The negative effects of life stress can arise from exposure to multiple forms of adversity including childhood sexual and physical abuse, premature deaths of family members, and exposure to chronic stressors such as violent neighborhoods and unsafe workplaces (Pearlin & Skaff, 1996; Seery, Holman, & Silver, 2010). Life stresses have been consistently linked to depression, substance abuse, poor health, and premature mortality, including suicide (Felitti et al., 1998; Gould et al., 1994; Horwitz, Widom, McLaughlin, & White, 2001; Thornicroft, 2011). Amidst the overwhelming evidence of pathology, recent studies have found resilience and posttraumatic growth resulting from some forms of adversity (Seery et al., 2010).
Research on adversity has often adopted a life course perspective, portraying stressful events as chains of risk in which one exposure tends to lead to another in probabilistic rather than deterministic fashion (Ben-Shlomo & Kuh, 2002, p. 287). A cumulative or snowball effect is produced when a cascade of adverse events becomes synergized into a “whole bigger than the sum of its parts” with prolonged and deep effects on the individual (Pearlin & Skaff, 1996; Thoits, 2010) including allostatic load burdens affecting biological and immune systems (Ben-Shlomo & Kuh, 2002).
As noted by its leading proponents, life course inquiry poses serious methodological and ethical challenges associated with longitudinal designs starting in early childhood, or, as an alternative, retrospective designs dependent upon the vagaries of memory (Ben-Schlomo & Kuh, 2002). As well, operationalizing and measuring adverse life events raise concerns about subjective differences in appraising their presence and severity and the ecological validity of standardized measures used with individuals from varying cultural and socioeconomic backgrounds.
The burgeoning body of literature on life stress underscores several points of significance for this study. First is the “long reach of childhood experiences” (Thoits, 2010, p. S47), i.e., childhood maltreatment has lasting negative consequences (Edwards, Holden, Felitti, & Anda, 2003; Felitti et al., 1998). Second, stressful events have nonspecific effects that can lead to physical and mental health problems (Thoits, 2010; Wickrama, Conger, & Abraham, 2005). Finally, harmful effects of stress stem from structural disadvantage (poverty, lack of housing and jobs, inadequate health care) as well as proximal experiences (child abuse, serious illness, violent victimization). Yet virtually all empirical research is confined to assessing the latter, in part because of the greater facility in measuring individual characteristics and experiences (Thoits, 2010). Not surprisingly, interventions target microlevel factors (family, intimate partners, peers) with some attention to those at the mesolevel (neighborhood, workplace; Aneshensel, 2009).
In this article, we use in-depth interviews and case study analyses to examine adverse life events reported by study participants who have a serious mental illness and history of homelessness and co-occurring substance use. We address the following research questions:
What are the types and frequencies of adverse life events reported?
How do participants describe and appraise these events?
We present this qualitative report as filling a significant gap in a rapidly expanding literature on adversity that is dominated by quantitative methods and findings.
Adversity Among Persons With Serious Mental Illness and Histories of Homelessness and Substance Use
It has become axiomatic that to have a serious mental illness (SMI) such as schizophrenia is to be troubled, isolated, and victimized (Parese & Wolf, 2005; Sells, Rowe, Fisk, & Davidson, 2003). For the subset of such persons who have the misfortune of becoming homeless, the co-occurrence of drug and alcohol abuse, health problems, injuries, and victimization is all too common (Druss & Bornemann, 2010; Metraux & Culhane, 1999; Padgett & Struening, 1992). The 25-year reduction in life expectancy of persons with serious mental illness is undoubtedly increased for those who become homeless, the latter group 3–4 times more likely to die prematurely than nonhomeless individuals (O’Connell, 2005).
Less common have been retrospective examinations of homeless individuals’ lives before they encountered the troubles of adulthood. Herman and colleagues examined adversity in the lives of 92 formerly homeless persons self-identified in a general U.S. population survey and found much higher rates of child abuse in the sample (Herman, Susser, Struening, & Link, 1997). Stein, Leslie, and Nyamathi (2002) surveyed 581 homeless women and found strong effects of parental substance use and child maltreatment on adult depression and substance abuse. Kim, Ford, Howard, and Bradford’s study of 239 homeless men found associations between childhood trauma and mental illness (although no associations were found for trauma and substance abuse; 2010). A qualitative study found gender-related traumas disproportionately affected formerly homeless women with serious mental illness (Padgett, Hawkins, Abrams, & Davis, 2006).
Homeless persons with serious mental illness are more likely to come from lower income backgrounds (Locke, Khadduri, & O’Hara, 2007). Thus, social causation is at work earlier in life, depriving them of human and social capital, i.e., resources necessary to fend off extreme poverty after the onset of mental illness (Hawkins & Abrams, 2007). Suffering associated with SMI—hearing voices, feeling lost in one’s head, and difficulty attending to daily needs—is compounded when living on the streets. Yet it may be overshadowed by basic needs for survival and safety (Draine, Salzer, Culhane, & Hadley, 2002).
