Abstract
In 2008, two-thirds of the annual global death toll was attributable to non-communicable diseases (NCDs). Defined as chronic conditions often caused or exacerbated by non-obligated lifestyle behaviours, the NCD epidemic has been fuelled by a combination of risk factors, including tobacco use, an unhealthy diet combined with lack of physical activity and overweight-obesity, and harmful alcohol use. The health consequences are mainly seen as cardiovascular diseases, diabetes, cancers and chronic respiratory problems. Generally associated with the West, they are now recognized as a global threat to public health. They are also an unsupportable global health economic burden. NCDs incidence can be significantly reduced through the adoption of proven and affordable interventional measures which are complementary to global health efforts already underway. To head off the certain future surge in morbidity and mortality, at record costs to health budgets worldwide, there is a pressing need to change global population's behaviours and choices in relation to these risk factors. The most pressing challenge in NCD prevention is combating the rise in overweight-obesity, which threatens individuals, communities and countries as never before. If not overcome, this may undo much of the progress seen in reducing the incidence of myocardial infarctions, strokes and some cancers evident from the 1960s onwards.
Non-Communicable diseases (NCDS) are defined as chronic non-transmissible diseases, usually acquired from, or exacerbated by, sub-optimal lifestyle choices. They include cardiovascular diseases, diabetes, cancers and chronic respiratory diseases, and today, are accountable for around two-thirds of the global death toll, with 80% of these preventable deaths occurring in the developing world.1
The epidemiological transition from communicable diseases (CDs) to non-communicable diseases (NCDs) being the major threat to health in low- and middle-income countries (LMICs) has emerged in the second half of the twentieth century.2 Diseases once traditionally associated with LMICs, such as malaria or HIV-AIDS, are now being rivaled, and soon will be surpassed in mortality importance, by NCDs to the extent that by 2020, NCD mortality is expected to exceed that of CDs in Africa.1,2 Following a first meeting in Moscow in early 2011, the United Nations High-Level Meeting (HLM) on Non-Communicable Diseases which took place in September 2011, marked a historical point as member states rallied together to develop a global response to the unprecedented surge in NCDs.3
NCD rates could be significantly reduced through the adoption of proven and affordable measures, many of which are complementary to global health efforts already underway. Finding ways to apply these solutions, and changing mindsets of those potentially affected by these diseases, is however a major challenge, requiring fresh approaches and thinking. There is an urgent need to change populations' behaviours and choices in their interactions with well-known and described risk factors, to avoid dramatic increases in morbidity and mortality from largely preventable disease. How best to effect this behavioural alteration is controversial, with opinion ranging from more ‘dirigiste’ interventions for individuals, society, countries and multinational corporations, to less direct, more subtle pressures, mostly at the level of individuals and their daily interactions.4,5
The biggest challenge facing individuals, societies and global health bodies is overweight-obesity. Developing since the 1960s and now gathering pace rapidly, it is, with ageing, contributing to major increases in the prevalence of raised blood pressure, raised cholesterol, type II diabetes and cancers.6,7 As successes against some vascular risk factors have become evident, especially in the West where the risk of heart attacks and strokes has fallen since the 1960s in many countries,8 the prevalence of overweight-obesity has increased to an alarming degree, and now threatens to undo progress made.6,7
In this article we explore the lessons we might be able to learn from other battles against global scourges, and from these lessons we consider approaches and solutions that might be employed in confronting overweight-obesity. In particular we focus on one recent communicable disease – HIV/AIDS – and one key NCD risk factor – tobacco consumption. In our discussion we ask whether the more ‘dirigiste’ approach taken to combat tobacco consumption would not be an effective approach to employ in tackling overweight-obesity, especially in motivating and helping people to make better choices around exercise and diet. We feel that more direct concerted action is now mandatory and should lead to more rapid impacts on people's perceptions, choices and behaviours.4,5
Methods
We searched PubMed, Embase and Wikipedia for all relevant articles from 1970 to 2011.
