Abstract
This study examined associations between mother–infant nighttime interactions and mother–infant attachment when infants were 12 months old. Forty-four mother–infant pairs participated in this study. For three consecutive nights at home, babies were observed in their cribs using a digital video system. Mothers reported on their nighttime interactions with their babies using a self-report diary and completed a questionnaire regarding child temperament. Attachment was assessed in the Strange Situation (Ainsworth, Blehar, Waters, & Wall, 1978). Mothers of securely attached infants had nighttime interactions that were generally more consistent, sensitive and responsive than those of insecurely attached infants. Specifically, in secure dyads, mothers generally picked up and soothed infants when they fussed or cried after an awakening.
Keywords: maternal responsiveness, attachment, infants, nighttime, sleep
Introduction
Popular parenting literature (e.g., Ferber, 1985/2006), as well as many pediatricians and psychologists (e.g., Meltzer & Mindell, 2004), suggest that parents should teach babies to soothe themselves to sleep by not responding to their cries for attention. These recommendations are based on evidence that parental nighttime interactions (e.g., rocking, feeding, parental presence) initiate and maintain sleep problems (Adair, Bauchner, Philipp, Levenson, & Zuckerman, 1991; Morrell & Cortina-Borja, 2002; Van Tassel, 1985). Attachment theory, however, suggests that parents respond quickly and sensitively to infants’ signals (e.g., Ainsworth, Bell, & Stayton, 1974), thus appearing at odds with this contemporary advice regarding handling sleep issues. With several exceptions (Scher, 2001; Scher & Asher, 2004), attachment researchers have not addressed this issue of nighttime responsiveness directly, even though daytime responsiveness has been researched extensively. From an evolutionary perspective, nighttime is associated with a greater likelihood of threatening conditions than daytime (Bowlby, 1969/1982; Norluchi, Kikucki, & Senoo, 2007), thus making the study of the attachment system during nighttime interactions especially important. Given the emphasis in the popular literature on teaching infants to soothe themselves to sleep, even when it involves crying for progressively longer periods of time (Adair et al., 1991; Ferber, 1985/2006), this issue is critical. This study examined the association between mother–infant nighttime interactions and infant attachment security.
The most common sleep problems in early childhood are the inability to fall asleep alone (sleep onset problems) and problems resuming sleep alone after an awakening (night waking problems) (Gaylor, Goodlin-Jones, & Anders, 2001). However, there are no standard criteria or clear definitions for infant sleep problems (Goodlin-Jones, Burnham, & Anders, 2000; Tikotzky & Sadeh, 2001). The main criterion for determining a sleep problem is parental distress regarding infants who do not fall asleep without their parents’ help (Ferber, 1985/2006; Gaylor et al., 2001). Further, sleep experts have found that night waking is normal in young children (Goodlin-Jones et al., 2000; Sadeh, 2002; Scher & Asher, 2004) and that “all children wake periodically during the night between sleep cycles” (Ferber, 1985/2006, p. 62). Thus, the real issue is in understanding why some infants cry when they wake at night and how to respond to their cries. Ferber asserted that infants cry when they wake because they are frustrated to find that the conditions they have learned to associate with falling asleep (e.g., being rocked, held or patted) are no longer present and, therefore, they need to reestablish those conditions to fall back to sleep. He cautioned that repeatedly going in to comfort a child is “often not the best thing to do” and “may only be strengthening a habit, not responding to a real need” (Ferber, 1985/2006, p. 99). He advised that infants learn sleep associations that do not involve parental support or intervention, although he also conceded more recently that parents can do whatever they feel is best “as long as it works” (Ferber, 1985/2006, p. 41).
Attachment theory provides another possible explanation for the problem of infants who cry for their parents at night. Bowlby contends that children are biologically programmed to respond with fear to certain situations. Conditions such as being alone and in darkness elicit fear because they signal potential danger, regardless of the real danger. Fear-inducing situations activate the attachment system and children display attachment behaviors (e.g., crying, protesting separation, clinging when frightened) to gain proximity to caregivers (Bowlby, 1973). These are innate behaviors, not learned habits. Ainsworth et al. (1974) described infant behaviors (e.g., crying, demands for contact, and intolerance of separation) that serve a biological function but are inconvenient to caregivers. Nighttime waking, particularly when it involves crying and demands for contact, is an example of an aspect of early development that may be inconvenient to parents in developed cultures. Infants, even those who have grown accustomed to the parental expectation of transitioning to sleep alone, may be biologically predisposed to signal their distress to these separations.
Attachment and sleep
Several studies have examined associations between attachment and sleep problems or sleep–wake behavior. In a study of toddlers whose mothers received treatment for their children’s sleep problem, Benoit et al. (1992) found that 100% of the mothers of toddlers with sleep problems had non-autonomous states of mind with regard to attachment, compared to 57% of the control group. Morrell and Steele (2003), in a study of 14–16-month-olds with sleep problems, found that ambivalent attachment was associated with concurrent and persistent sleep problems. Seifer, Sameroff, Dickstein, Hayden, and Schiller (1996) found, in a sample of adults with emerging psychiatric disorders, insecurely attached 12-month-olds had more parent-reported night wakings than securely attached infants. Thus, clinical studies of infants and toddlers suggest that sleep problems are associated with insecure attachment.
