Abstract
Aims
The Marijuana Treatment Project, a large multi-site randomized clinical trial, compared a delayed treatment control condition with a brief (two-session) and extended (nine-session) multi-component treatment among 450 marijuana-dependent participants. In this report we present treatment process data, including the fidelity of treatment delivery in the three community-based treatment settings as well as the relationships between treatment process and outcome.
Design
Independent evaluations of clinician adherence and competence ratings were made based on 633 videotaped sessions from 163 participants. Relationships between clinician adherence and competence, ratings of the working alliance and marijuana treatment outcomes were evaluated.
Findings
Protocol treatments were implemented with strong fidelity to manual specifications and with few significant differences in adherence and competence ratings across sites. In the brief two-session treatment condition, only the working alliance was associated significantly with frequency of marijuana use, but in the extended treatment therapist ratings of working alliance predicted outcomes, as did the interaction of alliance and curvilinear adherence.
Conclusions
Behavioral treatments for marijuana use were delivered in community settings with good fidelity. Participant and therapist working alliance scores were associated significantly with improved marijuana use outcomes in a brief behavioral treatment for adults with marijuana dependence. In extended treatment the therapist ratings of working alliance were associated with more positive outcome. However, in that treatment there was also a significant interaction between alliance and curvilinear adherence.
Keywords: Alliance, behavioral treatment, brief treatment, marijuana dependence, Marijuana Treatment Project, treatment process
INTRODUCTION
Marijuana is the most commonly used illicit substance in the United States and accounts for more substance use disorders than any other drug [1–4]. Marijuana use accounts for an increasingly large number of treatment admissions in the United States [5]. Nevertheless, comparatively little is known regarding the efficacy of treatment for marijuana use disorders. Reports from randomized clinical trials evaluating behavioral interventions for marijuana use disorders have begun to appear within the past 15 years [6–9], and generally support the efficacy of those behavioral approaches demonstrated previously to be efficacious for other substance use disorders, including motivational interviewing, cognitive–behavioral approaches and contingency management [10–12].
The Marijuana Treatment Project (MTP) [13] was a large, multi-site randomized controlled trial evaluating the efficacy of brief approaches [9] to marijuana treatment in a diverse patient population. Four hundred and fifty marijuana-dependent individuals were assigned randomly to: (1) a delayed treatment control condition; (2) a two-session brief intervention emphasizing motivational interventions; or (3) a nine-session intervention that integrated motivational enhancement therapy (MET), cognitive–behavioral therapy (CBT) and case management (CM). Regarding treatment outcomes, the group assigned to the nine-session treatment reduced marijuana use significantly more than the group assigned to the two-session treatment, and both groups improved significantly more than those assigned to the delayed treatment control group [13]. Although MTP was a rigorous multi-site trial of manual-guided treatments for marijuana dependence, it was significant in that it also included several design elements intended to enhance the real-world applicability of findings, including the use of community-based settings with diverse patient populations, and study clinicians drawn from the staff at those clinics [14]. This study thus provides an opportunity to address important questions regarding whether treatment integrity can be protected in the context of trials that place greater emphasis on external validity [14]. The first aim of this report is to evaluate the extent to which study treatments were implemented in accordance with manual guidelines and with sufficient fidelity and skill. We anticipated that, as defined in the treatment manuals, there would be a high degree of MET-consistent interventions applied in both the two- and nine-session treatments (i.e. high MET adherence), and that the degree of CBT consistent interventions would increase over time for the nine-session treatment. We also anticipated that using a centralized training strategy would result in limited variability in treatment implementation (mean adherence and skill levels) across sites.
The second aim of this report is to examine process–outcome relationships in these treatments. There has been little investigation to date of the relationship between treatment adherence, therapist competence and the working alliance in predicting drug use outcomes. When adherence has been assessed, in general there has been inconsistent evidence of strong relationships between treatment adherence and outcome [15,16]. However, in a recent evaluation of process–outcome relationships in cocaine treatment, Barber and colleagues [17] reported an interaction effect between alliance and adherence, suggesting a curvilinear relationship between adherence and alliance on treatment outcome. When the working alliance was strong, therapist adherence appeared to have little impact on treatment outcome, but when it was poor, adherence was associated strongly with outcome. Thus, using data from the MTP, we aimed to evaluate the extent to which therapist adherence and competence in delivering treatment, ratings of the working alliance and their interactions were associated with marijuana use outcomes.
METHODS
Overview of design
Detailed information about the study design, methods, treatments and main treatment outcomes have been provided in previous reports [13,18–20]. The study was conducted at three out-patient community-based sites. At each site, 150 participants were assigned randomly to one of three treatment conditions. The study treatments were manual-guided [19] and implemented over a 12-week (for extended treatment) or 5-week (for brief treatment) period.
Participants
Individuals were eligible for the study if they were 18 years of age or older, had a DSM-IV diagnosis of current marijuana dependence and used marijuana on at least 40 of the 90 days prior to screening. Participants were excluded if they had a current DSM-IV diagnosis of dependence on another drug or alcohol. Demographic information for the 450 participants who were randomized to treatment can be found in a previous report [15].
Treatments
Two-session intervention
The two-session intervention was delivered 1 week and 4 weeks following randomization, with a primary emphasis on MET and secondary emphasis on introducing coping skills.
