Abstract
Medicare assigns beneficiaries receiving low-income subsidies to plans with premiums below regional benchmarks. The number of these low premium plans fell in 2009, forcing the reassignment of 1.6 million beneficiaries. Using data from Part D plans, we found that CMS’s current risk adjustment scheme does not sufficiently compensate plans for the greater drug spending of low-income subsidy beneficiaries. Since plans can avoid these beneficiaries by raising their premiums above that of their competitors, premiums for all beneficiaries tend to rise over time. Paying more for subsidy and less for non-subsidy beneficiaries, or accounting for past drug use in the risk adjustment scheme could mitigate these perverse incentives.
Introduction
The Medicare Part D outpatient prescription drug program started in 2006, and by 2010 had more than 27 million beneficiaries enrolled.1 Drug benefits under the program are administered by private health insurance plans. Medicare risk-adjusts payments to the plans by taking into account each beneficiary’s prior-year inpatient and outpatient diagnoses, but not their prescription drug use. Low-income beneficiaries, who receive assistance through the low-income subsidy (LIS) program, use more and/or costlier drugs on average, so Medicare takes the additional step of increasing plan payments for this group using an “LIS multiplier.” Under the current rules, Medicare pays eight percent more for a beneficiary receiving the full subsidy compared to a similar beneficiary without the subsidy, and five percent more for those receiving partial subsidies.2 In 2009, 9.6 million beneficiaries received a full or partial subsidy.3 The goal of risk adjustment generally and the LIS multipliers specifically is to compensate plans fairly and to decrease incentives for plans both to avoid beneficiaries with unfavorable risk profiles and to attract those with favorable profiles.4–8
Although higher income beneficiaries must choose a plan, Medicare assigns low-income subsidy beneficiaries each year to stand-alone private Part D plans whose premiums are below a regional benchmark. If Medicare payments adequately compensate plans for the additional drug cost of subsidy beneficiaries, we would expect plans to compete for these beneficiaries by lowering premiums or limiting premium growth relative to competing plans. This competition for subsidized beneficiaries was one of the original program intentions. Conversely, plans that decide compensation for these beneficiaries is too low may increase premium bids to be higher than the premium bids of many of their competitors, thus higher than the regional benchmark, which reflects the average of the premium bids for all basic Part D plans in the area. If this happens, the above-benchmark plan would not receive any new subsidy beneficiaries and their existing subsidized enrollees would be reassigned.9 This has potential clinical repercussions for the reassigned beneficiaries, as they generally experience formulary changes that may require changes in their drug treatment regimen.
Our findings are consistent with a malfunctioning risk adjusted payment system and Part D market; fewer plans are participating in the subsidy market compared with earlier years. In 2006, 29 percent of Prescription Drug Plans (PDP) qualified for low-income subsidy assignment, but that number fell to 18 percent in 2009. Correspondingly, plan reassignments affected 1.1 million beneficiaries in 2007, 2.1 million in 2008, 1.6 million in 2009, and 1.2 million in 2010.3, 10, 11
These incentives to avoid assignment of subsidy beneficiaries are further reinforced over time by the increasing share of any losses that private plans bear. When Part D began in 2006, Medicare established risk corridors under which it shared plans’ losses or gains greater than 2.5 percent; the corridors doubled to 5 percent in 2008, and are expected to widen further starting in 2012.
We previously examined the performance of the Part D risk scores in a Medicare Advantage population and found that incorporating information on beneficiaries’ past year drug use markedly improved the accuracy of payments.12 With new data from stand-alone Prescription Drug Plan populations, the same result holds in that population (see appendix). We also now find that improving the risk adjustment accuracy could mitigate the relative underpayment for beneficiaries with the low-income subsidy.
In short, payment accuracy, particularly for low-income subsidy beneficiaries relative to other beneficiaries, is important not only for reducing plans’ incentives to dump and cream skim, but also for maintaining plan participation in the subsidy market, decreasing disruptions in plan enrollment, and minimizing premium growth for the entire Part D program. In this study, we examine the accuracy of the low-income subsidy multipliers and find them wanting.
Part D Low Income Subsidy
Eligibility
The subsidy includes two levels of premium assistance: full and partial. Those who automatically qualify (“deemed” eligible) for a full premium subsidy and limited copayments account for the great majority of subsidy beneficiaries (8.1 of 9.6 million in 2009). Many individuals deemed eligible also are eligible for Medicaid, i.e., the 6.3 million dual-eligible beneficiaries in 2009.3, 13 Also eligible for the full subsidy are beneficiaries with incomes less than 135 percent of the Federal Poverty Level and limited assets (≤$8,100 for a single person in 2009). Beneficiaries with incomes between 135 percent and 150 percent of the Federal Poverty Level and limited assets (≤$12,510 for a single person in 2009) can apply for a partial subsidy.
