Abstract
Background
Hospital readmission within 30-days of an index hospitalization is receiving increased scrutiny as a marker of poor quality patient care. This study identifies factors associated with 30-day readmission following General Surgery procedures.
Study Design
Using standard National Surgical Quality Improvement Project (NSQIP) protocol, preoperative, intraoperative, and postoperative outcomes were collected on patients undergoing inpatient General Surgery procedures at a single academic center between 2009 and 2011. Data were merged with our institutional clinical data warehouse to identify unplanned 30-day readmissions. Demographics, comorbidities, type of procedure, postoperative complications, and ICD-9 coding data were reviewed for patients who were readmitted. Univariate and multivariate analysis was utilized to identify risk factors associated with 30-day readmission.
Results
1442 General Surgery patients were reviewed. 163 (11.3%) were readmitted within 30 days of discharge. The most common reasons for readmission were gastrointestinal complaint/complication (27.6%), surgical infection (22.1%), and failure to thrive/malnutrition (10.4%). Comorbidities associated with risk of readmission included disseminated cancer, dyspnea, and preoperative open wound (p<0.05 for all variables). Surgical procedures associated with higher rates of readmission included pancreatectomy, colectomy, and liver resection. Postoperative occurrences leading to increased risk of readmission were blood transfusion, postoperative pulmonary complication, wound complication, sepsis/shock, urinary tract infection, and vascular complications. Multivariable analysis demonstrates that the most significant independent risk factor for readmission is the occurrence of any postoperative complication (OR 4.20, 95% CI 2.89–6.13).
Conclusions
Risk factors for readmission after General Surgery procedures are multi-factorial; however, postoperative complications appear to drive readmissions in surgical patients. Taking appropriate steps to minimize postoperative complications will decrease postoperative readmissions.
Key Concepts: Postoperative Readmission, Complications, Risk Factors, General Surgery
Introduction
In June of 2009, the Centers for Medicare and Medicaid Services (CMS) began publishing 30-day readmission data for selected medical diseases. As a result, hospital readmissions quickly became an important metric for measuring quality of patient care. In March of 2010, the Patient Protection and Affordable Care act was signed into law and within it, Section 3025 brought substance to holding hospitals accountable for 30-day hospital readmissions.1 When implemented, hospital reimbursements will be reduced based on an adjustment factor determined by an institution’s expected versus observed 30-day readmission rate. Section 3025 started the focus on readmissions for selected Medical diseases, but left the door open for CMS to extend this readmission policy to surgical procedures in fiscal year 2015. The CMS has already confirmed it will begin monitoring readmissions for vascular surgery procedures. Consequently, there is an intense focus on decreasing unnecessary surgical readmissions.2,3
From 2003 to 2004, 19.5% of all Medicare beneficiaries who were discharged from a hospital were readmitted within 30 days, leading to a cost of $17.4 billion. Kent and colleagues further estimate that a single readmission following pancreatic resection costs an average of $16,000 or more.4 In addition to the financial implications of hospital readmission, a patient’s unplanned return to the hospital further limits hospital resources. Moreover, for each patient readmitted, there is an opportunity lost to treat another patient who needs care. Regardless of the strain a readmission places on the healthcare system, it negatively impacts the patient’s quality of life. Reducing the number of 30-day readmissions following surgery is important not only for institutions, but also for patients.
The readmission problem is fundamentally different in surgical patients compared to medical patients.5,6 A majority (70.5%) of readmissions following a surgical procedure are due to a medical condition. Of Medicare beneficiaries undergoing major bowel surgery in 2003–2004, 16.6% were readmitted for GI problems, while only 6.4% were readmitted with a postoperative infection.7 Surgical patients have underlying co-morbidities similar to medical patients; however, what differentiates the surgical patient is the notion that they undergo a specific procedure which in and of itself carries an associated risk of readmission. The other major differentiating factor for surgical patients is that the intervention which puts these patients at risk for readmission, i.e. their operation, is planned. This suggests that there is an opportunity to intervene preoperatively to decrease the risk of readmission postoperatively.
