Abstract
Background
To examine ethnic differences in cardiometabolic risk profile in early age, and explore whether such differences can be explained by differences in body mass index (BMI) or waist circumference (WC).
Method
Anthropometric measurements, blood pressure and (in a subsample) fasting blood were collected during a health check of 2,509 children aged 5–6 years. Four ethnic groups were distinguished: Dutch (n = 2,008; blood n = 1,300), African descent (n = 199; blood n = 105), Turkish (n = 108; blood n = 57) and Moroccan (n = 194; blood n = 94). Ethnic differences in diastolic and systolic blood pressure (DBP/SBP), fasting glucose, low-density lipoprotein (LDL), high-density lipoprotein (HDL) and triglyceride levels were determined and the explanatory role of BMI and WC was examined with regression analysis.
Results
After adjustment for confounders, African descent children showed higher DBP (β2.22 mmHg; 95%CI:1.09–3.36) and HDL levels (β:0.09 mmol/l; 95%CI:0.03–0.16) compared to Dutch children (reference group). Turkish children showed higher SBP (β:1.89 mmHg; 95%CI:0.25–3.54), DBP (β:2.62 mmHg; 95%CI:1.11–4.13), glucose (β:0.12 mmol/L; 95%CI:0.00–0.25) and triglyceride levels (β:0.13 mmol/L; 95%CI:0.02–0.25). Higher BMI values were found in all non–Dutch groups (differences ranged from 0.53–1.03 kg/m2) and higher WC in Turkish (β:1.68 cm; 95%CI:0.99–2.38) and Moroccan (β:1.65 cm; 95%CI:1.11–2.19) children. BMI and WC partly explained the higher SBP/DBP and triglyceride levels in Turkish children.
Conclusion
Ethnic differences in cardiometabolic profile exist early in life and are partly explained by differences in BMI and WC. African children showed favourable HDL levels and Turkish children the most unfavourable overall profile, whereas their Moroccan peers have less increased cardiometabolic risk in spite of their high BMI and WC.
Introduction
Results of studies examining ethnic differences in risk of cardiovascular disease (CVD) and diabetes type 2 (DM2) are varied and sometimes conflicting. Overall, in Western countries (e.g. the USA/UK), cardiovascular mortality seems to be generally higher among ethnic minority groups compared to the host population [1]–[4]. The Netherlands is no exception to this; although the cardiovascular mortality among Moroccan tends to be lower [5]–[7]. Looking at the individual components of the cardiometabolic risk factors, African people, for example, tend to have healthier (higher) high-density lipoprotein (HDL) and lower triglyceride levels, but are more likely to be hypertensive than whites [8], [9]. The prevalence of hypercholesterolemia is lower among Turkish and Moroccan adults living in the Netherlands [7], [10]. However, part of this advantage is off-set by their relatively low HDL cholesterol, resulting in an unfavourable total/HDL cholesterol ratio, particularly in the Turkish population [7]. Paradoxically, the risk of developing DM2 and obesity is reported to be higher among all ethnic minority groups [6], [10]–[12].
Overweight is seen as an important trigger for developing DM2, hyperlipidaemia and hypertension [13]–[16]. Because overweight is more common in some ethnic minority groups, this might explain the ethnic differences in cardiometabolic risk profile.
Early-life exposures have been implicated in the aetiology of CVD, and the presence of cardiometabolic risk factors during childhood persist into adulthood [17]–[19]. Therefore, knowledge on early emergence of ethnic differences in cardiometabolic risk factors is important. Studies on this subject among several minority groups reported that these differences in childhood and adolescence generally follow adult patterns [20]–[24]. However, in most of these studies the children were aged ≥8 years or were adolescents (14–16 years). To our knowledge only one study, investigating an overweight and obese cohort (3–18 years), reported higher prevalence of cardiometabolic risk factors (e.g. low HDL-cholesterol, high triglycerides and impaired glucose tolerance) among overweight Turkish children compared to their Dutch and Moroccan overweight peers [25]. Data on healthy population-based measures in these particular groups are missing.
To gain additional knowledge, the present study was designed to examine ethnic differences in cardiometabolic risk profile in healthy children aged 5–6 years of Dutch, African descent,Turkish and Moroccan origin; the main ethnic groups living in the Netherlands. Furthermore, we determined to what extent body mass index (BMI; as a measure of total body fat) and waist circumference (WC; as a measure of abdominal fat) affect any observed differences. Since African descent children and particularly children from Turkish and Moroccan origin are consistently found to have high prevalence rates of overweight [26]–[29], and adiposity measures are correlated with cardiometabolic risk [30], [31], we hypothesized that BMI and WC would (partly) explain the ethnic difference in cardiometabolic risk profile.
Methods
Ethics Statement
The present study is part of the Amsterdam Born Children and their Development (ABCD) study. The main goal of this study is to examine and determine factors in early life (during pregnancy and infancy) that might explain the later health of the child with specific attention paid to ethnic inequalities. Approval was obtained from the Academic Medical Center Medical Ethical Committee, the VU University Medical Center Medical Committee and the Registration Committee of Amsterdam. All participating mothers gave written informed consent for themselves and their children.
Subjects
The design and rationale of the ABCD study have been described previously [32]. In brief, between January 2003 and March 2004 8,266 pregnant women were included in the study after their first antenatal visit to an obstetric caregiver (phase 1). They filled out an extensive pregnancy questionnaire about socio-demographic data, obstetric history, lifestyle, dietary habits, and psychosocial conditions. Of these respondents, 7,863 women gave birth to a viable singleton infant and 6,575 women gave permission to collect information obtained from the Youth Health Care (phase 2). Phase 3 of the study started in the summer of 2008. Around two weeks after their ABCD-child’s fifth birthday, 6,161 mothers who initially gave permission for follow-up (93.7% of 6,575) were sent a questionnaire (in Dutch, English or Turkish) in which they were also asked for permission on participation of their child in the physical examination and blood collection. Reasons for lack of follow-up included withdrawal from the study, infant or maternal death, and loss to follow-up due to unknown address or emigration. The questionnaire, returned by 4,488 mothers, provided information on their child’s health, development and behaviour. Various physical measurements, including height, bodyweight, WC and blood pressure (BP), took place in 3,321 children (taking about 1 h per child). In a subsample of 2,003 (60.3% of 3,321) children, whose parents gave additional permission apart from the physical examination, fasting blood was also collected (fasting plasma glucose (mmol/L), low-density lipoprotein (LDL; mmol/L), HDL (mmol/L), and triglyceride (mmol/L).
