Abstract
Previous research has described variability in menstrual cycle lengths within and across women, though less attention has focused on characterising patterns of bleeding. While clinical definitions for menstrual bleeding are often given in standard textbooks, the validity of conventional definitions has not been empirically evaluated in epidemiological studies. The definition of menstrual bleeding may affect the analysis of time to pregnancy and pregnancy dating that relies upon the last menstrual period. We used daily records of vaginal bleeding from a prospective cohort study that included 74 women trying to become pregnant who reported 430 bleeding episodes. A longitudinal mixture model (PROC TRAJ) was used to classify patterns of bleeding.
Among the first 74 bleeding episodes, 15% comprised only days with spotting or light bleeding (possibly representing non-menstrual bleeding given the length of the cycle defined by these bleeding episodes). When all 430 bleeding episodes were analysed, four distinct bleeding patterns emerged: (1) episodic bleeding comprising 1–3 days of spotting (10%), (2) bleeding lasting 3–6 days (40%), (3) bleeding lasting 6–8 days (33%), and (4) bleeding lasting 8–12 days (17%). These findings suggest that non-menstrual bleeding may be relatively common. Considerable variation in menstrual bleeding patterns is evident, and as such is likely to impact fecundity-related endpoints or gestational age estimates that rely upon menstrual cycle dates. The association between bleeding patterns and female fecundity awaits future research.
Keywords: cycle length, fecundity, gestation, menstruation, time to pregnancy, vaginal bleeding
Introduction
Clinicians and epidemiologists often define a menstrual cycle as the interval from the first day of bleeding in one cycle to the first day of bleeding in the next cycle. Inherent in this definition are two assumptions: (1) that any episodic bleeding, however defined, within this interval is irrelevant for establishing a cycle, and (2) that women can accurately recognise and recall only `real' days of menstrual bleeding when reporting cycle length. Without daily longitudinal capture of vaginal bleeding, it may be impossible to characterise menstrual cycle patterns to determine their relationship with female fecundity.
A number of important papers have focused on the variability of menstrual cycle length and duration of menstrual bleeding both within and between women in an attempt to understand the sources of such variation and its eventual meaning for female fecundity.1–6 However, specific attention to episodic bleeding or spotting in assessing variability is noticeably absent. Such bleeding was suggested to be indicative of ovulation,7 transitory hormonal disturbances or anatomical causes.8,9 Also, bleeding associated with implantation may affect pregnancy dating and reported time to pregnancy.10–12 To our knowledge, no attempt has been made to characterise variation in vaginal bleeding using daily data on bleeding and its intensity. The aim of this analysis is to determine patterns of menstrual bleeding based upon longitudinal measurement of bleeding patterns in a cohort of women trying to become pregnant.
Methods
Study design and sample
The analysis utilises data from a subcomponent of the New York State Angler Cohort Study (NYSACS).13 Specifically, women who previously participated in the NYSACS were recontacted in 1996–97 to ascertain their eligibility for a prospective pregnancy study, i.e. planning to discontinue contraception, aged 18–40 years and having no physician-diagnosed infertility. Ninety-nine women participated in the study. However, 25 women became pregnant in cycle 0 or 1 and were excluded because this study requires a minimum of two prospectively observed bleeding episodes and these women did not have them. As a result, 430 bleeding episodes contributed by 74 women were available for analysis. Thirty-nine (53%) women contributed 4 or fewer bleeding episodes while the remaining 35 (47%) women contributed up to 21 bleeding episodes. Women who were included in the sample did not differ from the 25 remaining women in the original sample in terms of age, number of living children, or observed menstrual cycle length or bleeding duration (Table 1).
Table 1.
Comparison of women from the original study who were included and excluded from this analysis
| Characteristic | Included n = 74 | Excluded n = 25 | P-valuea |
|---|---|---|---|
| Age mean (SD) | 30.0 (2.4) | 30.2 (2.6) | 0.67 |
| Number living children, mean (SD) | 0.9 (0.8) | 1.2 (0.8) | 0.17 |
| Menstrual cycle irregularb | 9.5% | 16.0% | 0.37 |
| Cycle length, mean (SD)b | 28.5 (2.5) | 28.9 (2.1) | 0.53 |
| Bleeding duration, mean (SD)b | 4.9 (1.5) | 4.8 (1.3) | 0.71 |
Wilcoxon or chi-squared test, two-sided.