LIS Auto-Enrollment
Each year, the Centers for Medicare and Medicaid Services (CMS) calculates the average plan bid across all plans nationally and pays plan sponsors a percentage of that average for each enrollee, adjusted by the enrollee’s risk score and, for the subsidy beneficiaries, a low-income subsidy multiplier. In plans with premiums below an annually calculated regional benchmark, Medicare pays the entire premium cost. Beneficiaries can still enroll in a non-benchmark plan (that is, a plan with premiums above the benchmark) by paying the amount above benchmark out of their own pockets. CMS automatically and randomly assigns subsidy beneficiaries who have not chosen a Part D plan to a below-benchmark plan through a process known as auto-enrollment (dual eligible beneficiaries) or facilitated enrollment (other subsidy beneficiaries).14
Risk adjustment approach
Medicare bases the current risk score on inpatient and outpatient diagnoses from the prior year in addition to age-sex categories and disability status.2 Medicare also uses multipliers to further increase payments for low-income subsidy and institutionalized populations because of concerns that the payment yielded by the risk score alone would not adequately reflect higher levels of drug spending by both groups, in part because of their lower drug cost-sharing requirements.15
Methods
The goal of our research was to determine whether the adjustments used by CMS for the subsidized group resulted in adequate prospective payments relative to the non-subsidized group. The current payments assume that on average, risk-adjusted plan drug spending for beneficiaries with the subsidy will be eight percent higher than spending for beneficiaries without the subsidy. To examine this issue, we collected data on individual drug spending by both those receiving a subsidy and those not receiving a subsidy, and calculated the total drug spending for each beneficiary, less contributions by CMS and by the individual beneficiary. This amount, i.e., the plan liability, indicates how much the plan spent on prescription drugs for the beneficiary. We compared actual plan drug spending for beneficiaries with and without the subsidy, relative the amount that CMS increases payments for beneficiaries with the subsidy. We also explored two potential payment improvements, i.e., simply increasing the low-income multiplier and adding information on past drug use to the risk adjustment calculation.
Study Population
The study population included beneficiaries who were continuously enrolled in a Prescription Drug Plan throughout 2007, and who had at least one month of enrollment in 2006. We required subsidy beneficiaries to have the subsidy for all of 2007, and excluded institutionalized beneficiaries because they face a separate multiplier.16 We examined Prescription Drug Plans across many geographic regions, basing our selection on a convenience sample of plans agreeing to participate in the study. We obtained drug claims and beneficiary information (e.g., subsidy status, enrollment, risk score) directly from files that the plans submitted to CMS for payment purposes. As a condition of obtaining the data, we removed identifying information including markets served, enrollees, and cost-sharing structures (more information on removal of identifying information is available in the technical appendix). The Kaiser Foundation Research Institute’s institutional review board approved the study protocol.
Plan Liability
In order to examine how various risk adjustment methods performed with respect to actual plan drug spending in 2007, i.e., plan liability, we used data from the Prescription Drug Event files, which include information on national drug codes, drug costs, patient payments, and low-income subsidy amounts. Plan liability for each beneficiary was calculated on the basis of Medicare coverage rules pertaining to prescription drugs (details of our calculation are available in the technical appendix).
LIS Multiplier Evaluation
The low-income subsidy multiplier within the prospective payment formula is designed to compensate for the greater drug spending of subsidy beneficiaries, relative to other beneficiaries, after risk adjustment. The multiplier and the risk adjustment approach are inherently linked, such that when the risk adjustment is more accurate, the multiplier is less relevant, and vice versa. To assess how well the multiplier performed its task, we compared the ratios of actual plan spending for subsidy to non-subsidy beneficiaries, under the current risk adjustment approach, to the expected ratios, i.e., the full subsidy multiplier (or ratio) of 1.08 and the partial subsidy multiplier of 1.05. We then examined the ratios of actual plan spending for subsidy to non-subsidy beneficiaries under alternative risk adjustment approaches that incorporated prior year drug information.
We hypothesized that the ratios of actual plan spending for full subsidy to non-subsidy beneficiaries under the current risk-adjustment approach would be greater than 1.08, suggesting that the current LIS multiplier does not fully compensate private plans for the greater drug spending by subsidy beneficiaries. We also hypothesized that incorporating prior year drug information into the risk adjustment approach would improve the accuracy of predicted plan spending, and mitigate the need for or reduce the magnitude of corrective multipliers.
To model how much each plan actually spent on prescription drugs for each beneficiary, we used linear regression and included each beneficiary’s Part D risk score, i.e., the RxHCC score, two indicators for the subsidy status (full or partial), and interactions between the two subsidy indicators and the risk score (the non-subsidy group was the reference group).17, 18 To assess the LIS multiplier under a more accurate risk adjustment approach, we constructed similar models, but replaced the RxHCC score with a predicted plan spending amount. We calculated the predicted spending using age, gender, RxHCC score, and prior year drug use by the beneficiary.
