Abstract
Objective
To compare the effects of a coverage expansion versus a Medicaid physician fee increase on children's utilization of physician services.
Primary Data Source
National Health Interview Survey (1997–2009).
Study Design
We use the Children's Health Insurance Program, enacted in 1997, as a natural experiment, and we performed a panel data regression analysis using the state-year as the unit of observation. Outcomes include physician visits per child per year and the following indicators of access to primary care: whether the child saw a physician, pediatrician, or visited an ER in the last year, and whether the parents reported experiencing a non-cost-related access problem. We analyzed these outcomes among all children, and separately among socioeconomic status (SES) quartiles defined based on family income and parents' education.
Principal Findings
Children's Health Insurance Program had a major impact on the extent and nature of children's insurance coverage. However, it is not associated with any change in the aggregate quantity of physician services, and its associations with indicators of access are mixed. Increases in physician fees are associated with broad-based improvements in indicators of access.
Conclusions
The findings suggest that (1) coverage expansions, even if they substantially reduce patient cost sharing, do not necessarily increase physician utilization, and (2) increasing the generosity of provider payments in public programs can improve access among low-SES children, and, through spillover effects, increase higher-SES children as well.
Keywords: Children's Health Insurance Program, physician utilization, physician fees, coverage expansion, access
The Patient Protection and Affordable Care Act (PPACA) takes several approaches to expanding access to health care. One approach is to expand public coverage by making anyone with income below 138 percent of the poverty level eligible for Medicaid. A second approach is embodied in the requirement that states increase their Medicaid physician fee schedules, so that they are no lower than Medicare's. The expansion of public coverage, which takes effect in 2014, is far-reaching and permanent. According to the Congressional Budget Office (), it will move roughly 15 million individuals onto Medicaid. The increase in fees is a much more limited provision—it applies only to so-called evaluation and management services provided by primary care physicians, and it only applies to services provided in 2013 or 2014.
We use a recent historic example—the establishment of the Children's Health Insurance Program (CHIP)—to measure the effects of a coverage expansion on the utilization of physician services, and we compare those effects with the effects of an increase in Medicaid physician fees. The prevailing view is that expanding eligibility for public coverage will, by reducing patient cost sharing, lead to an increase in the aggregate quantity of medical services provided. This view is embodied in the official estimates of the effects of health reform on national health spending (Office of the Actuary 2009, 2010). The findings presented below are not consistent with that prevailing model, but are consistent with a model in which the overall quantity of services and access to services is primarily determined by the generosity of provider payments.
Previous Literature
The existing literature on the effects of health insurance coverage expansions can be divided into two strands: (1) microlevel analyses that measure the effects specifically among individuals who newly gain coverage, and (2) macrolevel analyses that measure the effects of a coverage expansion on overall utilization patterns, including populations that did not become newly eligible or newly covered. The micro- and macrolevel strands differ in the assumptions that underlie the choice of methodology, and in the interpretation of their results. Microlevel analyses, by definition, assume that a coverage expansion only affects those individuals who become newly covered or newly eligible (i.e., “no spillovers”). Macrolevel analyses, in contrast, allow for two possibilities: (1) that a coverage expansion might have spillover effects on individuals who do not themselves become newly eligible or covered, and (2) that the aggregate effect of a coverage expansion depends on whether and how it impacts the supply side of the market. Notably, those two strands tend to arrive at very different conclusions regarding the effects of coverage expansions on utilization.
The seminal microlevel analysis is the RAND Health Insurance Experiment (HIE), a large-scale randomized trial conducted during the late 1970s and early 1980s (Newhouse and the Insurance Experiment Group 2011). The HIE compared individuals assigned to a health insurance plan with no cost sharing (free care), with individuals assigned to plans with cost sharing. Those in the free care plan were more likely to receive some medical services during the year, and they had substantially more medical encounters and higher expenditures. It is crucial to recognize that the HIE is a microlevel analysis—by design, it only tracked utilization patterns among study participants, and it was not designed to detect possible spillover effects on nonstudy participants.
Since the HIE, a vast number of microlevel analyses have used observational data to examine the effects of insurance coverage on utilization. Those studies have generally come to findings consistent with the HIE (Buchmueller et al. 1994). Some of the earlier observational studies consisted of cross-sectional comparisons between individuals with health insurance coverage versus those without. Newacheck et al. (1998), based on a simple cross-sectional bivariate comparison between insured versus uninsured, show that insured children have substantially more physician contacts per year than uninsured children. Long and Marquis (1994) also perform a cross-sectional analysis, but they control to the extent possible for observable differences—that comparison showed that insured children visit the doctor roughly once more per year compared with uninsured children. The more recent studies generally use coverage expansions as natural experiments. For example, Banthin and Selden (), using a difference-in-differences (DD) analysis, find that the expansion of eligibility for Medicaid between 1987 and 1996 increased the percentage of children with at least one doctor visit in the last year. Lurie (2007) also uses a DD design and finds that the CHIP expansions between 1996 and 2001 increased the percentage of children with at least one doctor visit. Selden and Hudson (2006), using an instrumental variables design that takes advantage of expansions in eligibility for public programs between 1996 and 2002, report that public coverage substantially increases the likelihood that a child has one or more ambulatory visits.1
The microlevel analysis that is most closely related to ours is by Currie and Gruber (1996). Their paper, which measures the effects of the 1980s Medicaid expansions on physician utilization and mortality among children, reports that gaining Medicaid eligibility is associated with a reduction in the share of children who did not see a doctor in the last year (from roughly 20 to 10 percent). They also report that Medicaid eligibility is associated with an increase in the number of doctor visits (roughly one visit per year), but that estimate is imprecisely estimated and is not statistically significant.