Nine-session intervention
The nine-session intervention was delivered over a 12-week period. The first two sessions were intended to be similar to the first two sessions of the two-session intervention. These were followed by seven additional sessions that integrated elements of CBT and CM. Clinicians were encouraged to use a MET interactional style throughout treatment. The CM interventions were intended to broaden the treatment’s capacity to meet the needs of a diverse population by helping participants with psychosocial problems to recognize practical barriers to stopping marijuana use, and to develop strategies to reduce those problems.
Clinicians and training
Clinician training and monitoring was based on methods used in previous multi-site trials for addiction [21,22]. As described in the main outcome paper [15], clinicians participated in a 2½-day didactic seminar, and were assigned four training cases (two nine-session and two two-session). Training sessions were videotaped for review, process ratings and supervision. During the main phase of the trial, all treatment sessions were videotaped for ongoing supervision.
Eleven clinicians were trained and certified to perform both study treatments. Ninety-one percent had master’s degrees; 9% had bachelor’s degrees. Six (55%) were female, all were Caucasian, and their average age was 44 years. Clinicians reported an average of 8.7 years of clinical experience, and most reported that they had had some previous exposure to motivational interviewing (73%), cognitive–behavioral therapy (82%) or case management (82%). Thus, these clinicians are similar to clinicians in other community-based settings participating in clinical research in the United States [23,24].
Assessments
Participant assessments
Diagnoses of substance abuse and dependence were determined by means of the Structured Clinical Interview for DSM-IV (SCID) [25]. The baseline and follow-up interviews also included the Addiction Severity Index (ASI) [26] and the Time-Line Follow-Back (TLFB) interview [27] was used to measure the frequency and pattern of marijuana use.
Process assessments
The Yale Adherence and Competence Rating Scale (YACS) [28] was used to assess therapist adherence (levels of delivery of manual-specified interventions) and competence (skill in delivering intervention). The YACS has been validated, refined and used in multiple studies and shown be highly sensitive to variations in process and its ability to detect differences across treatment settings and treatment approaches [11,29–33]. The YACS is comprised of multiple scales; several scales assess interventions common to many behavioral treatments for substance use disorders (e.g. assessment of substance use and general functioning, provision of support), while other scales are treatment-specific (e.g. interventions associated with treatments such as CBT, MET, Twelve-Step facilitation).
For each item, raters use two seven-point Likert-type scales: first, they rate the extent to which the intervention was present in the session (adherence rating), with scores ranging from [1] ‘intervention did not occur’ to [7] ‘present to a very high degree/dominated the session’. Secondly, they rate the skill with which the clinician delivered the intervention (competence rating), with scores ranging from ‘very poor’ [1] to ‘excellent’ [7]. The YACS has been found to be reliable in previous studies, with a mean intraclass correlation coefficient (ICC) estimate of 0.87 for the adherence dimension and a mean ICC estimate of 0.86 for the competence dimension across scales [28,34,35]. For the present study, five YACS scales were used; three treatment-specific (MET, CBT, CM) and two general (structure and facilitative conditions) scales.
Independent YACS ratings were completed using session tapes from one-half of the randomized sample (77 of the 146 participants assigned to the two-session treatment; 86 of the 156 participants assigned to the nine-session treatment). All available sessions for these participants were rated, resulting in a process evaluation sample of 633 sessions from 163 participants. Process raters were eight master’s level clinicians who had participated in the original psychometric evaluations of the YACS and multiple process evaluation studies in the past. Raters were blind to the participants’ treatment assignment and were trained through review of the rating manual and several practice ratings to achieve consensus.
The working alliance was evaluated using the client and therapist versions of the Working Alliance Inventory (WAI), administered after session 2 [36]. The WAI has been shown to have good factor structure, reliability, concurrent and predictive validity in several studies, including those with substance users [37–39]. Session 2 is a commonly used time-point for measuring the alliance, and scores collected at this time-point have been shown previously to predict treatment outcome [29].
Data analysis
To evaluate the psychometric properties of the adapted YACS, inter-rater reliability was evaluated using intraclass correlation coefficients (ICCs) on nine randomly selected sessions that were rated by all eight raters (e.g. a complete block design). With eight raters and an expected ICC of 0.85, we calculated the approximate number of subjects required with an alpha of 0.05 and a confidence interval width of 0.3 using the Bonett formula for ICC sample size estimation [40]. The sample size approximation came to 8. Simple correlations were used to evaluate relationships among and between the adherence and competence scales of the YACS. Simple correlations and analysis of variance (ANOVA) models were used to evaluate relationships of specific process variables (e.g. YACS and WAI scores) with treatment outcome (e.g. frequency of marijuana use, operationalized as percentage of days of marijuana use). Random regression models [41] were used to evaluate change in YACS scores over time and relationships between YACS, WAI, and marijuana use outcome measures.
RESULTS
Psychometric evaluation of the adherence/competence scale
Using the Shrout & Fleiss [42] fixed-effects model to estimate inter-rater reliabilities for independent samples, the five YACS scales were found to be reliable. Intraclass correlation coefficients ranged from 0.75 to 0.95 for the adherence dimension and from 0.85 to 0.91 for the competence dimension across the scales. Confirmatory factor analyses using the adherence dimension indicated that the hypothesized structure of the scales resulted in good-fitting models for all scales. The five adherence scales satisfied the criteria for evaluating goodness of fit GFI) [e.g. χ2/degrees of freedom ratio of less than 2, all had GFI and comparative fit (CFI) indices of 0.9 or above] [43].