Based on the model results, we estimated the average plan spending for three groups: 1) full subsidy; 2) partial subsidy; and 3) non-subsidy beneficiaries. We then compared these empirically-derived ratios of the spending for full subsidy to non-subsidy beneficiaries, with the ratios from the current LIS multiplier. We repeated these steps for the partial subsidy group. If the empirically-derived multipliers are larger than the CMS multipliers of 1.08 (full LIS) and 1.05 (partial LIS), the current payment is not adequate for the subsidy group relative to the non-subsidy group.
We report actual plan spending ratios between the subsidy and non-subsidy groups for each decile of the risk score, as well as the ratio for the entire population using the current RxHCC risk adjustment approach and alternative approaches that incorporate prior year drug information.
To assess risk adjustment approaches that incorporate prior year drug information, we included information on drug use or costs. For drug use, we included 48 separate therapeutic class indicators (e.g., anti-depressants or anti-hypertensive drugs) which were coded as “1” if a beneficiary had any drug use within the class and “0” otherwise. For prior year drug costs we summed costs for Part D drugs dispensed in 2006.19 These two approaches illustrate the range of types of information available on prior drug use.
Limitations
We used data from a sample of Prescription Drug Plans across the country, so the findings could be biased if our non-subsidy subjects are healthier or our subsidy subjects are sicker, compared with beneficiaries nationwide. This seems unlikely, however, because the mean risk score for our non-subsidy subjects was 1.0, which should be close to the national average; moreover, there were high ratios across all risk score deciles, and Medicare’s subsidy auto-assignment process is random.
We also focused on beneficiaries with continuous enrollment in 2007; beneficiaries who disenrolled or died during 2007 could have different cost profiles. In addition, we excluded from the study all institutionalized beneficiaries who likely had different cost profiles and who have a separate multiplier.20 We could not assess plan profitability because information on drug rebates was not available.21 Finally, we did not evaluate the characteristics of plans participating in the subsidy market or not.
Results
Beneficiary Characteristics and Distribution of Part D Drug Costs
Exhibit 1 presents the characteristics of the study subjects. The average risk score for non-subsidy beneficiaries was 1.0, which was CMS’s goal; low-income subsidy beneficiaries had an average risk score of 1.3 reflecting their greater disease burden. The mean plan drug spending in 2007 for non-subsidy beneficiaries was $800 compared to $1,300 among the subsidy group.
Exhibit 1.
Beneficiary Characteristics
| Non-LIS Subjects |
LIS Subjects |
|
|---|---|---|
| N= | 250,000 | 250,000 |
| Age Categories | % | % |
| <65 | 11 | 42 |
| 65–<70 | 26 | 15 |
| 70–<75 | 22 | 13 |
| 75–<80 | 18 | 12 |
| 80–<85 | 13 | 9 |
| 85–<90 | 7 | 6 |
| 90+ | 3 | 3 |
| Female | 62 | 63 |
| Drug cost>$265 (start of initial coverage period in standard benefit) |
78 | 86 |
| Drug cost>$2,400 (start of coverage gap in standard benefit) |
24 | 52 |
| True out-of-pocket (Troop) costs >$3,850 (start of catastrophic coverage in standard benefit) |
3 | 23 |
| Mean | Mean | |
| RxHCC Score | 1.0 | 1.3 |
| Number of Rx Therapeutic Classes | 4 | 6 |
| Prior Year Rx Cost (annualized)* | 1,600 | 3,400 |
| Plan Liability in 2007* | 800 | 1,300 |
Note: In order to mask the identity of the individual PDP plans in our sample, we first took a random stratified sample of non-LIS and LIS beneficiaries, then applied a random factor (+/− 2.5 percent) to each individual value before determining the sample mean or characteristic percentage. The presented information could represent artificial differences between the non-LIS and LIS groups by as much as 5 percent. LIS beneficiaries did not face a deductible or coverage gap.
Dollar amounts rounded to nearest $100
Plan Liability Ratios
The ratio of average plan drug spending for full subsidy beneficiaries compared to non-subsidy beneficiaries was 1.21 (95% CI: 1.20-1.21); the ratio for partial subsidy beneficiaries compared to non-subsidy beneficiaries was 1.09 (95% CI: 1.08-1.10).