The key difference between Currie and Gruber (1996) and our study is that they take a microlevel approach, whereas we take a macrolevel approach. Currie and Gruber simulate Medicaid eligibility and measure its effects at the level of the state-year-age group. Implicitly, this approach assumes that changes in utilization within a given age group have no spillover effects on utilization among children in other age groups. Dafny and Gruber (2005) use essentially the same methodology to measure the effect of Medicaid expansions on children's rate of hospitalization. These microlevel studies are not designed to detect spillovers or supply-side responses, and their results are therefore not appropriate for estimating aggregate utilization effects.
Macrolevel analyses of coverage expansions clearly reject the “no spillovers” assumption. Stewart and Enterline (1993) analyzed the effects on physician utilization of the establishment of the National Health Service (NHS) in England and Wales in the late 1940s (Stewart and Enterline 1993). They compared physician utilization patterns pre- versus post-NHS separately among groups that gained coverage (women, the elderly, and low-income men) and those that already had coverage prior to the NHS (high-income men). Their results show that the NHS substantially increased physician utilization among the groups that gained coverage, and substantially reduced physician utilization among high-income men who generally already had coverage.
Another classic macrolevel analysis is Enterline et al. They analyzed the effects of the establishment in 1970 of Quebec's universal coverage scheme (Enterline 1973). They conducted a pair of household surveys (one preexpansion, one post) focusing on physician utilization patterns. They found that the overall average number of physician visits was precisely unchanged following universal coverage (5.04 per person per year both pre- and post-), but they found strong evidence that the expansion redistributed services across income groups. The lowest-income group, who was most likely to gain coverage, increased their physician visit rate by 18.2 percent, whereas the highest-income group, which generally already had coverage, decreased their physician visit rate by 9.4 percent.
Finkelstein (2009) also examines the macrolevel effects of a major coverage expansion, in this case, the implementation of the U.S. Medicare program for the elderly beginning in 1966 (Finkelstein 2009). She reports that the establishment of Medicare was associated with an increase in system-wide hospital utilization and hospital spending roughly six times larger than what would be predicted based on the demand-side response to reduced cost sharing reported in the HIE findings. Her analysis suggests that the Medicare-induced increase in spending occurred both among the elderly (the target population) and the nonelderly (a spillover population). The positive spillover effect that Finkelstein observes is likely due to supply-side effects and the fact that, when first introduced, Medicare provided very generous cost-based reimbursements to hospitals, which encouraged hospitals to expand capacity.
Using the results of microlevel analyses to estimate the macrolevel effects of a coverage expansion appears to be an unwarranted oversimplification. The fundamental problem with the microlevel approach is that it assumes that we can identify a control group that is unaffected by the coverage expansion. If spillover effects exist, either due to queuing or to a change in the reimbursement environment, then an unaffected group may not exist. Stewart and Enterline et al.'s results indicate that spillovers can reduce utilization among the previously insured (due to queuing), whereas Finkelstein's results indicate that supply-side spillovers can increase utilization.
There is a more specific concern with using the HIE results to simulate the effects of coverage expansions, as some have done.2 The most well-known and widely cited HIE results are those comparing enrollees in different types of indemnity (unmanaged) health insurance plans with varying levels of patient cost sharing. That comparison ignores the utilization effects of managed care techniques such as utilization review, limited provider panels, and gatekeeping. As abundant evidence indicates (including the HMO arm of the HIE experiment itself), managed care can affect utilization and spending to at least the same degree as cost sharing.
A third related strand of literature is on the effects of increasing Medicaid fees on utilization and access. Those studies show fairly consistently that increased payment generosity leads to increased access to services and increased utilization. Previous analyses have examined the effects of Medicaid fees on physician participation (Adams 1994) and the effects of increased global capitation payments on utilization (Shen and Zuckerman 2009). The most recent and carefully done study in this strand is by Decker (2010), who finds that increases in Medicaid physician fees increase the number of physician visits among Medicaid enrollees and lead to a shift in the site of care (toward physician offices and away from hospital outpatient and emergency departments).
What Is CHIP, and What Does It Do?
Children's Health Insurance Program was established as Title XXI of the Social Security Act by the Balanced Budget Act of 1997 (BBA). CHIP and Medicaid are layered programs, in the sense that CHIP eligibility begins at the income level where Medicaid eligibility ends and extends to higher-income levels. In both the Medicaid and CHIP programs, income eligibility cutoffs vary by state. Typical current Medicaid income cutoffs are 100 percent of the federal poverty level (FPL) for older children, and 185 percent of the FPL for younger children. Children up to age 19 may be eligible for the Medicaid and CHIP programs, and CHIP income eligibility cutoffs in 2009 ranged from 155 percent of the of the FPL in North Dakota to 400 percent in New York—typically cutoffs are between 200 and 300 percent of the FPL.