Fidelity: clinician adherence and competence
In order to compare directly session content for the two treatments, Table 1 presents YACS ratings for the two-and nine-session treatments for both the adherence and competence dimensions. For session 1, mean CBT adherence scores were significantly higher in the two-session treatment than the nine-session treatment and structure (STR) scores were significantly higher in the nine-session treatment than the two-session treatment. MET, CM and facilitative condition (FC) scores were not significantly different by condition. On the competence dimension for session 1, both MET and STR scores were higher for the nine-session treatment than the two-session treatment, and there were no differences in CBT, FC or CM competence by treatment. There were no significant differences in session 2 scores by condition for either the competence or adherence dimensions of any of the scales. Overall, these ratings compare favorably with ratings obtained by previous multi-site trials of CBT and MET involving doctoral-level therapists [28,34,44].
Table 1.
Adherence and competence scores in sessions 1 and 2 by treatment condition.
| Brief treatment (2-session)
|
Extended treatment (9-session)
|
F | df | P | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Session 1, brief treatment n = 77, extended treatment n = 86 | |||||||
| Adherence (quantitative) ratings | |||||||
| CBT | 2.46 | 0.83 | 2.08 | 0.81 | 8.89 | 1161 | 0.00 |
| MET | 3.50 | 0.79 | 3.59 | 0.92 | 0.38 | 1161 | 0.54 |
| CM | 1.24 | 0.39 | 1.37 | 0.56 | 2.61 | 1161 | 0.11 |
| FC | 3.17 | 0.79 | 3.30 | 0.78 | 1.18 | 1161 | 0.28 |
| STR | 3.03 | 0.59 | 3.38 | 0.64 | 13.06 | 1151 | 0.00 |
| Competence (qualitative) ratings | |||||||
| CBT | 3.97 | 0.51 | 3.93 | 0.78 | 0.11 | 1152 | 0.74 |
| MET | 4.18 | 0.48 | 4.38 | 0.77 | 3.96 | 1160 | 0.05 |
| CM | 3.90 | 0.75 | 3.86 | 0.92 | 0.03 | 172 | 0.86 |
| FC | 4.19 | 0.47 | 4.35 | 0.75 | 2.53 | 1161 | 0.11 |
| STR | 4.16 | 0.40 | 4.36 | 0.77 | 4.12 | 1161 | 0.04 |
| Session 2, brief treatment n = 44, extended treatment n = 76 | |||||||
| Adherence (quantitative) ratings | |||||||
| CBT | 2.36 | 1.00 | 2.15 | 0.76 | 1.65 | 1118 | 0.20 |
| MET | 2.95 | 0.95 | 2.72 | 1.04 | 1.38 | 1118 | 0.24 |
| CM | 1.46 | 0.70 | 1.47 | 0.77 | 0.00 | 1118 | 0.94 |
| FC | 3.73 | 0.86 | 3.54 | 0.89 | 1.31 | 1118 | 0.25 |
| STR | 2.88 | 0.72 | 2.88 | 0.83 | 0.16 | 1118 | 0.69 |
| Competence (qualitative) ratings | |||||||
| CBT | 3.89 | 0.70 | 3.87 | 0.80 | 0.02 | 1113 | 0.89 |
| MET | 4.09 | 0.64 | 4.04 | 0.77 | 0.14 | 1114 | 0.70 |
| CM | 4.04 | 0.84 | 4.00 | 1.03 | 0.03 | 159 | 0.86 |
| FC | 4.15 | 0.65 | 4.14 | 0.62 | 0.01 | 1118 | 0.94 |
| STR | 4.06 | 0.59 | 3.99 | 0.64 | 0.31 | 1118 | 0.58 |
CBT: cognitive–behavioral therapy scale; MET: motivational enhancement therapy scale; CM: case management scale; FC: facilitative conditions scale; SD: standard deviation; STR: structure scale. Scores range from 1 to 7, with higher scores indicating higher levels of adherence or competence.
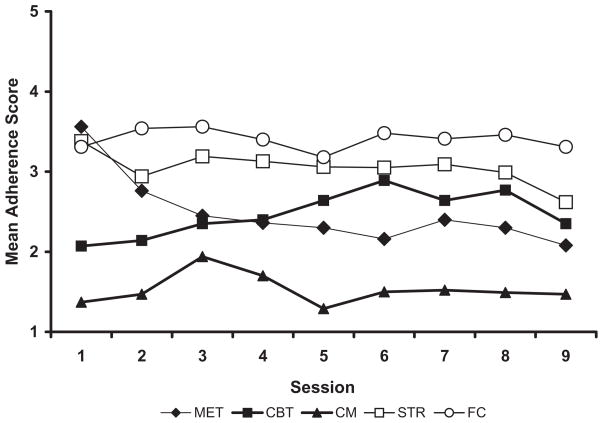
Random effect regression analyses were used to evaluate change in adherence scores over time for the 86 participants in the nine-session treatment (raw data are presented in Fig. 1). There were significant effects for time for the MET (t(484) = −8.32, P < 0.01), CBT (t(478) = 6.4, P < 0.01) and STR scales (t(487) = −3.34, P < 0.01), suggesting significant decreases in MET and STR scores over time and increases in CBT scores over time, which was consistent with manual guidelines and our hypotheses. Effects of time for the CM and FC scales were not significant, indicating that delivery of these elements was comparatively stable across time.