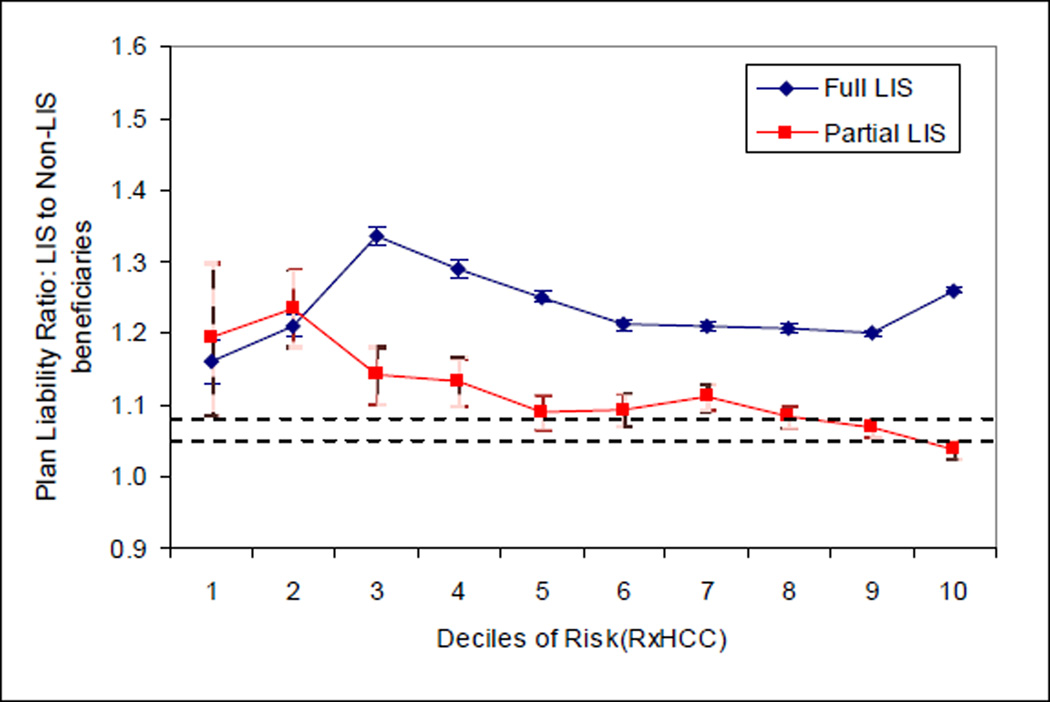
In other words, plans spent substantially more for subsidy beneficiaries (21 percent more on average for a full subsidy beneficiary than for a non-subsidy beneficiary), than predicted by the current CMS Part D payment formula (which predicted eight percent more for full subsidy than non-subsidy beneficiaries). One exception is for beneficiaries receiving a partial subsidy who have the highest predicted risk (i.e., in the highest risk score decile) for whom the ratio was 1.04. Exhibit 2 displays these ratios by deciles of Part D risk scores.
Exhibit 2. Ratio of Adjusted Mean Plan Liability of LIS to Non-LIS by Risk Decile Using Current Risk Adjustment Approach.
Note: This exhibit presents the plan liability ratios and 95% confidence intervals for LIS to non-LIS beneficiaries for each risk decile, based on the current risk adjustment approach (RxHCC). The dotted lines represent the current LIS multipliers of 1.08 (full) and 1.05 (partial), respectively.
Because actual spending exceeded predicted spending for the subsidy beneficiaries, plans have a strong incentive to avoid enrolling beneficiaries with the LIS subsidy, relative to enrolling non-subsidy beneficiaries.
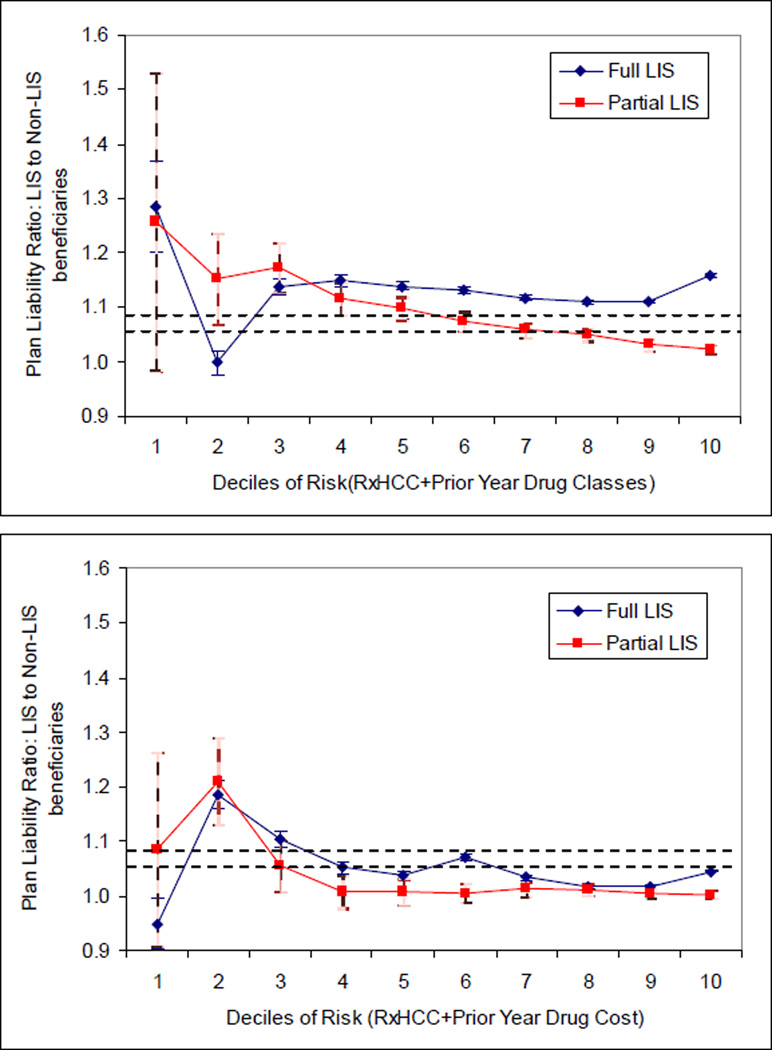
As seen in Exhibit 3, the ratio of actual plan spending for the subsidy to non-subsidy beneficiaries was much closer to the ratio expected by CMS (and built into the existing LIS multipliers), after improvements to the risk adjustment approach by accounting for prior-year prescription drug use: for example, when including information on the types of drugs used in the prior year, i.e., therapeutic class indicators, the ratio was 1.10 (95% CI: 1.10-1.11) for the full subsidy group compared to the non-subsidy group, and 1.06 (95% CI: 1.06-1.07) for the partial subsidy group. Using a slightly different risk adjustment approach that incorporated the total amount spent on Part D drugs in the prior year, the ratios were 1.05 (full subsidy, 95% CI: 1.05-1.05) and 1.04 (partial subsidy, 95% CI: 1.03-1.04). These values indicate a continued need to increase payments for subsidy beneficiaries even after use of more accurate risk adjustment approaches, e.g., paying 10 percent more (i.e., a multiplier of 1.10) for full subsidy beneficiaries if using therapeutic class indicators in the risk adjustment formula.
Exhibit 3. Ratio of Adjusted Mean Plan Liability of LIS to Non-LIS by Risk Decile Using Alternative Risk Adjustment Approaches.
Note: This exhibit displays the plan liability ratios and 95% confidence intervals for LIS to non-LIS beneficiaries for each risk decile. The top panel uses risk deciles based on RxHCC scores and prior year drug use information (48 therapeutic class indicators); the bottom panel uses risk deciles based on RxHCC scores and prior year drug costs. The dotted lines represent the current LIS multipliers of 1.08 (full) and 1.05 (partial), respectively.
Discussion