Children's Health Insurance Program is large enough that its effects appear clearly in aggregate coverage statistics. In 2009, roughly 20 percent of children were in families in the CHIP income range—low enough to be CHIP-eligible, but too high to be Medicaid-eligible. In that year, 6.3 percent of children were enrolled in CHIP on a point-in-time basis, and 9.8 percent of children were enrolled in CHIP at some point during the year. According to the U.S. Census Bureau, there has been a decline, beginning in 1998, in the share of children uninsured and, at the same time, an increase in the share of children with public coverage (DeNavas-Walt, Proctor, and Lee 2006; DeNavas-Walt, Proctor, and Smith 2010). The adult population, which was not directly affected by CHIP, experienced very different trends, with rates of uninsurance increasing over that period.
Expansion of the CHIP program has important effects on both the demand and supply sides of the market for physician services. Among children who enroll in CHIP, some would otherwise be uninsured—for those children, the most obvious effect of CHIP is a reduction in patient cost sharing. Other children who enroll in CHIP would otherwise be enrolled in a private plan—they also enjoy a reduction in cost sharing because CHIP, compared with private plans, generally has much lower deductibles, copayments, and coinsurance. From a demand perspective, therefore, we would expect CHIP to increase utilization.
However, enrolling children in CHIP has important supply-side effects that would tend to constrain physician utilization. CHIP plans tend to employ managed care tools, such as gatekeepers and closed panels, much more intensively than private plans.3 CHIP expansions also appear to reduce the average payment rate that physicians receive. For children who enroll in CHIP rather than a private health plan, the difference in payment rates is substantial. Based on an actuarial model built by Ingenix for the American Academy of Pediatrics, the national average payment rate for a physician office visit was $81 for a privately insured child versus only $47 for a child enrolled in a public plan (Medicaid or CHIP) (Ingenix Consulting 2009a, b). (The Ingenix model, unfortunately, does not differentiate between payment rates under Medicaid versus CHIP.) There is also evidence to suggest that physicians' revenue from treating Medicaid and CHIP patients is even lower than the revenue they receive from treating the uninsured even taking into account charity care and uncollected bills (Gruber and Rodriguez 2007).4
The effect of CHIP on physician utilization will therefore reflect several factors, including: (1) lower levels of patient cost sharing among enrollees, (2) the expanded use of managed care tools, and (3) a reduction in the average fees that physicians receive. As those factors can work in opposite directions, the net effect of CHIP remains uncertain a priori.
Methodology and Data Sources
The goal of our analysis is to measure the macrolevel effects of CHIP expansions and changes in Medicaid fees on aggregate physician utilization, including direct effects among children who newly enrolled in public coverage as well as indirect spillover effects among high socioeconomic status (SES) children who were not eligible and did not enroll. Possible spillover effects could include increased utilization due to expanded provider capacity (as found in Finkelstein's Medicare analysis) or a decrease in utilization due to queuing (as found in Enterline's Canadian and British analyses).
Our approach is to compare trends in utilization and access among children living in states with (1) large CHIP expansions versus small CHIP expansions, and (2) increases versus decreases in Medicaid physician fees. We chose the state-year as our unit of observation and calculated our key predictors and outcomes as state-year averages. We specifically chose not to make comparisons between children enrolled in CHIP versus other children within a state. If there are any spillover effects, this type of within-state comparison will produce misleading results because the group of children outside the CHIP income range will be affected by CHIP as well.
Our data on physician utilization come from the NHIS, which is a large-scale annual household survey conducted jointly by the National Center for Health Statistics and the Bureau of the Census. The NHIS “sample child” questionnaire includes detailed items on utilization of physician services, hospitals, and emergency rooms. We performed our analysis at the National Center for Health Statistics Research Data Center using non-publicly available files that identified respondents' state of residence. The number of sample children used in each year ranges from 8,518 in 2008 to 13,747 in 1997. In total, we used 150,475 child-year observations to create our state-year files. About 4 percent of the NHIS sample children (6,270 of 156,745) were excluded from the analysis because one or more key data items had missing values.
Our regression analyses include Census division-year fixed effects to allow for region-specific time trends and state-fixed effects to account for idiosyncratic state characteristics. We use the following general linear specification:
| (1) |
where s indexes states, d indexes Census divisions, t indexes years, αs is a set of state-fixed effects, βd,t is a set of division-year fixed effects, Xs,t is a limited set of time-variant controls (the natural logarithm of gross state product per capita, and the unemployment rate), Fees,t is the state's Medicaid physician fee index for primary care services, and  is an index of the size of each state's CHIP expansion that is equal to the predicted share of the under-19 population enrolled in CHIP. These regressions are referred to as “reduced form” models because they take the predicted value from a first-stage model (
is an index of the size of each state's CHIP expansion that is equal to the predicted share of the under-19 population enrolled in CHIP. These regressions are referred to as “reduced form” models because they take the predicted value from a first-stage model ( ) and enter it directly into the second-stage model. All outcome variables are entered into the regressions in their natural units (e.g., visits per year, or the share of children [0,1]). We calculate robust standard errors to account for clustering at the state level using Stata's “cluster()” option (StataCorp, College Station, TX, USA).