Few studies of this population have documented the subjective contexts and meaning of long-term exposure to adversity. Instead, research has focused on the problems of adulthood that have led homeless persons into the service system, especially mental illness and co-occurring substance abuse. The significance of this inquiry is enhanced by the recent emphasis on mental health recovery (Deegan, 2007; Leamy, Bird, LeBoutillier, Williams, & Slade, 2011). Thus, individuals with SMI embark upon journeys of recovery with a unique set of capabilities and limitations that service providers must take into account (Ridgway, 2001). To narrow the focus to current measurable problems risks overlooking adverse events from earlier years as well as individuals’ subjective meanings that are not easily captured through standardized measures.
Method
Qualitative interviews conducted for this analysis were part of Phase I of a parent study funded by the National Institute of Mental Health. The parent study’s design—purposively selecting individuals who fit minimal criteria of having achieved a degree of mental health recovery—ensured that we would recruit a somewhat higher-functioning cohort to learn from their experiences.
Forty interviews were conducted and transcribed verbatim between September 2010 and May 2011. Interviewees were recruited from two New York City area programs serving formerly homeless persons with SMI, virtually all of whom also had substance abuse in the past or were using currently. Inclusion criteria included: over age 18, English-language fluency, DSM-IV diagnosis of serious mental illness, and history of homelessness and substance use.
Senior staff members from the two program sites were asked to nominate 20 individuals who met the inclusion criteria; 10 with less than 5 years of program tenure and 10 with 5 or more years of tenure. We stratified the sample in this way to ensure inclusion of clients with shorter and longer-term familiarity with their program.
To minimize bias, two staff members from each agency were asked to independently nominate eligible individuals; only those who were jointly nominated were asked to participate. Of the 40 individuals nominated, 31 agreed to participate in the study. To achieve the desired sample size of 40, a second round of joint nominations was conducted. The primary reason for refusal was the lack of availability or interest in study participation. Study participants were paid a $30 incentive per interview plus a roundtrip subway Metrocard valued at $4.50. All study protocols were approved by the authors’ affiliated human subjects committee.
The interview guide included casting-a-wide-net questions and focused probes for mental health and psychiatric treatment experiences, substance use and recovery, and homeless episodes. The overall goal of the interviews was to understand from the participants’ perspectives how they were currently doing, and, most importantly, how that status was achieved and what life experiences preceded it, both positive and negative. Although interviewers did not directly inquire about adverse and traumatic events, they were trained to sensitively probe if and when such events were mentioned.
Case study analyses were developed using the following sources of data: verbatim transcripts, interviewer feedback forms (IFFs), which described the study participant (SP)’s nonverbal and other behaviors during the interview, and case summaries compiled by the project director. These sources of data were inventoried using a checklist derived from the work of Lloyd and Turner (2008). In keeping with their definition, we defined adversity as “the occurrence of normatively undesirable life events....that may have the potential for long term consequences (2008, p. 2).
The Adverse Life Events Checklist (ALEC) included Lloyd and Turner’s original 41 items with some modifications. First, 10 items were added to represent life experiences of this population and their adult status (the original checklist was developed for adolescents). The additional items (shown in Table 1 marked with ‘+’) represented adult experiences, e.g., loss of partner due to divorce or separation and events specific to this population, e.g., psychiatric symptoms, sex work, homelessness, psychiatric hospitalization, and incarceration. Second, some items were slightly modified in wording (marked with an asterisk in Table 1).
Table 1.
Demographic Characteristics
| N = 38 | |
|---|---|
| Sex | |
| Male | 30 |
| Female | 8 |
| Race/Ethnicity | |
| African-American | 22 |
| American-Indian/Native-American | 2 |
| Asian-American | 1 |
| Caucasian | 4 |
| Hispanic-American | 6 |
| Mixed Race | 3 |
| Education | |
| Grade School | 5 |
| High School | 16 |
| College | 14 |
| Post-Graduate | 3 |
| Marital Status | |
| Married | 0 |
| Divorced | 8 |
| Separated | 4 |
| Never Married | 24 |
| Widowed | 2 |
| Relationship Status | |
| Committed Relationship | 5 |
| Casual Dating | 3 |
| Single | 30 |
| Have Children | |
| Yes | 18 |
| No | 20 |
| Employment Status | |
| Unemployed | 25 |
| Part-Time Employment | 11 |
| Full-time Employment | 0 |
| Unavailable | 2 |
| Mean Age | 50 |
As originally developed, the checklist was treated as a simple unweighted count in calculating exposure (Turner & Lloyd, 2003). Test re-test evidence of reliability for lifetime adversity checklists was found to be satisfactory (Wheaton, Roszell, & Hall, 1997).
Two interviews were excluded because of the lack of specificity surrounding descriptions of adverse life events. For each of the remaining 38 participants, the lead interviewer (one of three graduate students, all of whom had experience working with this population) used the ALEC to inventory case study data and record the incidence and frequency of experiences. To enhance accuracy, a sample of 10 transcripts was randomly selected and independently inventoried by another team member. Differences were discussed until consensus was reached.
Results
Adverse Life Events: Frequencies and Types Among Demographic Subgroups
Table 2 shows the demographic characteristics of the sample. As shown, participants were 50 years of age on average, predominantly male, African-American, never married, single, unemployed, and had an educational level of high school or more. In calculating frequencies of events, we found seven items received no endorsement, and these were removed from calculations of frequencies and averages. These events were either less likely to occur (“lost home to natural disaster” or less likely to meet the participant’s threshold of reportage in a qualitative interview (“chased but not caught …”).