Figure 1.
Mean adherence scores across time, extended (nine-session) treatment; n = 86. MET: motivational enhancement therapy scale; CBT: cognitive-behavioral therapy scale; CM: case management scale; STR: structure scale; FC: facilitative conditions scale.
Mean CM scores were comparatively low across time (although they peaked early in treatment, as prescribed in the manual). Exploratory analyses suggested that these interventions were used as intended, and there was a strong relationship between pretreatment ASI composite scores and delivery of CM, where participants who had a mean CM score of 2 or more had significantly higher baseline ASI psychological composite scores than those with lower mean CM scores (mean baseline ASI psychological composite 0.30 versus 0.12, F = 11.58, P = 0.001) and ASI employment composite scores (mean 0.44 versus 0.24, F = 9.20, P = 0.003). That is, there appears to have been a relationship between baseline severity and therapist application of CM whereby participants who had more severe symptoms at baseline were treated with more CM.
In terms of YACS ratings for the two-session treatment, CM, structure (STR) and facilitative conditions (FC) adherence scores increased from session 1 to session 2 (n = 44, P = 0.05) and, as anticipated, MET scores decreased between the two sessions (3.6 to 2.9, F = 11.70, P = 0.00, df = 1,43).
Site differences
Site differences were evaluated using ANOVA models and are presented in Table 2. For the adherence scales, there were no significant site effects in the two-session treatment. There were two statistically significant site effects for the nine-session treatment, where mean MET and FC
Table 2.
Mean adherence and competence ratings by site.
| Site 1
|
Site 2
|
Site 3
|
F | df | P | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||||
| 2-session treatment, adherence dimension | |||||||||
| CBT | 2.29 | 0.59 | 2.45 | 0.84 | 2.61 | 0.84 | 1.22 | 2,74 | 0.30 |
| MET | 3.31 | 0.76 | 3.33 | 0.57 | 3.33 | 0.67 | 0.01 | 2,74 | 0.99 |
| CM | 1.32 | 0.40 | 1.25 | 0.34 | 1.35 | 0.55 | 0.34 | 2,74 | 0.72 |
| FC | 3.57 | 0.78 | 3.22 | 0.74 | 3.36 | 0.67 | 1.42 | 2,74 | 0.25 |
| STR | 3.00 | 0.53 | 2.73 | 0.35 | 3.10 | 0.74 | 2.73 | 2,74 | 0.07 |
| 9-session treatment, adherence dimension | |||||||||
| CBT | 2.19 | 0.51 | 2.38 | 0.56 | 2.51 | 0.59 | 2.34 | 2,83 | 0.10 |
| MET | 2.50 | 0.78 | 2.87 | 0.70 | 2.90 | 0.53 | 3.05 | 2,83 | 0.05 |
| CM | 1.53 | 0.47 | 1.56 | 0.46 | 1.56 | 0.39 | 0.04 | 2,83 | 0.96 |
| FC | 3.42 | 0.45 | 3.19 | 0.46 | 3.51 | 0.56 | 3.11 | 2,83 | 0.05 |
| STR | 3.07 | 0.50 | 3.08 | 0.36 | 3.26 | 0.31 | 1.75 | 2,83 | 0.18 |
| 2-session treatment, competence dimension | |||||||||
| CBT | 2.20 | 0.78 | 2.33 | 1.12 | 2.70 | 0.90 | 2.11 | 2,74 | 0.13 |
| MET | 3.67 | 0.82 | 3.58 | 0.70 | 3.57 | 0.85 | 0.12 | 2,74 | 0.88 |
| CM | 1.38 | 0.77 | 1.22 | 0.47 | 1.33 | 0.48 | 0.25 | 2,40 | 0.78 |
| FC | 3.61 | 0.92 | 3.28 | 0.69 | 3.49 | 0.65 | 1.12 | 2,74 | 0.33 |
| STR | 2.83 | 0.59 | 2.60 | 0.56 | 2.96 | 0.85 | 1.78 | 2,74 | 0.18 |
| 9-session treatment, competence dimension | |||||||||
| CBT | 2.07 | 0.55 | 2.12 | 0.66 | 2.48 | 0.64 | 3.29 | 2,83 | 0.04 |
| MET | 2.91 | 0.80 | 3.15 | 0.73 | 3.32 | 0.67 | 2.12 | 2,82 | 0.13 |
| CM | 1.44 | 0.56 | 1.28 | 0.42 | 1.49 | 0.49 | 1.31 | 2,79 | 0.28 |
| FC | 3.57 | 0.58 | 3.34 | 0.52 | 3.72 | 0.68 | 2.70 | 2,83 | 0.07 |
| STR | 3.18 | 0.52 | 3.07 | 0.44 | 3.45 | 0.43 | 4.29 | 2,83 | 0.02 |
CBT: cognitive–behavioral therapy scale; MET: motivational enhancement therapy scale; CM: case management scale; FC: facilitative conditions scale; STR: structure scale.
scores differed by site. Regarding competence ratings, there were no significant site differences in the two-session treatment. For the nine-session treatment, CBT and STR scores were significantly higher in site 3 versus site 2. Overall, however, the comparatively few site effects seen, given the number of comparisons (three sites × two dimensions × five scales), suggests that the training and monitoring protocol in this trial was associated with consistent delivery of the protocol treatments. Similarly, ANOVA models were used to evaluate whether there were significant differences across the 11 clinicians in adherence and competence ratings, or outcome (percentage of days using marijuana). Overall, even using liberal P-values (<0.20) as suggested by Crits-Christoph & Mintz [45] to evaluate therapist effects, few differences were found.