) and enter it directly into the second-stage model. All outcome variables are entered into the regressions in their natural units (e.g., visits per year, or the share of children [0,1]). We calculate robust standard errors to account for clustering at the state level using Stata's “cluster()” option (StataCorp, College Station, TX, USA).
The Medicaid fee index reflects fees paid for primary care services and is calculated from a series of reports by Stephen Norton, Stephen Zuckerman, and others at the Urban Institute. It is defined such that a value of 1.00 indicates that Medicaid fees are equal to Medicare fees for the same services. That index, although it is the best available, has several notable limitations: (1) it only reflects fees paid through Medicaid fee-for-service and primary care case management arrangements, which excludes Medicaid HMO plans; and (2) it does not separately report (or, in earlier years, even incorporate) fees paid in CHIP plans; and the underlying data are only gathered roughly every 4 years.5
Budgetary surpluses and shortfalls appear to be the main factors prompting states to change their Medicaid fees. Other factors affecting fees include legal challenges by providers and changes in federal policy such as the repeal of a provision for “adequate payment levels for obstetrical and pediatric services” in late 1997 (Medicaid and CHIP Payment and Access Commission 2011). Therefore, on the whole, it seems reasonable to treat the Medicaid fee as exogenous.
The size of each state's CHIP expansion was measured using the predicted values from a regression of the actual share of children enrolled in CHIP (from administrative data) on two key features of state CHIP programs: the share of children who were made newly income-eligible for public coverage due to CHIP, and the share of children who were income-eligible for CHIP but subject to a long (6 months or greater) waiting period. The share of children income-eligible for CHIP and the share subject to long waiting periods were both simulated for each state-year by applying that state's program rules to a fixed national sample of children from the 2004 Survey of Income and Program Participation. (See Appendix SA1.) This generally follows the “simulated instrument” approach used by Currie and Gruber (1996).
One of our analytical goals was to distinguish, to the extent possible, between the direct effects of CHIP among those children who enrolled in CHIP versus the indirect spillover effects among children whose family income was too high to be eligible. With this goal in mind, we divided children into four SES groups (SES quartiles). As a summary measure of SES, we used a child's predicted likelihood of enrolling in public coverage (Medicaid or CHIP), as a function of their families' economic and educational characteristics. Children in quartile 1 have the highest family incomes and the most highly educated parents, and are least likely to be enrolled in public coverage, whereas children in quartile 4 have the lowest family incomes and the least well educated parents and are the most likely to be enrolled in public coverage. (See Appendix SA1 for details.)
A much more detailed description of the methodology and data sources is available in Appendix SA1. Appendix SA1 includes descriptive analyses of state CHIP program features, formal mathematical descriptions of the regression models, as well as detailed regression output, including OLS results, 2SLS results, and first-stage regressions.
Results
Table 1 describes the differences between states with small, medium, and large CHIP expansions. States with large expansions tended to have more restrictive Medicaid income eligibility criteria in 1997, they tended to expand income eligibility more through their CHIP programs, and they also tended to be more urban, to have larger Latino populations, and not to be in the Midwest. Those differences underscore the need to include state- and division-year fixed effects. Table 1 also presents the mean number of physician visits per child per year in 1997–1998 (pre-CHIP), and the percent change from 1997–1998 to 2008–2009 (multiple years were pooled to increase stability in these estimates). Based on these simple descriptive statistics, large CHIP expansions do not appear to increase physician utilization—physician utilization decreased relatively more in states with the largest expansions.
Table 1.
A Comparison of States with Small versus Large Children's Health Insurance Program (CHIP) Expansions
| Characteristics of State Populations | Small CHIP Expansion | Medium CHIP Expansion | Large CHIP Expansion |
|---|---|---|---|
| Share of children enrolled in CHIP, 2009 (%) | 3.8 | 5.9 | 8.5 |
| Share of children eligible for Medicaid, 1997 rules (%) | 31.1 | 27.5 | 27.8 |
| Share of children eligible for Medicaid/CHIP, 2009 rules (%) | 46.8 | 50.2 | 50.3 |
| CHIP expansion population, 2009 (%) | 15.8 | 22.7 | 22.5 |
| Share of children in CHIP expansion population and subject to 6+ month waiting period under 2001 rules (%) | 2.2 | 3.8 | 2.4 |
| Urban (%) | 76.2 | 72.3 | 86.1 |
| Income per capita ($2,000, 000s) | 29.1 | 28.7 | 30.2 |
| In poverty (%) | 9.9 | 10.7 | 13.1 |
| Education levels among adults | |||
| Less than high school degree (%) | 17.0 | 18.9 | 22.5 |
| 4-Year college degree (%) | 24.8 | 23.2 | 24.8 |
| Black (%) | 10.2 | 11.3 | 14.8 |
| Latino (%) | 8.4 | 4.6 | 21.7 |
| Number of children, 2009 (millions) | 26.0 | 20.6 | 32.4 |
| List of states | AZ, CO, CT, DC, DE, IA, ID, IL, IN, MI, MN, ND, NH, NM, NV, OR, SC, TN, UT, VA, VT, WA, WI, WY | AK, AL, AR, HI, KS, KY, MA, ME, MO, MT, NC, NE, NJ, OH, OK, PA, RI, SD, WV | CA, FL, GA, LA, MD, MS, NY, TX |
| Region | |||
| Northeast (%) | 5.7 | 37.3 | 17.2 |
| South (%) | 19.7 | 31.1 | 52.2 |
| Midwest (%) | 45.8 | 28.1 | 0.0 |
| West (%) | 28.8 | 3.5 | 30.7 |
| Physician visits per child per year, 1997–1998 | 3.35 | 3.61 | 3.17 |
| Physician visits per child per year, 2008–2009 | 3.34 | 3.62 | 3.14 |
| Change in physician visits, 1997–1998 versus 2008–2009 (%) | −0.4 | 0.5 | −1.1 |
Notes. States are assigned to terciles by ranking states by the predicted share of children enrolled in CHIP in 2009 and grouping states, so that roughly equal numbers of children would be included in each tercile. Source is author's calculations. Predicted CHIP enrollment shares are calculated using Medicaid and CHIP income eligibility criteria and CHIP waiting periods (see Appendix SA1). The characteristics of state populations are calculated from 2000 Census data (as reported in the Area Resources File).