The global health context of NCDs and obesity – a burgeoning conundrum
In 2008, 36 million people died from NCDs worldwide, representing 63% of the 57 million deaths that year. By 2030, the date rate is expected to reach 52 million, around five times the death rate of CDs.9 Cardiovascular diseases are responsible for the largest proportion of NCD-related deaths under the age of 70 (39%), followed by cancers (27%). Together with chronic respiratory disease and diabetes, they are responsible for almost 80% of deaths caused by NCDs.1,2,3,9,10
This major healthcare burden does not simply affect the elderly; NCDs claim 9 million people's lives under 60 years of age every year and as such give dire predictions for the economic effect repercussions of LMICs, where NCDs have the most impact.10 Strong evidence links poverty, lack of education and other social determinants to such diseases and their risk factors. A vicious cycle reinforces this downward spiral, as NCDs and their risk factors worsen poverty while poverty results in rising rates of such diseases.2,9,10
The prevention of NCDs could help to reduce poverty, particularly since the majority of expenditures for treatment in low- and middle-income countries are paid to private healthcare systems, representing up to 50% of the total health expenditure of some LMICs.2,9 The World Health Organization's (WHO) World Health Report 2010 states that each year 100 million people descend into poverty because they had to pay directly for health services. A multi-country review of drug costs showed that it costs an average of two to eight days wages to purchase a one-month supply of at least one cardiovascular medicine.11
The report ‘The Global Economic Burden of non-Communicable Diseases’ issued to coincide with the UN conference and produced by the World Economic Forum, shows clearly that taking the next 20 years, NCDs will cost more than US$ 47 trillion, representing around 50% of global GDP in 2010, and pushing millions of people below the poverty line.12 By contrast, mounting evidence highlights how millions of deaths can be averted and economic losses reduced by billions of dollars if added focus is put on prevention. A recent WHO report underlines that population-based measures for reducing tobacco and harmful alcohol use, as well as unhealthy diet and physical inactivity, are estimated to cost US$ 2 billion per year for all low- and middle-income countries, which in fact translates to less than US$ 0.40 per person.12
Despite controversy over the definition of the ideal weight, and how to measure it,14 it is best defined as a BMI range of 21 to 23 kg/m2, with the goal of maintaining lifelong BMI in the range 18.5 to 24.9 kg/m2. There is increased co-morbidity risk for BMIs in the range 25.0 to 29.9 kg/m2 (‘overweight’), and moderate-to-severe risk for BMIs greater than 30 kg/m2 (‘obesity’).13
The worldwide prevalence of obesity has nearly doubled between 1980 and 2008. Globally, 10% of men and 14% of women in the world were obese (BMI ≥30 kg/m2) in 2008, compared to 5% for men and 8% for women in 1980.6 In the USA, obesity has now become a critical problem, though other countries are vying for parity, with nearly 70% of adults classified as overweight compared with fewer than 25% 40 years ago.15 Worldwide, 2.8 million people die each year as a result of being overweight (including obesity). An estimated 35.8 million (2.3%) of global Disability Adjusted Life Years (DALYs) are caused by overweight or obesity, with an even larger impact in the USA18 which rivals and possibly exceeds those statistics for tobacco consumption. Overweight and obesity lead to adverse metabolic effects on blood pressure, cholesterol, triglycerides and insulin resistance. Raised BMI also increases the risks not only of cardiovascular diseases but also several cancers – breast, colon/rectum, endometrium, kidney, oesophagus (adenocarcinoma) and pancreas.19
There is no sign of this trend reversing spontaneously; if it continues it has been modelled that there will be an additional 65 million obese adults in the USA and 11 million more obese adults in the UK by 2030, consequently accruing an additional 6–8.5 million cases of diabetes, 5.7–7.3 million cases of heart disease and stroke, 492,000–669,000 additional cases of cancer, and 26–55 million quality-adjusted life years forgone for USA and UK combined16 (Figure 1).