The present study includes 2,509 singleton children (aged 5–6 years) from the main ethnic groups living in the Netherlands (Dutch, African descent, Turkish and Moroccan origin), for which the 5-year questionnaire and the physical examination, was completed. Of these children 1,556 (62.0% of 2,509) had known fasting blood values (fasting glucose, and various lipid levels). Ethnicity of the child was based on the country of birth of the child’s mother and her mother (self reported) in order to include children from both first-generation (born outside the Netherlands) and second-generation (born in the Netherlands, but with a grandmother born in another country) mothers. Because they have a similar ethnic background (all originally from sub-Saharan Africa) [5], children from Surinam (Surinam-Creole), the Antilles, Ghana and other Sub-Saharan African origin were combined in the ‘African descent’ group.
The ethnic groups were composed as follows: Dutch (n = 2,008; for blood values n = 1,300) African descent (n = 199; for blood values n = 105), Turkish (n = 108; for blood values n = 57) and Moroccan (n = 194; for blood values n = 94). Children from ethnic groups other than those mentioned above (n = 812; for blood values n = 447) were excluded, because their numbers would be too small to analyze separately.
Comparison of the included 1,556 participants with measured fasting blood with the 953 (2,509–1,556) participants without fasting blood measurement, showed a higher proportion of Dutch ethnicity (83.5% vs. 74.3%; p<0.001) and lower systolic BP (SBP; 97.4 vs. 98.6 mmHg; p = 0.001) and diastolic BP (DBP; 57.4 vs. 58.8 mmHg; p<0.001) but no difference on mean BMI and WC.
Measurements
The outcome variables measured were: BP expressed in mmHg (SBP and DBP), fasting plasma glucose (mmol/L), LDL (mmol/L), HDL (mmol/L), and triglyceride (mmol/L). For BP, first a test measure was made (to comfort/relax) the child followed by a 10-min rest period. The device used was the Omron 705 IT (Omron Healthcare Inc, Bannockburn, IL, USA) with its appropriate cuff size (arm circumference 17–22 cm). Then, BP was measured twice on the right arm in sitting position, with the arm supported at heart level. These two measurements were considered valid if they did not differ by more than 10 mmHg, otherwise BP was measured a third time. SBP and DBP (mmHg) were calculated by taking the mean value of the two valid measures. Capillary blood was taken in the morning between 7:45 and 8:30 by finger prick collected in a validated kit developed for ambulatory purposes (LabAnywhere, Haarlem, the Netherlands) [33].
For the present study the variables of body composition were: BMI (kg/m2) and WC (cm). To calculate BMI, height was measured to the nearest millimeter using a Leicester portable height measure (Seca), and weight to the nearest 100 gram using a Marsden weighing scale, (model MS-4102). WC was measured midway between the costal border and the iliac crest to the nearest millimeter using a Seca measuring tape. Overweight/obesity was defined by the age- and sex specific International Obesity Task Force (IOTF) guidelines [34].
Data Analysis
Demographic ethnic differences between anthropometrics and cardiometabolic risk factors were examined with χ2-tests (categorical data) or ANOVA (continuous data). Linear regression was used to examine ethnic differences in SBP and DBP, glucose, LDL, HDL and triglyceride levels, and the role of BMI and WC in explaining these differences. In order to be able to research the explanatory role of BMI and WC for ethnic differences in blood pressure, glucose and cholesterol levels these variables should be associated with these outcome variables in general. Therefore first, the associations of BMI and WC with these cardiometabolic risk factors were assessed with linear regression after adjustment for age, sex, and ethnicity. Because SBP, DBP and WC are associated with height, all models including these variables were additionally adjusted for child’s height. Second, to detect any ethnic differences in BMI, WC, SBP, DBP, glucose, LDL, HDL and triglyceride levels analysis were performed with adjustment for age, sex and, where appropriate, additionally for height (model 1). Third, for only those cardiometabolic risk factors in which ethnic differences were present in model 1 (Dutch = reference group), as well as having an association with BMI or WC in general, the explanatory role of BMI or WC was assessed in two separate models by adding BMI or WC (including height) to model 1.
To provide an adequate fit, all models were tested for possible non-linearity. Interactions between BMI and WC with ethnicity were tested to reveal possible ethnic-specific associations. Restricted cubic splines (RCS) were used in the regression analysis to examine and characterize an association that is suspected to be non-linear by using higher order piecewise polynomials to accommodate potential changes in the direction of the association across the exposure distribution [35]. If the results for a given model indicated that a linear model provided an adequate fit (likelihood ratio test: p-value >0.05), we report the results from a linear model.
Because fasting triglyceride concentrations were positively skewed, we used log values in regression analyses; the distributions and the residuals in the regression models became normal with these transformations.
Statistical analyses were conducted using R 2.12.1. A p-value <0.05 was regarded as statistically significant.
Results
Table 1 presents the characteristics of the children at age 5–6 years, stratified for ethnicity. Dutch children were on average younger (p = 0.01), but there were no differences between the ethnic groups with respect to percentage boys and girls. The percentage overweight/obese was highest among Turkish (27.0%) and Moroccan (26.2%) children (Dutch 6.6%). Ethnic differences in metabolic parameters, adjusted for age and sex are described below.