Table 2 describes the differences among the children in the SES quartiles. As expected, the quartiles differ dramatically in family income levels, mother's educational achievement, and trends in coverage. Among the children in quartile 1 (the highest SES group), the share enrolled in private coverage was about 95 percent both in 1997–1998 and in 2008–2009, and the share enrolled in public coverage increased by <2 percentage points (from 0.3 to 2.2 percent). Consequently, if we find that CHIP is associated with changes in utilization among children in SES quartile 1, we can interpret those effects mainly as spillover effects. In contrast, in the lower-SES quartiles (3 and 4), enrollment in public coverage increased substantially between 1997–1998 and 2008–2009. In quartile 3, the main coverage shift was from private to public, whereas in quartiles 4, there were major shifts both from private to public coverage and from uninsured to public coverage.
Table 2.
A Comparison of Children in Different Socioeconomic Status Quartiles
| Highest | Lowest | |||
|---|---|---|---|---|
| Characteristics of Children | Q1 | Q2 | Q3 | Q4 |
| Family income (%) | ||||
| <100% FPL | 0.0 | 0.0 | 3.7 | 70.7 |
| 100–300% FPL | 3.9 | 43.3 | 84.4 | 29.3 |
| 300–500% FPL | 44.5 | 40.0 | 8.9 | 0.0 |
| ≥500% FPL | 51.6 | 16.7 | 3.0 | 0.0 |
| Mother's education (%) | ||||
| Less than high school degree | 0.3 | 4.8 | 18.1 | 38.7 |
| 4-Year college degree | 64.8 | 17.6 | 9.2 | 2.3 |
| Coverage, 1997–1998 (%) | ||||
| Medicaid/CHIP | 0.3 | 1.9 | 11.7 | 50.2 |
| Private | 95.0 | 90.0 | 66.3 | 24.1 |
| Uninsured | 2.5 | 5.7 | 18.5 | 22.2 |
| Coverage, 2008–2009 (%) | ||||
| Medicaid/CHIP | 2.2 | 9.0 | 39.9 | 73.4 |
| Private | 94.0 | 80.1 | 41.6 | 11.0 |
| Uninsured | 1.9 | 7.2 | 14.5 | 11.0 |
| Change in coverage, 1997–1998 versus 2008–2009 (percentage points) | ||||
| Medicaid/CHIP | 1.9 | 7.1 | 28.2 | 23.3 |
| Private | −1.0 | −9.9 | −24.7 | −13.2 |
| Uninsured | −0.5 | 1.5 | −4.0 | −11.2 |
| Doctor visits per child per year | 3.7 | 3.4 | 3.1 | 3.2 |
| Saw doctor in last year (%) | 86.1 | 80.7 | 74.7 | 73.5 |
| Saw pediatrician in last year (%) | 57.8 | 46.6 | 41.5 | 40.6 |
| One or more visits to an emergency room in last year (%) | 15.9 | 17.9 | 21.7 | 26.9 |
| Experienced access problem due to waiting (%) | 6.2 | 6.9 | 8.6 | 11.0 |
Notes. Children are assigned to a socioeconomic status quartile on the basis of their predicted likelihood of enrolling in Medicaid or Children's Health Insurance Program (CHIP) (see Appendix SA1 for details). Source is author's calculations using the National Health Interview Surveys (1997–2009). The coverage statistics are calculated using the years indicated; all other statistics are calculated using all years.
Figure 1 summarizes the estimated effects of CHIP expansions on insurance coverage, using the parameter estimates from the reduced form models described above. The height of each bar is scaled to represent the difference between a large CHIP expansion state (predicted enrollment of 8.3 percent) versus a small CHIP expansion state (predicted enrollment of 4.0 percent, i.e., a difference of 4.3 percentage points). These regression results, consistent with the descriptive statistics in Table 2, indicate that the direct enrollment effects of CHIP were heavily concentrated in quartiles 2 through 4 (i.e., the middle- and lower-income groups). The regression results also suggest that crowdout is roughly 1-for-1 in quartile 2 but is much smaller in quartiles 3 and 4. Among children in quartiles 1 and 2 (the two higher-income groups), the size of their state's CHIP expansion made little difference to whether they were uninsured. Among children in quartiles 3 and 4, in contrast, the larger CHIP expansions are associated with reductions in uninsurance.