Figure 1.
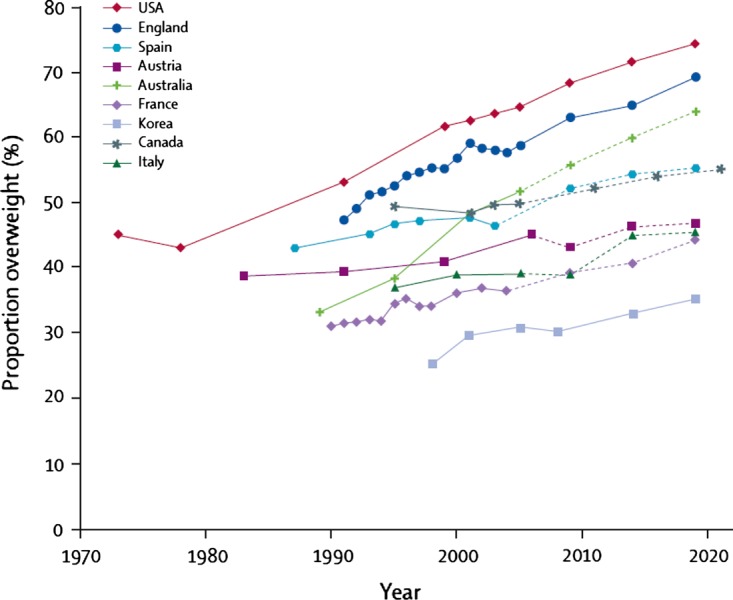
Percentage of the World Population who are overweight - with a BMI over 25 kg/m2 OECD data
Infants and young children are not spared: in 2008, WHO estimated 40 million (6%) preschool children who had a weight-for-height more than two standard deviations above the WHO child growth standards media, and with evidence that overweight children tend to become overweight adults,17 this is a worrying prediction of future trends.17 The combined medical costs associated with treatment of these preventable diseases are estimated to increase by $48–66 billion/year in the USA and by £1.9–2 billion/year in the UK by 2030.
It is generally accepted that this phenomenon has happened for many complex and complicated reasons, including decreased physical activity (changes in jobs, in housing, in transport, in social patterns), increased availability of energy-rich cheap food (enriched with sugar, salt and saturated fat). There is a real danger that it has now become the norm to accept cumulative excess weight gain, just as it was the norm for people to smoke cigarettes in the 1930s to 1990s, leading to the premature development of the many adverse metabolic consequences described above.
Exhortation and support for individuals to undertake dietary and exercise programmes are only modestly successful, while recidivism is typical. More conventional medicalized interventions can be strikingly effective at effecting weight loss but presently are only offered to the most severely affected (morbidly obese) people, usually with significant comorbid disease burdens.20
The relative ‘successes’ seen in combating HIV-AIDS and tobacco consumption – are there any translatable lessons for overweight-obesity interventions?
Lessons from HIV-AIDS
HIV is a communicable disease with identifiable behavioral risk factors. It leads to a chronic debilitating disease that is usually fatal in the absence of early detection and effective treatment. Although behaviour plays a major role in risk for HIV, for prevention efforts there is a need to integrate both behavioural and biomedical approaches — for example, promoting condom use and advances in biomedical interventions (e.g., microbicides, pre-exposure prophylaxis, and treatment as prevention) to allow a complementary reduction in transmission.21,22
Over the years, HIV-AIDS experts have come to accept three realities:
The search for cause and cure, and the fight against the pandemic must be global rather than national;
Prevention must inevitably be linked to early diagnosis;
Treatment must be available globally to be most effective.