As reported at baseline interview for describing menstruation during the past 12 months.
Data collection
Consenting women were interviewed by a research nurse to capture their medical and reproductive history, environmental exposures and selected lifestyle factors during the previous 12 months believed relevant for human fecundity. Subsequently, the nurse instructed the women in the proper use of home pregnancy test kits and daily diaries that were designed to capture all vaginal bleeding (including any spotting), sexual intercourse and relevant time-varying covariates (i.e. cigarette smoking, alcohol and caffeine consumption, vitamin use and consumption of sport fish from environmentally contaminated water bodies). The daily information was collected on pre-addressed and postage-paid cards, which were mailed weekly. The research nurse monitored compliance and prompted women by telephone when cards were delayed by one week.
Operational definitions
Characteristics of the women were obtained from the baseline interview. Information about vaginal bleeding or spotting was obtained from the daily diary. No a priori definition of menstruation was provided for participating women. The daily diary asked women to record and quantify all vaginal bleeding and spotting irrespective of expected menses as follows: 0 (none), 1 (spotting), 2 (light bleeding), 3 (moderate bleeding), or 4 (heavy bleeding). Data collection was censored according to pregnancy outcomes: the day following the first positive pregnancy test for women giving birth; the day following a pregnancy loss for women with spontaneous losses; and the day following completion of 12 menstrual cycles determined to be at risk for pregnancy given the occurrence of one or more acts of sexual intercourse during the predefined fertile window based on the Ogino-Knaus method.14,15 In the current analysis, we restricted bleeding records to bleeding observed before the first positive pregnancy test, thus excluding any bleeding during pregnancy.
We defined any days of bleeding as a bleeding episode. When days with bleeding were separated by a single non-bleeding day, they were still treated as a single bleeding episode. Inter-bleeding intervals were defined as two or more consecutive days without any bleeding. When daily records started or ended on days of bleeding, the corresponding bleeding episodes were excluded, as it was not clear how long they lasted before or after the records. For purposes of this study, we use the term `non-menstrual bleeding' to denote bleeding episodes not meeting the definition of menstruation. Menstruation was defined as bleeding followed by an inter-bleeding interval consistent with an ovulatory cycle lasting 20 or more days from the first day of the bleeding to the last day before next bleeding.16
Statistical analysis