Figure 1.

Estimated Effects on Insurance Coverage of a Large versus Small Children's Health Insurance Program (CHIP) Expansion (all children and separately by socioeconomic status quartile)Notes. The bar heights represent the estimated effects of CHIP enrollment under a large versus small expansion (i.e., a difference in enrollment of 4.7 percentage points) estimated using reduced form models. Children are assigned to a socioeconomic status quartile on the basis of their family income and parents' educational status (see Appendix SA1 for details). The drop bars indicate ±1 standard error. The results represent enrollment differences in percentage points. *p < .10, **p < .05, ***p < .01
Figure 2 summarizes the estimated coefficients on the CHIP expansion variable from a series of reduced form models. In the analyses of physician visits, all of the estimates are close to zero and not statistically significant. Unfortunately, the results on doctor visits are not precisely estimated due to the variability in the underlying measure. The only statistically significant results are as follows: in quartile 4, CHIP is associated with a decrease in the share of children visiting the emergency room, and in quartile 2, CHIP is associated with an increase in the share of children whose parents report experiencing a non-cost-related access problem.
Figure 2.
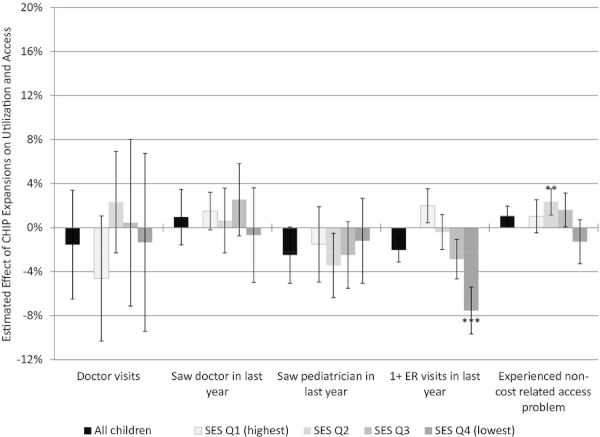
Estimated Effects on Utilization of a Large versus Small Children's Health Insurance Program (CHIP) Expansion (all children, and separately by socioeconomic status quartile)Notes. The bar heights represent the estimated effects of CHIP enrollment under a large versus small expansion (i.e., a difference in enrollment of 4.7 percentage points) estimated using reduced form models. Children are assigned to a socioeconomic status quartile on the basis of their family income and parents' educational status (see Appendix SA1 for details). The drop bars indicate ±1 standard error. The results represent enrollment differences in percentage points. *p < .10, **p < .05, ***p < .01
Figure 3 summarizes the estimated coefficients on the Medicaid physician fee index. The height of the bars in Figure 3 is scaled to represent the estimated difference between an increase of 15 percent in the fee index versus a decrease of 15 percent. To give some context, relatively large difference (30 percentage points) is equal to the observed difference between states in the top versus bottom tercile in terms of the change in the fee index between 1998 and 2008. To put that gap in another context, it is somewhat smaller than the temporary increase in Medicaid physician fees for primary care physician services called for in PPACA.
Figure 3.

Estimated Effects on Utilization of an Increase versus Decrease in the Medicaid Physician Primary Care Fee Index (all children, and separately by socioeconomic status quartile)Notes. The bar heights represent the estimated effects of a large increase (plus 15 percent) versus a large decrease (minus 15 percent) in the Medicaid physician fee index for primary care services (i.e., a difference of 30 percentage points) estimated using reduced form models. Children are assigned to a socioeconomic status quartile on the basis of their family income and parents' educational status (see Appendix SA1 for details). The drop bars indicate ±1 standard error. The results represent enrollment differences in percentage points. *p < .10, **p < .05, ***p < .01
Compared with the size of a state's CHIP expansion, increasing Medicaid physician fees is more clearly associated with improvements in access, both among low- and high-SES children. Based on the point estimates, increasing Medicaid fees is associated with increases in the number of physician visits per year among children in all SES groups, although none of those estimates is statistically significant. Increasing Medicaid fees is associated with a statistically significant increase in the likelihood that children in SES quartile 2 saw a pediatrician in the last year. Increasing Medicaid fees is also clearly related to a reduction in non-cost-related access problems among both among low- and high-income children.
Conclusions
The key conclusions are the following:
From the patient's perspective, CHIP reduced the level of cost sharing that low- and middle-income children faced. However, we do not observe a corresponding increase in aggregate physician utilization. This implies that supply-side effects of CHIP—either the use of managed care tools or the relatively low reimbursement rates, or both—may have limited the utilization effect of the coverage expansion.
Among low-income children, increasing Medicaid fees appears to improve access to care. Increasing Medicaid fees also appears to have positive spillover effects on physician utilization among higher-income children.
In general, these findings argue strongly against the idea that the effect of expanding coverage on utilization can be deduced simply from the reduction in patient cost sharing. The nature of the coverage—for example, does the coverage consist of a tightly managed product? does the coverage pay providers generously?—appears to be critical.