In particular, the value of prevention with anti-retroviral drugs for individuals with and without HIV has emphasized the overlap of treatment and prevention, and reinforces the need for integrated strategies for epidemic control. Thirty years into the HIV/AIDS epidemic, clearly the separation of biomedical and behavioural prevention is deemed outdated and inefficient.22
Using these inclusive, holistic and focused approaches to screening, detection and treatment, in 2009, for the first time in history, the yearly incidence of HIV has levelled off, and started to decrease.21,22 Financial support nevertheless needs to be continuous: the global economic crisis has substantially affected funding for HIV.22
Lessons from measures to curb tobacco consumption
Tobacco consumption (usually cigarette smoking) is closely linked to chronic lung disease, cardiovascular disease and cancers. In 1964, the first US Surgeon General's report on the effects of smoking on health was released. In the nearly 50 years since, extensive data from thousands of studies have consistently substantiated the devastating effects of smoking on the lives of tens of millions of people around the world.23
From 1919, more tobacco was sold as cigarettes than in any other form, and consumption rose steadily until 1945, when it peaked at 12 manufactured cigarettes per adult male per day. Thereafter it remained at around 10 manufactured cigarettes per day until 1974 which marked the start of a steady and continuous decrease to 4.6 manufactured cigarettes per adult male per day in 1992. Similar consumption patterns were seen in women, though smoking rates, which only rose two to three decades after men's, continued to increase in women for two to three decades after they started to fall in men.24
A special and important feature of cigarette-smoking is the extent to which this adverse ‘behavioural choice’ is driven through addiction to nicotine. Nicotine is one of the most addictive substances known, and cigarette smoking is a true addiction for very many people, with many complex cues and triggers. The powerful addicting effects of commercial tobacco products are mediated by diverse actions of nicotine at multiple types of nicotinic receptors in the brain. Evidence suggests that there may be psychosocial, biologic, and genetic determinants associated with different trajectories observed among population subgroups as they move from adolescent experimentation to adult heavy smoking.25,26
Notwithstanding, or indeed probably because of, the highly-addictive nature of tobacco consumption, there has been extensive, sophisticated use of legislation against sales, distribution, packaging and advertising, pricing manipulation through taxation, prevention of smoking in public or work places, and public disapproval and rejection of smokers, in the battle to reduce this problem. Self-help, group-help, stopping smoking advice and support in the form of clubs and clinics all make important contributions to quit-rates, as does the use of nicotine substitutes or replacement products, and other pharmacological approaches.26 Lung cancer rates in men have fallen sharply over the last three decades as a result of the marked reduction in people smoking cigarettes long-term.27 See Figures 2 and 3.
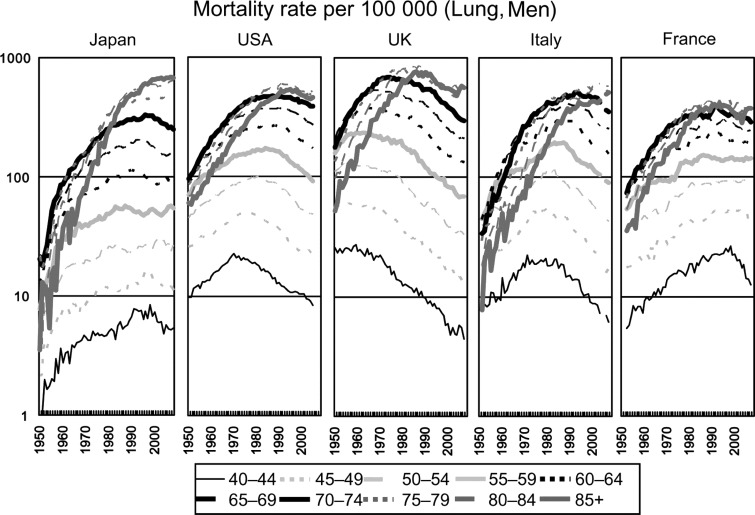
Figure 2.
(From reference 27 with permission). Lung cancer rates in men in five different countries, 1950 to present
Figure 3.