There is a paucity of information that focuses on readmission rates among surgical patients. Most of the studies that do exist focus on procedure-specific readmission rates within precise patient populations.4,8–13 A recent study which followed 33,936 patients after coronary artery bypass graft surgery showed that 16.5% were readmitted within 30 days or discharge.13 The most common reason for readmission was postoperative infection (16.9%). The authors identified a risk profile for patients who were at increased risk for postoperative infection. High risk patients included women, obesity, unplanned re-operations, and patients who had a longer hospital length of stay. Similarly, a recent series investigated readmission following 149,622 colorectal surgery cases for colon cancer.11 The authors note that hospital length of stay, comorbidities, and postoperative complications are each significantly associated with readmission. Finally, in a series which analyzed 1643 pancreaticoduodenectomies, younger age, considerable blood loss, postoperative complications, and vessel resection were found to be independent risk factors for readmission.8
These previous studies highlight the importance of decreasing readmissions following complex General Surgery procedures. The purpose of this study is to examine factors associated with 30-day hospital readmission after a variety of General Surgery procedures among a diverse patient population. We acknowledge that factors associated with 30-day readmission following General Surgery procedures are multi-factorial. The current study was undertaken to better understand which factors appear to be most commonly associated with readmission. Specifically, we hypothesize that postoperative complications in particular increase the chance of a patient returning to the hospital.
Methods
Study Population and Methods
This is a retrospective study utilizing patients who were enrolled in American College of Surgeons National Surgical Quality Improvement Program (ACS/NSQIP) that underwent inpatient General Surgery procedures at Emory University Hospital between October 2009 and July 2011. Outpatient procedures were excluded. Standard NSQIP data were gathered prospectively by the ACS/NSQIP trained nurses at our institution. 135 variables were analyzed, including preoperative risk factors, intraoperative variables, and 30-day postoperative morbidity and mortality outcomes for patients undergoing General Surgery procedures in the inpatient setting.14
Following a protocol approved by our Institutional Review Board, each patient’s index admission was linked via identifier codes to our institution’s clinical data warehouse to search for unplanned readmissions within 30-days of discharge. Comorbid factors for each patient were obtained and outcome data were ascertained at 30-day follow-up as previously described. We further determined if patients experienced a postoperative complication, and if so, when this occurred relative to readmission. Lastly we identified the ICD-9 codes associated with readmission in an effort to determine why the patient was readmitted. Patients were excluded from the study if they died during their index hospitalization or if the readmission was a planned aspect of their postoperative course (e.g.: chemotherapy).
Study Variables and Definitions
The primary outcome of interest was 30-day hospital readmission following an inpatient General Surgery Procedure. To facilitate data analysis based on type of procedure, we created General Surgery procedure categories based on the prioritized diagnostic groups identified by Schilling, et al.15 To allow for further analysis, the following complication categories were created based upon process improvement opportunities which would target and prevent specific postoperative complications: transfusion; postoperative pulmonary complications (PPC) (prolonged postoperative ventilation>48 hours, pneumonia, unplanned intubation); wound (superficial surgical site infection (SSI), organ space SSI, deep incisional SSI, wound disruption); sepsis/shock (sepsis and septic shock); urinary tract infection (UTI); renal (acute renal failure, progressive renal insufficiency); cardiac (myocardial infarction, cardiac arrest requiring CPR); neurologic (peripheral nerve injury, cerebrovascular accident, coma >24 hours; vascular (pulmonary embolism, DVT requiring therapy, graft/prosthesis/flap failure); and a category for patients with no complications.
Statistical Analysis
Univariate analysis was utilized to identify factors associated with 30-day readmission. The association between demographic characteristics or preoperative comorbid conditions on 30-day readmission was compared using chi-squared tests for categorical variables (or Fisher’s exact tests if needed) and ANOVA tests for continuous variables. In addition to preoperative comorbid conditions, we examined the association between operative procedure and postoperative complications on 30-day readmission. The association between these variables and the probability of readmission was assessed using chi-squared tests. Multivariable logistic regression was used to evaluate the independent association between complications and readmissions, controlling for possible confounders. Confounders were tested one at a time in a model along with complications to see if the association between complications and readmission changed. A final model was created using all the most influential variables. P-values less than 0.05 were considered significant. Cochran-Armitage trend test was used to determine the association between number of complications and the rate of readmission. All statistical analyses were performed using SAS 9.2 (SAS Institute, Inc., Carry, NC) and SPSS 17 (IBM SPSS Inc, Chicago).