By contrast, in studies with community samples of normal Israeli infants, attachment has not been associated with sleep problems or with objective night waking and sleep efficiency. In a study of 94 1-year-old infants, Scher (2001) found that attachment security, assessed with the Strange Situation, was not associated with parent-reported sleep problems or actigraphic measures of sleep efficiency and night waking. Similarly, Scher and Asher (2004) found that attachment security, assessed by the Attachment Q-Sort (Waters & Deane, 1985), was not associated with parent-reported sleep problems, bedtime settling strategies, or actigraphic measures of sleep efficiency and night waking in 12-month-olds. Thus, these studies failed to find support for the link between attachment and infant sleep. With the exception of Scher (2001) and Scher and Asher (2004), these studies relied on parent report rather than observational measures of sleep problems. Given that parents of children differing in attachment quality may differentially report child problems, it is critical that observational studies be conducted.
The present study
The purpose of this study was to investigate the associations between mother–infant nighttime interactions and mother–infant attachment security when infants were 12 months old. Unlike prior studies of attachment and sleep, this study used video observation of nighttime interaction rather than maternal report or actigraphic measures of infant sleep behavior. This methodology provides the opportunity to observe the quality of mother–infant interactions rather than relying upon frequency counts or durations of infant sleep behaviors, such as the number and length of awakenings.
Secure mother–infant dyads were expected to be characterized by more consistent, sensitive, and responsive maternal behavior during nighttime interactions than insecure dyads. According to attachment theory, the development of secure attachment results from experiences with an available, reliable and comforting caregiver (Ainsworth et al., 1978; Bowlby, 1969/1982). Infants in securely attached relationships were expected to signal clearly when they woke during the night. This hypothesis rests on the assumption that a history of responsive caregiving leads secure infants to expect that their needs will be met quickly and sensitively.
Method
Participants
Fifty-two 12-month-old infants were recruited into the study. Digital video observations were collected for 46 of the 52 infants. (The video recordings of two infants were lost due to technical errors and six infants were not videotaped at all because they either slept in the living room or in their parents’ room.) Analyses were conducted with the 44 infants (29 male) for whom video observations were available. Of this group, 36 were White (non-Hispanic), 4 were Asian-American, 3 were African-American, and 1 was Biracial. Twenty-seven were first born, 15 were second born, and 2 were fourth born. Thirty-nine infants were born full-term (37–41 weeks gestation), 3 were post-term (over 41 weeks gestation), and 2 were premature (less than 37 weeks gestation). Mean infant age at the time of the study was 12.8 months (Range 11–14 months; SD = .77).
Mothers’ age at the time of the study ranged from 24–44 years of age (Median = 32). Annual family income ranged from $40,000 (US$) to $200,000 (US$) (Median = $92,000). Fifteen mothers described themselves as homemakers, 14 were working full-time, 14 were working part-time, and 1 was a part-time student. Six mothers had a high school diploma, 3 had an associate’s degree, 19 had a college degree, 11 had a master’s degree, and 5 had a professional degree or a doctoral degree (see Table 1).
Table 1.
Maternal and infant characteristics.
| Characteristics | Min. | Max. | M | SD | % |
|---|---|---|---|---|---|
| Attachment classification (% secure) | 61 | ||||
| Infants’ gender (% male) | 66 | ||||
| Infants’ age at time of study (months) | 11.4 | 14.4 | 12.78 | .77 | |
| Ethnicity of infants (% Caucasian) | 82 | ||||
| Ethnicity of mothers (% Caucasian) | 82 | ||||
| Mothers’ age at time of study (years) | 24 | 44 | 32.61 | 4.60 | |
| Family income (US$) | 40,000 | 200,000 | 98,629 | 36,209 | |
| First born (%) | 61 | ||||
| Full-term (%) | 89 | ||||
| Mother as main weekday caregiver since birth (%) |
64 |
Most (57%) of the infants and their mothers were recruited by word of mouth, 14% were recruited from a university childcare center, 18% from mothers’ groups, 9% from a pediatric practice, and 2% from the workplace. Healthy, singleton infants and their married, English-speaking mothers were included. Mothers were required to be the primary caregivers at night, defined as providing at least 75% of the nighttime caregiving. Exclusion criteria included any evidence of abnormal pregnancy or delivery and chronic health problems in the mother or infant. Families were compensated $100 (US$) for their participation. Consent was obtained from all participating mothers.
Procedure
Data were collected in the home and in the laboratory when infants were between 11 and 14 months of age. For three consecutive nights, a video camera was placed next to the infant’s crib to record the infant’s night of sleep, including bedtime and night waking interactions. The video recordings were limited to events that took place while infants were in their cribs. The total number of hours of video observation collected for all the participants combined was 1273 with a minimum of 5 and a maximum of 38.5 hours per participant (Median 28.9). Mothers were asked to fill out a nighttime diary each morning and to= complete a demographic and temperament questionnaire in the home. After completing the nighttime observations and questionnaires at home, mothers and babies participated in the Strange Situation Procedure (Ainsworth et al., 1978) in the laboratory.
Measures
Description of digital video system
Objective data on nighttime interactions were obtained using a digital video system. Video/audio observations were recorded directly to a computer hard disk as digital media. The base of the system is a multi port video capture card which captured a separate audio track for each video track and gave the capture frame rate and level of video compression desired. The computer was a standard Dell desktop with 1 megabyte of ram and a 3 gigahertz processor. A desktop computer was used because the video capture card was not available for a laptop.
Using standard video coax cabling, two Sony color cameras designed for security and surveillance were connected to the capture card. These fixed focus, auto iris cameras are small, durable, cost effective, and have night vision capabilities with built-in infrared illuminators. Typically, one camera was mounted to a microphone stand next to the crib and the other was clamped onto a nearby shelf or piece of furniture. The single boundary microphone was connected to a small pre-amplifier allowing level control. The computer, microphone and amplifier were usually stored under the crib.