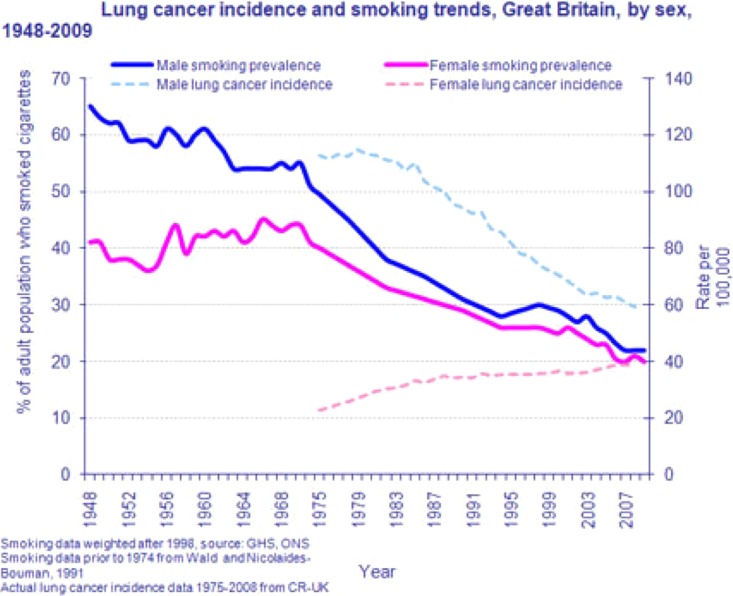
General Lifestyle Survey 2009: Smoking and drinking among adults, 2009, Office for National Statistics. 2011
Conclusions
Approaches, attitudes and attributes
As in HIV–AIDS, and cigarette smoking, lifestyle interventions are essential to addressing globesity. Prevention, screening and interventions around weight, food and exercise for obesity, must be closely coordinated, as has been the case in HIV-AIDS. Aggressive information campaigns, legislation, restrictions on sale and taxation, have worked effectively and cumulatively in combating tobacco and so should, we feel, be implemented in some form for obesity. Taxing ‘bad’ foods, and making access harder at the same time, seems a reasonable first step, and is now being adopted.
Further powerful stimuli are required to effect and sustain change. It is undeniable that biomedical interventions (e.g. generic statins, antihypertensive and anti-diabetic medications, or aspirin) benefit people at significant risk of, or already suffering from, cardiometabolic diseases, yet this ‘over-medicalized’ approach should not be the primary way to approach the problem – just as it should not be the case for smoking-cessation that the only way to quit is through a clinic, using prescribed interventions (either because it is too ‘late’ in the life-cycle of the disease, or, the medicalization leads to alienation for some, or, would mean very widespread use of medicine such as a ‘polypill’ used on a global scale). Table 1 compares all three health contexts.
Table 1.