Results
Patient Demographics
A total of 1,442 patients were identified in our NSQIP database that underwent General Surgery procedures from October 2009 up to July 2011. A total of 163 patients were readmitted within 30 days of discharge from their index hospitalization for an overall readmission rate of 11.3%. Patient demographics and risk factors associated with readmission are listed in Table 1. Age, race, gender and transfer status were not associated with an increased risk of readmission. ASA class significantly differed between the two groups, with ASA 4 and ASA 5 patients being at significantly higher risks of readmission (OR 11.60 and 23.50, respectively). Twenty-eight point eight percent of patients requiring readmission were hospitalized for greater than 24 hours before their surgical procedure, whereas only 17.8% of patients not requiring readmission were admitted more than one day preoperatively (p =0.0008).
Table 1.
Demographics and Risk Factors for Readmission
| Patient variable | No readmission (n=1,279) n (%) | Readmission cohort (n=163) n (%) | p Value | OR | 95% CI |
|---|---|---|---|---|---|
| Age, y, mean (SD) | 55.8(15.1) | 56.0 (15.8) | 0.9096 | ||
| Sex | 0.9858 | 1.00 | 0.72, 1.39 | ||
| Male | 552(88.6) | 71 (11.4) | |||
| Female | 733(88.6) | 94 (11.4) | |||
| Race | 0.7145 | 1.06 | 0.76, 1.48 | ||
| White | 920(89.1) | 113 (10.9) | |||
| Non-white | 459(88.4) | 60 (11.6) | |||
| ASA Class | 0.0013 | ||||
| Class 1 | 47(97.9) | 1(2.1) | 1.00 | ||
| Class 2 | 397(91.9) | 35(8.1) | 4.14 | 0.55, 30.95 | |
| Class 3 | 753(87.6) | 107(12.4) | 6.68 | 0.91, 48.91 | |
| Class 4 | 77(80.2) | 19(19.8) | 11.60 | 1.50, 89.49 | |
| Class 5 | 2(66.7) | 1(33.3) | 23.50 | 1.05, 528.1 | |
| Transfer Status | 0.4484 | 1.27 | 0.69, 2.33 | ||
| Yes | 82(86.3) | 13 (13.7) | |||
| No | 1197(88.9) | 150(11.1) | |||
| Pre-Op length of stay >24 h | 228(17.8) | 47(28.8) | 0.0008 | 1.87 | 1.29, 2.70 |
| No complication | 925(93.7) | 62(6.3) | |||
| Any complication | 354(77.8) | 101(22.2) | <0.0001 | 4.26 | 3.03, 5.98 |
| Complication type* | |||||
| Transfusion | 196(82.0) | 43(18.0) | <0.0001 | 1.98 | 1.35, 2.90 |
| PPC | 61(71.8) | 24(28.2) | <0.0001 | 3.45 | 2.08, 5.71 |
| Wound complication | 132(73.7) | 47(26.3) | <0.0001 | 3.52 | 2.40, 5.17 |
| Sepsis/shock | 70(66.7) | 35(33.3) | <0.0001 | 4.73 | 3.03, 7.37 |
| UTI | 25(62.5) | 15(37.5) | <0.0001 | 5.08 | 2.62, 9.86 |
| Cardiac | 11(84.6) | 2(15.4) | 0.6508 | 1.43 | 0.31, 6.52 |
| Vascular | 14(56.0) | 11(44.0) | <0.0001 | 6.36 | 2.84, 14.25 |
| Renal | 20(71.4) | 8(28.6) | 0.0106 | 3.19 | 1.38, 7.35 |
| Neurologic | 10(83.33) | 2(16.67) | 0.6364 | 1.58 | 0.34, 7.26 |
| Timing of first complication | |||||
| During index Admission | 293(82.1) | 64 (17.9) | <.0001 | 0.36 | 0.22, 0.59 |
| After discharge | 61(62.2) | 37(37.8) | |||
In some cases numbers do not add up to 2,242 secondary to missing data points.
