Abstract
Background
The American College of Surgeons Case Log (ACS Case Log) represents a data system that satisfies the American Board of Surgery (ABS) Maintenance of Certification (MOC) program, yet has broad data fields for surgical subspecialties. Using the ACS Case Log, we have developed a method of data capture, categorization, and reporting of acute care surgery fellows' experiences.
Study Design
In July 2010, our Acute Care Surgery fellowship required our fellows to log their clinical experiences into the ACS Case Log. Cases were entered similar to billable documentation rules. Keywords were entered that specified institutional services and/or resuscitation types. This data was exported in comma separated value format, de-identified, and structured by Current Procedural Terminology (CPT) codes relevant to acute care surgery and sub-stratified by fellow and/or fellow year.
Results
Fifteen report types were created consisting of operative experience by service, procedure by major category (cardiothoracic, vascular, solid organ, abdominal wall, hollow viscus, and soft tissue), total resuscitations, ultrasound, airway, Intensive Care Unit services, basic neurosurgery, and basic orthopaedics. Results are viewable via a secure web application, accessible nationally, and exportable to many formats.
Conclusions
Utilizing the ACS Case Log satisfies the ABS MOC program requirements and provides a method for monitoring and reporting acute care surgery fellow experiences. This system is flexible to accommodate the needs of surgical subspecialties and their training programs. As documentation requirements expand, efficient clinical documentation is a must for the busy surgeon. Although, our data entry and processing method has the immediate capacity for acute care surgery fellowships nationwide, multiple larger decisions regarding national case log systems should be encouraged.
INTRODUCTION
In 1984, the Accreditation Council for Graduate Medical Education (ACGME) case log was first used to capture procedures by general surgery residents.(1) Currently, from the time internship begins, procedural case logs are required ACGME documentation from 20 accredited residency specialties through a web-based system initiated in 2000. Upon residency completion from procedure-based specialties, residency case logs are mandatory to apply for certification by specialty boards, such as the American Board of Surgery (ABS).
After obtaining board certification in General Surgery, the ABS Maintenance of Certification (MOC) program "requires ongoing participation in a national, regional or local outcomes database or quality assessment program" and maintenance of a 12-month operative log to apply for re-certification in any ABS specialty. The American College of Surgeons (ACS) provides a case log system that satisfies MOC requirements, is organized by Current Procedural Terminology (CPT) codes, similar to the ACGME case log system, and also allows documentation of diagnoses and complications.(2)
Subspecialty surgery fellowships and subspecialty board certification processes are also increasingly requiring documentation of procedural experiences. Over 30 subspecialties, including pediatric, cardiothoracic and colorectal surgery, are using the ACGME resident case log,(3) while some fellowships are creating parallel, independent data entry systems, like the American Association for Surgery of Trauma (AAST) acute care surgery case log system.(4) In duplicate fashion, the ABS certification process for Surgical Critical Care requires data entry of critical care cases into a system designed only for the certification process. At the same time, certified general surgeons in fellowship training are simultaneously using the ACS Case Log given its data export feature that satisfies application for becoming a Fellow of the ACS, hospital credentialing, and long-term MOC requirements.
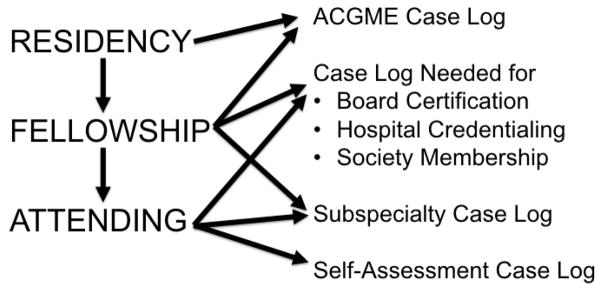
Despite the numerous data entry systems (Figure 1), experiential and procedural logs are valuable for trainees, program directors, hospitals, and specialty boards to quantify procedural character, quality and volume. Efforts to minimize data entry duplication would enhance efficacy and improve efficiency. Using the flexible ACS Case Log, we have developed a method of data capture, categorization, and reporting of acute care surgery fellows' experiences.