Comparison of cigarette smoking, HIV-AIDS and overweight-obesity
| Disease | Tobacco-related Cancers | AIDS | Overweight - Obesity |
|---|---|---|---|
| Risk Factors | Tobacco exposure – mainly in the form of cigarette smoking | Unprotected Sex Needle Sharing Mother to Child Blood Transfusion |
Diet Lack of Exercise (minor genetic) |
| Historical Epidemiologic and Biologic Trends to Date | Smoking tobacco started in 17th century, but mass production of cigarettes and mass farming of nicotine led to mass consumption of cigarettes more by men than by women from early 20th century. In 1955 60% smoking rate, by 1970s, 55% and by 2007–8 around 20% in the UK | HIV emerged in the early 1980s in the context of blood transfusions, MSM, and drug addicts sharing infected needles. AIDS is the late manifestation of chronic immunodeficiency. Effective prophylactic and preventive drug regimens are now available to help reduce horizontal and vertical transmission rates. | Obesity known since ancient times, with adverse health consequences realized in ancient Greece and Egypt, and again in 18th century UK. Major change since WW2 esp since 1960s with more sedentary lifestyle coupled with major increase in calorie availability and consumption Prevalence increase as per text |
| Drivers/Promotors | Nicotine is intensely addictive Behavioural and social cues Price and availability of cigarettes Historic role models ‘cool’ - and promotion by advertising, brands |
Sex is enjoyable Monogomy not uniform Stigma of using condoms Stigma of homosexual sex in some countries Drug abuse Infected blood |
Easy and cheap to obtain high-GI high-calorie, high-fat, high-salt foods Some evidence of mild addiction/likings for certain ‘bad’ foods. Food and mood related. Vegetables and good foods less exciting, and can be expensive to buy and time-consuming to prepare TV, computers, lack of regular exercise times, cars not bicycles etc Childhood obesity rates rising sharply |
| Vulnerable period in life | Adolescence for starting smoking, then lifelong exposure through addiction, and climbing risk of cancer and other problems | Adolescence to middle-age (related mainly to sexual intercourse) | Significant weight gain and development of overweight and obesity is now very common aged 20 to 40 |
| International Efforts | RCP London report 1962 US Surgeon's General Report (1964) United Nations Meeting MDGs Research Funding |
HLM (1994) MDG Goals Research Funding |
Moscow Meeting (April 2011) UN HLM (September 2011) |
| Strategies | Public Health Campaigns Behavioural Modification Nicotine Replacement Council and Group Therapy |
Public Health Campaigns Global cooperation Prevention (condoms) Early Diagnosis Treatment for all (ARTs for all) |
Public Health Campaigns Behavioural Modification Paying for better food choices, for gym membership |
| Corporate Responsibility | Zero Tolerance Restricting cigarette distribution and sales Making less harmful products Avoiding economic exploitation of poorer countries |
Council and Group Therapy Provision of free, or heavily-subsidized, medication and other necessary equipment for LMICs |
Removing or making access difficult to fast food stores Reducing salt, saturated fat, calorie-contents of readily available foods Calorie and RDA charts on foods bought or served |
| Successes | Reduction of smoking population from 80% to 20% of UK adults in 60 years Reduction in Lung Cancers especially men |
First time that the epidemic may be reversed (seeing trends reverse if all ART treated) | At best some evidence from selected countries of a ‘flattening off’ of the rate of rise of overweight-obesity prevalence. |
| Favourable Trends | Yes, though less progress over last decade with ‘recalcitrant’ 15–20% smoking rates | Signs of a turnaround in global prevalence, and follow-through from HIV to AIDS | Steady deterioration with more overweight and obesity; at best some hints at stabilization in some countries |
Weight gain is particularly an issue for adolescents and young adults – moving from home and school to colleges and universities means exposure to alcohol, cheap high GI foods, and the desire to ‘shake off the shackles’ and enjoy life. These all conspire to promote rapid accumulation of body fat in many young people; this is often accepted as ‘normal’.28 Fat parents are more likely, for both genetic and behavioural reasons, to produce fat children, and fat children are more likely to become fat adults, and fat parents themselves. Breaking this ‘inevitability’ and ‘passive acceptance’ we feel is the key to success in the prevention of obesity.
We feel that the main ‘preventive’ priority in the ‘fight against fat’ is to target adolescents and young adults who are not yet obese, but close to, or already achieving overweight, and intensively to try to persuade them to adapt their behaviours. Lifelong weight charts, with mandatory yearly weight checks in school, university, workplace, and with each health service interaction, will help focus attention on this obvious risk factor. This, however, needs vigorous re-enforcement with calibrated, accessible and digestible information on the risks of overweight-obesity, strongly promoting exercise and good food choices. Here we believe that a number of exciting IT-based, readily accessible products could be of real value, as these are more likely to be acceptable to, and drive engagement with, at-risk younger cohorts. These should also of course include good advice on smoking and safer-sex.