This study examined the performance of the risk adjusted payment scheme in Part D and particularly the low-income subsidy multipliers. We used a large, national sample of Part D beneficiaries enrolled in traditional Medicare. We found that the current subsidy multiplier levels of 1.08 and 1.05 do not adequately account for the differences in actual plan drug spending between subsidy and non-subsidy beneficiaries. Improving the accuracy of the risk adjustment approach, such as by incorporating information on prior prescription drug use into the risk adjustment formula, ameliorated the inadequacy of the LIS multiplier but did not mitigate the need for a corrective multiplier completely.
Inadequate adjustment for subsidy beneficiaries appears to have had predictable and adverse consequences for the low income subsidy beneficiaries; trends over the first four years of the program indicate that fewer plans, including those that offered below-benchmark plans in previous years, now qualify for subsidy assignment, which requires premiums below regional benchmarks.10 Inadequate adjustment for subsidy beneficiaries likely contributes - potentially in a major way - to this trend. In short, an inadequate low-income subsidy multiplier creates an incentive for plans to increase their bids so they are above the anticipated benchmark each year, though this incentive is tempered by potential but unlikely losses of non-subsidy enrollees.22
When repeated year after year, such trends reduce the number of lower priced Part D plans for all beneficiaries and create plan instability for subsidy beneficiaries. In particular, if a plan that was below benchmark bids above benchmark in the following year, subsidy beneficiaries have the choice of paying the additional premium above benchmark, or changing plans (by active choice or reassignment) and almost certainly formularies.9, 10
Part D Market Effects
In the first years of Part D, participating plans had ceilings on both profit and loss because of statutory risk corridors, which by law have widened over time. This increasing risk exposure exacerbates any effects of the differential plan spending between subsidy and non-subsidy beneficiaries - i.e., Prescription Drug Plans may be even less willing to take on low-income subsidy beneficiaries as the government shares less of any losses. Because the benchmark is based on each year’s bids, plans that successfully bid above the expected average each year will avoid being a below-benchmark plan, and thus avoid assignment of subsidy beneficiaries. In other words, the low-income subsidy payment adjustment and assignment process may have contributed to increases in Part D premiums, which is the opposite of the competitive effect originally intended.9, 23
Potential Program Refinements
Prior to the introduction of Part D, it was difficult, if not impossible, to predict the performance of the risk adjusters and the subsidy multipliers, or their impact on the Part D market. The program, however, is now in its fifth year, so adequate data exist for refining the program’s incentives.