Table 1. Characteristics of the study sample stratified for ethnicity.
| Dutch n = 2008 (n = 1300 for blood) | African descent n = 199 (n = 105 for blood) | Turkish n = 108 (n = 57 for blood) | Moroccan n = 194 (n = 94 for blood) | |
| Mean (SD) or % | ||||
| Age (years) | 5.7 (0.5) | 5.9 (0.5) | 5.9 (0.5) | 6.1 (0.6) |
| Sex % boys | 50.8 | 47.1 | 52.0 | 56.7 |
| Height (cm) | 116.9 (5.7) | 119.1 (6.0) | 116.7 (5.3) | 118.1 (6.4) |
| Weight (kg) | 21.0 (2.9) | 22.8 (4.3) | 22.5 (3.8) | 23.1 (4.3) |
| BMI (kg/m2) | 15.4 (1.3) | 16.0 (2.0) | 16.5 (2.0) | 16.5 (1.9) |
| Waist circumference (cm) | 52.3 (3.3) | 53.2 (4.8) | 54.4 (4.7) | 54.5 (4.7) |
| Overweight/obese % | 6.6 | 17.8 | 27.0 | 26.2 |
| Systolic BP (mmHg) | 97.5 (8.5) | 99.0 (8.9) | 99.5 (8.8) | 99.8 (9.3) |
| Diastolic BP (mmHg) | 57.4 (7.8) | 60.4 (7.4) | 60.4 (8.5) | 59.5 (7.6) |
| Glucose (mmol/L) | 4.6 (0.5) | 4.5 (0.5) | 4.7 (0.4) | 4.6 (0.5) |
| LDL cholesterol (mmol/L) | 2.3 (0.6) | 2.4 (0.7) | 2.4 (0.6) | 2.3 (0.6) |
| HDL cholesterol (mmol/L) | 1.30 (0.31) | 1.40 (0.34) | 1.35 (0.26) | 1.30 (0.26) |
| Triglyceride (mmol/L) | 0.64 (0.30) | 0.64 (0.33) | 0.75 (0.45) | 0.64 (0.26) |
Association between Body Composition and Cardiometabolic Risk Factors
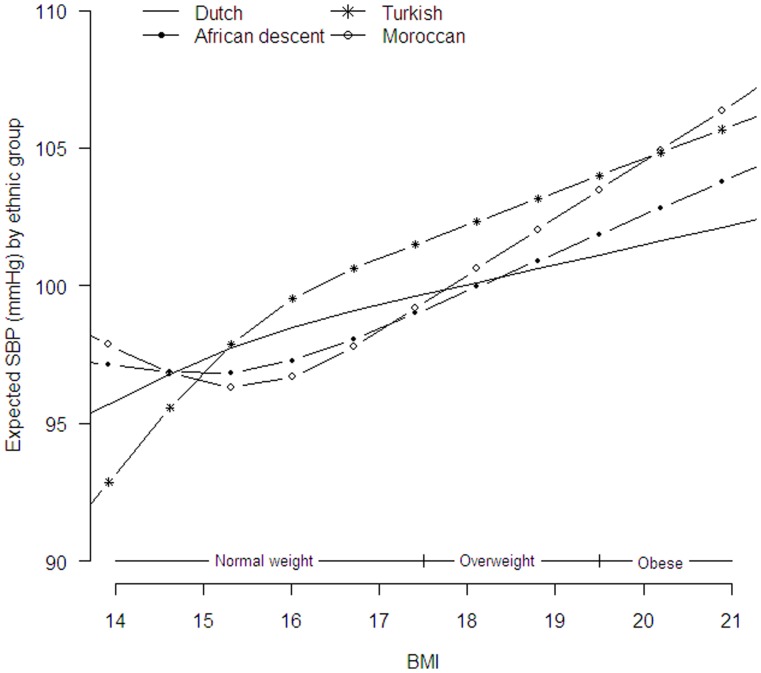
Table 2 presents overall associations between the cardiometabolic risk factors and BMI or WC adjusted for age, sex, height (for SBP, DBP and WC) and ethnicity. BMI was non-linear and showed an ethnic-specific association with SBP (likelihood ratio test p = 0.02; Figure 1). Figure 1 showed a steeper increase in SBP with increasing BMI in Turkish (across the whole BMI range) and Moroccan (in the mid normal and overweight BMI range) children compared to the ethnic Dutch children. BMI was linear, not ethnic-specific associated with DBP and glucose; one unit increase in BMI (kg/m2) resulted in 1.24 mmHg increase in DBP (95%CI: 0.88, 1.60) and a small increase of 0.05 mmol/L in glucose levels (95%CI: 0.02, 0.08; Table 2). No associations were found between BMI and LDL, HDL and triglyceride.
Table 2. Associations of body mass index (BMI) and waist circumference (WC) with cardiometabolic risk factors.
| Systolic BP (mmHg) | Diastolic BP (mmHg) | Glucose (mmol/L) | LDL cholesterol (mmol/L) | HDL cholestrol (mmol/L) | (log)triglyceride (mmol/L) | |
| BMI (kg/m2) | 2.01 (1.50,2.52) * † | 1.24 (0.88, 1.60) | 0.05 (0.02, 0.08) | 0.01 (−0.02, 0.05) | 0.00 (−0.02, 0.02) | 0.01 (−0.01, 0.04) |
| WC (cm) | 1.48 (1.04, 1.92) | 1.02 (0.61, 1.42) | 0.02 (−0.01, 0.05) | 0.04 (0.00, 0.09) | −0.02 (−0.04, 0.00) | 0.05 (0.02, 0.08) |
Beta’s are adjusted for age, sex and ethnicity; models including SBP, DBP or WC are additionally adjusted for height.
Bold indicates significant different from reference group;
Non-linear association: estimated betas for mean BMI (15.3 kg/m2).
Figure 1. Estimated expected SBP (mmHg) per ethnic group, as a function of the child’s BMI.
Overweight status cut off scores based on boys with mean age 5.5 years [34].
All associations with WC were linear and similar for all ethnic groups (likelihood ratio test p<0.10). One unit increase in WC (cm) was associated with an increase of 1.48 mmHg in SBP (95%CI: 1.04, 1.92), and 1.02 mmHg in DBP (95%CI: 0.61, 1.42; Table 2). Furthermore, one unit increase in WC was also associated with a small increase of 0.04 mmol/L in LDL (95%CI: 0.00, 0.09) and 0.05 mmol/L in triglyceride levels (95%CI: 0.02, 0.08). No association was found between WC, glucose and HDL.