Process–outcome relationships
Table 3 provides simple correlations between adherence and competence ratings and the main outcome measure, percentage of days of marijuana use. For the two-session treatment, only the FC scale was associated significantly with outcome, where higher mean FC adherence and competence scores were associated with fewer days of marijuana use. In the nine-session treatment, higher mean MET adherence and competence scores were correlated significantly with more days of marijuana use. Similarly, higher mean CM scores were correlated significantly with more days of marijuana use.
Table 3.
Relationship between mean adherence and competence scores and outcome (percentage days of marijuana use), simple correlations.
| Scale | r |
|---|---|
| 2-session treatment (n = 77) | |
| Adherence scores | |
| Mean CBT | −0.082 |
| Mean MET | 0.069 |
| Mean CM | −0.075 |
| Mean STR | −0.145 |
| Mean FC | −0.283* |
| Competence scores | |
| Mean CBT | −0.12 |
| Mean MET | −0.04 |
| Mean CM | −0.186 |
| Mean STR | −0.0073 |
| Mean FC | −0.256 |
| 9-session treatment (n = 86) | |
| Adherence scores | |
| Mean CBT | −0.182 |
| Mean MET | 0.415** |
| Mean CM | 0.322** |
| Mean STR | 0.198 |
| Mean FC | 0.006 |
| Competence scores | |
| Mean CBT | −0.112 |
| Mean MET | 0.273** |
| Mean CM | 0.133 |
| Mean STR | 0.089 |
| Mean FC | 0.04 |
CBT: cognitive–behavioral therapy scale; MET: motivational enhancement therapy scale; CM: case management scale; FC: facilitative conditions scale; STR: structure scale.
P < 0.05;
P < 0.01.
Relationships between adherence, competence and outcome
In order to explore further the relationships between adherence and competence and outcome, general linear regression models were used to predict drug treatment outcome (percentage of days in treatment that marijuana was used) from YACS adherence and competence ratings. Baseline marijuana was included as a covariate all these analyses. For these analyses, only MET adherence and competence were considered, because MET was the primary active intervention in both the brief and extended treatments.
Does adherence predict outcome in a linear or curvilinear fashion?
In both the two-session and nine-session treatments, linear adherence (e.g. mean MET adherence score) did not predict outcome (two-session: t = 0.40, P = 0.69, nine-session: t = 1.44, P = 0.15). Similarly, adherence was not a curvilinear predictor of outcome in either treatment (two-session: t = 0.21, P = 0.83, nine-session: t = 1.73, P = 0.09).
Does competent delivery of treatment predict outcome?
Competence in delivering MET did not predict treatment outcome in either treatment (two-session: t = 1.12, P = 0.27, nine-session: t = 1.19, P = 0.24).
Do adherence and competence together predict outcome?
We investigated whether competence had an additive effect with adherence in predicting outcome. In a model predicting outcome from both adherence and competence, the inclusion of both terms again failed to predict outcome (two-session: adherence: t = −0.71, P = 0.48, competence: t = 1.26, P = 0.21; nine-session: adherence: t = 1.83, P = 0.07, competence: t = −1.06, P = 0.29).
Does the interaction of adherence and competence predict outcome?
In both treatments, the interaction between adherence and competence was not a significant predictor of treatment outcome (two-session: t = −0.46, P = 0.65, nine-session: t = 0.69, P = 0.49).
Working alliance ratings
Overall, participant rated WAI-C scores were high across the bond, task and goal subscales (mean scores for the nine-session treatment were, respectively, 6.0, 6.1 and 6.1 on the seven-point Likert scale). There were no significance differences between the two-session and nine-session treatments from the participant perspective (bond F = 0.85, task F = 0.05, goal F = 0.09). However, WAI-T scores indicated that from the clinicians’ perspective, bonds (F = 4.6, P = 0.04), tasks (F = 6.1, P = 0.02) and goals (F = 4.5, P = 0.04) were all rated more positively after the second session in the nine-session versus the two-session treatment. In both treatments, ratings from the clinicians’ perspective (WAI-T scores) were somewhat lower than the participant ratings (WAI-C scores) and, as in previous evaluations [37,38], correlations of participant and therapist from the same sessions were only moderate (0.28 for the two-session treatment and 0.34 for the nine-session treatment).
The relationship of the working alliance and outcome was examined using general linear models. In the two-session treatment, participant-rated alliance predicted outcome (t = −2.97, P < 0.001) significantly, with better alliance predicting fewer days of marijuana use. Therapist-rated alliance was also related significantly to outcome (t = −3.68, P < 0.001). In the nine-session treatment, however, patient-rated alliance did not predict days of marijuana use (t = −0.81, P = 0.41), but therapist-rated alliance predicted significantly fewer days of marijuana use (t = −2.25, P = 0.03).