Our results, in conjunction with upward trends in Part D premiums and decreasing number of below-benchmark plans, suggest that revisions to the Part D prospective payment approach are urgently needed. These revisions could use one of three general approaches.
First, Medicare could raise the existing low-income subsidy multiplier. This simple approach would mitigate perverse incentives to avoid subsidy beneficiaries. It would not, however, reduce systematic variations in the accuracy of the current risk adjustment approach within the subsidy and non-subsidy populations and thus would not affect plans’ incentives to select favorable risks within each of these populations. In other words, this approach could help address incentives against one segment of the Part D market, but fail to address incentives to select favorable risks within each market segment.
Second, Medicare could develop a separate risk adjustment formula (without prior year drug information) calibrated specifically for subsidy beneficiaries, which Medicare already does for beneficiaries with end stage renal disease. Such an approach could improve the accuracy of payments within both the subsidy and non-subsidy populations, but not necessarily address the incentives with respect to the subsidy market as a whole. To remain budget neutral, both of these first two approaches would require payment reductions for non-subsidy beneficiaries, who constitute about two-thirds of all Part D beneficiaries; the potential consequences of such reductions are unknown. In other words, this approach addresses incentives to select favorable risks within each market segment, but fails to address incentives against the subsidy market.
Third, improving the accuracy of the risk adjustment approach, such as by including information on prior year drug use would remove much of the difference in plan spending between subsidy and non-subsidy beneficiaries, and would also allocate payments across beneficiaries differently than the current process by decreasing the amount of underestimation for high cost beneficiaries and overestimation for low cost beneficiaries. Because risk adjustment will never and should never be completely accurate, some form of correction for differences in plan spending for subsidy and non-subsidy beneficiaries may continue to be needed.
Balancing Competing Incentives with Policy Goals
Any payment or market refinements need to balance policy goals of access, choice, and stability, and address a number of competing incentives. For example, incorporating past costs into future payment calculations abandons fully prospective payment and potentially increases incentives for overuse. It also decreases incentives for cost-effective drug use as plans would effectively be reimbursed some fraction of current drug costs in the following year for those enrollees who remain with the plan. Historically, this has been a major concern of CMS.
Incorporating prior year drug information by using indicators that specify whether beneficiaries took medications in particular therapeutic drug classes instead of factoring in prior-year costs could promote efficiency relative to using past year costs. It might encourage cost-effective prescribing patterns within drug classes, while also reducing incentives for underuse.24 Whatever the refinements, evaluation of the consequences for beneficiary drug adherence, health, and Parts A and B costs is needed.25, 26, 27
While these findings indicate compelling problems with the structure of the Part D market because of the low-income subsidy, CMS should replicate our analyses among all Part D enrollees, as well as in more current time periods. Over time, we also anticipate that some plans might focus on the subsidy market but offer substantially more restricted drug benefits (such as limited formularies or more stringent utilization management, i.e., skimping) than plans participating only in the non-subsidy market. Whether such restricted plans provide adequate access or value for beneficiaries is unknown.
Conclusion
Refining the current risk adjustment approach could ameliorate the current perverse incentive for plans to avoid or shed subsidy beneficiaries, and reduce the market instability that has forced many subsidy beneficiaries into new plans each year. These findings combined with ongoing changes in the Part D low-income subsidy market highlight the critical need to monitor and refine the actual incentives of Part D, as well as to be vigilant for unintended consequences. In effect, post-market surveillance of Medicare policy is needed.28, 29
Acknowledgments
Funding Source
The Medicare Payment Advisory Committee, National Institute on Aging (R01 AG029316), Commonwealth Fund, and the Alfred P. Sloan Foundation provided funding for the study. Neither the funding agencies nor any of the private plans providing data influenced the decision to submit the manuscript for publication. Similarly, the statements in the manuscript are those of the authors, and do not reflect the positions of any of the funding agencies, plans, or institutions in which the authors are affiliated.