The difference between ‘smoking’, which is driven through short-term nicotine-dependency induced craving-relief, and has no health benefit, and ‘eating’ which self-evidently is essential to maintain vitality, is obvious. But, some behavioural, genetic and societal factors in the overweight-obese may well produce similar behaviour-sets as we see in smokers.29 Nicotine-replacement, or substitution, is acceptable and successful in weaning nicotine-addicted people off cigarettes; getting people to make good food choices, and keep away from making bad ones, is a similar concept we feel. Ensuring that poorer-quality sugar-rich foods cannot be distributed so cheaply and readily by avaricious food companies is essential (thus mirroring societies' increasingly disapproving attitude to the major tobacco manufacturers, which set the scene for the deployment of legal instruments). Just because the battles with centralized conglomerated food manufacturers over the addition of salt, and phosphate, to food have not yet been won is no reason to stop trying – it arguably took four decades to ‘cow’ Big Tobacco, at least in many parts of the world. Provision of personal financial incentives to choose better foods, taxing less wholesome foodstuffs, providing free gym membership for those who attend, and who lose weight, all could all be important components of a successful strategy.
Of course, it may well be that with current and growing economic challenges to cheap food production, food distribution, and personal transport, there will be a necessary ‘rowing back’ in people's habits, choices and behaviour, as food and nutrient security and over-abundance may become less obvious. But it would be complacent to rely on this happening soon enough. It is also surely not right to leave these matters entirely to ‘market forces’, as these same forces have helped produce the abhorrent outcome of 20% of the world's population suffering from over-nutrition at the same time as 15% suffer from under-nutrition.30
If we employed measures which were a genuine marker of a societal ‘zero tolerance’ to obesity - as was seen with smoking – it would not be so easy (or desirable) to get fat, nor so easy to stay fat. This stricter approach of course still recognizes that behaviours are often complex and complicated, driven by many factors such as genetics and addictions, and judgmentalism per se has no value in providing solutions. All interventions, at the levels of the individual, family, community, country and internationally, need to be carefully coordinated and applied with precision. Overall though, we strongly advocate a much more ‘dirigiste’ approach to overweight-obesity over more subtle, gentle approaches; the sheer size and scale of this obesity pandemic now mandates urgent, concerted and co-ordinated action – the time for indecision has long gone.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Not applicable
Guarantor
DG
Contributorship
Eric Heymann and David Goldsmith were both equally involved in the conception and writing of the article.
Reviewer
Paul Clayton
References
- 1.Global Status Report on Noncommunicable Diseases. 2010. [(last accessed 21 September 2011)]. WHO 2011. See http://www.who.int/chp/ncd_global_status_report/en/index.html .
- 2.Alwan A, MacLean D A review of non-communicable disease in low and middle-income countries. International Health 2009;1:3–9 [DOI] [PubMed] [Google Scholar]
- 3. [(last accessed 24 September 2011)]. See http://www.un.org/en/ga/president/65/issues/ncdiseases.shtml .
- 4.Rayner G, Lang T Is nudge an effective public health strategy to tackle obesity? No. BMJ 2011;342:d2177 doi: 10.1136/bmj.d2177 [DOI] [PubMed] [Google Scholar]
- 5.Grant BC, Bassin S The challenge of paediatric obesity: more rhetoric than action. N Z Med J 2007;120:U2684 [PubMed] [Google Scholar]
- 6.Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL The global obesity pandemic, shaped by global drivers and local environments. Lancet 2011;378:804–814 [DOI] [PubMed] [Google Scholar]
- 7.Wysham CH New perspectives in type 2 diabetes, cardiovascular risk, and treatment goals. Postgrad Med 2010;122:52–60 [DOI] [PubMed] [Google Scholar]
- 8.Unal B, Critchley JA, Capewell S Modelling the decline in coronary heart disease deaths in England and Wales, 1981–2000: comparing contributions from primary prevention and secondary prevention. BMJ 2005;331:614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beaglehole R, Bonita R, Horton R, et al. Lancet NCD Action Group; NCD Alliance Priority actions for the non-communicable disease crisis. Lancet 2011;377:1438–47 Epub 2011 Apr 5 [DOI] [PubMed] [Google Scholar]
- 10.Dans A, Ng N, Varghese C, Tai ES, Firestone R, Bonita R The rise of chronic non-communicable diseases in southeast Asia: time for action. Lancet 2011;377:680–9 [DOI] [PubMed] [Google Scholar]
- 11.World Health Organisation : World Health Report 2010
- 12.World Economic Forum, Harvard School of Public Health. 2011. The Global Economic Burden of Non-Communicable Diseases. September.