Finally, we examined the interaction between adherence and alliance. In both treatments, the interaction of linear adherence and alliance failed to predict treatment outcome (two-session: t = 1.74, P = 0.09, nine-session: t = −0.21, P = 0.84). We also examined the interaction of curvilinear adherence and alliance in predicting outcome, as hypothesized above. In the two-session treatment this interaction did not predict treatment outcome significantly (t = 1.68, P = 0.10). However, in the nine-session treatment this interaction predicted outcome significantly (t = 2.77, P = 0.01).
DISCUSSION
Several aspects of treatment process were evaluated in a large multi-site trial of brief (two-session MET/CBT) and extended (nine-session MET/CBT/CM) behavioral treatments for marijuana dependence. In general, the multi-component treatments appeared to be implemented with good fidelity to manual specifications. Mean scale scores for the MET and CBT scales, as well as the general, non-specific scores (structure and facilitative conditions), were comparable to those in previous studies which used more highly trained and closely supervised clinicians [28,34]. There were very few significant differences in adherence, competence and working alliance ratings across the three treatment sites and little evidence of meaningful variability due to therapist effects.
As one of the first multi-site clinical trials for marijuana dependence using an effectiveness model, MTP is notable in several respects. In particular, it was implemented in three community-based treatment settings, recruited a more diverse sample of participants than seen in previous studies of marijuana users, and the treatments were implemented by predominantly master’s-level counselors drawn from community-based programs. The data suggest that the treatments were delivered largely as defined in the manual, site effects were minimal and treatments were well accepted by participants. These findings suggest that studies that emphasize external validity need not necessarily do so at the expense of internal validity. One limitation of the current study was that complete adherence and competence ratings were completed for only half the study sample. However, this sample was relatively large, was selected randomly and included all participating clinicians, and a comparable proportion of participants from the three sites. MTP is also notable in its implementation of an integrated multi-component treatment. When we examined the relationship between treatment fidelity and treatment outcome, the data suggested that adherence, competence and their combination were not associated strongly with marijuana use outcomes. This may reflect, in part, the limited range of variability in adherence and competence scores (that is, fairly high adherence and competence were found across the board) that may result in limited impact on treatment outcome [46] in controlled trials.
One treatment dimension that has been associated consistently with better outcomes is the working alliance [47,48]. In this study, both participants’ and therapists’ working alliance scores were associated significantly with marijuana use outcomes in the two-session intervention. In the nine-session treatment participant-rated alliance did not predict outcome, but higher therapist-rated alliance was associated significantly with fewer days of marijuana use. However, in the nine-session treatment, there was a significant interaction effect between alliance and curvilinear adherence. When alliance was high adherence had less impact on outcome, but when alliance was weaker, therapist adherence to treatment was substantially more influential. This replicates that seen in psychosocial treatment for cocaine [49].
One possibility for the differential findings in the two forms of treatment is that, in the two-session treatment, clinicians had little time to work with participants and implement interventions, so the quality of the relationship played a comparatively large role in outcome. However, in the nine-session treatment the working alliance was only part of a larger array of interventions and processes. In effect, these data suggest that alliance was, to some extent, a ‘necessary but not entirely sufficient’ treatment component in this trial. That is, the MTP data suggest that there may be a certain minimal level of alliance, below which specific interventions may be of limited use in fostering positive change. Given a sufficient level of alliance, however, use of specific, empirically grounded interventions may be able to exert their effects. At the other end of the continuum, at very high levels of alliance, the effect of those interventions may be more difficult to determine.
Acknowledgments
Support for this project was provided by a series of awards from the Center for Substance Abuse Treatment (award numbers UR4 TI11273, UR4 TI11310, UR4 TI11274, and UR4 TI11270). The MTP Research Group also includes Ken Christiansen PsyD, Mark Litt PhD, Bonnie McRee MPH, Nadia Solowij PhD, Robert Stephens PhD and Janice Vendetti MPH. We gratefully acknowledge the contributions of the study therapists and staff at Evergreen Treatment Services, Seattle, Washington; the University of Connecticut Health Center, Farmington, Connecticut; and the Village South, Miami, Florida, as well as Tami Frankforter and the raters who participated in this project. Support for this project was provided by a series of awards from the Center for Substance Abuse Treatment (award numbers UR4 TI11273, UR4 TI11310, UR4 TI11274 and UR4 TI11270).
Footnotes
Declarations of interest
None.