There are several advantages of this system. First, it allows for capturing an entire night without the use of time-lapse equipment and the video files can be watched in real-time. Second, no additional effort is required of the mothers because the system is activated each night by a pre-set timer to turn on each evening and turn off each morning. Third, the system is minimally disruptive to the baby’s sleep because it is quiet and adds no visible light to the room due to the infrared illuminators. Finally, the digital files (as opposed to videotape) provide a convenient way to view, code and archive the data.
Overview of coding system for mother–infant nighttime interactions
The first author, blind to infant attachment status, coded each of the video files by increasing the speed of the video/audio to 16 times normal speed during the times that the infant appeared to be asleep and watching the events of interest (i.e., bedtime and night wakings) at normal speed. The following information was recorded at bedtime: time in crib, whether put in crib awake or asleep, and whether infant cried in crib before falling asleep. The following information was recorded for each awakening: time awake, confidence that infant is awake, whether and how infant vocalizes, who responds to the awakening, latency to respond to crying, and how the infant is put back to sleep. A distinction was made between infants who vocalized and those who signaled distress during an awakening. A vocalization was defined as any sound emitted by the infant (i.e., coos, grunts, whimpers, babbles, or brief cry noises) that was not sufficient enough to be considered a signal of distress (i.e., fussing or crying).
Infants differed in whether and how they signaled an awakening. Some infants (“clear signalers”) signaled their awakenings clearly by standing at the crib railing and crying or fussing or sitting up and crying. Their signals seemed directed at their caregivers as though they were calling for them. Others (“not clear signalers”) signaled more passively and with less intensity, merely vocalized, or never seemed to wake. Thus, infants were coded as either “clear signalers” or “not clear signalers” based on their predominant method of signaling.
In terms of patterns of nighttime interaction, there were differences in whether and how mothers and infants interacted during the night. Some dyads had no interaction during the night and others had multiple interactions. Some of those interactions were smooth, in tune and responsive. Infants were responded to quickly, picked up and later either returned to their crib to resume sleeping or taken into the parents’ bed. Other interactions consisted of multiple attempts at soothing, ineffective soothing attempts (i.e., rubbing the baby’s back in the crib while the baby continued to cry) or showed little consistency in the type of soothing method used from one waking to another. Thus, each infant–mother dyad was assigned a global code to describe its overall pattern of nighttime interaction. This was arrived at through a two-step process.
Each signaled awakening observed during the three nights was coded according to the following methods of responding: (1) no response/let cry, (2) let cry (at least 5 minutes) and then soothe, (3) soothe in crib (including lay back down, give pacifier, cover with blanket, pat back), (4) pick up, (5) increase physical contact (first soothe in crib and then pick up), (6) multiple attempts/no clear pattern (four or more attempts at soothing or fewer than four attempts which could not be described using one of the previous methods of responding). See Appendix A for additional details.
Second, a global code to characterize the overall pattern of nighttime interaction per dyad was determined according to the most commonly used method of responding per awakening across the three nights of observation. Infants who either did not wake or did not signal distress during the three nights were coded “no wake/ no signal.” Infants who woke and signaled, but were usually not responded to were coded “no response.” Infants who signaled distress and were usually picked up or soothed in their cribs were coded “pick up/soothe.” Infants who were usually soothed with four or more attempts at one awakening or an array of attempts across all the awakenings were coded “multiple attempts/inconsistent.”
To determine inter-rater reliability, 20% of the videotapes were coded by a second rater. Observers showed agreement by coding each awakening with the same method of responding and by coding each dyad with the same overall classification for mother–infant pattern of nighttime interaction. There was 71% agreement (kappa = .58) between coders on the method of responding assigned to each awakening. There was 89% agreement (kappa = .85) between coders on the assignment to category for child signaling and to pattern of nighttime interaction, which served as the primary data for analyses.
Maternal self-report of nighttime interactions
A nighttime self-report diary allowed mothers to report bedtime and night waking interactions. This was used as an adjunct to the video observations. Mothers reported on how infants were put to sleep at bedtime and what transpired if infants woke during the night, such as whether a parent responded to the awakening and how the infant fell back to sleep. The measure was based on Anders’ sleep–wake diary (Goodlin-Jones, Burnham, Gaylor, & Anders, 2001) and Sadeh’s Brief Infant Sleep Questionnaire (Sadeh, 2005).
Mother–infant attachment relationship
Attachment was assessed using the Strange Situation Procedure (Ainsworth et al., 1978). This 24-minute laboratory task is designed to increasingly stress the infant to assess his or her reliance on the mother for comfort during distress. The infant and mother are separated and reunited twice and the infant’s attachment behaviors during the reunion episodes are coded in terms of proximity-seeking, contact maintenance, resistance, and avoidance (Ainsworth et al., 1978). Infant–mother dyads are assigned to one of four classifications: secure, avoidant, resistant, or disorganized. Upon reunion, infants classified as secure (B) seek out whatever contact is needed and calm easily in the presence of their mothers. Infants classified as avoidant (A) turn away from their mothers when distressed. Infants classified as resistant (C) show angry resistance to attempts by their mothers to calm them. Infants classified as disorganized (D) appear to lack a strategy for dealing with distress in the mother’s presence or show a breakdown in their strategies for dealing with distress. For the purposes of this study, infant–mother dyads were grouped as either secure (B) or insecure (A, C, or D) because of the small sample size.
