOI] [PubMed] [Google Scholar]
- 2.Enzinger MF, Weiss SW. Liposarcoma. In: Weiss SW, Goldblum JR, editors. Soft tissue tumors. 4. St. Louis: Mosby; 2001. pp. 641–690. [Google Scholar]
- 3.Dei Tos AP, Pedeutour F. Atypical lipomatous tumour/well differentiated liposarcoma. In: Fletcher CDM, Unni KK, Mertens F, editors. Pathology and genetics of tumors of soft tissues and bone. Lyon: WHO Organization Classification of Tumours; 2002. pp. 35–37. [Google Scholar]
- 4.Evans HL, Soule EH, Winkelmann RK. Atypical lipoma, atypical intramuscular lipoma, and well differentiated retroperitoneal liposarcoma: a reappraisal of 30 cases formerly classified as well differentiated liposarcoma. Cancer. 1979;43:574–584. doi: 10.1002/1097-0142(197902)43:2<574::AID-CNCR2820430226>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 5.Evans HL. Liposarcoma and atypical lipomatous tumors: A study of 66 cases followed for a minimum of 10 years. Surg Pathol. 1988;1:41–54. [Google Scholar]
- 6.Rosai J, Akerman M, Dal Cin P, DeWever I, Fletcher CD, Mandahl N. Combined morphologic and karyotypic study of 59 atypical lipomatous tumors. Evaluation of their relationship and differential diagnosis with other adipose tissue tumors (a report of the CHAMP Study Group) Am J Surg Pathol. 1996;20:1182–1189. doi: 10.1097/00000478-199610000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Davis EC, Ballo MT, Luna MA, Patel SR, Roberts DB, Nong X, et al. Liposarcoma of the head and neck: The University of Texas M. D. Anderson Cancer Center experience. Head Neck. 2009;31:28–36. doi: 10.1002/hed.20923. [DOI] [PubMed] [Google Scholar]
- 8.Fanburg-Smith JC, Furlong MA, Childers EL. Liposarcoma of the oral and salivary gland region: a clinicopathologic study of 18 cases with emphasis on specific sites, morphologic subtypes, and clinical outcome. Mod Pathol. 2002;15:1020–1031. doi: 10.1097/01.MP.0000027625.79334.F5. [DOI] [PubMed] [Google Scholar]
- 9.Nikitakis NG, Lopes MA, Pazoki AE, Ord RA, Sauk JJ. MDM2 +/CDK4 +/p53 + oral liposarcoma: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:194–201. doi: 10.1067/moe.2001.116815. [DOI] [PubMed] [Google Scholar]
- 10.Gagari E, Kabani S, Gallagher GT. Intraoral liposarcoma: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:66–72. doi: 10.1016/S1079-2104(00)80016-5. [DOI] [PubMed] [Google Scholar]
- 11.Sobral AP. de Oliveira Lima DN, Cazal C, Santiago T, das Gracas Granja Mattos M, Melo B, et al. Myxoid liposarcoma of the lip: correlation of histological and cytological features and review of the literature. J Oral Maxillofac Surg. 2007;65:1660–1664. doi: 10.1016/j.joms.2006.06.264. [DOI] [PubMed] [Google Scholar]
- 12.Nascimento AF, McMenamin ME, Fletcher CD. Liposarcomas/atypical lipomatous tumors of the oral cavity: a clinicopathologic study of 23 cases. Ann Diagn Pathol. 2002;6:83–93. doi: 10.1053/adpa.2002.32375. [DOI] [PubMed] [Google Scholar]
- 13.Henefer EP, Borghesani EP, Sacks FR. Lipsarcoma of the cheek. J Oral Surg. 1976;34:1039–1043. [PubMed] [Google Scholar]
- 14.Larson DL, Cohn AM, Estrada RG. Liposarcoma of the tongue. J Otolaryngol. 1976;5:410–414. [PubMed] [Google Scholar]
- 15.Saunders JR, Jaques DA, Casterline PF, Percarpio B, Goodloe S., Jr Liposarcomas of the head and neck: a review of the literature and addition of four cases. Cancer. 1979;43:162–168. doi: 10.1002/1097-0142(197901)43:1<162::AID-CNCR2820430124>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 16.Yamada K, Dohara Y, Nagata M, Kawashima K, Yamashita S. A case of liposarcoma of the cheek. Jap J Clin Oncol. 1979;9:123–130. [Google Scholar]
- 17.Sadeghi EM, Sauk JJ., Jr Liposarcoma of the oral cavity. Clinical, tissue culture, and ultrastructure study of a case. J Oral Pathol. 1982;11:263–275. doi: 10.1111/j.1600-0714.1982.tb00166.x. [DOI] [PubMed] [Google Scholar]