Multiple patients had more than one complication, thus numbers and percentages for this category will be greater than 2242 and 100%, respectively
Reason for Readmission
The reasons for readmission, based upon administrative ICD-9 coding data, are listed in Table 2. Gastrointestinal (GI) complaints and complications (nausea, vomiting, bowel obstruction, etc.) combined with surgical infections accounted for nearly half of all readmissions (27.6 and 22.1%, respectively). When sub-divided by procedure category, over 50% of readmissions following colectomy, liver resection, and pancreatectomy were also GI complaints/complications and surgical infections. Following these top two reasons for readmission, the ICD-9 diagnoses varied widely for the entire cohort and when further sub-divided by procedure.
Table 2.
Readmission Reasons by ICD-9 Codes
| Reason for readmission | ICD-9 Codes | n | % |
|---|---|---|---|
| GI complication | 8.45, 289.59, 531.4, 534.4, 536.8, 540.9, 552.2, 552.21, 552.8, 558.9, 560.1, 560.39, 560.81, 560.89, 560.9, 564, 569.62, 569.69, 576.1, 577, 577.1, 578, 787.01, 997.4 | 45 | 27.6 |
| Surgical infection | 38.19, 567.22, 996.62, 996.63, 996.69, 997.62, 998.51, 998.59, 999.31 | 36 | 22.09 |
| FTT/Malnutrition | 262, 263.9, 275.3, 276.5, 276.51, 458, 783.7 | 17 | 10.43 |
| Wound Complication | 553.21, 718.46, 998.12, 998.13, 998.32, 998.6, 998.83 | 13 | 7.98 |
| GU complication | 403.91, 584.9, 599, 599.71, 599.84, 996.64 | 8 | 4.91 |
| Vascular complication | 440.24, 441.01, 441.4, 557, 557.1, 557.9, 996.1, 996.74 | 6 | 3.68 |
| Pulmonary Complaint | 415.19, 486, 511, 511.19, 518.81, 786.52, 997.39 | 6 | 3.68 |
| Cardiac complaint | 410.21, 414.01, 414.06, 427.89, 428, 428.23 | 5 | 3.07 |
| Pain | 338.18, 789.07, 789.09 | 3 | 1.84 |
| Fever | 507, 780.6, 780.62 | 4 | 2.45 |
| Transplant complication | 996.81, 996.82, 996.84 | 3 | 1.84 |
| Neurologic complaint | 780.2, 786.59 | 2 | 1.23 |
| Other | 155.1, 157, 158.8, 189, 195.2, 198.3, 249, 250.13, 250.7, 250.8, 252.1, 289.7, 311, 482.42, 620.2, 996.52, 998.89 | 15 | 9.20 |
Comorbidities
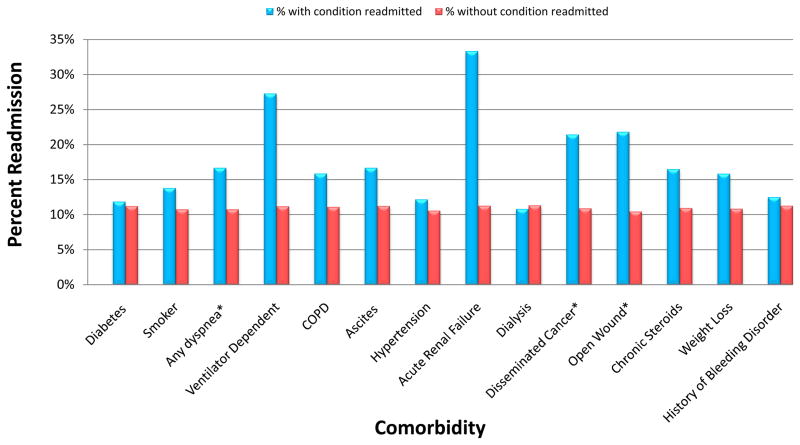
Figure 1 shows readmission rates based upon patients’ comorbidity profile. Patients with a diagnosis of disseminated cancer (n=56) or an open wound (n=110) preoperatively were over two times more likely to be readmitted (p=0.015 and 0.0003, respectively). Additionally, patients with a history of dyspnea (n=138) were over 50% more likely to be readmitted (OR 1.55, p=0.036). Comorbidities without statistically significant impact on risk of readmission included diabetes (n=228), smoker (n=261), COPD (n=63), preoperative ventilator dependence (n=11), ascites (n=24), hypertension requiring medication (n=674), chronic steroid use (n=97), unintentional preoperative weight loss (n=139), history of bleeding disorders (n=56), acute renal failure (n=3), and chronic renal failure requiring dialysis (n=37).