The correlation between BMI and WC was found to be strong (r = 0.77; p-value <0.001).
Ethnic Differences in Cardiometabolic Risk Profile
Table 3 presents data on ethnic differences in cardiometabolic risk factors after adjustment for age and sex. Compared with the ethnic Dutch children (reference group), African descent children showed a higher BMI (β: 0.53 kg/m2; 95%CI: 0.32–0.74), DBP (β: 2.22 mmHg; 95%CI: 1.09–3.36) and HDL levels (β: 0.09 mmol/L; 95%CI: 0.03–0.16). The Turkish children showed a higher BMI (β: 1.02 kg/m2; 95%CI: 0.75–1.30), WC (β: 1.68 cm; 95%CI: 0.99–2.38), SBP (β: 1.89 mmHg; 95%CI: 0.25–3.54), DBP (β: 2.62 mmHg; 95%CI: 1.11–4.13), glucose levels (β: 0.12 mmol/L; 95%CI: 0.00–0.25) and triglyceride levels (β: 0.13 mmol/L; 95%CI: 0.02–0.25). The Moroccan children showed only higher BMI (β: 1.03 km/m2; 95%CI: 0.81–1.24) and WC (β: 1.65 cm; 95%CI: 1.11–2.19) compared to the ethnic Dutch children.
Table 3. Ethnic differences in cardiometabolic risk factors (ethnic Dutch = reference group) and the effect of additional adjustment for body mass index (BMI) or waist circumference (WC).
| African descent | Turkish | Moroccan | |||
| Adjusted? | Difference (95%CI) | ||||
| BMI (kg/m2) | Model 1 | 0.53 (0.32, 0.74) * | 1.02 (0.75, 1.30) | 1.03 (0.81, 1.24) | |
| Waist circumference (cm) | Model 1 | 0.47 (−0.06, 1.00) | 1.68 (0.99, 2.38) | 1.65 (1.11, 2.19) | |
| Systolic BP (mmHg) | Model 1 | 0.34 (−0.89, 1.57) | 1.89 (0.25, 3.54) | 0.98 (−0.28, 2.23) | |
| BMI† | –$ | 0.17 (−1.81, 2.15) | – | ||
| WC | – | 1.11 (−0.53, 2.76) | – | ||
| Diastolic BP (mmHg) | Model 1 | 2.22 (1.09, 3.36) | 2.62 (1.11, 4.13) | 1.13 (−0.04, 2.29) | |
| BMI | 1.83 (0.70, 2.96) | 1.76 (0.24, 3. 28) | – | ||
| WC | 2.14 (1.01, 3.27) | 2.09 (0.57, 3.61) | – | ||
| Glucose (mmol/L) | Model 1 | −0.03 (−0.13, 0.06) | 0.12 (0.00, 0.25) | 0.01 (−0.09, 0.12) | |
| BMI | – | 0.10 (−0.03, 0.23) | – | ||
| WC | – | – | – | ||
| LDL cholesterol (mmol/L) | Model 1 | 0.04 (−0.08, 0.17) | 0.09 (−0.08, 0.25) | −0.03 (−0.18, 0.09) | |
| BMI | – | – | – | ||
| WC | – | – | – | ||
| HDL cholesterol (mmol/L) | Model 1 | 0.09 (0.03, 0.16) | 0.04 (−0.04, 0.12) | −0.02 (−0.09, 0.04) | |
| BMI | – | – | – | ||
| WC | – | ||||
| (log)triglyceride (mmol/L) | Model 1 | −0,02 (−0.11, 0.06) | 0.13 (0.02, 0.25) | 0.01 (−0.08, 0.10) | |
| BMI | – | – | – | ||
| WC | – | 0.06 (−0.01, 0.22) | – | ||
Model 1: Adjusted for age and sex; models including SBP, DBP or WC are additionally adjusted for height.
Bold indicates significant different from reference group;
Non-linear association: estimated beta for mean BMI (15.3 kg/m2);
- No ethnic differences present in model 1 and/or association with BMI/WC (Table 2).
Explanatory Role of Body Composition for Ethnic Differences in Cardiometabolic Risk Profile
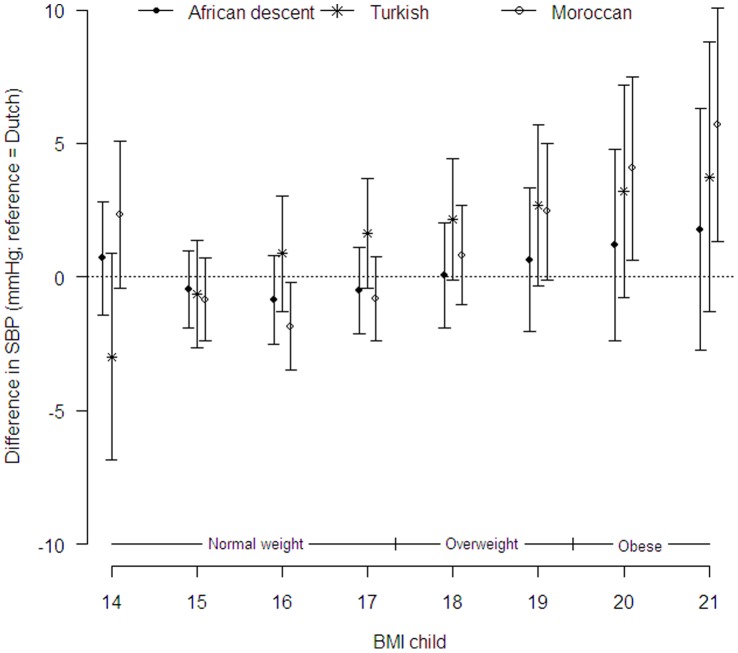
Adjustment for BMI had little effect on the size of glucose and blood lipid differences in all ethnic groups (Table 3). There was a strong effect of BMI on DBP (linear, not ethnic specific) and SBP (non-linear, ethnic specific (likelihood ratio test p = 0.02)). Figure 2 shows that the differences in SBP for the Turkish children are attenuated after adjustment for BMI. The differences in SBP in Turkish children became non-significant across the whole BMI range. Although no mean differences in SBP were found in the Moroccan children in model 1 (table 3), after adjustment for BMI obese Moroccan children showed higher SBP compared to the Dutch children (figure 2). The difference in DBP in African descent and Turkish children became smaller after adjustment for BMI. However, DBP remained 1.83 mmHg (95%CI: 0.709–2.96) higher in African descent and 1.76 mmHg (95%CI: 0.24–3.28) higher in Turkish children compared to the Dutch children.