Figure 1.
Current utilization of surgery case logs.
METHODS
Procedural and clinical experiences of Surgical Critical Care and Acute Care Surgery fellows were logged in the ACS Case Log, starting in July 2010. This system was used to capture experiences believed to be relevant to fellow training. Using CPT codes, experiences and cases were entered identically to billable rules and documentation submitted to our electronic medical record. Annually, CPT codes are updated by the ACS Case Log and currently reflect any 2012 CPT changes. When relevant, in the ACS Case Log free-text "Notes" field, specific keywords were entered that specified unique fellow services, resuscitation types (Burn, Blunt, Penetrating), and focused abdominal sonography for trauma (FAST) test characteristics. This data was exported in comma separated value format and de-identified. IRB approval was obtained for the purposes of this publication.
Operative procedures, bedside procedures, and free-text designated resuscitations were parsed using STATA programming (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP). Coupling the code for evaluation and management of the critically ill (99291) with standardized free-text, we differentiated resuscitations from daily critical care time. Critical care time also captured elements essential for critical care certification such as hemodynamic monitoring, ventilator support, cardiac resuscitation, dialysis/hemofiltration, and nutritional support.
Relevant bedside diagnostic and therapeutic procedures were also captured. Ultrasound modalities measured were FAST examination performance with sensitivity and specificity reporting, in addition to transesophageal, transthoracic, and Doppler mode echocardiography exams. Bedside airway procedures captured included intubation, tracheostomy, and cricothyroidotomy. Bedside Intensive Care Unit (ICU) vascular procedures were subcategorized into placements of central venous catheters, arterial catheters, intraosseous access, inferior vena cava filters, transvenous pacers, Swan-Ganz catheters, and intra-aortic balloon pumps. Other bedside procedures included bronchoscopy, endoscopy, tube thoracostomy, percutaneous endoscopic gastrostomy, application of negative pressure wound therapy, provision of conscious sedation, paracentesis (including peritoneal lavage), thoracentesis, external cardioversion, cardiopulmonary resuscitation, laceration repair, port removal, and urinary system imaging.
For operative procedures with multiple CPT codes, the number of operative cases was kept distinct from the individual intra-operative CPT coded procedures performed. Based on our prior work and proposed curriculum in acute care surgery,(5,6) major operative procedures were then structured into six main Acute Care Surgery categories: Cardiothoracic, Vascular, Abdominal Wall, Gastrointestinal and Genitourinary, Solid Organ, and Soft Tissue. Cardiothoracic procedures ranged from exploration of penetrating thoracic wounds, thoracotomy, thoracoscopy, open sternal fixation, open rib fixation, cardiorraphy, pericardial window, lung resection, lung hernia repair, and esophageal repair. Vascular CPTs covered ligation or repair of major vasculature, vein harvest and/or ligation, amputation, and spinal exposures. Abdominal wall CPT codes covered exploratory laparotomy, diagnostic laparoscopy, exploration of penetrating wounds, hernias (ventral, femoral, inguinal, lumbar, laparoscopic), mesh manipulation, and evisceration repair. Gastrointestinal and Genitourinary CPTs covered the hollow viscus organs (stomach, small bowel, large bowel and bladder), endoscopy, and enteral feeding access. Soft tissue CPTs covered skin grafting, escharotomy, burn excision, fasciotomy, débridement, and myofasciocutaneous flap construction.
Orthopedic procedures represented a combination of bedside extremity closed treatment covering splinting, reduction, and external fixation. Neurosurgical CPTs included lumbar puncture, burr hole, ventricular access, craniotomy, and shunt creation and/or revision.
RESULTS
Each fellow's experience is collapsed into a single row of data covering the CPT groupings described in the methods. Using this structured programmed method to categorize ACS Case Log data, quarterly data processing time is one-hour for eight fellows.