Table 2.
Adverse Life Events Checklist (Total N=38)1
| N | % | ||
|---|---|---|---|
| 1 | Failed a grade in school or dropped out* | 20 | 53 |
| 2 | Father or mother experienced unemployment* | 4 | 11 |
| 3 | Sent away from home or kicked out of the house for doing something wrong | 3 | 8 |
| 4 | Abandoned by one or both parents | 11 | 30 |
| 5 | Lived in an orphanage, a foster home, a group home, or were a ward of the state as a child | 6 | 16 |
| 6 | Lived apart from parents* | 12 | 32 |
| 7 | Parents divorced or separated | 13 | 34 |
| 8 | Lost custody of a child* | 8 | 21 |
| 9 | Discovered spouse/boyfriend/girlfriend/partner was unfaithful | 0 | 0 |
| 10 | Lost a spouse/boyfriend/girlfriend/partner through divorce or separation† | 16 | 42 |
| 11 | Lost home because of a natural disaster | 0 | 0 |
| 12 | Had a serious accident or injury due to a psychiatric illness or substance abuse that was life-threatening or caused long-term disability† | 4 | 11 |
| 13 | Had a serious accident or injury due to other reasons besides psychiatric problems or substance abuse* | 6 | 16 |
| 14 | Had sexual intercourse when not wanted because forced or threatened | 3 | 8 |
| 15 | Touched or made to touch someone else in a sexual way because forced or threatened | 2 | 5 |
| 16 | Regularly physically abused by parent(s), step-parent(s), grandparent(s) or guardian(s) | 6 | 16 |
| 17 | Regularly emotionally abused by caretaker(s) | 7 | 18 |
| 18 | Physically abused or injured by spouse/boyfriend/girlfriend/partner | 0 | 0 |
| 19 | Emotionally abused or injured by spouse/boyfriend/girlfriend/partner† | 0 | 0 |
| 20 | Physically abused or injured by someone else known | 2 | 5 |
| 21 | Shot at with a gun or threatened with another weapon but not injured | 1 | 3 |
| 22 | Shot with a gun or badly injured with another weapon | 3 | 8 |
| 23 | Chased but not caught where there was potential for real injury if caught | 0 | 0 |
| 24 | Physically assaulted or mugged | 5 | 13 |
| 25 | In a car crash in which someone was killed or badly injured | 1 | 3 |
| 26 | Made a suicide attempt or had suicidal ideations† | 12 | 32 |
| 27 | Experienced psychotic symptoms† | 27 | 71 |
| 28 | Hospitalized for psychiatric reasons† | 32 | 84 |
| 29 | Lived on the streets or in shelters† | 30 | 79 |
| 30 | Did sex work or prostitution† | 2 | 5 |
| 31 | Incarcerated in jail or prison† | 14 | 37 |
| 32 | Witnessed a serious accident or disaster where someone was hurt very badly or killed | 3 | 8 |
| 33 | Witnessed a family member being regularly physically or emotionally abused* | 5 | 13 |
| 34 | Witnessed someone chased but not caught or threatened with serious harm | 0 | 0 |
| 35 | Witnessed someone get shot at or attacked with another weapon | 3 | 8 |
| 36 | Witnessed someone seriously injured by a gunshot or some other weapon | 1 | 3 |
| 37 | Witnessed someone get killed by being shot, stabbed, or beaten | 1 | 3 |
| 38 | Told that a family member/significant other/friend/acquaintance had been shot, but not killed | 0 | 0 |
| 39 | Told that a family member/significant other/friend/acquaintance had been killed with a gun or other weapon | 2 | 5 |
| 40 | Told that a family member/significant other/friend/acquaintance had died suddenly or been seriously hurt | 8 | 21 |
| 41 | Told that a family member/significant other/friend/acquaintance killed him- or herself | 2 | 5 |
| 42 | Told that a family member/significant other/friend/acquaintance had been raped | 1 | 3 |
| 43 | Told that a family member/significant other/friend/acquaintance developed a serious illness† | 7 | 18 |
| 44 | Experienced the death of mother/step-mother* | 13 | 34 |
| 45 | Experienced the death of father/step-father* | 8 | 21 |
| 46 | Experienced the death of a sibling* | 8 | 21 |
| 47 | Experienced the death of a spouse/boyfriend/girlfriend/partner* | 4 | 11 |
| 48 | Experienced the death of child* | 5 | 13 |
| 49 | Experienced the death of a grandparent* | 2 | 5 |
| 50 | Experienced the death of another loved one* | 6 | 16 |
| 51 | Experienced the death of a very close friend* | 5 | 13 |
Note.
Adapted from Lloyd.
Items have been modified.
Items have been added to be more population specific.
Returning to Table 1, the proportion of participants reporting having experienced the remaining 44 events was highest for psychiatric hospitalization and other experiences that were part of the parent study’s sampling criteria (serious mental illness and homelessness). About one-third had been incarcerated (37%), experienced suicidality (32%), been abandoned by one or both parents (30%), and experienced the death of a mother or stepmother (34%). Further losses included experiencing the death of a father or stepfather (21%), death of a sibling (21%), and death of a child (13%). Over one half of participants (53%) had failed a grade or dropped out of school.