Figure 2. Difference in SBP (mmHg) per ethnic group (Dutch = reference group), as a function of the child’s BMI.
Overweight status cut off scores based on boys with mean age 5.5 years [34].
Adjustment for WC showed results comparable to BMI, although WC explained the ethnic differences to a lesser degree, except for the triglyceride levels in Turkish children. After additional adjustment for WC, the higher triglyceride levels in Turkish children attenuated. Because Moroccan children did not differ in blood pressure, glucose, LDL, HDL and triglyceride level from the ethnic Dutch children in model 1, the explanatory role of BMI and WC was not tested (Table 3).
Discussion
This study examined ethnic differences in cardiometabolic risk profile, and the explanatory role of BMI and WC in a healthy population of Dutch, African descent, Turkish and Moroccan 5–6 year olds. We found that ethnic differences in cardiometabolic risk profile do exist at young age. All non-Dutch groups showed higher BMI and WC values compared to the Dutch children, except for WC in the African children. After adjustment for confounders (age, sex and height), African descent children showed higher DBP levels and more favourable HDL levels, and Turkish children higher SBP and DBP and somewhat higher glucose and triglyceride levels. On the other hand, the Moroccan children (except for the higher BMI and WC) showed hardly any differences in cardiometabolic risk profile. BMI and WC partly explained the ethnic difference in BP, glucose and triglyceride levels, but ethnic differences remained for DBP (African descent and Turkish).
Ethnic differences in cardiometabolic risk profile have been reported in both adults and children [9], [20], [22], [24], [25], [36], [37], with lower rates of CVD in Africans (especially men) and Moroccans and higher rates among Turkish groups compared to the host population. A Dutch study among overweight/obese Turkish and Moroccan children showed significantly higher rates of cardiometabolic risk in Turkish children relative to their Moroccan and ethnic Dutch peers [25]. The present data support the notion that Turkish children have a more adverse cardiometabolic risk profile compared to Moroccan and ethnic Dutch children. Children in Turkish cohorts appear to have high mean glucose and triglyceride levels, but also high HDL-cholesterol. Probably immigration of Turkish children to the Netherlands has an additional adverse effect on cardiometabolic risk profile [38].
Adiposity is seen as an important factor in explaining cardiometabolic outcomes [15], [39] and we found higher rates of overweight in all ethnic minority groups. Unexpectedly, the associations between BMI and WC, and the different blood measures, were weak or even absent. There is evidence that, at least in adults, visceral fat promotes systemic inflammation by secreting inflammatory acute phase proteins, resulting in a higher risk of developing metabolic diseases, especially diabetes [40], [41]. Possibly, this mechanism may not be present at such a young age [42], or the variations in BMI, WC or the blood chemistry values were too small. In addition, BMI and WC were highly correlated (r = 0.77) which might explain why data didn’t show much differences in the association between BMI and WC with the other cardiometabolic risk factors. This suggests that the distinctiveness between overall and abdominal fat is low in young children.
After adjustment for BMI and WC the DBP of Turkish and African descent children remained higher. Furthermore, Turkish and Moroccan infants showed a steeper increase in SBP with increasing BMI resulting in a higher SBP in obese Moroccan children. This implies that other mechanisms also influence blood pressure in these children. Rapid growth velocity during infancy is seen as a risk factor for elevated blood pressure [43]. Previous findings of the ABCD study showed that rapid growth in the first 6 months is more common in infants of Turkish, Moroccan and African origin [44], Ujcic-Voortman et al. reported that Turkish adults have higher C-reactive protein levels [45], a marker of inflammation associated with elevated BMI [46] and increased risk of coronary heart diseases [47]. Although causation is hard to prove, hypothetically, this might have its origin in early life and already influence BP in Turkish children; still, more research is needed to substantiate this hypothesis. In addition, the higher DBP in the African descent children might be related to the renin-angiotensin-aldosteron system and potassium balance [48]. There is evidence that children from African-American origin have a lower urinary excretion rate of potassium, which makes them predisposed to hypertension [48]. This might be due to differences in diet such as high sodium and low potassium intake and hereditary predisposition [48]–[50].
Despite higher BMI levels, African adults and children tend to have a healthier lipid profile. Higher levels of HDL are often found in both adults and children from African descent [9], [20], [24]. For example, the Chase Study of Whincup et al. (which included black African-Caribbean children aged 9–10 years) found higher HDL levels in this group compared to white Europeans (% difference HDL: 1.9; 95% CI: 0.2–3.6) after adjustment for age and sex [24]. Although this might indicate a genetic component, the mechanisms responsible for these differences are not yet elucidated. However, there is evidence that the -514T hepatic lipase allele, which is associated with low hepatic lipase activity and increased HDL concentration, is more common among African people [51].
The higher HDL levels in Africans are often accompanied by lower triglyceride levels [9], [24], [52]. The combination of higher HDL levels and lower triglyceride levels suggest that African people may have a different deposition of fat. Less abdominal fat, frequently described in Africans [52]–[54], is associated with decreased adipose cell basal lipolysis, resulting in higher HDL and lower triglyceride levels [9]. Although our study did not show lower triglyceride levels in the African descent group, these differences may become more visible in adolescent or adult age. Moreover, we need to bear in mind that the ‘African descent’ group is composed of all those from sub-Saharan African origin (including Surinamese-Creole and Antilles) which makes it a heterogeneous group. Although these children have a comparable ethnic background, the cardiometabolic risk profiles may differ between these smaller groups. Nevertheless, sub-analyses indicate no differences between Black Africans (sub-Saharan) and Black Caribbean’s (Surinam-Creole and Antilles) in all outcome variables (results not shown).