Results are viewable by each of our fellows, faculty, and program director via a secure web application, REDCap (Research Electronic Data Capture; http://www.project-redcap.org),(7) accessible nationally, and exportable to variety of statistical packages and formats (PDF, Excel, SAS, STATA, SPSS, or R). Using the CPT designated categories, we created 15 report types (Table 1), and each structured by CPT codes and sub-stratified by fellow and fellowship year. The operative experience is also reported by the service on which the fellows train including: Trauma, Burn, Emergency General Surgery, Reconstructive General Surgery, and Thoracic services. An example of one data report representing a 12-month log of eight fellows is shown in Table 2.
Table 1.
Acute Care Surgery Case Log Report Types
| Report Types |
|---|
| Operative experience by service |
| Procedures by major category |
| Total resuscitations |
| Ultrasound |
| Airway |
| ICU Vascular access |
| Other ICU services |
| Operative thoracic |
| Operative abdominal wall |
| Operative GI and GU |
| Operative solid organ |
| Operative vascular |
| Operative Skin and Soft Tissue |
| Basic neurosurgical procedures |
| Basic orthopaedic procedures |
GI, gastrointestinal; GU, genitourinary.
Table 2.
Sample One-Year Report from ACS Case Log Data Export Manipulation
| Fellow | Fellow year | OR Trips | CT | Vascular | Solid organ | Abdominal wall | GI and GU | Soft tissue |
|---|---|---|---|---|---|---|---|---|
| A | First | 52 | 8 | 2 | 7 | 19 | 5 | 22 |
| B | First | 53 | 8 | 4 | 17 | 5 | 25 | 1 |
| C | First | 93 | 9 | 3 | 18 | 30 | 24 | 74 |
| D | First | 111 | 11 | 2 | 18 | 35 | 18 | 24 |
| E | Second | 80 | 21 | 9 | 17 | 46 | 41 | 18 |
| F | Second | 124 | 24 | 4 | 34 | 62 | 43 | 9 |
| G | Second | 132 | 25 | 5 | 14 | 40 | 51 | 9 |
| H | Second | 119 | 16 | 3 | 13 | 16 | 28 | 2 |
OR, operating room, CT, cardiothoracic, GI, gastrointestinal; GU, genitourinary.
CONCLUSIONS
Utilization of the ACS Case Log to record operative and educational experience simultaneously satisfies the MOC program requirements and provides a single method for monitoring both individual fellow and program experiences in acute care surgery. This system is adequately flexible to accommodate the needs of a variety of surgical subspecialties and their training programs. As documentation requirements expand, efficient clinical documentation is a must for the busy surgeon. Although our data entry and processing method has the immediate capacity for all acute care surgery fellowships nationwide, multiple larger decisions regarding a national case log system must be made.
A universal data entry and reporting system that fulfills the requirements of all surgeons, training programs, individual societies and independent credentialing committees should be considered (Figure 2). Creating new independent systems will create continued stress along career transitions among primary users, and will produce data that will be harder to manage and interpret.
Figure 2.
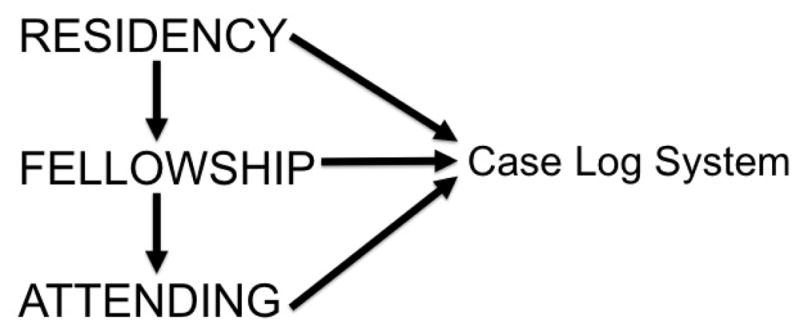
Ideal surgery case log system.
The ACGME case log is the pioneer of these data capture efforts and has the advantage of long history of consistent CPT based reporting,(8) data export, and handheld device data entry. Also, it has over 20 years of data organized by trauma sub-categories but one disadvantage is absence of acute care surgery reporting.(9) Other disadvantages of this system include the inability to upload aggregate data, lack of outcome reporting, and inability to compare to a national outcomes database like National Surgical Quality Improvement Program (NSQIP).