For the epidemiological description of the duration of bleeding of different intensities, we used only one (the first completely recorded) bleeding episode per woman (n = 74). In the next step, we used all available bleeding episodes (n = 430) to investigate the effects of defining menstruation as a bleeding episode with specific characteristics on the distribution of inter-bleeding interval lengths. The following definitions of bleeding episodes were used: those with days of any bleeding, days with at least light bleeding, days with at least moderate bleeding and days with just heavy bleeding. We assessed the relation between bleeding duration and intensity score (intensity of bleeding summed up across the days of bleeding) graphically. We further investigated whether there were distinct categories of bleeding episodes. This analysis was based on a longitudinal mixture model investigating the clustering of trajectories defined by bleeding intensity on consecutive days of the bleeding episode. The respective algorithm is implemented in PROC TRAJ in SAS.17 The optimal number of clusters was defined based on Bayesian Information Criterion, following general recommendations.17
Results
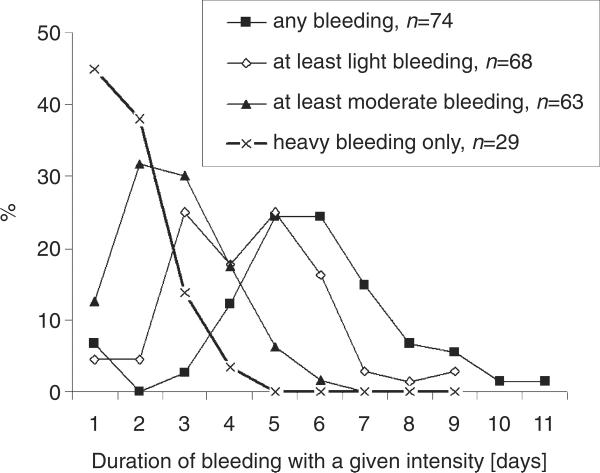
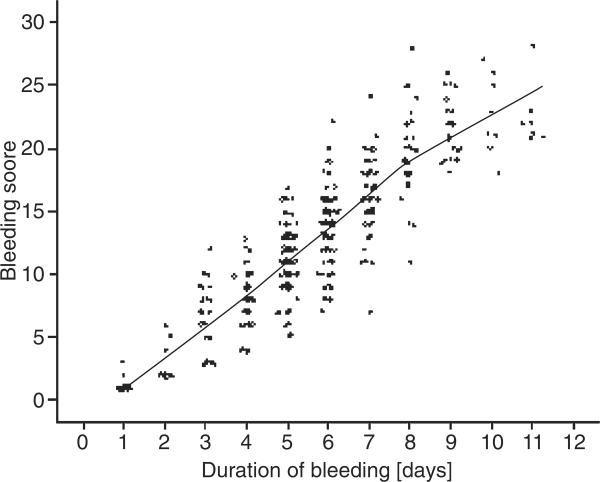
Among the first 74 bleeding episodes recorded in the study, (i) 6 (8%) episodes comprised only spotting, (ii) 5 (7%) episodes included days of light bleeding but no moderate or heavy bleeding, (iii) 32 (43%) episodes included days of moderate bleeding but no heavy bleeding, and (iv) 29 (39%) episodes included days of heavy bleeding. The duration of heavy bleeding was typically 1–2 days; at least moderate bleeding was typically 2–3 days while at least light bleeding was typically 3–6 days (Fig. 1). Using any reported bleeding, the duration of bleeding episodes was typically 4–7 days. Bleeding score (intensity integrated over the duration of bleeding) increased in a linear fashion with increasing duration of bleeding, indicating that shorter bleeding episodes are not compensated by a greater bleeding intensity (Fig. 2).
Figure 1.
Distribution of the duration of episodes defined by different bleeding intensity.
Figure 2.
Association between duration of bleeding and bleeding score combining duration and intensity. (NOTE: Points represent individual records while the line represents a locally weighted regression.)
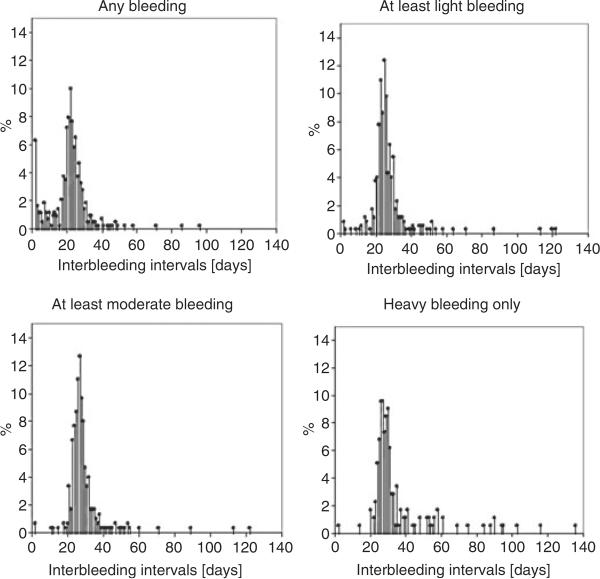
Defining menstruation as bleeding episodes containing moderate to heavy bleeding ensured that inter-bleeding intervals cumulated mostly in the expected range of 20–40 days (Fig. 3). On the contrary, allowing for bleeding episodes containing only light bleeding (or with spotting or spotting alone) resulted in a substantial fraction of unlikely short inter-bleeding intervals. Specifically, the graph for any bleeding and at least light bleeding is different from the graphs for the other two patterns in Fig. 3.
Figure 3.
Distribution of inter-bleeding intervals by definition of menstruation as bleeding episodes containing days with: any bleeding, at least light bleeding, at least moderate bleeding and heavy bleeding only.