- 18.Suzuki H, Nagayama M, Kaneda T, Oka T. Liposarcoma of the cheek in an infant. J Oral Maxillofac Surg. 1984;42:180–184. doi: 10.1016/S0278-2391(84)80030-0. [DOI] [PubMed] [Google Scholar]
- 19.Charnock DR, Jett T, Heise G, Taylor R. Liposarcoma arising in the cheek: report of a case and review of the literature. J Oral Maxillofac Surg. 1991;49:298–300. doi: 10.1016/0278-2391(91)90225-B. [DOI] [PubMed] [Google Scholar]
- 20.Ruacan S, Onerci M, Gedikoglu G, Dal T. Liposarcoma of the cheek: report of a case. J Oral Pathol Med. 1993;22:46–47. doi: 10.1111/j.1600-0714.1993.tb00119.x. [DOI] [PubMed] [Google Scholar]
- 21.Nakahara H, Shirasuna K, Terada K. Liposarcoma of the floor of the mouth: a case report. J Oral Maxillofac Surg. 1994;52:1322–1324. doi: 10.1016/0278-2391(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 22.Laco J, Mentzel T, Hornychova H, Kohout A, Jirousek Z, Ryska A. Atypical lipomatous tumors of the tongue: report of six cases. Virchows Arch. 2009;455:383–388. doi: 10.1007/s00428-009-0835-6. [DOI] [PubMed] [Google Scholar]
- 23.Lucas DR, Nascimento AG, Sanjay BK, Rock MG. Well-differentiated liposarcoma. The Mayo Clinic experience with 58 cases. Am J Clin Pathol. 1994;102:677–683. doi: 10.1093/ajcp/102.5.677. [DOI] [PubMed] [Google Scholar]
- 24.Kacker A, Taskin M. Atypical intramuscular lipoma of the tongue. J Laryngol Otol. 1996;110:189–191. doi: 10.1017/S0022215100133146. [DOI] [PubMed] [Google Scholar]
- 25.Saddik M, Oldring DJ, Mourad WA. Liposarcoma of the base of tongue and tonsillar fossa: A possibly underdiagnosed neoplasm. Arch Pathol Lab Med. 1996;120:292–295. [PubMed] [Google Scholar]
- 26.Senyuva C, Yucel A, Okur I, Dervisoglu S. A well-differentiated giant liposarcoma originating from the buccal fat pad. Ann Plast Surg. 1996;37:439–443. doi: 10.1097/00000637-199610000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Kamikaidou N, Kirita T, Mishima K, Sugimura M. Liposarcoma of the cheek: report of a case. J Oral Maxillofac Surg. 1998;56:662–665. doi: 10.1016/S0278-2391(98)90469-4. [DOI] [PubMed] [Google Scholar]
- 28.Nelson W, Chuprevich T, Galbraith DA. Enlarging tongue mass. J Oral Maxillofac Surg. 1998;56:224–227. doi: 10.1016/S0278-2391(98)90873-4. [DOI] [PubMed] [Google Scholar]
- 29.Orita Y, Nishizaki K, Ogawara T, Yamadori I, Yorizane S, Akagi H, et al. Liposarcoma of the tongue: case report and literature update. Ann Otol Rhinol Laryngol. 2000;109:683–686. doi: 10.1177/000348940010900713. [DOI] [PubMed] [Google Scholar]
- 30.Moritani N, Yamada T, Mizobuchi K, Wakimoto M, Ikeya Y, Matsumura T, et al. Atypical lipomatous tumor of the tongue: report of a case. Acta Med Okayama. 2010;64:257–261. doi: 10.18926/AMO/40134. [DOI] [PubMed] [Google Scholar]
- 31.Moore PL, Goede A, Phillips DE, Carr R. Atypical lipoma of the tongue. J Laryngol Otol. 2001;115:859–861. doi: 10.1258/0022215011909198. [DOI] [PubMed] [Google Scholar]
- 32.Nunes FD, Loducca SV, Oliveira EM, Araujo VC. Well-differentiated liposarcoma of the tongue. Oral Oncol. 2002;38:117–119. doi: 10.1016/S1368-8375(01)00030-6. [DOI] [PubMed] [Google Scholar]
- 33.Hattori H. Atypical lipomatous tumor of the lip with pleomorphic lipoma-like myxoid area, clinically simulating mucocele. J Oral Pathol Med. 2002;31:561–564. doi: 10.1034/j.1600-0714.2002.00151.x. [DOI] [PubMed] [Google Scholar]
- 34.Capodiferro S, Scully C, Maiorano E. Lo Muzio L, Favia G. Liposarcoma circumscriptum (lipoma-like) of the tongue: report of a case. Oral Dis. 2004;10:398–400. doi: 10.1111/j.1601-0825.2004.01040.x. [DOI] [PubMed] [Google Scholar]
- 35.Angeles RM, Vasquez J, Kim O. Pathologic quiz case: an 86-year-old man with a painless right tongue mass. Atypical lipomatous tumor of the tongue. Arch Pathol Lab Med. 2005;129:253–254. doi: 10.5858/2005-129-253-PQCAYM. [DOI] [PubMed] [Google Scholar]