Table 3 shows that women had more adverse events on average than men, and that older participants had experienced more adversity, the latter probably reflecting a longer period of exposure because of older age. None of the group differences in Table 3 were statistically significant. In the following section, we go beneath and beyond these numbers to document the contexts and meaning of adversity as recounted by the participants.
Table 3.
Group Comparisons
| N=38 | Frequency 336 |
Average 8.842 |
|---|---|---|
| Gender | ||
| Female (n= 8) | 87 | 10.88 |
| Male (n= 30) | 249 | 8.3 |
| Age | ||
| 20–29 (n= 3) | 20 | 6.67 |
| 30–39 (n= 3) | 23 | 7.67 |
| 40–49 (n= 10) | 67 | 6.70 |
| 50–59 (n= 16) | 149 | 8.28 |
| >60 (n= 6) | 77 | 12.83 |
| Race/Ethnicity | ||
| Non-African-American (n= 13) | 119 | 9.15 |
| African-American (n= 25) | 217 | 8.68 |
Adversity Over the Life Course: Cross-Case Findings
Cross-case analyses of adversity in the qualitative data revealed the following patterns or themes: social losses because of death and estrangement, the significance of chronic stressors as well as acute events, and the cumulative lifetime nature of adversity. We discuss each of these themes and offer quotes illustrative of how participants described adverse events. Finally, case vignettes are offered as illustrations of cumulative adversity.
Social losses: Premature deaths and estrangement
The losses due to family deaths shown in Table 1 are notable. In addition to poor health, participants cited suicide, homicide, and severe alcoholism as causes of premature death. For one participant, the accumulation of losses led him to the brink of suicide:
.... my brother was my best friend outside of my mother. My mother had already died and then my brother … had lung cancer and he died. That was devastating. Then my granddaughter died....all in the same month. So that was you know, too much for me … because I really prayed hard that God would take me and not my brother because my brother had so much to live for. I felt like I had nothing to live for, I really did.
For another participant, the loss of his mother was exacerbated by his father’s decisions about her medical care after a tragic accident:
I’m the youngest of five kids. My mother passed away when I was 5 years old. … And you know, my mother passed out and hit her head on the sidewalk and went into a coma. And my father .... did not agree to let them do no head surgery and all that. So she passed away. On that day my father came home, that was the first time I seen my father cry. I’ll never forget that day.
Another participant felt his mother’s death was the cause of much of his later problems:
And that’s where, I think, it began. After she passed, I started hearing her voice and seeing things. And I became extremely angry … then even started hating my family. And to be honest, that’s all that I truly remember for at least 20 years. And that was my life from the time I was 16 ‘til about 39.
Though not fully captured in Table 1, social losses included relationships eroded by estrangement, incarceration, and long-term hospitalization. Tense relationships with family and friends were rooted in shared histories of mental illness, inadequate or absent parenting, stealing to support a drug habit, and stigma-related rejection. Long institutional stays in prison or a psychiatric hospital produced diminishing contacts with family and friends who had problems of their own and could ill afford the time or emotional effort needed to maintain relationships. One male participant noted:
When I was 16 years old, I was incarcerated...I had a sex offense... I did 12 years out of the 18 years, ‘cause I was goin’ through so much turmoil. I was fightin’ in prison all the time. I was just wild back then. And using drugs. You know drugs you can get in prison, right?
Inadequate or nonexistent parenting led to strained or severed relationships with their children and caregivers (usually the mother), and, in many instances, loss of custody. As one female participant reported, loss of her children motivated her recovery:
And I basically was a crack addict ....between ’82 and ’90, that’s when I went into crack and coke and weed. So, that was an ongoing battle. What happened to curtail that is that my children were taken away from me and I was told if I stayed clean, took medications, go to a program, I would have a chance of getting back my children.
Beyond acute events: The toll of chronic stress
For participants, poverty and deprivation, poor health, and social exclusion took a toll less measurable or discrete.
It was rough. Because there was so many of us, you know. Either we didn’t have shoes, or we didn’t have clothes. And you had to be really doing bad, your feet would have to be on the ground before the family could afford buying you another pair of shoes.
Another related:
[my life] … it’s all a blur to me. Like most of it is incarceration. Like … we was poor when I was growing up. I remember when coming up as a kid my stepfather … used to always verbally abuse my mother and verbally abuse us. … there was seven of us kids and we all had different fathers, so that gave him more ammunition to throw at my mother.....He was around ‘til I was about 12 years then he moved out.
A young male participant recalled a similar degree of family turmoil:
Damn there was a lot of madness that made me want to get out of myself even before I was a teen....a lot of crazy stuff. Watching my father … beat my mother almost to death. There were times when we didn’t have anything to eat … there are a lot of things that I’d like to forget … Why at 9. 10, 11, and 12, I was doing all the crazy things … ‘cause I didn’t feel I was worthy. So I medicated a long time whether it was running, staying outside of the house, picking up an illegal substance, drinking alcohol, at 10, 11, witnessing abuse at home, and separation, and no lights. Livin’ in five different places in a year....‘cause my mom dragged us around ‘cause she couldn’t afford to pay.
Poor health and a variety of chronic conditions undermined daily life. As one woman declared:
I’m diagnosed with chronic severe depression …. That’s my psychiatric diagnosis. Then I have lupus.....I have chronic asthma, high blood pressure, menopause, oh my god I can name so many things..... before I was taking 30 something different medications everyday. Now I’m down to 9.....I have Graves disease also.