It is well known that overweight in childhood tracks into adulthood [55] and there is also evidence that the same accounts for blood pressure and lipid levels [56], [57]. As we shown in this study overweight is highest in Turkish and Moroccan children and has already its consequences in Turkish children. As a result of the high prevalence of overweight in Moroccan children, the currently lower CVD rates in Moroccan adults might converge towards the prevalence rates of ethnic Dutch adults, or beyond when these children become adults. This implies that preventing high levels of overweight and other cardiometabolic risk factors during childhood might decrease risk of CVD later in life.
To our knowledge, this is the first study to examine ethnic differences in cardiometabolic risk profile in a European cohort including population-based Turkish and Moroccan children. When interpreting our results, some limitations should be taken into account. First, only a subsample of children had blood taken. Due to small groups, the lack of significant differences may be due to lack of power. Alternatively, we might have underestimated the ethnic differences in cardiometabolic risk due to selection of the group with fasting blood measures. The children with fasting blood measures had a lower mean BP, which suggests a relative healthier group compared to the children without fasting blood measures. However, no differences were found in mean BMI and WC. Second, previous studies showed sex differences in adiposity measures, BP and lipid levels [54], [58]. Due to small groups we weren’t able to stratify our results by sex. In addition, we found no evidence to stratify by sex; likelihood ratio test did not show any ethnic specific associations with sex for all outcome measures (results not shown). We only adjusted for sex as a confounder. Third, measuring BP in children is more difficult than in adults, e.g. readings are likely to be falsely high in children who find it difficult to relax their arm during the measurement. To control for falsely high or low blood pressures, the BP measurements were performed according to a standardized protocol which included a test measurement before actual measurements were taken [59]. Finally, WC is difficult to measure. Due to lack of a standardized technique to measure WC in children, caution is required when comparing WC between studies. Especially in overweight children, variability in measurement may increase with higher levels of body fat [60]. However, WC as measured in the present study represents the measurement site most closely associated with cardiometabolic risk factors in overweight children [61].
In conclusion, there are ethnic differences in cardiometabolic risk profile at the age of 5–6 years, with favourable HDL levels in African descent children and Turkish children showing the most adverse profile. Moroccan peers have less increased cardiometabolic risk in spite of their high BMI and WC. Although the associations between BMI and WC with the other cardiometabolic risk factors were weak; the ethnic differences in blood pressure, glucose and triglyceride level appeared to be partly accounted for by ethnic differences in adiposity. Future studies should focus on other explanatory factors such as early rapid growth during infancy [43], specific diet components (e.g. sodium and potassium intake) [49] or inflammatory markers [45]. Longitudinal research is needed to determine whether these findings lead to a higher risk of CVD in adult age in the different ethnic groups. Although not all differences are explained by the higher adiposity rates, weight management in children is important to prevent ethnic disparities in cardiometabolic function during childhood and later in life.
Acknowledgments
This work would not have been possible without the input from the participants, primary schools, students and youth health care centers in Amsterdam. We also thank Wim Busschers for his statistical advice.
Funding Statement
This work was supported by the Academic Medical Centre, Amsterdam, the Public Health Services, Amsterdam, and by the Netherlands Organization for Health Research and Development (ZonMw; grant number: 2100.0076), The Hague. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Kurian AK, Cardarelli KM (2007) Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis 17: 143–152. [PubMed] [Google Scholar]
- 2. McKeigue PM, Shah B, Marmot MG (1991) Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 337: 382–386. [DOI] [PubMed] [Google Scholar]
- 3. Smith SC Jr, Clark LT, Cooper RS, Daniels SR, Kumanyika SK, et al. (2005) Discovering the full spectrum of cardiovascular disease: Minority Health Summit 2003: report of the Obesity, Metabolic Syndrome, and Hypertension Writing Group. Circulation 111: e134–e139. [DOI] [PubMed] [Google Scholar]
- 4. Winkleby MA, Robinson TN, Sundquist J, Kraemer HC (1999) Ethnic variation in cardiovascular disease risk factors among children and young adults: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. JAMA 281: 1006–1013. [DOI] [PubMed] [Google Scholar]
- 5. Bos V, Kunst AE, Keij-Deerenberg IM, Garssen J, Mackenbach JP (2004) Ethnic inequalities in age- and cause-specific mortality in The Netherlands. Int J Epidemiol 33: 1112–1119. [DOI] [PubMed] [Google Scholar]
- 6. Dijkshoorn H, Uitenbroek DG, Middelkoop BJ (2003) [Prevalence of diabetes mellitus and cardiovascular disease among immigrants from Turkey and Morocco and the indigenous Dutch population]. Ned Tijdschr Geneeskd 147: 1362–1366. [PubMed] [Google Scholar]
- 7. Ujcic-Voortman JK, Bos G, Baan CA, Uitenbroek DG, Verhoeff AP, et al. (2010) Ethnic differences in total and HDL cholesterol among Turkish, Moroccan and Dutch ethnic groups living in Amsterdam, the Netherlands. BMC Public Health 10: 740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sumner AE (2009) Ethnic differences in triglyceride levels and high-density lipoprotein lead to underdiagnosis of the metabolic syndrome in black children and adults. J Pediatr 155: S7–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zoratti R (1998) A review on ethnic differences in plasma triglycerides and high-density-lipoprotein cholesterol: is the lipid pattern the key factor for the low coronary heart disease rate in people of African origin? Eur J Epidemiol 14: 9–21. [DOI] [PubMed] [Google Scholar]