The ACS Case Log is a newer data system maintained by the ACS that captures data appropriate for board certification, society requirements, credentialing hurdles, MOC needs, and provides NSQIP comparative reports. It functions on multiple platforms including handheld devices, exports data, and has upload capability of aggregate data chunks. Currently, it demonstrates the capability for subspecialty information relevant to colorectal surgery and obstetrics, but lacks data fields focused on acute care surgery. We have created a unique solution to this by taking advantage of the free-text "Notes" field. A better solution would be standardized checkboxes for relevant information that would decrease the need for natural language processing, but that currently does not exist for acute care surgery fields. For acute care surgery fellowship programs, important fields relate to resuscitation type, critical care services, broad ultrasound and echocardiography use, and acute care surgery service sub-types. Reporting is a feature of the ACS Case Log, but it is not organized by broader categories of interest to particular subspecialties, and requires CPT manipulation and re-organization that we implemented externally. Our reporting system identifies variability in experiences that allows our trainees to hone in on deficiencies before completing training, and also identifies general fellowship weaknesses that our program uses quarterly to strengthen future service experiences. Our acute care surgery fellows are required to enter data daily and ensure their logs are complete prior to completion of our program.
The AAST acute care surgery case log captures information in a similar manner to those described above, but does not have real-time reporting capability and is only utilized by the trainees among a small cadre of accredited fellowship programs in acute care surgery (currently eight).(4) Additionally, to satisfy MOC, duplicate entry into the ACS Case Log may be necessary, and even if it is not done during fellowship, the ACS Case Log or other system will then have to be learned as an acute care surgery fellowship is finished.
The ultimate goal is validated automated data capture in real-time. The advent of the electronic medical record (EMR) systems and hospital informatics allow all of this data to be automatically captured without the fallibility or workload associated with manual entry. For example, anesthesia information management systems can automatically capture cases to ACGME requirements with at least 95% accuracy. When comparing this to manual resident entry, >50% of anesthesia residents under- or over-report their total case counts by at least 5%.(10) Other non-procedural specialties are also exploring automated data capture.(11) Given the disadvantage of manual entry in our method and the lack of verifiable compliance with data entry, we are currently engaging the institutional informatics department about automating data collection to match the ACS Case Log fields of entry and reduce the duplicative clerical burden on our fellows.
We believe the leadership within the ACGME, ABS, and specialty societies should unite in defining a single data capture system with the broadest capabilities and modification options. The opportunity cost of spending the time and resources on consolidation now will offset the hazards of managing multiple independent data systems in the future. Given the ACS Case Log remains up-to-date with ICD and CPT codes, is maintained free-of-charge, offers uploading from automated EMR data dumps, and has the flexibility to accommodate subspecialty needs, it seems logical that the ACS Case Log may be a good choice towards data system consolidation. Despite not directly processing data in triplicate among the ACS, ACGME and AAST case log systems, we compare their major characteristics in Table 3. Although our process is transportable nationwide and our group is capable of providing novel reporting for acute care surgery fellowships using its exporting feature and transforming this using STATA into web-viewable data via REDCap, the ACS Case Log reporting features could be easily upgraded after a consensus decision on CPT categorization, similar to the relatively stable ACGME classification and reporting of resident cases. Streamlining toward a single data system and its reporting infrastructure may result in an optimal case log solution.
Table 3.
Capabilities of Three Surgery Case Log Systems
| Case log characteristics | ACGME | AAST | ACS |
|---|---|---|---|
| Multi-platform entry, including handheld devices | X | X | |
| On-demand raw data exports | X | X | |
| On-demand reports | X | X | |
| On-demand data comparison to national data | X | ||
| Accepts aggregate data uploads | X | ||
| Satisfies board certification exam requirements | X | ||
| Data fields for surgical subspecialties | X | X | |
| Data fields dedicated for acute care surgery | X | X* | |
| Fulfills society admissions (ie FACS) and hospital credentialing | X | X | X |
| Satisfies ABS MOC program and board re-certification | X |
Created via data export manipulation.
ABS, American Board of Surgery; ACGME, Accreditation Council for Graduate Medical Education; AAST, American Association for Surgery of Trauma; ACS, American College of Surgeons; MOC, maintenance of certification.