From a federal budgetary perspective, these results are good news—if we extrapolate from the results in this article, the expansions of public coverage called for in PPACA will not have any effect on aggregate utilization of physician services. From the enrollee's perspective, the results are mixed—the benefits of expanded public coverage may lie primarily in improved financial protection, rather than a sheer increase in services received. These findings also support the idea that public health insurance plans can have spillover effects on children who do not themselves gain coverage, and that those spillover effects can either increase utilization (if the public plan's reimbursement environment is made more generous) or reduce utilization (if coverage is expanded without making reimbursement more generous).
As it is conventionally understood, our policy options are either to expand coverage and increase health spending or to leave coverage gaps and hold the line on spending. That dilemma is false. Coverage expansions by themselves do not necessarily spur increases or decreases in overall utilization—what does appear to matter is the nature of the coverage and the generosity of provider reimbursements in the public program. The policy questions that we should be focusing on are as follows: (1) the degree to which we want the rationing of medical services to occur based on out-of-pocket costs and the ability to pay versus nonprice factors such as queuing, and (2) the degree to which we want our financing of the health care system to be redistributive. Expanding public coverage clearly moves in the direction of redistributive financing. Depending on how we choose to set reimbursement levels in our public programs, expansion coverage may or may not move in the direction of increased utilization and increased system spending.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported by the Robert Wood Johnson Foundation. The author thanks Paul Ginsburg for his guidance, Cynthia Saiontz-Martinez for her expert programming, Deborah Rose for her assistance accessing the data, and Marisa Dowling for her help preparing the manuscript. The views presented here are those of the author and do not represent the Center for Studying Health System Change.
Disclosure: None.
Disclaimer: None.
Notes
Non-cost-related access problems are summarized using a binary variable that equals 1 if the parent reports that they have delay in getting care for their child in the last 12 months because of any of the following reasons: (1) “You couldn't get through on the telephone,” (2) “You couldn't get an appointment for [your child] soon enough,” (3) “Once you get there, [your child] has to wait too long to see the doctor,” or (4) “The clinic/doctor's office wasn't open when you could get there.”
The CMS Office of the Actuary (OACT), when producing their official estimates of the effects of health reform, relied in part on a 1993 report by the Congressional Budget Office (http://www.cbo.gov/ftpdocs/105xx/doc10585/1993_11_bevavior.pdf). That CBO report draws heavily on the RAND HIE. The OACT analyses are available at https://www.cms.gov/ActuarialStudies/Downloads/HR3200_2009-10-21.pdf and http://www.cms.hhs.gov/ActuarialStudies/Downloads/S_PPACA_2010-01-08.pdf.
Based on the author's calculations using the 2009 National Health Interview Survey (NHIS), the share of children whose parents report a gatekeeper arrangement was 47 percent among privately insured children and 78 percent among children enrolled in CHIP. (Gatekeeping was identified by those responding yes to the following NHIS item: “If [you need/he needs/she needs] to go to a different doctor or place for special care, [do you/does he/does she] need approval or a referral? Do not include emergency care.”) The share of children whose parents report that they are free to see any doctor who accepts the plan was 48 percent among privately insured children versus 25 percent among children enrolled in CHIP.
Gruber and Rodriguez (2007) use a detailed visit-level data on physician billing and payments to compare physician revenues for services provided to uninsured patients with revenues for otherwise identical services provided to insured patients. They report that three quarters of physicians receive lower fees for serving Medicaid patients than for serving the uninsured, and that for almost 60 percent of physicians, the Medicaid fees are less than two-thirds the fees paid by the uninsured. Unfortunately, that type of comparison is not available specifically for pediatrician services provided to children enrolled in CHIP.
We performed two tests to examine whether the Medicaid fee index we use is a fairly broad indicator of physician payment generosity in Medicaid and CHIP plans. First, for the most recent year possible (2008), we compared our Medicaid fee index with a comparable measure of physician fees used by Ingenix in an actuarial model of the cost of children's health coverage. The Ingenix fees include both Medicaid and CHIP plans, and they are based on “a mixture of managed and unmanaged FFS claim experience” (Ingenix Consulting 2009b). We found that the population-weighted correlation between the Ingenix fees and our fee index was very high (r = 0.8587). Second, we measured the percent change in the two fee indices using the available years (from 2003 to 2008 for our Medicaid fee index, and from 2002 to 2008 for the Ingenix fee index). The correlation in state-level changes is positive (r = 0.0880), although not nearly as strong as the correlation in levels. (Unfortunately, the Ingenix measure of fees is not available for any years prior to the implementation of CHIP, which prevents us from incorporating it directly into our analyses.)