- 10. El FF, Bruijnzeels MA, Foets MM, Hoes AW (2008) Different distribution of cardiovascular risk factors according to ethnicity: a study in a high risk population. J Immigr Minor Health 10: 559–565. [DOI] [PubMed] [Google Scholar]
- 11. Hoffman RP (2009) Metabolic syndrome racial differences in adolescents. Curr Diabetes Rev 5: 259–265. [DOI] [PubMed] [Google Scholar]
- 12. Uitewaal PJ, Manna DR, Bruijnzeels MA, Hoes AW, Thomas S (2004) Prevalence of type 2 diabetes mellitus, other cardiovascular risk factors, and cardiovascular disease in Turkish and Moroccan immigrants in North West Europe: a systematic review. Prev Med 39: 1068–1076. [DOI] [PubMed] [Google Scholar]
- 13. Allcock DM, Gardner MJ, Sowers JR (2009) Relation between Childhood Obesity and Adult Cardiovascular Risk. Int J Pediatr Endocrinol 2009: 108187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Corvalan C, Uauy R, Stein AD, Kain J, Martorell R (2009) Effect of growth on cardiometabolic status at 4 y of age. Am J Clin Nutr 90: 547–555. [DOI] [PubMed] [Google Scholar]
- 15. Freedman DS, Dietz WH, Srinivasan SR, Berenson GS (1999) The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics 103: 1175–1182. [DOI] [PubMed] [Google Scholar]
- 16. Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS (2001) Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics 108: 712–718. [DOI] [PubMed] [Google Scholar]
- 17. Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, et al. (2005) Racial differences in the tracking of childhood BMI to adulthood. Obes Res 13: 928–935. [DOI] [PubMed] [Google Scholar]
- 18. Morrison JA, Friedman LA, Gray-McGuire C (2007) Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the Princeton Lipid Research Clinics Follow-up Study. Pediatrics 120: 340–345. [DOI] [PubMed] [Google Scholar]
- 19. Morrison JA, Friedman LA, Wang P, Glueck CJ (2008) Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J Pediatr 152: 201–206. [DOI] [PubMed] [Google Scholar]
- 20. Donin AS, Nightingale CM, Owen CG, Rudnicka AR, McNamara MC, et al. (2010) Ethnic differences in blood lipids and dietary intake between UK children of black African, black Caribbean, South Asian, and white European origin: the Child Heart and Health Study in England (CHASE). Am J Clin Nutr 92: 776–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harding S, Maynard M, Cruickshank JK, Gray L (2006) Anthropometry and blood pressure differences in black Caribbean, African, South Asian and white adolescents: the MRC DASH study. J Hypertens 24: 1507–1514. [DOI] [PubMed] [Google Scholar]
- 22. Walker SE, Gurka MJ, Oliver MN, Johns DW, Deboer MD (2010) Racial/ethnic discrepancies in the metabolic syndrome begin in childhood and persist after adjustment for environmental factors. Nutr Metab Cardiovasc Dis 22: 141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Whincup PH, Gilg JA, Papacosta O, Seymour C, Miller GJ, et al. (2002) Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. BMJ 324: 635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Whincup PH, Nightingale CM, Owen CG, Rudnicka AR, Gibb I, et al. (2010) Early emergence of ethnic differences in type 2 diabetes precursors in the UK: the Child Heart and Health Study in England (CHASE Study). PLoS Med 7: e1000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. van Vliet M, von Rosenstiel IA, Schindhelm RK, Brandjes DP, Beijnen JH, et al. (2009) Ethnic differences in cardiometabolic risk profile in an overweight/obese paediatric cohort in the Netherlands: a cross-sectional study. Cardiovasc Diabetol 8: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. de Hoog MLA, van Eijsden M, Stronks K, Gemke RJBJ, Vrijkotte TGM (2011) Overweight at age two years in a multi-ethnic cohort (ABCD study): the role of prenatal factors, birth outcomes and postnatal factors. BMC Public Health 11: 611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fredriks AM, Van Buuren S, Sing RA, Wit JM, Verloove-Vanhorick SP (2005) Alarming prevalences of overweight and obesity for children of Turkish, Moroccan and Dutch origin in The Netherlands according to international standards. Acta Paediatr 94: 496–498. [DOI] [PubMed] [Google Scholar]
- 28. Kolsgaard ML, Andersen LF, Tonstad S, Brunborg C, Wangensteen T, et al. (2008) Ethnic differences in metabolic syndrome among overweight and obese children and adolescents: the Oslo Adiposity Intervention Study. Acta Paediatr 97: 1557–1563. [DOI] [PubMed] [Google Scholar]
- 29. Lynch WC, Heil DP, Wagner E, Havens MD (2007) Ethnic differences in BMI, weight concerns, and eating behaviors: comparison of Native American, White, and Hispanic adolescents. Body Image 4: 179–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hirschler V, Aranda C, Calcagno ML, Maccalini G, Jadzinsky M (2005) Can waist circumference identify children with the metabolic syndrome? Arch Pediatr Adolesc Med 159: 740–744. [DOI] [PubMed] [Google Scholar]
- 31. Lawlor DA, Benfield L, Logue J, Tilling K, Howe LD, et al. (2010) Association between general and central adiposity in childhood, and change in these, with cardiovascular risk factors in adolescence: prospective cohort study. BMJ 341: c6224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van Eijsden M, Vrijkotte TGM, Gemke RJBJ, van der Wal MF (2011) Cohort Profile: The Amsterdam Born Children and their Development (ABCD) Study. Int J Epidemiol 40: 1176–86. [DOI] [PubMed] [Google Scholar]
- 33. Gootjes J, Tel RM, Bergkamp FJ, Gorgels JP (2009) Laboratory evaluation of a novel capillary blood sampling device for measuring eight clinical chemistry parameters and HbA1c. Clin Chim Acta 401: 152–157. [DOI] [PubMed] [Google Scholar]
- 34. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320: 1240–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15: 361–387. [DOI] [PubMed] [Google Scholar]
- 36. Agyemang C, Addo J, Bhopal R, Aikins AG, Stronks K (2009) Cardiovascular disease, diabetes and established risk factors among populations of sub-Saharan African descent in Europe: a literature review. Global Health 5 7: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Leest LATM, van Dis SJ, Verschuren WMM (2002) Hart en vaatziekten bij allochtonen in Nederland. Een cijfermatige verkenning naar leefstijl- en risicofactoren, ziekte en sterfte. 261858006.