Acute care surgery is still in evolution,(12) and hopefully, the data system solution we outlined further prompts the surgical leadership to define a more efficient solution that is broad enough for multiple surgical specialties, such as the ACS Case Log. Almost thirty years ago, general surgery was the pioneer in data entry and reporting for residents, and we have the opportunity to continue this effort for all surgeons.
Acknowledgments
Support: AHRQ Health Services 5T32HS013833-08, AHRQ (m.b.p.); Vanderbilt CTSA grant 1 UL1 RR024975 from NCRR/NIH (REDCap infrastructure).
ABBREVIATIONS
- AAST
American Association for Surgery of Trauma
- ABS
American Board of Surgery
- ACGME
Accreditation Council for Graduate Medical Education
- ACS
American College of Surgeons
- CPT
Current Procedural Terminology
- EMR
electronic medical record
- FAST
focused abdominal sonography for trauma
- ICU
Intensive Care Unit
- MOC
Maintenance of Certification
- NSQIP
National Surgical Quality Improvement Program
- REDCap
Research Electronic Data Capture
Footnotes
Disclosure Information: Nothing to disclose.
Abstract presented at the 25th Eastern Association for the Surgery of Trauma meeting, Lake Buena Vista, FL, January 2012.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Brown DL. Using an anesthesia information management system to improve case log data entry and resident workflow. Anesth Analg. 2011;112:260–261. doi: 10.1213/ANE.0b013e3181fe0558. [DOI] [PubMed] [Google Scholar]
- 2.Resilience Software. American College of Surgeons Surgeon Specific Registry (Case Log) Vancouver, Canada: [Accessed February 19, 2012]. Available from: https://acspbls.resiliencesoftware.com. [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education (ACGME) ACGME Resident Case Log. Chicago, Illinois: [Accessed February 19, 2012]. Available from: https://www.acgme.org/ResidentDataCollectionNet/ACGME/ResidentCaseLogs/Login.aspx. [Google Scholar]
- 4.American Association for the Surgery of Trauma (AAST) Acute Care Surgery Case Log. Chicago, Illinois: [Accessed February 19, 2012]. Available from: http://www.aast.org/AcuteCareSurgery/ACSCaseLog.aspx. [Google Scholar]
- 5.Diaz JJ, Miller RS, May AK, Morris JA. Acute care surgery: a functioning program and fellowship training. Surgery. 2007;141:310–316. doi: 10.1016/j.surg.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Hoyt DB, Kim HD, Barrios C. Acute care surgery: a new training and practice model in the United States. World J Surg. 2008;32:1630–1635. doi: 10.1007/s00268-008-9576-y. [DOI] [PubMed] [Google Scholar]
- 7.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Accreditation Council for Graduate Medical Education (ACGME) ACGME Case Log Statistical Reports. Chicago, Illinois: [Accessed February 19, 2012]. Available from: http://www.acgme.org/residentdatacollection/documentation/statistical_reports.asp. [Google Scholar]
- 9.Patel MB, Guillamondegui OD, May AK, Diaz JJ. Twenty-Year Analysis of Surgical Resident Operative Trauma Experience. J Surg Res. 2012 doi: 10.1016/j.jss.2012.04.061. (in press) [DOI] [PubMed] [Google Scholar]
- 10.Simpao A, Heitz JW, McNulty SE, et al. The design and implementation of an automated system for logging clinical experiences using an anesthesia information management system. Anesth Analg. 2011;112:422–429. doi: 10.1213/ANE.0b013e3182042e56. [DOI] [PubMed] [Google Scholar]
- 11.Bhattacharya P, Van Stavern R, Madhavan R. Automated data mining: an innovative and efficient web-based approach to maintaining resident case logs. J Grad Med Educ. 2010;2:566–570. doi: 10.4300/JGME-D-10-00025.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis KA, Rozycki GS. Acute care surgery in evolution. Crit Care Med. 2010;38:S405–410. doi: 10.1097/CCM.0b013e3181ec55c8. [DOI] [PubMed] [Google Scholar]