References
- 1.Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances and inhalants. Basic findings from the National Comorbidity Study. Exp Clin Psychopharmacol. 1994;2:244–68. [Google Scholar]
- 2.Kessler RC, Crum RM, Warner LA, Nelson CB, Schulendberg J, Anthony JC. Lifetime co-occurence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Study. Arch Gen Psychiatry. 1997;54:313–21. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- 3.Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291:2114–21. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- 4.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:566–76. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 5.Substance Abuse and Mental Health Administration. Results from the 2007 National Study on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Administration; 2008. [Google Scholar]
- 6.Copeland J, Swift W, Roffman RA, Stephens RS. A randomized controlled trial of brief cognitive-behavioral interventions for cannibis use disorder. J Subst Abuse Treat. 2001;21:55–64. doi: 10.1016/s0740-5472(01)00179-9. [DOI] [PubMed] [Google Scholar]
- 7.Stephens RS, Roffman RA, Simpson EE. Treating adult marijuana dependence: a test of the relapse prevention model. J Consult Clin Psychol. 1994;62:92–9. doi: 10.1037//0022-006x.62.1.92. [DOI] [PubMed] [Google Scholar]
- 8.Budney AJ, Higgins ST, Radonovich KJ, Novy PL. Adding voucher-based incentives to coping skills and motivational enhancement improves outcomes during treatment for marijuana dependence. J Consult Clin Psychol. 2000;68:1051–61. doi: 10.1037//0022-006x.68.6.1051. [DOI] [PubMed] [Google Scholar]
- 9.Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68:898–908. [PubMed] [Google Scholar]
- 10.Budney AJ, Moore BA, Rocha HL, Higgins ST. Clinical trial of abstinence-based vouchers and cognitive-behavioral therapy for cannabis dependence. J Consult Clin Psychol. 2006;74:307–16. doi: 10.1037/0022-006X.4.2.307. [DOI] [PubMed] [Google Scholar]
- 11.Carroll KM, Easton CJ, Nich C, Hunkele KA, Neavins TM, Sinha R, et al. The use of contingency management and motivational/skills-building therapy to treat young adults with marijuana dependence. J Consult Clin Psychol. 2006;74:955–66. doi: 10.1037/0022-006X.74.5.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kadden RM, Litt MD, Kabela-Cormier E, Petry NM. Abstinence rates following behavioral treatments for marijuana dependence. Addict Behav. 2007;32:1220–36. doi: 10.1016/j.addbeh.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MTP Research Group. Brief treatments for cannabis dependence: findings from a randomized multisite trial. J Consult Clin Psychol. 2004;72:455–66. doi: 10.1037/0022-006X.72.3.455. [DOI] [PubMed] [Google Scholar]
- 14.Carroll KM, Rounsaville BJ. Bridging the gap between research and practice in substance abuse treatment: a hybrid model linking efficacy and effectiveness research. Psychiatr Serv. 2003;54:333–9. doi: 10.1176/appi.ps.54.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barber JP, Crits-Christoph P, Luborsky L. Effects of therapist adherence and competence on patient outcome in brief dynamic therapy. J Consult Clin Psychol. 1996;64:619–22. doi: 10.1037//0022-006x.64.3.619. [DOI] [PubMed] [Google Scholar]
- 16.Henry WP, Strupp HH, Butler SF, Schacht TE, Binder JL. Effects of training in time-limited dynamic psychotherapy: changes in therapist behavior. J Consult Clin Psychol. 1993;61:434–40. doi: 10.1037//0022-006x.61.3.434. [DOI] [PubMed] [Google Scholar]
- 17.Barber JP, Gallop P, Crits-Christoph P, Frank A, Thase ME, Weiss RD. The role of therapist adherence, therapist competence, and alliance in predicting outcome of individual drug counselling: results from the national institute drug abuse collaborative cocaine treatment study. Psychother Res. 2006;16:229–40. [Google Scholar]
- 18.Stephens RS, Babor TF, Kadden R, Miller M MTP Research Group. The Marijuana Treatment Project: rationale, design, and participant characteristics. Addiction. 2002;97:109–24. doi: 10.1046/j.1360-0443.97.s01.6.x. [DOI] [PubMed] [Google Scholar]
- 19.Steinberg K, Roffman RA, Carroll KM, McRee B, Babor TF, Miller M, et al. Brief Counseling for Marijuana Dependence: A Manual for Treating Adults. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2005. [Google Scholar]
- 20.Steinberg KL, Roffman RA, Kadden R, Carroll KM, Kabela E, Miller M, et al. Tailoring cannabis dependence treatment for a diverse population. Addiction. 2002;97:135–42. doi: 10.1046/j.1360-0443.97.s01.5.x. [DOI] [PubMed] [Google Scholar]
- 21.Carroll KM, Kadden R, Donovan D, Zweben A, Rounsaville BJ. Implementing treatment and protecting the validity of the independent variable in treatment matching studies. J Stud Alcohol. 1994;(Suppl 12):149–55. doi: 10.15288/jsas.1994.s12.149. [DOI] [PubMed] [Google Scholar]
- 22.Crits-Christoph P, Siqueland L, Chittams J, Barber JP, Beck AT, Frank A, et al. Training in cognitive, supportive-expressive, and drug counseling therapies for cocaine dependence. J Consult Clin Psychol. 1998;66:484–92. doi: 10.1037//0022-006x.66.3.484. [DOI] [PubMed] [Google Scholar]
- 23.Ball SA, Bachrach K, DeCarlo J, Farentinos C, Keen M, McSherry T, et al. Characteristics of community clinicians trained to provide manual-guided therapy for substance abusers. J Subst Abuse Treat. 2002;23:309–18. doi: 10.1016/s0740-5472(02)00281-7. [DOI] [PubMed] [Google Scholar]