Four trained coders (not including the coders of nighttime interaction) were used to classify the infant–mother attachment relationship. Each attended a 2-week training course on coding organized patterns of attachment (ABC) offered by Alan Sroufe and disorganized patterns of attachment (D) offered by Elizabeth Carlson or Mary Main, all experts in the assessment of attachment. All coders had passed reliability tests for classifying organized attachment, achieving at least 80% agreement with the expert coders. Two of the four coders had also passed reliability tests for classifying disorganized attachment, achieving at least 80% agreement with the expert coders. All Strange Situations were double-coded. Each pair of raters included one rater reliable on coding disorganized attachment. When there were disagreements between raters, the procedure was coded by a third reliable coder (i.e., the other coder who was reliable on organized and disorganized attachment), with final classifications determined by conferencing of the three coders. In this sample, the agreement between raters was 75% agreement (kappa = .47) for secure versus insecure classifications used in analyses here. (Agreement was 77% for three-category distinctions, and 68% for four-category distinctions, with kappas of .54 and .49, respectively.) Although this level of agreement is somewhat lower than often obtained, this is compensated for by the use of two raters on every Strange Situation, rather than only for a subset. Thus, all Strange Situation classifications were concordant at the level of the 4-way classification, or involved a third coder who independently coded and conferenced with the first two coders to determine classification.
Maternal perceived temperament
Temperament has been associated with attachment status and maternal sensitivity (Seifer, Schiller, Sameroff, Resnick, & Riordan, 1996); therefore, infant temperament data were collected from mothers. Perceived temperament was assessed using five subscales from the Revised Infant Behavior Questionnaire (IBQ-R; Gartstein & Rothbart, 2003). The five subscales are Distress to Limitations, Fear, Soothability, Cuddliness, and Smiling and Laughter. The IBQ-R is a 184-item instrument that assesses 14 dimensions of temperament in infants between the ages of 3 and 12 months. Parents indicate on a 7-point scale (never to always) how frequently their infants responded to events (e.g., visiting a new place) in specific ways during the past week. An initial evaluation of the IBQ-R supports the reliability and validity of the instrument (Gartstein & Rothbart, 2003).
Results
Results are presented in the following order. First, the sample is described in terms of attachment classification. Second, preliminary analyses conducted to examine any confounding variables are presented. Third, the sample is described in terms of infant and mother nighttime behaviors. Finally, the central study hypotheses regarding the differences in the ways secure and insecure mother–infant dyads interact at night are presented.
Attachment classifications
Sixty-one percent (N = 27) of the infants were classified secure in the Strange Situation, 27% (N = 12) were classified disorganized, 7% (N = 3) were classified resistant, and 5% (N = 2) were classified avoidant. Of the infants classified disorganized, 5 had secondary secure classifications, 6 had secondary resistant classifications, and 1 had a secondary avoidant classification. To allow sufficient power to detect differences, attachment was considered as a dichotomous variable. Thus, 61% (N = 27) were classified secure and 39% percent (N = 17) were classified insecure (avoidant, resistant, or disorganized).
Preliminary analyses
Preliminary analyses were conducted to examine associations between attachment and temperament. T-tests of maternal perceived temperament (five subscales) and attachment at 12 months showed no significant differences for secure and insecure dyads (see Table 2). In addition, temperament was not correlated with either the infants’ rate of signaling their distress after an awakening or the overall pattern of nighttime interaction. Clear signaling was correlated with two temperament subscales (Distress to Limitations .339 and Fear .341). Compared with insecure infants, more secure infants had mothers who were their main caregivers during the weekday, χ2(1, N = 44) = 6.04, p = .01. No other associations between demographic variables and attachment were significant.
Table 2.
Preliminary analyses of associations between attachment and temperament.
| Temperament subscales | Secure (N = 27) | Insecure (N = 17) |
|---|---|---|
| 1. Distress to limitations | M = 3.66 | M = 3.26 |
| 2. Fear | M = 3.11 | M = 2.89 |
| 3. Soothability | M = 5.22 | M = 5.33 |
| 4. Cuddliness | M = 5.59 | M = 5.60 |
| 5. Smiling and laughing | M = 5.36 | M = 5.46 |
Note: p < .05.
Infant and mother behaviors at night
Infant and mother nighttime behaviors are described in five areas: how infants are put to sleep at bedtime, how often infants wake in their cribs during the night, how often infants signal their awakenings by fussing or crying, how often mothers respond to the infants’ signaled awakenings, and whether infants are taken into the parents’ bed after an awakening (see Table 3). First, mothers reported on whether or not they stayed with their babies until the infants had fallen asleep at bedtime for each of the three nights of observation. Thirty-five percent reported staying all three nights, 9% stayed two nights, 4% stayed one night, and 48% never stayed. Second, the number of awakenings observed across the three nights while babies slept in their cribs ranged from 0 to 11 (N = 44, M = 3.77, SD = 2.78). Third, the number of times babies were observed across the three nights to signal that they were awake by fussing or crying ranged from 0 to10 (N = 41, M = 3.12, SD = 2.69). Fourth, the number of times mothers were observed across the three nights to respond to babies who signaled their awakening with fussing or crying ranged from 0 to 9 (N = 34, M = 2.8, SD = 2.56). Finally, 75% of mothers (N = 33) reported that they never brought their babies into their beds after an awakening and 25% (N = 11) reported taking their babies into their beds at least one of the three nights. There were no differences between secure and insecure dyads in any of these behaviors.
Table 3.
Ranges, means, standard deviations and percentages for infant and mother behaviors during night wakings.
| Variable (observed across the three nights) | Min. | Max. | M | SD | % |
|---|---|---|---|---|---|
| 1. Percent of mothers who put babies to bed awake | 48 | ||||
| 2. Number of infant awakenings in crib | 0 | 11 | 3.77 | 2.78 | |
| 3. Number of signaled awakenings in crib | 0 | 10 | 3.12 | 2.69 | |
| 4. Number of caregiver responses to signaled awakenings | 0 | 9 | 2.8 | 2.56 | |
| 5. Percent of mothers who took babies into their beds after an awakening at least one night |
25 |
Mother–infant nighttime interactions
Clear signaling of awakenings
It was hypothesized that secure infants would be more likely than insecure infants to signal their awakenings clearly. There were no significant differences in the percentage of infants who signaled clearly as a function of attachment, χ2(1, N = 44) = 3.20, p = .07, although the percentage of infants who signaled clearly tended to be higher for securely attached than insecurely attached infants. For the securely attached infants, 63% were “clear signalers” and 37% were “not clear signalers.” For the insecurely attached infants, 35% were “clear signalers” and 65% were “not clear signalers” (see Table 4).