Study participants who had been taking antipsychotic medication had to contend with weight gain and diabetes.
I got diagnosed with the sugar diabetes in the psychiatric hospital. The day I went in there, before I got sent upstairs, they stopped the medication ‘cause they knew. My sugar was 400 that day that they found out I was diabetic….. all these doctors and pharmacists and people that make this medicine, they know these side effects but they don’t tell you ‘til you come down with something.
Lack of income, in combination with few job skills, left many participants coping with shortages of basic amenities. While disability checks and income supports such as food stamps were barely sufficient to cover basic needs, little money was left over. One woman recalled her younger days attending a community college:
Because by the time I paid the rent, paid the phone bill, gas bill, and electricity, I had 10 dollars left. … So, I had to walk to school, I didn’t have car fare. The money that I got from the food stamps was just enough for a month. I didn’t eat. I would sit in the cafeteria but everyone else was eating, so the stress put me in the hospital three times …
Social exclusion and stigma also took their toll. One older male participant summed this up as a responsibility he had to shoulder:
I have brothers and sisters but I decided to be more independent … you know there’s a stigma. … They still look at me from a different perspective, they’re not educated about my illness nor do they want to be.
Cumulative adversity: Case vignettes
In this section, we present vignettes and schematic diagrams of individual life trajectories that illustrate the interrelating and cumulative effects of adversity. All names and potentially identifying information have been changed to protect their identities.
Case study #1
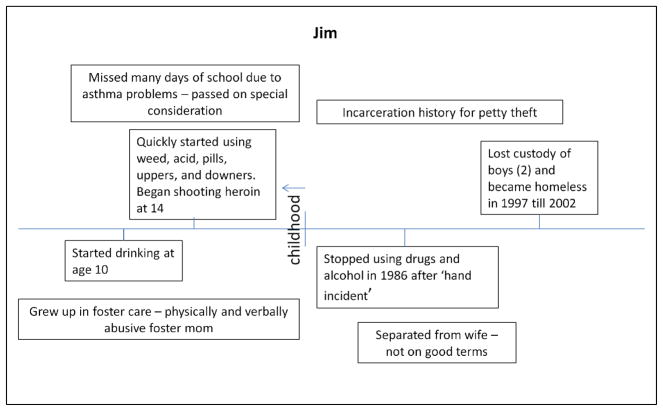
Jim is a 59 year old white male who is separated from his wife and has recently enjoyed renewed relationships with his adult sons. As shown in Figure 1, Jim was raised by an abusive foster mother, suffered from severe childhood asthma, and began abusing alcohol and drugs at an early age.
... it was hard for me growing up because I had all of this racing thinking all of the time. Like my mind pretty much tortured me. I mean it was constantly racing and drugs .... and it was just like, I was abused as a kid, um physically and mentally. I was adopted; this whole nightmare scenario, but in any case I never met my real parents. They probably did me a bigger favor than the woman who ended up adopting me who abused me.
Figure 1.
Case study of Jim.
As an adult, Jim had several jail sentences for petty theft and was homeless for 5 years in his late 40s. He attributes his ability to stop abusing drugs to an incident in his mid-30s when he was hospitalized and almost lost his hand because of a severe infection related to his drug use.
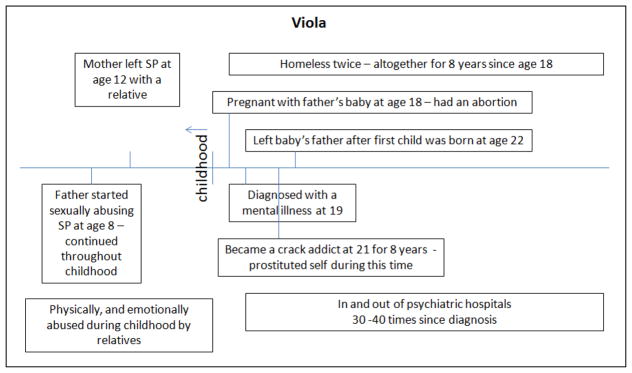
Case study #2
Viola is 51 years old, of Afro-Caribbean descent and has lived in the United States since age 18 (see Figure 2). While growing up abroad, she was abandoned by her mother and repeatedly sexually abused by her biological father. Upon arrival in the United States, Viola found out she was pregnant (by her father) while being hospitalized for the first time due to mental illness. After an abortion and psychiatric treatment, she was reunited with her mother who was living in New York City and also suffering from mental illness. Viola spent most of her 20s in the throes of crack addiction, in and out of psychiatric hospitals, and homeless. She married, divorced, and had three children during this time; all were removed into foster care. When asked what she thought had caused her mental illness, Viola made it clear:
Figure 2.
Case study of Viola.
… it’s the incest. What happened to me as a child, because I was physically abused, sexually abused, and emotionally abused. So, basically that was a culmination of it all. …..my mother left me in [home country] … 12 years old … with a relative. And if I didn’t work, I couldn’t go to school because I couldn’t afford the bus fare. I was treated like an unpaid maid. Cook, clean, you name it. And I think that attributed to when I finally came to America and saw my mother, I was so angry at her that she would abandon me. That came into it too.