- 24.McCarty D, Fuller BE, Arfken C, Miller M, Nunes EV, Edmundson E, et al. Direct care workers in the National Drug Abuse Treatment Clinical Trials Network: characteristics, opinions, and beliefs. Psychiatr Serv. 2007;58:181–90. doi: 10.1176/appi.ps.58.2.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV, Patient Edition. Washington, DC: American Psychiatric Press; 1995. [Google Scholar]
- 26.McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 27.Sobell LC, Sobell MB. A technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, editors. Measuring Alcohol Consumption. NJ: The Humana Press; 1992. pp. 41–72. [Google Scholar]
- 28.Carroll KM, Nich C, Sifry R, Frankforter T, Nuro KF, Ball SA, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57:225–38. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- 29.Carroll KM, Nich C, Ball SA, McCance-Katz E, Rounsaville BJ. Treatment of cocaine and alcohol dependence with psychotherapy and disulfiram. Addiction. 1998;93:713–28. doi: 10.1046/j.1360-0443.1998.9357137.x. [DOI] [PubMed] [Google Scholar]
- 30.Perepletchikova F, Kazdin AE. Treatment integrity and therapeutic change: issues and research recommendations. Clin Psychol Sci Pract. 2005;12:365–83. [Google Scholar]
- 31.Kahler CW, Metrik J, LaChance HR, Ramsey SE, Abrams DB, Monti PM, et al. Addressing heavy drinking in smoking cessation treatment: a randomized clinical trial. J Consult Clin Psychol. 2008;76:852–62. doi: 10.1037/a0012717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morgenstern J, Irwin TW, Wainberg ML, Parsons JT, Muench F, Bux DA, Jr, et al. A randomized controlled trial of goal choice interventions for alcohol use disorders among men who have sex with men. J Consult Clin Psychol. 2007;75:72–84. doi: 10.1037/0022-006X.75.1.72. [DOI] [PubMed] [Google Scholar]
- 33.Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, Shi J, et al. Efficacy of disulfiram and cognitive-behavioral therapy in cocaine-dependent outpatients: a randomized placebo controlled trial. Arch Gen Psychiatry. 2004;64:264–72. doi: 10.1001/archpsyc.61.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carroll KM, Connors GJ, Cooney NL, DiClemente CC, Donovan DM, Longabaugh RL, et al. Internal validity of Project MATCH treatments: discriminability and integrity. J Consult Clin Psychol. 1998;66:290–303. doi: 10.1037//0022-006x.66.2.290. [DOI] [PubMed] [Google Scholar]
- 35.Martino S, Ball SA, Nich C, Frankforter TL, Carroll KM. Community program therapist adherence and competence in motivational enhancement therapy. Drug Alcohol Depend. 2008;97:37–48. doi: 10.1016/j.drugalcdep.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Horvath AO, Greenberg LS. The development of the Working Alliance Inventory. In: Greenberg LS, Pinsof WM, editors. The Psychotherapeutic Process: A Research Handbook. New York, NY: Guilford Press; 1986. pp. 529–56. [Google Scholar]
- 37.Cecero JJ, Fenton LR, Nich C, Frankforter T, Carroll KM. Focus on the therapeutic alliance: the psychometric properties of six measures across three treatments. Psychotherapy. 2001;38:1–11. [Google Scholar]
- 38.Tichenor V, Hill CE. A comparison of six measures of the working alliance. Psychotherapy. 1989;26:195–9. [Google Scholar]
- 39.Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychol Assess. 1989;1:207–10. [Google Scholar]
- 40.Bonett DG. Sample size requirements for estimating intra-class correlations with desired precision. Stat Med. 2002;21:1331–5. doi: 10.1002/sim.1108. [DOI] [PubMed] [Google Scholar]
- 41.Gibbons RD, Hedeker D, Elkin I, Waternaux C, Kraemer HC, Greenhouse JB, et al. Some conceptual and statistical issues in analyses of longitudinal psychiatric data. Arch Gen Psychiatry. 1993;50:739–50. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- 42.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–9. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 43.Hu L, Bentler PM. Cutoff fit criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equat Model. 1999;6:1–55. [Google Scholar]
- 44.Carroll KM, Nich C, Rounsaville BJ. Contribution of the therapeutic alliance to outcome in active versus control psychotherapies. J Consult Clin Psychol. 1997;65:510–14. doi: 10.1037//0022-006x.65.3.510. [DOI] [PubMed] [Google Scholar]
- 45.Crits-Christoph P, Mintz J. Implications of therapist effects for the design and analysis of comparative studies of psychotherapies. J Consult Clin Psychol. 1991;59:20–6. doi: 10.1037//0022-006x.59.1.20. [DOI] [PubMed] [Google Scholar]
- 46.Carroll KM. Constrained, confounded, and confused: why we know so little about therapist effects. Addiction. 2001;96:203–6. doi: 10.1046/j.1360-0443.2001.9622032.x. [DOI] [PubMed] [Google Scholar]
- 47.Horvath AO, Luborsky L. The role of the therapeutic alliance in psychotherapy. J Consult Clin Psychol. 1993;61:561–73. doi: 10.1037//0022-006x.61.4.561. [DOI] [PubMed] [Google Scholar]
- 48.Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: a meta-analysis. J Couns Psychol. 1991;38:139–49. [Google Scholar]
- 49.Barber JP, Foltz C, Crits-Christoph P, Chittams J. Therapists’ adherence and competence and treatment discrimination in the NIDA Collaborative Cocaine Treatment Study. J Clin Psychol. 2004;60:29–41. doi: 10.1002/jclp.10186. [DOI] [PubMed] [Google Scholar]