Table 4.
Clear signaling of awakenings in securely and insecurely attached infants.
| Clear signaling of awakenings | Secure dyads (N = 27) | Insecure dyads (N = 17) |
|---|---|---|
| Infants who signal clearly | 17 (14.1) | 6 (8.9) |
| Infants who do not signal clearly | 10 (12.9) | 11 (8.1) |
Patterns of mother–infant nighttime interaction
To investigate the hypothesis that secure infants are more likely to have consistent, sensitive, responsive maternal behavior during nighttime interactions than insecure infants, a 2 (attachment classification: secure vs. insecure) x 4 (pattern of nighttime interaction: no wake/no signal vs. no response vs. pick up/soothe vs. multiple attempts/inconsistent) Pearson chi-square analysis was performed. The patterns of nighttime interaction differed by attachment security, χ2 (3, N = 44) = 11.04, p < .01. The results are shown in Table 5 and Figure 1.
Table 5.
Patterns of nighttime interactions in secure and insecure dyads.
| Patterns of nighttime interactions | Secure dyads (N = 27) |
Insecure dyads (N = 17) |
|---|---|---|
| Number of infants who do not wake or signal | 4 (6.1) | 6 (3.9) |
| Number of infants who signal and no one responds | 8 (6.1) | 2 (3.9) |
| Number of infants who signal and are picked up or soothed in crib |
12 (8.6) | 2 (5.4) |
| Number of infants who signal and caregiver responds with multiple attempts or inconsistently |
3 (6.1) | 7 (3.9) |
Figure 1.
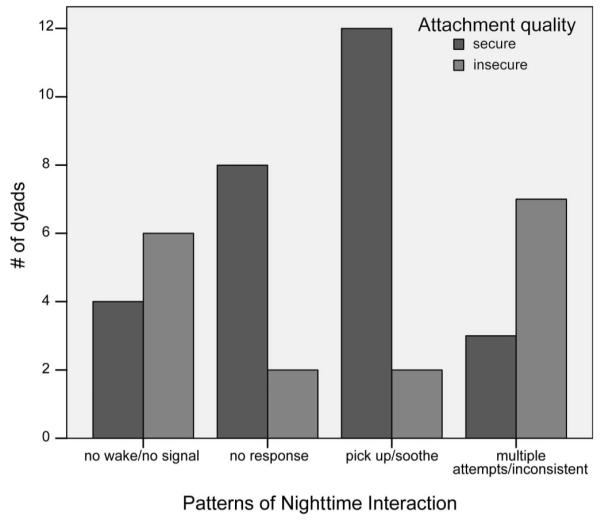
Patterns of mother–infant nighttime interactions for secure and insecure dyads.
Secondary analyses were performed to identify which patterns of nighttime interaction differentiated secure and insecure dyads. A series of chi-square goodness of fit tests were performed. The results indicated that securely and insecurely attached dyads differed significantly for the “pick up/soothe” pattern of nighttime interaction, χ2 (1, N = 14) = 7.14, p < .01, with the mothers of secure infants more likely to pick up and soothe infants who woke and signaled. For the “no wake/no signal,” “no response,” “multiple attempts/inconsistent” patterns, the results were as follows: χ2 (1, N = 10) = .40, p = .53, χ2 (1, N = 10) = 3.6, p = .06, χ2 (1, = N = 10) = 1.6, p = .21, respectively.
Discussion
The purpose of this study was to investigate the differences between secure and insecure mother–infant dyads in the way they interact at night when infants are 12 months old. Patterns of nighttime interaction were significantly different for secure and insecure dyads. The interactions most characteristic of secure dyads involved infants signaling their awakenings with fussing or crying and mothers responding quickly by picking up and soothing the baby. These interactions were usually smooth, the responses were generally in tune with the baby’s signals, and the methods of responding were similar from one awakening to the next.
To further explore differences in nighttime interactions between secure and insecure dyads, each pattern of interaction was examined independently. First, comparisons were made between securely and insecurely attached infants who never woke or never signaled distress. There were no significant differences. In other words, “good sleepers” (i.e., infants who do not disturb their parents during the night either because they never wake or they never make their awakenings known to their parents by fussing or crying) are not significantly more likely to be securely attached than insecurely attached. Second, comparisons were made between mothers in secure and insecure dyads who generally did not respond to their infants’ signaled awakenings. There were no significant differences, although mothers in secure dyads were more likely to use the “no response” pattern of interaction than mothers in insecure dyads. Third, comparisons were made between mothers in secure and insecure dyads who generally picked up and soothed their infants when they woke and fussed or cried. As expected, mothers of secure infants were significantly more likely to be characterized by the “pick up/soothe” pattern of interaction than mothers of insecurely attached infants. Finally, comparisons were made between mothers in secure and insecure dyads who generally made multiple soothing attempts or were inconsistent in terms of the ways they responded across all awakenings. There were no significant differences between mothers in secure and insecure dyads. Thus, the overall finding that the patterns of nighttime interaction vary by attachment classification is due to mothers in secure dyads being more likely to pick up and soothe their infants when the infants wake and fuss or cry during the night as compared to mothers in insecure dyads.