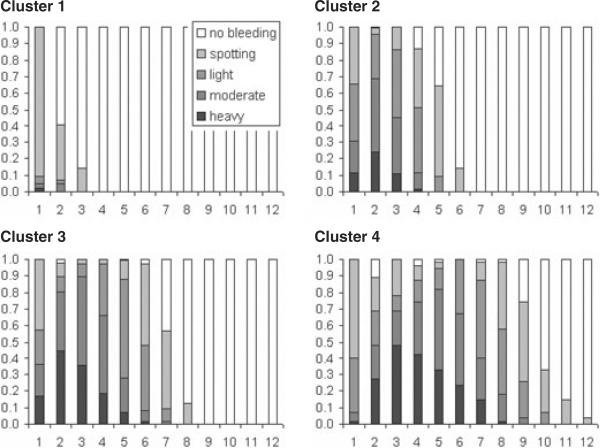
Using the mixture model and all data to classify bleeding episodes according to how the intensity of bleeding changes during the consecutive days of bleeding, four distinct bleeding patterns were identified (Fig. 4). In the first cluster, there were bleeding episodes comprising 1–3 days of spotting (10% of analysed episodes). The second cluster is characterised by bleeding episodes lasting from 3 to 6 days (40%), the third cluster as bleeding episodes lasting from 6 to 8 days (33%), and the fourth cluster as lasting from days 8 to 12 (17%). In clusters 3 and 4, the bleeding days were sometimes interrupted by non-bleeding days as reflected by the white proportion of the histogram bars. Also in clusters 3 and 4, the day with maximal intensity of bleeding was increasingly delayed with respect to the beginning of the bleeding episode (i.e. the second or third day for cluster 3 but days 3–5 for cluster 4). Single days of spotting separated from the preceding or following bleeding days by a single non-bleeding day occurred more frequently at the beginning than at the end of a bleeding episode (data not shown). While cluster 1 can be nearly unequivocally interpreted as spotting episodes, the remaining clusters display bleeding intensity and duration consistent with clinical understanding of menstrual bleeding. Clusters 2 and 3 show a similar beginning of the bleeding episode, and differ only by its duration. Cluster 4 contains bleeding episodes starting with lower intensity, building up towards highest bleeding intensity and slowly declining again. All three clusters 2–4 demonstrated a crescendo – decrescendo pattern for bleeding intensity.
Figure 4.
Intensity of bleeding on consecutive days during bleeding episodes from different clusters (x-axis: consecutive days of bleeding; y-axis: proportion of bleeding episodes in the cluster).
Discussion
We observed a substantial amount of variability in both the duration and intensity of vaginal bleeding episodes among women trying to get pregnant who were participating in a prospective study with daily capture of any vaginal bleeding. Non-menstrual bleeding as presumed based on the subsequent interval until next bleeding occurred frequently (8% of first observed bleeding episodes belonged in this category).
While we found many more bleeding episodes than one would expect if all were truly menstrual, we did not attempt to distinguish which of these bleeding episodes could be correctly recognised by the woman as non-menstrual. This perspective may overestimate the extent of the problem, as an individual woman, based on recurrent patterns of bleeding and additional symptoms, may be able to differentiate non-menstrual bleeding from menstruation. In this cohort study, women were asked to use pregnancy test kits on the day of expected menstruation. We hoped this additional information would allow us to understand which days of bleeding were regarded by the women as menstrual, but women frequently tested their urines in the second half of their cycle and not just on the expected day of menses as the protocol requested.