Exhibit A1: Performance of Risk Adjustors Relative to Plan Liability
| Risk Adjuster | Non-LIS Subjects |
LIS Subjects | |||
|---|---|---|---|---|---|
| MAPE | Adj R^2 |
MAPE | Adj R^2 |
||
| Demographics | Age+gender | 620 | 0.0108 | 737 | 0.0084 |
| RxHCC | RxHCC (score) | 520 | 0.2056 | 612 | 0.2438 |
| Prior Drug | RxClass (48 indicators) | 406 | 0.4105 | 526 | 0.3833 |
| Information | Cost (annualized) | 420 | 0.4776 | 478 | 0.5687 |
| RxHCC+ Prior Drug |
RxHCC+RxClass (48 indicators) |
403 | 0.4173 | 516 | 0.4118 |
| Use Info | RxHCC+Prior Cost (annualized) |
392 | 0.5225 | 451 | 0.6034 |
Source: Authors’ analysis
Notes: Includes all subjects with at least one month of enrollment in 2006. Cost (annualized) = 12*actual drug expenditure in 2006/months of enrollment in 2006. The MAPE (Mean Absolute Prediction Error) is the average of the absolute difference between the predicted and actual plan liability for each subject.
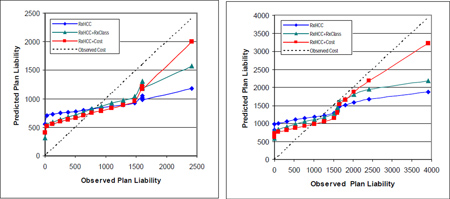
Exhibit A2: Comparison of Predicted Versus Observed Plan Liability, by 5 percentile Groups Based on Observed Liability Among Non-LIS (left panel) and LIS (right panel) Beneficiaries
Source: Author’s analysis
Note: The 45-degree line represents equality between predicted and observed liability; values above the 45-degree line indicate that predicted liability exceeded observed liability for the group and vice versa.
Footnotes
Disclosures
Hsu, Fung, Huang, Price, and Fireman work in the Center for Health Policy Studies, Division of Research, which is located within the Kaiser Permanente Medical Care Program. Hui works at the Kaiser Pharmacy Outcomes Research Group, which also is located within Kaiser Permanente. Kaiser sells Medicare Advantage policies. Dow provides econometric research consultation for the Division of Research. Bertko is a MedPAC commissioner. Newhouse is a director of and holds equity in Aetna, which sells Part D policies.
References
- 1.The Kaiser Family Foundation. Medicare Part D Spotlight: Part D Plan Availability in 2010 and Key Changes Since 2006. Washington D.C.: The Henry J. Kaiser Family Foundation; 2009. Nov 6, [Google Scholar]
- 2.Robst J, Levy JM, Ingber MJ. Diagnosis-based risk adjustment for medicare prescription drug plan payments. Health Care Financ Rev. 2007 Summer;28(4):15–30. [PMC free article] [PubMed] [Google Scholar]
- 3.The Kaiser Family Foundation. Medicare: Low-Income Assistance Under the Medicare Drug Benefit. Washington D.C.: The Henry J. Kaiser Family Foundation; 2009. [Google Scholar]
- 4.Cutler DM, Reber S. Paying for Health Insurance: the Tradeoff Between Competition and Adverse Selection. Quarterly Journal of Economics. 1998 May;:433–466. [Google Scholar]
- 5.Huskamp HA, Rosenthal MB, Frank RG, Newhouse JP. The Medicare prescription drug benefit: how will the game be played? Health Aff (Millwood) 2000;19(2):8–23. doi: 10.1377/hlthaff.19.2.8. [DOI] [PubMed] [Google Scholar]
- 6.Newhouse JP. Risk adjustment: where are we now? Inquiry. 1998 Summer;35(2):122–131. [PubMed] [Google Scholar]
- 7.Newhouse J, Buntin MB, Chapman JD. Risk Adjustment And Medicare: Taking A Closer Look. Health Affairs. 1997;16:26–43. doi: 10.1377/hlthaff.16.5.26. [DOI] [PubMed] [Google Scholar]
- 8.Pauly MV, Zeng Y. Adverse selection and the challenges to stand-alone prescription drug insurance. Front Health Policy Res. 2004;7:55–74. doi: 10.2202/1558-9544.1051. [DOI] [PubMed] [Google Scholar]
- 9.Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Washington D.C.: 2008. Mar, [Google Scholar]
- 10.The Kaiser Family Foundation. Medicare Part D 2009 Data Spotlight: Low-Income Subsidy Plan Availability. Washington D.C.: The Henry J. Kaiser Family Foundation; 2008. Nov, [Google Scholar]
- 11.Changes by the Centers for Medicare and Medicaid Services (CMS) in the method used to calculate the benchmark also have contributed to these trends. Between 2007 and 2008 CMS changed from unweighted to enrollment-weighted benchmarks. CMS established a de minimis rule in an effort to minimize disruptions in plan enrollment for LIS beneficiaries. In 2009 CMS altered the methodology to use LIS enrollment versus all enrollment for weighting. In 2010, the benchmarks were calculated using MAPD premiums before Part A/B rebates were applied. CMS also changed its notification policy in 2010, such that it began notifying all LIS beneficiaries whose plan ceased to be benchmark plans for the upcoming year, meaning that the plan no longer had one of the low available premiums. In 2010, 2.2 million beneficiaries received this notice. Before 2010, CMS only notified the small number of LIS beneficiaries who chose plan, instead of being assigned; if a beneficiary had been assigned, then CMS automatically reassigned the beneficiary.