In terms of how infants signaled their awakenings, differences were in the direction of securely attached infants signaling their awakenings more clearly than insecurely attached infants, but the difference was not significant. The power to detect differences was weak in this study. It is plausible that differences would have reached significance with a larger sample size. However, it is also possible that the expected association between attachment and clear signaling does not exist.
Viewed in light of attachment theory and research, the results of the present study can be interpreted as showing that consistent, sensitive responses to infant signals of distress relate to attachment security, even at night. In other words, mothers of securely and insecurely attached infants are not different in terms of how frequently they respond to their infants’ signaled awakenings; they are different in that, when they respond, mothers of securely attached infants are more likely to respond sensitively and consistently. In a meta-analysis on parental antecedents of infant attachment, De Wolff and van IJzendoorn (1997) found that sensitivity (i.e., the ability to perceive the infant’s signals accurately and respond promptly and appropriately) is a better predictor of attachment than contiguity of response (i.e., the promptness or frequency of the mother’s responses, not taking into account appropriateness). This may explain why this present study found associations between attachment and the quality of mothers’ responses to awakenings, but not their frequency of responding.
van IJzendoorn and Hubbard (2000) found that mothers of avoidant infants actually picked up their crying infants more quickly than other mothers. Although the number of avoidant infants in our study was too small (n = 2) to allow specific comparisons, the van IJzendoorn and Hubbard finding is interesting to consider as related to our findings more generally. van IJzendoorn and Hubbard interpreted their findings to suggest that mothers whose infants are avoidantly attached to them may pick them up “too quickly” because of discomfort in hearing the cry. A lack of power did not allow a full test of this possibility.
It is interesting to compare this data set with the findings from prior studies of attachment and sleep. In terms of bedtime settling practices, about half (52%) of the mothers reported staying with their babies until babies fell asleep at bedtime. Thus, putting 12-month-old babies to bed asleep is common despite cautions against such practices. Furthermore, whether mothers helped their infants transition to sleep was not related to attachment, which is consistent with the findings of prior studies (Scher & Asher, 2004). In terms of night waking, the majority of infants (93%) had at least one night waking during the three nights of observation. Scher (2001) reported that more than 50% of the 12-month-olds were classified as nightwakers. In the present study, the rate of waking did not relate to attachment security. Although some prior studies reported that insecure 12-month-olds were more likely to awaken (Seifer et al., 1996), that finding was based on maternal report from a sample of mothers with mental illness. In studies that used community samples (Scher, 2001; Scher & Asher, 2004), security of attachment was not related to frequency of nightwaking. Thus, it seems that there is not evidence that how often infants wake at night is related to attachment, at least in a low-risk sample.
Limitations and future directions
This study has several limitations that limit generalization of the results. First, the sample was small, self-selected and consisted mostly of upper-middle class non-Hispanic white mothers. Second, the cross-sectional design does not allow for an examination of whether and how mother–infant interactions changed over time. Third, the digital video recordings captured only those interactions that occurred while infants were in their cribs. Thus, how mothers and infants interacted when babies were out of their cribs or whether mothers responded differently off camera or during nights other than the three that were recorded is not known. Finally, the rate of disorganized attachment (27%) was high for this low-risk sample. In typical, middle class families, about 15% of infants develop disorganized attachments (van IJzendoorn, Schuengel, & Bakersmans-Kranenburg, 1999). Mothers were recruited largely by word of mouth and told that the purpose of the study was to learn more about what mothers do at night, how their babies sleep, and how it relates to mother–infant interactions during the day. It is not clear why the majority of the infants classified as insecure were disorganized, but it may be that the findings only relate to disorganized attachment.
Nonetheless, this study provides important new information about the differences in the patterns of interactions between secure and insecure mother– infant dyads. A prospective, longitudinal study needs to be conducted with larger samples to verify and expand on these patterns and to help in understanding how these patterns develop over time. A larger sample would also provide the power to evaluate how different attachment classifications relate to patterns of nighttime interaction. Future research should include measures that allow for an examination of the consistency between daytime and nighttime interactions in terms of sensitivity and attachment. To do so, it may be necessary to observe mothers and infants during the day in somewhat stressful contexts that trigger the attachment system (Smith & Pederson, 1988).
Summary
In conclusion, this study examined the association between attachment quality and mother–infant interaction at night. It combined the well-established assessment of attachment (i.e., Ainsworth’s Strange Situation) with new digital video technology that captured naturalistic mother and infant interactions during the night in real-time with minimal disruption. The focus was on observing the interactions of a low-risk community sample as opposed to those seeking treatment for a perceived sleep problem in their infants.
The primary finding was that mothers of securely attached infants had nighttime interactions that were generally more consistent, sensitive and responsive than those of insecurely attached infants. Specifically, in secure dyads, mothers generally picked up and soothed infants when they woke and fussed or cried. In insecure dyads, mothers generally made multiple soothing attempts and tended to be inconsistent in terms of the methods of responding they used across all awakenings. Secure and insecure dyads did not differ significantly in terms of whether there was generally no contact between mothers and infants during the night or whether mothers generally soothed infants during the night. This study suggests that, at least in terms of attachment security, it is not simply whether the infant wakes or whether the mother responds to the infant’s fussing or crying during awakenings, but rather, for those mothers who generally do respond, whether the response is sensitive, consistent and in tune with the baby’s needs.
Acknowledgements
This research was supported in part by National Institutes of Mental Health grants 52135 and 74374 to the second author. We thank Elizabeth Peloso for her help developing the methodology and the families who participated in the study.
Appendix A.
Code Catalog for Nighttime Interaction
This is a description of the steps involved in coding the nighttime videos used to calculate agreement between observers. Observers need to show agreement in two ways:
Observers need to code each awakening with the same method of responding.