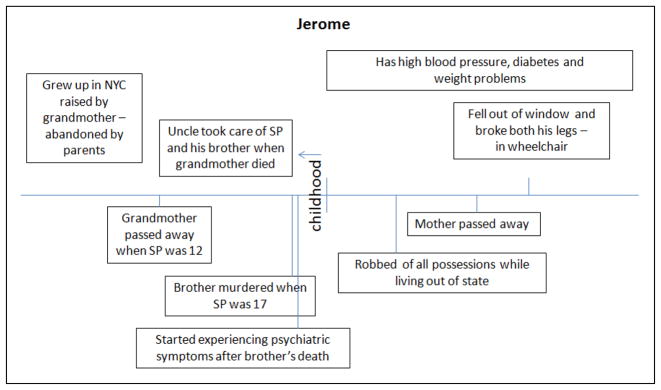
Case study #3
Jerome is a 39-year-old African American man recovering from two broken legs at the time of the interview. The injury, incurred by an accidental fall from his apartment window, left him in a wheelchair awaiting rehabilitation. As shown in Figure 3, Jerome and his brother were abandoned by their parents and raised by a grandmother in Harlem who died when Jerome was 12. Jerome suffers from diabetes, weight problems, and hypertension; he blames his bipolar disorder on the trauma of his brother’s murder while the boys were living with an uncle:
… I think it all started when my brother was murdered when I was 17. And it just used to be times when I’ll find myself outside just walking around at 3 or 4 in the morning and I wonder what am I doing out? And I couldn’t tell anybody what was going on …
Figure 3.
Case study of Jerome.
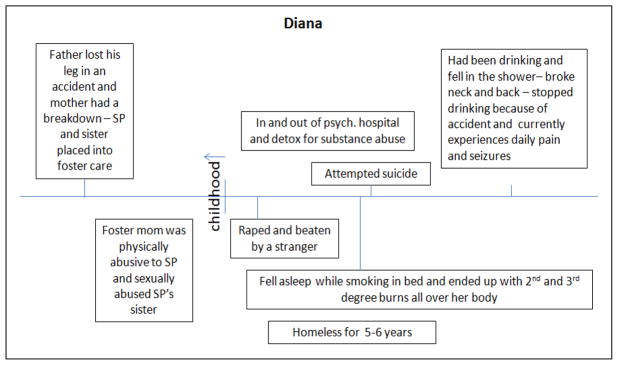
Case study #4
Diana is a 48-year-old Native American whose life story represents an intense accumulation of adverse traumatic events. As a child, she and her sister spent 8 years in foster care after their mother was hospitalized for mental illness and their father lost a leg in a traffic accident. The foster mother proved to be both physically and sexually abusive.
You see the foster mother did that to me [shows scar on wrist] ....She sharpened the spoon and cut my wrist. She threw me down a flight of stairs, broke my arm. ….it was very hard to deal with that because the lady [sexually molested SP’s sister]. They said she would never have kids but she had two, so thank God.
A heavy drinker, Diana gave up alcohol after falling and breaking her neck and back. Prior to that, she fell asleep while smoking and suffered third degree burns over much of her body. Those injuries led Diana to an unsuccessful attempt at suicide and an additional psychiatric hospitalization. At the time of the interview, she was taking multiple pain medications and suffering from diabetes. No longer drinking, Diana attributes her survival to spiritual faith.
I believe because he [God] saved my life..… I could say me, but it wasn’t me. No human could have done that. Even the doctors say God because they said “You should be dead or have some type of a problem and you don’t.” At one point in time I didn’t believe in anything, you know, just drink my life away and be happy, but when I had these accidents happen then I started believing because I think no one in their right mind should be alive through all of this.
The preceding vignettes were chosen to illustrate the chain of adverse events and their cumulative nature over time. Childhood abandonment and severe maltreatment gave way to adolescent abuse of drugs and alcohol, and these, in turn, gave way to problems in adulthood: debilitating injuries, weight gain and diabetes, heavy reliance on medications for physical and mental problems, and multiple social losses. In this context, serious mental illness was one among many forms of adversity and was cast by participants as more of a problem in the past than in the present.
Discussion
The findings of this study point to substantial exposure to adverse events in addition and related to serious mental illness, history of substance abuse, and homelessness. These events included incarceration, suicidality, childhood abuse, and multiple losses of family and friends. Moreover, chronic stressors (poor health, poverty, social isolation, and stigma) were frequently reported, many related to the adverse events shown in Table 1.
As noted earlier, findings of adverse experiences are not new or surprising given the study population of interest. However, the temporal depth, multiplicity and cumulative nature of exposure to adversity are noteworthy. We also point out the possibility that these constitute only a fraction of the number of such experiences, because they were not systematically elicited by interviewers.
It is perhaps unsurprising that many of the chronic problems had their origins in the acute events of participants’ lives. Homelessness, for example, brings poor health and chronic pain from violent injuries and accidents. Social isolation results from the premature deaths of social others and from troubled relationships rooted in the turmoil of mental illness and substance abuse. Poverty and mental illness have a corrosive effect, rendering participants dependent upon disability income and living a marginal existence. Social losses—premature deaths of family members as well as severed relationships with parents, siblings, children, and friends—point to seriously depleted social networks similar to those found in other studies (Hawkins & Abrams, 2007; Perese & Wolf, 2005).