- 12.Hsu J, Huang J, Fung V, et al. Distributing $800 Billion: An Early Assessment Of Medicare Part D Risk Adjustment. Health Aff. 2009 Jan 1;28(1):215–225. doi: 10.1377/hlthaff.28.1.215. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Supplemental Security Income recipients, and those enrolled in Medicare Savings Programs also are eligible for the full subsidy.
- 14.If a PDP moves from below- to above-benchmark, CMS reassigns its enrollees to another below-benchmark plan via auto- or facilitated enrollment. Those who chose to enroll in their original plan are notified that they can change plans to avoid paying a premium.
- 15.CMS increases the risk adjusted prospective payment by a single multiplier per beneficiary: 1.08 for full subsidy, 1.05 for partial subsidy, 1.21 for institutionalized and disabled, and 1.08 for other institutionalized beneficiaries.
- 16.Meijer E, Karoly LA, Michaud PC. Estimates of Potential Eligibility for Low-Income Subsidies Under Medicare Part D: RAND Corporation. 2009. [Google Scholar]
- 17.Fishman PA, Goodman MJ, Hornbrook MC, Meenan RT, Bachman DJ, O'Keeffe Rosetti MC. Risk adjustment using automated ambulatory pharmacy data: the RxRisk model. Med Care. 2003 Jan;41(1):84–99. doi: 10.1097/00005650-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Shen Y, Ellis RP. How profitable is risk selection? A comparison of four risk adjustment models. Health Econ. 2002 Mar;11(2):165–174. doi: 10.1002/hec.661. [DOI] [PubMed] [Google Scholar]
- 19.If a beneficiary had fewer than 12 months of enrollment in 2006, we annualized 2006 costs by multiplying actual costs by 12 and dividing by the months enrolled (results using alternative definitions for prior year costs were similar)
- 20.Huskamp HA, Stevenson DG, Keating NL, Newhouse JP. Rejections Of Drug Claims For Nursing Home Residents Under Medicare Part D. Health Aff. 2008 Mar 1;27(2):560–567. doi: 10.1377/hlthaff.27.2.560. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Because rebates apply post-hoc and in aggregate, however, they are unlikely to affect our conclusions that subsidy beneficiaries are less profitable than non-subsidy beneficiaries, and that including information on prior drug use or cost in the formula would improve its accuracy
- 22.Neuman P, Strollo MK, Guterman S, et al. Medicare Prescription Drug Benefit Progress Report: Findings From A 2006 National Survey Of Seniors. Health Aff. 2007 Aug 21;:w630–w643. doi: 10.1377/hlthaff.26.5.w630. 2007. [DOI] [PubMed] [Google Scholar]
- 23.Statement by Mark B. McClellan, Centers for Medicare & Medicaid Services On The Medicare Prescription Drug Benefit: House Committee on Ways and Means; Jun 14 2006.
- 24.NORC at the University of Chicago. Continuation of Drug Risk Adjustment December 2006
- 25.Hsu J, Price M, Huang J, et al. Unintended Consequences of Caps on Medicare Drug Benefits. N Engl J Med. 2006 Jun 1;354(22):2349–2359. doi: 10.1056/NEJMsa054436. 2006. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y, Donohue JM, Lave JR, O'Donnell G, Newhouse JP. The effect of Medicare Part D on drug and medical spending. N Engl J Med. 2009 Jul 2;361(1):52–61. doi: 10.1056/NEJMsa0807998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Other features of the Part D program features may have exacerbated the churning of subsidy beneficiaries, including changes in the calculation of benchmarks, and the widening of the risk corridors. These changes or other program features such as reinsurance calculations, reassignment protocols, risk corridors, or formulary regulations also affect the subsidy market stability
- 28.Psaty BM, Burke SP. Protecting the health of the public--Institute of Medicine recommendations on drug safety. N Engl J Med. 2006 Oct 26;355(17):1753–1755. doi: 10.1056/NEJMp068228. [DOI] [PubMed] [Google Scholar]
- 29.Okie S. Safety in numbers--monitoring risk in approved drugs. N Engl J Med. 2005 Mar 24;352(12):1173–1176. doi: 10.1056/NEJMp058029. [DOI] [PubMed] [Google Scholar]