Observers need to code each dyad with the same overall classification for mother– infant pattern of nighttime interaction.
Step 1: Nighttime Video Coding
Watch the video and complete one “Nighttime Video Coding” sheet for each of the three nights of video. Refer to the accompanying “Nighttime Diary” that mothers completed. Record:
Dates (e.g., 8/16 – 8/17) (night of the 16th into morning of the 17th)
Night (i.e., 1, 2, or 3)
ID # (i.e., child’s subject code)
Bedtime
Time in crib (hr:min) (time baby is put in the crib)
Who put baby to bed (Mom, Dad, Other) (may need to refer to mother’s diary)
Stays until asleep (Yes/No) (whether the mom reports staying until the baby fell asleep at bedtime)
Baby cried before falling asleep (Yes/No/N/A) (If mom does not stay until asleep, indicate whether the baby cries in their crib before falling asleep)
Brief description of bedtime interaction
Awakenings
An awakening is defined as a transition from sleep to waking. According to Hayes (2002), “an awakening is behaviourally defined when the individual engages in conscious behaviors that reflect awareness of their surroundings such as eyes open, talking, or positional and motor movements incompatible with sleep (sitting up, walking, etc) …” (p. 25). Awakenings last at least 1–2 minutes.
- Confidence (how confident you are that the baby is awake)
- not sure awake
- probably awake
- definitely awake
Time awake (hr:min:sec)
- Vocalization (any sound emitted by baby)
- No vocalization
- Mild vocalization (whines/whimpers/grunts/coos/babbles/brief cry noise)
- Signals distress (Fusses/Cries)
Responder (Mom, Dad, Other, No one) and time (time response occurred)
Latency to respond to cry (how many minutes the baby fussed/cried before the caregiver responded. Round to the nearest half minute.)
Stays until asleep (Yes, No, N/A) (whether the mother reports staying until baby falls back to sleep)
If no, does baby cry (Yes, No, N/A) (If caregiver does not stay until back to sleep, indicate whether the baby cries)
Describe awakening (write a brief description of the awakening. Include times where appropriate)
General
Total # of awakenings (only those awakenings coded “probably” or “definitely” awake)
Time woke up in the morning
Time out of crib for that night
Step 2: Code Each Soothing Attempt per Awakening
For each awakening (that is considered probably or definitely awake), record the following information on a spreadsheet:
Subject code
Night (1,2,3) – which night the awakening occurred
Time (hr:min) – time of the awakening
Signals distress (Yes, No) – whether the baby signaled distress (fussed/cried)
Responder (Mom, Dad, No one) – who responded to the awakening (exclude awakenings when someone other than parent responded)
Return (#) – the number of times caregiver had to return to perform more soothing attempts for that awakening
Latency (min) – how many minutes the baby fussed/cried before the caregiver responded. (Round to the nearest half minute)
- R1 – R6 (or more if needed) – assign one of the following 5 codes for each soothing attempt performed during that awakening:
- no response/let cry
- stands by crib (no touch)
- resettles (repositions baby, lays baby back down, give pacifier/cuddly, cover with blanket)
- pats/rubs back, belly or head
- picks up
Step 3: Assign One Method of Responding per Signaled Awakening
Describe the method of responding (based on R1 – R5 from Step 2) using the following codes:
no response/let cry (when no one responds to baby’s signal of distress during an awakening)
let cry/soothe (1 to 2,3,4,5) (for caregivers who let infants cry at least 5 min and then respond with either picking up or soothing in crib)
soothe in crib (2,3,4) (when standing by crib, resettling, and/or rubbing back are the first and only response)
pick up (5) (when picking up is the first and only response)
increasing physical contact (2,3,4 to 5) (to begin with soothing in crib and then to pick up)
multiple soothing strategies/no clear pattern (for caregivers who make 4 or more attempts at soothing or those who make fewer soothing attempts that do not fit within the above methods)
Step 4: Assign a Summary Code for the Pattern of Nighttime Interaction
Assign each dyad one of the following overall pattern of nighttime interaction codes according to the caregiver’s most frequently used method of response (from Step 3) across the three nights.