- 38. van Vliet M, Heymans MW, von Rosenstiel IA, Brandjes DP, Beijnen JH, et al. (2011) Cardiometabolic risk variables in overweight and obese children: a worldwide comparison. Cardiovasc Diabetol 10: 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Eckel RH, Krauss RM (1998) American Heart Association call to action: obesity as a major risk factor for coronary heart disease. AHA Nutrition Committee. Circulation 97: 2099–2100. [DOI] [PubMed] [Google Scholar]
- 40. Fontana L, Eagon JC, Trujillo ME, Scherer PE, Klein S (2007) Visceral fat adipokine secretion is associated with systemic inflammation in obese humans. Diabetes 56: 1010–1013. [DOI] [PubMed] [Google Scholar]
- 41. Huxley R, Mendis S, Zheleznyakov E, Reddy S, Chan J (2010) Body mass index, waist circumference and waist:hip ratio as predictors of cardiovascular risk–a review of the literature. Eur J Clin Nutr 64: 16–22. [DOI] [PubMed] [Google Scholar]
- 42. Corvalan C, Uauy R, Kain J, Martorell R (2010) Obesity indicators and cardiometabolic status in 4-y-old children. Am J Clin Nutr 91: 166–174. [DOI] [PubMed] [Google Scholar]
- 43. Thiering E, Bruske I, Kratzsch J, Hoffmann B, Herbarth O, et al. (2012) Peak growth velocity in infancy is positively associated with blood pressure in school-aged children. J Hypertens 30: 1114–1121. [DOI] [PubMed] [Google Scholar]
- 44. de Hoog MLA, van Eijsden M, Stronks K, Gemke RJBJ, Vrijkotte TGM (2011) The role of infant feeding practices in the explanation for ethnic differences in infant growth: the Amsterdam Born Children and their Development study. Br J Nutr 106: 1592–1601. [DOI] [PubMed] [Google Scholar]
- 45. Ujcic-Voortman JK, Baan CA, Verhoeff AP, Krol A, Seidell JC (2011) Ethnic differences in systemic inflammation: An investigation of C-reactive protein levels among Moroccan, Turkish and Dutch groups in the Netherlands. Atherosclerosis 218: 511–6. [DOI] [PubMed] [Google Scholar]
- 46. Timpson NJ, Nordestgaard BG, Harbord RM, Zacho J, Frayling TM, et al. (2011) C-reactive protein levels and body mass index: elucidating direction of causation through reciprocal Mendelian randomization. Int J Obes (Lond) 35: 300–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Buckley DI, Fu R, Freeman M, Rogers K, Helfand M (2009) C-reactive protein as a risk factor for coronary heart disease: a systematic review and meta-analyses for the U.S. Preventive Services Task Force. Ann Intern Med 151: 483–495. [DOI] [PubMed] [Google Scholar]
- 48. Palacios C, Wigertz K, Martin BR, Braun M, Pratt JH, et al. (2010) Racial differences in potassium homeostasis in response to differences in dietary sodium in girls. Am J Clin Nutr 91: 597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Savica V, Bellinghieri G, Kopple JD (2010) The effect of nutrition on blood pressure. Annu Rev Nutr 30: 365–401. [DOI] [PubMed] [Google Scholar]
- 50. Turban S, Miller ER III, Ange B, Appel LJ (2008) Racial differences in urinary potassium excretion. J Am Soc Nephrol 19: 1396–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Vega GL, Clark LT, Tang A, Marcovina S, Grundy SM, et al. (1998) Hepatic lipase activity is lower in African American men than in white American men: effects of 5′ flanking polymorphism in the hepatic lipase gene (LIPC). J Lipid Res 39: 228–232. [PubMed] [Google Scholar]
- 52. Desilets MC, Garrel D, Couillard C, Tremblay A, Despres JP, et al. (2006) Ethnic differences in body composition and other markers of cardiovascular disease risk: study in matched Haitian and White subjects from Quebec. Obesity (Silver Spring) 14: 1019–1027. [DOI] [PubMed] [Google Scholar]
- 53. Deurenberg P, Yap M, van Staveren WA (1998) Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord 22: 1164–1171. [DOI] [PubMed] [Google Scholar]
- 54. Nightingale CM, Rudnicka AR, Owen CG, Cook DG, Whincup PH (2010) Patterns of body size and adiposity among UK children of South Asian, black African-Caribbean and white European origin: Child Heart And health Study in England (CHASE Study). Int J Epidemiol 40: 33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Singh AS, Mulder C, Twisk JW, van MW, Chinapaw MJ (2008) Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 9: 474–488. [DOI] [PubMed] [Google Scholar]
- 56. Beckett LA, Rosner B, Roche AF, Guo S (1992) Serial changes in blood pressure from adolescence into adulthood. Am J Epidemiol 135: 1166–1177. [DOI] [PubMed] [Google Scholar]
- 57. Srinivasan SR, Frontini MG, Xu J, Berenson GS (2006) Utility of childhood non-high-density lipoprotein cholesterol levels in predicting adult dyslipidemia and other cardiovascular risks: the Bogalusa Heart Study. Pediatrics 118: 201–206. [DOI] [PubMed] [Google Scholar]
- 58. Owen CG, Nightingale CM, Rudnicka AR, Sattar N, Cook DG, et al. (2010) Physical activity, obesity and cardiometabolic risk factors in 9- to 10-year-old UK children of white European, South Asian and black African-Caribbean origin: the Child Heart And health Study in England (CHASE). Diabetologia 53: 1620–1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. van Dijk AE, van Eijsden M, Stronks K, Gemke RJBJ, Vrijkotte TGM (2010) Cardio-metabolic risk in 5-year-old children prenatally exposed to maternal psychosocial stress: the ABCD study. BMC Public Health 10: 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wang J, Thornton JC, Bari S, Williamson B, Gallagher D, et al. (2003) Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutr 77: 379–384. [DOI] [PubMed] [Google Scholar]
- 61. Johnson ST, Kuk JL, Mackenzie KA, Huang TT, Rosychuk RJ, et al. (2010) Metabolic risk varies according to waist circumference measurement site in overweight boys and girls. J Pediatr 156: 247–252. [DOI] [PubMed] [Google Scholar]