The quantity and severity of adverse events reported by study participants make their survival remarkable in itself - several exclaimed that they were surprised to still be alive. Although beyond the scope of this report, gaining an understanding of how persons successfully overcome serious mental illness, substance abuse, and homelessness—as well as prior traumatic events—is a key goal of Phase II of the parent study now under way. We know from studies of trauma in other populations that positive outcomes are possible (Seery et al., 2010).
This study has limitations and strengths worth mentioning. First, our sample consisted of participants rated as showing modest progress toward mental health recovery. Thus, it is not representative of the population of formerly homeless adults with serious mental illness, nor does it represent the larger population of individuals with serious mental illness. Second, this study took place in New York City, and its findings cannot be considered representative of the experiences of rural or small town formerly homeless adults with SMI. At the same time, we note that participants’ demographic characteristics resemble those of their counterparts in other large cities in the United States (Locke et al., 2007).
Strengths of the study include several strategies for rigor used to reduce bias (Padgett, 2012). These included independently corroborated nominations for sample recruitment, independent ratings of adverse events using items from a previously validated checklist, and use of multiple sources of data for the case study analyses.
Recommendations for Practice, Policy, and Research
We present these findings to call attention to the extent of adversity but as importantly to contextualize it and explore its meaning for the survivors. The breadth and depth of this adversity represent often latent and poorly understood sources of emotional destabilization that undermine providers’ well-intended efforts to address manifest problems--as if serious mental illness, substance abuse, and homelessness were not enough to draw their attention.
Virtually all interventions for this population are intended to stabilize psychiatric symptoms and control or eliminate substance use while supplying some form of housing, whether temporary or permanent. Integrated treatment of mental illness and substance abuse has become widely embraced (Green & Drake, 2011), yet policies that focus solely on dual diagnoses risk neglecting underlying traumas dating from childhood. (Green et al., 2010).
Assistance in reclaiming a healthy, socially and economically productive life depends in part upon addressing the often-hidden psychological burdens of previous traumas, as well as the ongoing chronic stressors of poverty and social isolation. In this context, the promise of mental health recovery needs to be broadened to address complications beyond the admittedly daunting challenges of a serious mental illness such as schizophrenia. Research is needed that takes into account the life course perspective as well as broader contexts of influence in adulthood.
Figure 4.
Case study of Diana.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health (ROI MH084903). The authors thank the study participants for sharing their lives and stories.
References
- Aneshensel CS. Toward explaining mental health disparities. Journal of Health and Social Behavior. 2009;50:377–394. doi: 10.1177/002214650905000401. [DOI] [PubMed] [Google Scholar]
- Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology. 2002;31:285–293. doi: 10.1093/ije/31.2.285. [DOI] [PubMed] [Google Scholar]
- Deegan PE. The lived experience of using psychiatric medicine in the recovery process and a shared decision making program to support it. Psychiatric Rehabilitation Journal. 2007;31:62–69. doi: 10.2975/31.1.2007.62.69. [DOI] [PubMed] [Google Scholar]
- Draine J, Salzer MS, Culhane DP, Hadley TR. Role of social disadvantage in crime, joblessness, and homelessness among persons with serious mental illness. Psychiatric Services. 2002;53:565–573. doi: 10.1176/appi.ps.53.5.565. [DOI] [PubMed] [Google Scholar]
- Druss BG, Bornemann TH. Improving health and health care for persons with serious mental illness: The window for US federal policy change. Journal of the American Medical Association. 2010;303:1972–1973. doi: 10.1001/jama.2010.615. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the Adverse Childhood Experiences Study. The American Journal of Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Gould DA, Stevens NG, Ward NG, Carlin AS, Sowell HE, Gustafson B. Self-reported childhood abuse in an adult population in a primary care setting: Prevalence, correlates, and associated suicide attempts. Archives of Family Medicine. 1994;3:252–256. doi: 10.1001/archfami.3.3.252. [DOI] [PubMed] [Google Scholar]
- Green AI, Drake RE. Current epidemiology and emerging interventions for people with co-occurring mental illness and substance use disorders. Journal of Dual Diagnosis. 2011;7:1–3. doi: 10.1080/15504263.2011.571624. [DOI] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I: Associations with first onset of DSM–IV disorders. Archives of General Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins R, Abrams C. Disappearing acts: The social networks of formerly homeless individuals with co-occurring disorders. Social Science and Medicine. 2007;65:2031–2042. doi: 10.1016/j.socscimed.2007.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman DB, Susser ES, Stuening EL, Link BL. Adverse childhood experiences: Are they risk factors for adult homelessness? American Journal of Public Health. 1997;87:249–255. doi: 10.2105/ajph.87.2.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz AV, Widom CS, McLaughlin J, White HR. The impact of childhood abuse and neglect on adult mental health: A prospective study. Journal of Health and Social Behavior. 2001;42:184–201. doi: 10.1192/bjp.184.5.416. [DOI] [PubMed] [Google Scholar]
- Kim MM, Ford JD, Howard DL, Bradford DW. Assessing trauma, substance abuse, and mental health in a sample of homeless men. Health & Social Work. 2010;35:39–48. doi: 10.1093/hsw/35.1.39. [DOI] [PubMed] [Google Scholar]
- Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. A conceptual framework for personal recovery in mental health: Systematic review and narrative synthesis. British Journal of Psychiatry. 2011;199:445–452. doi: 10.1192/bjp.bp.110.083733. [DOI] [PubMed] [Google Scholar]
- Lloyd DA, Turner RJ. Cumulative lifetime adversities and alcohol dependence in adolescence and young adulthood. Drug and Alcohol Dependence. 2008;93:217–226. doi: 10.1016/j.drugalcdep.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke G, Khadduri J, O’Hara A. Dennis D, Locke G, Khadduri J, editors. Housing models. National symposium on homelessness research. 2007 Retrieved from http://aspe.hhs.gov/hsp/homelessness/symposium07/locke/index.htm.