no wake/no signal (babies who never wake and/or never signal distress during awakenings across the three nights of observation)
no response (the most frequent response to signaling distress during awakenings is no response)
pick up/soothe (the most frequent response to signaling distress during awakenings is either 3, 4, or 5 from step 3)
multiple attempts/inconsistent (either 6 is the most frequent response or a mixture of 1–6 is used such that no one method predominates)
References
- Adair R, Bauchner H, Philipp B, Levenson S, Zuckerman B. Night waking during infancy: Role of parental presence at bedtime. Pediatrics. 1991;87:500–504. [PubMed] [Google Scholar]
- Ainsworth MDS, Bell S, Stayton D. Infant–mother attachment and social development: Socialization as a product of reciprocal responsiveness to signals. In: Richards M, editor. The integration of the child into the social world. Cambridge University Press; Cambridge: 1974. pp. 99–135. [Google Scholar]
- Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Lawrence Erlbaum Associates; Hillsdale, NJ: 1978. [Google Scholar]
- Benoit D, Zeanah CH, Boucher C, Minde KK. Sleep disorders in early childhood: Associations with insecure maternal attachment. Journal of American Academy of Child and Adolescent Psychiatry. 1992;31:86–93. doi: 10.1097/00004583-199201000-00013. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss. Vol. 2: Separation: Anxiety and anger. Basic Books; New York: 1973. [Google Scholar]
- Bowlby J. Attachment and loss. 2nd ed. Vol. 1: Attachment. Basic Books; New York: 1982. (Original work published 1969) [Google Scholar]
- De Wolff MS, van IJzendoorn MH. Sensitivity and attachment: A meta-analysis on parental antecedents of infant attachment. Child Development. 1997;68:571–591. [PubMed] [Google Scholar]
- Ferber R. Solve your child’s sleep problems. Simon and Schuster; New York: 2006. (Original work published 1985) [Google Scholar]
- Gartstein MA, Rothbart MK. Studying infant temperament via the revised infant behavior questionnaire. Infant Behavior and Development. 2003;26(1):64–86. [Google Scholar]
- Gaylor EE, Goodlin-Jones BL, Anders TF. Classification of young children’s sleep problems: A pilot study. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:61–67. doi: 10.1097/00004583-200101000-00017. [DOI] [PubMed] [Google Scholar]
- Goodlin-Jones BL, Burnham MM, Anders TF. Sleep and sleep disturbances: Regulatory processes in infancy. In: Sameroff AJ, Lewis M, Miller SM, editors. Handbook of developmental psychopathology. 2nd ed Kluwer Academic/Plenum Publishers; New York: 2000. pp. 309–325. [Google Scholar]
- Goodlin-Jones BL, Burnham MM, Gaylor EE, Anders TF. Night waking, sleep–wake organization, and self-soothing in the first year of life. Developmental and Behavioral Pediatrics. 2001;22:226–233. doi: 10.1097/00004703-200108000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes MJ. Methodological issues in the study of arousals and awakenings during sleep in the human infant. In: Salzarulo P, Ficca G, editors. Awakening and Sleep-wake Cycle Across Development. John Benjamins Publishing; Amsterdam: 2002. pp. 23–46. [Google Scholar]
- Meltzer LJ, Mindell JA. Nonpharmacologic treatments for pediatric sleeplessness. Pediatric Clinics of North America. 2004;51:135–151. doi: 10.1016/s0031-3955(03)00178-0. [DOI] [PubMed] [Google Scholar]
- Morrell J, Cortina-Borja M. The developmental change in strategies parents employ to settle young children to sleep, and their relationship to infant sleeping problems, as assessed by a new questionnaire: The parental interactive bedtime behaviour scale. Infant and Child Development. 2002;11:17–41. [Google Scholar]
- Morrell J, Steele H. The role of attachment security, temperament, maternal perception, and care-giving behavior in persistent infant sleeping problems. Infant Mental Health Journal. 2003;24:447–468. [Google Scholar]
- Norluchi M, Kikuchi Y, Senoo A. The functional neuroanatomy of maternal love: Mother’s response to infant’s attachment behaviors. Biological Psychiatry. 2007;63:415–423. doi: 10.1016/j.biopsych.2007.05.018. [DOI] [PubMed] [Google Scholar]
- Sadeh A. Sleep fragmentation and awakening during development: Insights from actigraphic studies. In: Salzarulo P, Ficca G, editors. Awakenings and sleep–wake cycles across development. John Benjamin Publishing; Amsterdam: 2002. pp. 199–211. [Google Scholar]
- Sadeh A. A brief screening questionnaire for infant sleep problems: Validation and findings for an internet sample. Pediatrics. 2005;114:570–577. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]
- Scher A. Attachment and sleep: A study of night waking in 12-month-old infants. Developmental Psychobiology. 2001;38:274–285. doi: 10.1002/dev.1020. [DOI] [PubMed] [Google Scholar]
- Scher A, Asher R. Is attachment security related to sleep–wake regulation? Mothers’ reports and objective sleep recordings. Infant Behavior and Development. 2004;27:288–302. [Google Scholar]
- Seifer R, Sameroff AJ, Dickstein S, Hayden LC, Schiller M. Parental psychopathology and sleep variation in children. Child and Adolescent Psychiatric Clinics of North America. 1996;5(3):715–727. [Google Scholar]
- Seifer R, Schiller M, Sameroff AJ, Resnick S, Riordan K. Attachment, maternal sensitivity, and infant temperament during the first year of life. Developmental Psychology. 1996;32(1):12–25. [Google Scholar]
- Smith PB, Pederson DR. Maternal sensitivity and patterns of infant–mother attachment. Child Development. 1988;59(4):1097–1101. doi: 10.1111/j.1467-8624.1988.tb03262.x. [DOI] [PubMed] [Google Scholar]
- Tikotzky L, Sadeh A. Sleep patterns and sleep disruptions in kindergarten children. Journal of Clinical Child Psychology. 2001;30:581–591. doi: 10.1207/S15374424JCCP3004_13. [DOI] [PubMed] [Google Scholar]
- van IJzendoorn MH, Hubbard ROA. Are infant crying and maternal responsiveness during the first year related to infant–mother attachment at 15 months? Attachment and Human Development. 2000;2:371–391. doi: 10.1080/14616730010001596. [DOI] [PubMed] [Google Scholar]
- van IJzendoorn MH, Schuengel C, Bakermans-Kranenburg M. Disorganized attachment in early childhood: Meta-analysis of precursors, concomitants, and sequelae. Development and Psychopathology. 1999;11:225–250. doi: 10.1017/s0954579499002035. [DOI] [PubMed] [Google Scholar]
- Van Tassel EB. The relative influence of child and environmental characteristics on sleep disturbances in the first and second years of life. Journal of Developmental and Behavioral Pediatrics. 1985;6:81–86. [PubMed] [Google Scholar]
- Waters E, Deane KE. Bretherton I, Waters E, editors. Defining and assessing individual differences in attachment relationships: Q-methodology and the organization of behavior in infancy and early childhood. Growing points of attachment theory and research. Monographs of the Society of Research in Child Development. 1985;50:41–65. [Google Scholar]