We also found an association between menstrual cycle length and intensity of bleeding arguing against a compensatory mechanism of higher intensity of bleeding in short bleeding episodes. As our data did not contain a more objective measurement of bleeding intensity, such as the number of tampons or sanitary pads used, it is possible that the association was partly caused by women's perceptions that longer bleeding is also more severe. Previous research cautioned against subjective measurement of the intensity of bleeding,18 but much of this criticism was related to retrospectively reported data. However, a high intensity and long duration of bleeding may be caused by underlying gynaecological pathology such as endometriosis or uterine fibroids.18 One previous study of adolescents reported changes with regard to bleeding intensity with age.16 In this study of adolescents the percentage of light and severe bleeding decreased with age; our findings add information that there is a substantial variation in bleeding intensity among adult women. We further recognise the potential for any prospective pregnancy study to over-represent less fecund women (or couples) and, if subfecundity is associated with a higher fraction of bleeding abnormalities, also to overestimate the frequency of the latter. The expected time to pregnancy distribution and incidence of pregnancy loss for this cohort argues against this possibility.19
Our study has some important limitations. The clinical interpretation of different categories of bleeding episodes obtained in our study is not clear. Recent efforts in the field of obstetrics and gynaecology to harmonise such terminology have not addressed the relationship between bleeding and fecundity.18 We were not able to study the association between patterns of bleeding and time to pregnancy, given our limited cohort size, which also affected the precision of estimated fractions and prohibited a more detailed analysis, for example, regarding consecutive bleeding episodes. Clinical research focuses less on episodic bleeding than on heavy menstrual bleeding apart from the assessment of hormonal control of ovulation.8 Our findings suggest that a relatively large percentage of women (8% of first recorded bleeding episodes) experience spotting. This emphasises the importance of continued efforts to delineate the association between bleeding patterns and fecundity.20,21
Our findings are important for investigators interested in the evaluation of potential reproductive toxicants, as duration and intensity of bleeding is frequently a study outcome and often dependent upon retrospective report. Previous work has utilised the conventional definition of a menstrual cycle while ignoring other bleeding during the cycle. In addition, many of the environmental exposures reported to adversely affect menstrual function by shortening or lengthening the inter-bleeding interval or bleeding duration are within error ranges arising from misinterpretation of non-menstrual bleeding as menstruation and, thus, ignore dysfunctional bleeding.20,21 Contrarily, our findings add perspective for clinicians who typically rely on self-reported menstrual bleeding for estimating gestation, in deciding when a couple should seek infertility-related treatment or for responding to menstrual cycle-related complaints. These data suggest the continued need for research on the menstrual cycle, particularly in characterising patterns and their meaning for female fecundity or gynaecological pathology.
Our results pertaining to menstrual bleeding patterns must await corroboration in the light of our limited sample size and the lack of an objective measurement of bleeding intensity. Also, they need to be interpreted with the caveat that the cohort may over-represent less fecund women (or couples), given the exclusion of women becoming pregnant in cycles 0 and 1 as they did not have at least two complete bleeding episodes prospectively measured. We did attempt to address this last important limitation in the original study by using self-reported menstrual cycle data for the past 12 months before enrolment into the cohort, and found no significant differences in the reported duration of cycles between women included in the analysis and those not included.
In sum, defining a menstrual cycle for the purposes of research requires more attention to the typology of bleeding patterns including episodic bleeding. Continued reliance on overly simplistic definitions such as `day one' to `day one' may hinder a better understanding of the biological relevance of menses and female fecundity and later onset adult diseases.
Acknowledgement
This study was supported by the Intramural Research Program at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, Bethesda, MD, USA. Dr Mikolajczyk's work was performed during a postdoctoral fellowship at the Epidemiology Branch of the above institute.