- 13.Health Implications of Obesity National Institutes of Health Consensus Development Conference Statement 1. National Institutes Of Health Consensus Development Panel On The Health Implications Of Obesity. Ann Int Med 1985;103:1073–7 [PubMed] [Google Scholar]
- 14.Walls HL, Stevenson CE, Mannan HR, et al. Comparing trends in BMI and waist circumference. Obesity (Silver Spring) 2011;19:216–9 [DOI] [PubMed] [Google Scholar]
- 15.Lavie CJ, Milani RV, Ventura HO Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol 2009;53:1925–32 [DOI] [PubMed] [Google Scholar]
- 16.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378:815–25 [DOI] [PubMed] [Google Scholar]
- 17.Han JC, Lawlor DA, Kimm SY Childhood obesity. Lancet 2010;375:1737–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jia H, Lubetkin EI Obesity-related quality-adjusted life years lost in the U.S. from 1993 to 2008. Am J Prev Med 2010;39:220–7 [DOI] [PubMed] [Google Scholar]
- 19.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 2009;9:88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benraouane F, Litwin SE Reductions in cardiovascular risk after bariatric surgery. Curr Opin Cardiol 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Narayan KM, Ali MK, del Rio C, Koplan JP, Curran J Global noncommunicable diseases–lessons from the HIV-AIDS experience. N Engl J Med 2011;365:876–8 [DOI] [PubMed] [Google Scholar]
- 22.Padian NS, McCoy SI, Karim SS, et al. HIV prevention transformed: the new prevention research agenda. Lancet 2011;378:269–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. [(last accessed 24 September 2011)]. See http://www.cdc.gov/tobacco/data_statistics/sgr/2010/index.htm .
- 24.Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults and trends in smoking cessation – United States, 2008. MMWR Morb Mortal Wkly Rep 2009;58:1227–32 [PubMed] [Google Scholar]
- 25.Raupach T, van Schayck CP Pharmacotherapy for smoking cessation: current advances and research topics. CNS Drugs 2011;25:371–82 [DOI] [PubMed] [Google Scholar]
- 26.Healthy lives, healthy people – a tobacco control plan for England. Department of Health report March 2011. Commentary from Royal College of Physicians by Professor John Britton.
- 27.Katanoda K, Yako-Suketomo H Time trends in lung cancer mortality between 1950 and 2008 in Japan, USA and Europe based on the WHO mortality database. Jpn J Clin Oncol 2011;41:1046–7 [DOI] [PubMed] [Google Scholar]
- 28.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA Emerging adulthood and college-aged youth: an overlooked age for weight-related behaviour change. Obesity (Silver Spring) 2008;16:2205–11 [DOI] [PubMed] [Google Scholar]
- 29.Davis C, Curtis C, Levitan RD, Carter JC, Kaplan AS, Kennedy JL Evidence that 'food addiction' is a valid phenotype of obesity. Appetite 2011;57:711–717 [DOI] [PubMed] [Google Scholar]
- 30.International Federation of the Red Cross Annual Disaster Report (2011). See http://www.ifrc.org/en/publications-and-reports/world-disasters-report/ (last accessed 24 September 2011)