- Metraux S, Culhane DP. Family dynamics, housing, and recurring homelessness among women in New York City homeless shelters. Journal of Family Issues. 1999;20:371–396. doi: 10.1177/019251399020003004. [DOI] [Google Scholar]
- O’Connell JJ. Premature mortality in homeless populations: A review of the Literature. Nashville, TN: National Health Care for the Homeless Council, Inc; 2005. [Google Scholar]
- Padgett DK. Qualitative and mixed methods in public health. Thousand Oaks, CA: Sage; 2012. [Google Scholar]
- Padgett DK, Hawkins RL, Abrams C, Davis A. In their own words: Trauma and substance abuse in the lives of formerly homeless women with serious mental illness. American Journal of Orthopsychiatry. 2006;76:461–467. doi: 10.1037/1040-3590.76.4.461. [DOI] [PubMed] [Google Scholar]
- Padgett DK, Struening E. Victimization and traumatic injuries among the homeless: Associations with alcohol, drug, and mental problems. American Journal of Orthopsychiatry. 1992;62:525–534. doi: 10.1037/h0079369. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Skaff MM. Stress and the life course: A paradigmatic alliance. The Gerontologist. 1996;36:239–247. doi: 10.1093/geront/36.2.239. Retrieved from http://gerontologist.oxfordjournals.org/content/36/2/239.full.pdf. [DOI] [PubMed] [Google Scholar]
- Perese EF, Wolf M. Combating loneliness among persons with severe mental illness; Social network interventions’ characteristics, effectiveness, and applicability. Issues in Mental Health Nursing. 2005;26:591–609. doi: 10.1080/01612840590959425. [DOI] [PubMed] [Google Scholar]
- Ridgway P. Restorying psychiatry disability: Learning from first person recovery narratives. Psychiatric Rehabilitation Journal. 2001;24:335–343. doi: 10.1037/h0095071. Retrieved from http://128.197.26.3/cpr/repository/articles/pdf/ridgway2001.pdf. [DOI] [PubMed] [Google Scholar]
- Seery MD, Holman EA, Silver RC. Whatever does not kill us: Cumulative lifetime adversity, vulnerability, and resilience. Journal of Personality and Social Psychology. 2010;99:1025–1041. doi: 10.1037/a0021344. [DOI] [PubMed] [Google Scholar]
- Sells DJ, Rowe M, Fisk D, Davidson L. Violent victimization of persons with co-occurring psychiatric and substance use disorders. Psychiatric Services. 2003;54:1253–1257. doi: 10.1176/appi.ps.54.9.1253. [DOI] [PubMed] [Google Scholar]
- Stein JA, Leslie MB, Nyamathi A. Relative contributions of parent substance use and childhood maltreatment to chronic homelessness, depression, and substance abuse problems among homeless women: Mediating roles of self-esteem and abuse in adulthood. Child Abuse & Neglect. 2002;26:1011–1027. doi: 10.1016/S0145-2134(02)00382-4. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Stress and health: Major findings and policy implications. Journal of Health and Social Behavior. 2010;51:S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Thornicroft G. Physical health disparities and mental illness: The scandal of premature mortality. The British Journal of Psychiatry. 2011;199:441–442. doi: 10.1192/bjp.bp.111.092718. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Cumulative adversity and drug dependence in young adults: racial/ethnic contrasts. Addiction. 2003;98:305–15. doi: 10.1046/j.1360-0443.2003.00312.x. Retrieved from https://campus.fsu.edu/bbcswebdav/institution/academic/social_sciences/sociology/Reading%20Lists/Mental%20Health%20Readings/Turner-Addiction-2003.pdf Wheaton, B. [DOI] [PubMed] [Google Scholar]
- Roszell P, Hall K. The impact of twenty childhood and adult traumatic stressors on the risk of psychiatric disorder. In: Gotlib IH, Wheaton B, editors. Stress and adversity over the life course: Trajectories and turning points. Cambridge, UK: Cambridge University Press; 1997. pp. 50–72. [Google Scholar]
- Wickrama KAS, Conger RD, Abraham WT. Early adversity and later health: The intergenerational transmission of adversity through mental disorder and physical illness. The Journals of Gerontology: SERIES R. 2005;60B(II):125–129. doi: 10.1093/geronb/60.special_issue_2.s125. Retrieved from http://psychsocgerontology.oxfordjournals.org/content/60/Special_Issue_2/S125.full.pdf. [DOI] [PubMed] [Google Scholar]