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Technical Appendix to “A Comparison of Two Approaches to Increasing Access to Care: Expanding Coverage versus Increasing Physician Fees”.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Adams K. The Effect of Increased Medicaid Fees on Physician Participation and Enrollee Service Utilization in Tennessee. Inquiry. 31:173–89. [PubMed] [Google Scholar]
- Banthin JS, Selden TM. The ABCs of Children's Health Care: How the Medicaid Expansions Affected Access, Burdens, and Coverage between 1987 and 1996. Inquiry. 40(2):133–45. doi: 10.5034/inquiryjrnl_40.2.133. [DOI] [PubMed] [Google Scholar]
- Buchmueller TC, Grumbach K, Kronick R, Kahn JG. The Effect of Health Insurance on Medical Care Utilization and Implications for Insurance Expansion: A Review of the Literature. Medical Care Research and Review. 1994;62(1):3–30. doi: 10.1177/1077558704271718. [DOI] [PubMed] [Google Scholar]
- Congressional Budget Office. H.R. 3590, Patient Protection and Affordable Care Act, Cost Estimate for the Bill as Passed by the Senate on December 24, 2009 [accessed March 10, 2010]. Available at http://www.cbo.gov/ftpdocs/113xx/doc11307/Reid_Letter_HR3590.pdf.
- Currie J, Gruber J. Health Insurance Eligibility, Utilization of Medical Care, and Child Health. Quarterly Journal of Economics. 1996;111(2):431–66. [Google Scholar]
- Dafny L, Gruber J. Public Insurance and Child Hospitalizations: Access and Efficiency Effects. Journal of Public Economics. 2005;89(1):109–29. [Google Scholar]
- Decker SL. Changes in Medicaid Physician Fees and Patterns of Ambulatory Care. Inquiry. 2010;46(3):291–304. doi: 10.5034/inquiryjrnl_46.03.291. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Lee CH. Income, Poverty, and Health Insurance Coverage in the United States: 2005 U.S. Census Bureau, P60-231. [accessed January 25, 2010]. Available at https://www.census.gov/prod/2006pubs/p60-231.pdf.
- DeNavas-Walt C, Proctor BD, Smith JC. 2010. Income, Poverty, and Health Insurance Coverage in the United States: 2009 P60-238. [accessed October 14, 2010]. Available at http://www.census.gov/prod/2010pubs/p60-238.pdf.
- Enterline P. The Distribution of Medical Services before and after ‘Free' Medical Care—The Quebec Experience. New England Journal of Medicine. 1973;289:1174–8. doi: 10.1056/NEJM197311292892206. [DOI] [PubMed] [Google Scholar]
- Finkelstein A. The Aggregate Effects of Health Insurance: Evidence from the Introduction of Medicare. Quarterly Journal of Economics. 2009;122(1):1–37. [Google Scholar]
- Gruber J, Rodriguez D. How Much Uncompensated Care Do Doctors Provide? No. 13585. Available at http://papers.nber.org/papers/w13585. [DOI] [PubMed]
- Ingenix Consulting. 2009a. 2009 AAP Pediatric Medical Cost Model [accessed January 29, 2010]. Available at http://www.aap.org/research/PediatricMedicalCostModel.xls.
- Ingenix Consulting. 2009b. 2009 Pediatric Medical Cost Model, Methodology [accessed January 29, 2010]. Available at http://www.aap.org/research/Methodology.pdf.
- Long SH, Marquis MS. The Uninsured ‘Access Gap’ and the Cost of Universal Coverage. Health Affairs. 1994;13(2):211–20. doi: 10.1377/hlthaff.13.2.211. [DOI] [PubMed] [Google Scholar]
- Lurie IZ. Differential Effect of the State Children's Health Insurance Program Expansions by Children's Age. Health Services Research. 2007;44(5, Part 1):1504–20. doi: 10.1111/j.1475-6773.2009.01005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicaid and CHIP Payment and Access Commission. MACPAC March 2011 Report to the Congress on Medicaid and CHIP [accessed March 16, 2011]. Available at http://www.macpac.gov/reports/MACPAC_March2011_web.pdf.
- Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. Health Insurance and Access to Primary Care for Children. New England Journal of Medicine. 1998;338(8):513–9. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- Newhouse JP, The Insurance Experiment Group . Free for All? Lessons from the RAND Health Insurance Experiment. Cambridge, MA: Harvard University Press; 2011. [Google Scholar]
- Office of the Actuary. Estimated Financial Effects of the ‘America’s Affordable Health Choices Act of 2009' (H.R. 3200), as Reported by the Ways and Means Committee [accessed October 21, 2009]. Available at https://www.cms.gov/ActuarialStudies/Downloads/HR3200_2009-10-21.pdf.
- Office of the Actuary. 2010. Estimated Financial Effects of the ‘Patient Protection and Affordable Care Act,’ as Amended Centers for Medicare and Medicaid Services [accessed April 26, 2010]. Available at https://www.cms.gov/ActuarialStudies/Downloads/PPACA_2010-04-22.pdf.
- Selden TM, Hudson JL. Access to Care and Utilization among Children: Estimating the Effects of Public and Private Coverage. Medical Care. 2006;44(5 suppl):I19–26. doi: 10.1097/01.mlr.0000208137.46917.3b. [DOI] [PubMed] [Google Scholar]
- Shen Y-C, Zuckerman S. The Effect of Medicaid Payment Generosity on Access and Use among Beneficiaries. Health Services Research. 2009;40(3):723–44. doi: 10.1111/j.1475-6773.2005.00382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart WH, Enterline PE. Effects of the National Health Service on Physician Utilization and Health in England and Wales. New England Journal of Medicine. 1961;265:1187–94. doi: 10.1056/NEJM196112142652405. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