- 36.Allon I, Vered M, Dayan D. Liposarcoma of the tongue: clinico-pathologic correlations of a possible underdiagnosed entity. Oral Oncol. 2005;41:657–665. doi: 10.1016/j.oraloncology.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 37.Chan WY, McHenry ID, Carter LM, Reall G, Wales CJ. Gingival liposarcoma: an unusual polyp. Br J Oral Maxillofac Surg. 2008;46:150–151. doi: 10.1016/j.bjoms.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 38.DeWitt J, Heidelman J, Summerlin DJ, Tomich C. Atypical lipomatous tumors of the oral cavity: a report of 2 cases. J Oral Maxillofac Surg. 2008;66:366–369. doi: 10.1016/j.joms.2006.10.035. [DOI] [PubMed] [Google Scholar]
- 39.Paragis Sanchez T, Bannwart C, Murilo Araujo D, Dos Santos Pinto D, Jr, Thome Capuano AC. Well-differentiated liposarcoma of the tongue. A case report. Minerva Stomatol. 2008;57:383–387. [PubMed] [Google Scholar]
- 40.Stout AP. Liposarcoma-the malignant tumor of lipoblasts. Ann Surg. 1944;119:86–107. [PMC free article] [PubMed] [Google Scholar]
- 41.Minic AJ. Liposarcomas of the oral tissues: a clinicopathologic study of four tumors. J Oral Pathol Med. 1995;24:180–184. doi: 10.1111/j.1600-0714.1995.tb01162.x. [DOI] [PubMed] [Google Scholar]
- 42.Dei Tos AP, Doglioni C, Piccinin S, Sciot R, Furlanetto A, Boiocchi M, et al. Coordinated expression and amplification of the MDM2, CDK4, and HMGI-C genes in atypical lipomatous tumours. J Pathol. 2000;190:531–536. doi: 10.1002/(SICI)1096-9896(200004)190:5<531::AID-PATH579>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 43.Fusetti M, Silvagni L, Eibenstein A, Chiti-Batelli S, Hueck S. Myxoid liposarcoma of the oral cavity: case report and review of the literature. Acta Otolaryngol. 2001;121:759–762. doi: 10.1080/00016480152583728. [DOI] [PubMed] [Google Scholar]
- 44.Cunha IW, Kowalski LP, Soares FA. Dedifferentiated liposarcoma of the oral cavity with angiosarcomatous dedifferentiation. Virchows Arch. 2005;446:456–459. doi: 10.1007/s00428-005-1207-5. [DOI] [PubMed] [Google Scholar]
- 45.Hudson C, Cove P, Adekeye EO. Liposarcoma of the head and neck: report of case and review of the literature. J Oral Surg. 1978;36:380–383. [PubMed] [Google Scholar]
- 46.Dei Tos AP, Pedeutour F. Dedifferentiated liposarcoma. In: Fletcher CDM, Unni KK, Mertens F, editors. Pathology and Genetics of tumors of soft tissues and bone. Lyon: WHO Organization Classification of Tumours; 2002. pp. 38–39. [Google Scholar]
- 47.Henricks WH, Chu YC, Goldblum JR, Weiss SW. Dedifferentiated liposarcoma: a clinicopathological analysis of 155 cases with a proposal for an expanded definition of dedifferentiation. Am J Surg Pathol. 1997;21:271–281. doi: 10.1097/00000478-199703000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Elgar F, Goldblum JR. Well-differentiated liposarcoma of the retroperitoneum: a clinicopathologic analysis of 20 cases, with particular attention to the extent of low-grade dedifferentiation. Mod Pathol. 1997;10:113–120. [PubMed] [Google Scholar]
- 49.Billings SD, Henley JD, Summerlin DJ, Vakili S, Tomich CE. Spindle cell lipoma of the oral cavity. Am J Dermatopathol. 2006;28:28–31. doi: 10.1097/01.dad.0000189615.13641.4b. [DOI] [PubMed] [Google Scholar]
- 50.Jham BC, Nikitakis NG, Scheper MA, Papadimitriou JC, Levy BA, Rivera H. Granulomatous foreign-body reaction involving oral and perioral tissues after injection of biomaterials: a series of 7 cases and review of the literature. J Oral Maxillofac Surg. 2009;67:280–285. doi: 10.1016/j.joms.2008.01.052. [DOI] [PubMed] [Google Scholar]
- 51.Fletcher CD, Akerman M. Dal Cin P, de Wever I, Mandahl N, Mertens F, et al. Correlation between clinicopathological features and karyotype in lipomatous tumors. A report of 178 cases from the Chromosomes and Morphology (CHAMP) Collaborative Study Group. Am J Pathol. 1996;148:623–630. [PMC free article] [PubMed] [Google Scholar]
- 52.Wescott WB, Correll RW. Multiple recurrences of a lesion at the base of the tongue. J Am Dent Assoc. 1984;108:231–232. doi: 10.14219/jada.archive.1984.0450. [DOI] [PubMed] [Google Scholar]