References
- 1.Harlow SD, Lin X, Ho MJ. Analysis of menstrual diary data across the reproductive life span applicability of the bipartite model approach and the importance of within-woman variance. Journal of Clinical Epidemiology. 2000;53:722–733. doi: 10.1016/s0895-4356(99)00202-4. [DOI] [PubMed] [Google Scholar]
- 2.Guo Y, Manatunga AK, Chen S, Marcus M. Modeling menstrual cycle length using a mixture distribution. Biostatistics. 2006;7:100–114. doi: 10.1093/biostatistics/kxi043. [DOI] [PubMed] [Google Scholar]
- 3.Meyer PM, Zeger SL, Harlow SD, Sowers M, Crawford S, Luborsky JL, et al. Characterizing daily urinary hormone profiles for women at midlife using functional data analysis. American Journal of Epidemiology. 2007;165:936–945. doi: 10.1093/aje/kwk090. [DOI] [PubMed] [Google Scholar]
- 4.Small CM, Manatunga AK, Klein M, Feigelson HS, Dominguez CE, McChesney R, et al. Menstrual cycle characteristics: associations with fertility and spontaneous abortion. Epidemiology. 2006;17:52–60. doi: 10.1097/01.ede.0000190540.95748.e6. [DOI] [PubMed] [Google Scholar]
- 5.Wilcox AJ, Dunson DB, Weinberg CR, Trussell J, Baird DD. Likelihood of conception with a single act of intercourse: providing benchmark rates for assessment of post-coital contraceptives. Contraception. 2001;63:211–215. doi: 10.1016/s0010-7824(01)00191-3. [DOI] [PubMed] [Google Scholar]
- 6.Harlow SD, Zeger SL. An application of longitudinal methods to the analysis of menstrual diary data. Journal of Clinical Epidemiology. 1991;44:1015–1025. doi: 10.1016/0895-4356(91)90003-r. [DOI] [PubMed] [Google Scholar]
- 7.Lynch CD, Zhang J. The research implications of the selection of a gestational age estimation method. Paediatric and Perinatatal Epidemiology. 2007;21(Suppl. 2):86–96. doi: 10.1111/j.1365-3016.2007.00865.x. [DOI] [PubMed] [Google Scholar]
- 8.Livingstone M, Fraser IS. Mechanisms of abnormal uterine bleeding. Human Reproduction Update. 2002;8:60–67. doi: 10.1093/humupd/8.1.60. [DOI] [PubMed] [Google Scholar]
- 9.Ferenczy A. Pathophysiology of endometrial bleeding. Maturitas. 2003;45:1–14. doi: 10.1016/s0378-5122(03)00068-9. [DOI] [PubMed] [Google Scholar]
- 10.Harville EW, Wilcox AJ, Baird DD, Weinberg CR. Vaginal bleeding in very early pregnancy. Human Reproduction. 2003;18:1944–1947. doi: 10.1093/humrep/deg379. [DOI] [PubMed] [Google Scholar]
- 11.Speert H, Guttmacher AF. Frequency and significance of bleeding in early pregnancy. JAMA. 1954;155:712–715. doi: 10.1001/jama.1954.03690260004002. [DOI] [PubMed] [Google Scholar]
- 12.Gjessing HK, Skjaerven R, Wilcox AJ. Errors in gestational age: evidence of bleeding early in pregnancy. American Journal of Public Health. 1999;89:213–218. doi: 10.2105/ajph.89.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vena JE, Buck GM, Kostyniak P, Mendola P, Fitzgerald E, Sever L, et al. The New York Angler Cohort Study: exposure characterization and reproductive and developmental health. Toxicology and Industrial Health. 1996;12:327–334. doi: 10.1177/074823379601200305. [DOI] [PubMed] [Google Scholar]
- 14.Ogino K. Ovulationstermin und Konzeptionstermin. Zentralblatt für Gynäkologie. 1930;54:464–479. [Google Scholar]
- 15.Knaus H. Eine neue Methods zur Bestimmung des Ovulationstermines. Zentralblatt für Gynäkologie. 1929;53:2193–2202. [Google Scholar]
- 16.Flug D, Largo RH, Prader A. Menstrual patterns in adolescent Swiss girls: a longitudinal study. Annals of Human Biology. 1984;11:495–508. doi: 10.1080/03014468400007411. [DOI] [PubMed] [Google Scholar]
- 17.Jones BS, Nagin DS, Roeder K. A SAS procedure based on mixture models. Sociological Methods and Research. 2001;29:374–393. [Google Scholar]
- 18.Woolcock JG, Critchley HO, Munro MG, Broder MS, Fraser IS. Review of the confusion in current and historical terminology and definitions for disturbances of menstrual bleeding. Fertility and Sterility. 2008;90:2269–2280. doi: 10.1016/j.fertnstert.2007.10.060. [DOI] [PubMed] [Google Scholar]
- 19.Buck Louis GM, Dmochowski J, Lynch C, Kostyniak P, McGuinness BM, Vena JE. Polychlorinated biphenyl serum concentrations, lifestyle and time-to-pregnancy. Human Reproduction. 2009;24:451–458. doi: 10.1093/humrep/den373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Toft G, Hagmar L, Giwercman A, Bonde JP. Epidemiological evidence on reproductive effects of persistent organochlorines in humans. Reproductive Toxicology. 2004;19:5–26. doi: 10.1016/j.reprotox.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Buck Louis GM, Lynch CD, Cooney MA. Environmental influences on female fecundity and fertility. Seminars in Reproductive Medicine. 2006;24:147–155. doi: 10.1055/s-2006-944421. [DOI] [PubMed] [Google Scholar]