Figure 1.
Comorbidity profile of readmitted patients. * p <0.05
Procedures
Readmission frequency for the most common operative procedures within our cohort is listed in Table 3. Patients undergoing a pancreatectomy had the highest readmission rate (17.9%) for any procedure at our institution, followed by patients undergoing colectomy with or without colostomy (12.6%), small bowel resection (11.8%), gastrectomy (11.4%), and ventral hernia repair (11.0%). Procedures with low 30-day readmission rates in our analysis included parathyroidectomy (7.7%), thyroidectomy (2.9%), and mastectomy (2.0%).
Table 3.
Readmission by Procedure
| Procedure | n | No readmission (n=1,279) n (%) | Readmission cohort (n=163) n (%) |
|---|---|---|---|
| Pancreatectomy | 190 | 156 (82.11) | 34 (17.89) |
| Colectomy +/− colostomy | 230 | 201 (87.39) | 29 (12.61) |
| Small bowel resection | 93 | 82 (88.17) | 11 (11.83) |
| Gastrectomy | 44 | 39 (88.64) | 5 (11.36) |
| Ventral Hernia Repair | 100 | 89 (89.00) | 11 (11.00) |
| Liver Resection | 124 | 112 (90.32) | 12 (9.68) |
| Cholecystectomy | 74 | 67 (90.54) | 7 (9.46) |
| Parathyroidectomy | 39 | 36 (92.31) | 3 (7.69) |
| Thyroidectomy | 35 | 34 (97.14) | 1 (2.86) |
| Mastectomy | 101 | 99 (98.02) | 2 (1.98) |
| Other* | 412 | 364 (88.35) | 48 (11.65) |
Remaining general surgery and vascular procedures, including bariatric/foregut surgery, exploratory laparotomy, aneurysm repair, and soft tissue excision/reconstruction.
Complications
Patients who had one or more complications after their surgical procedure were over four times more likely to be readmitted (OR 4.26, 95% CI 3.03–5.98). Multivariable modeling was conducted controlling for demographic variables (Table 1) and comorbidities (Figure 1) but none made a significant impact on the relationship between complications and readmissions. A final model with all variables that made more than a 2% change to the OR for complications is shown in Table 4. After controlling for preoperative open wound, preoperative sepsis, ASA class and procedure (pancreatectomy), the odds of readmission only slightly decreased (OR 4.20, 95% CI 2.89–6.13). The only other significant variable affecting the odds of readmission was pancreatectomy (OR 1.7, 95% CI 1.09–2.66). No interactions between complications and other variables were found significant.
Table 4.
Multivariable Model
| Variable | Adjusted Odds Ratio for Readmission | 95% CI |
|---|---|---|
| Preoperative sepsis | 1.18 | (0.70, 1.99) |
| Preoperative open wound | 1.28 | (0.71, 2.29) |
| ASA 1 | 1.00 | --- |
| ASA 2 | 2.75 | (0.36, 20.91) |
| ASA 3 | 3.25 | (0.43, 24.30) |
| ASA 4 | 3.78 | (0.47, 30.43) |
| ASA 5 | 5.07 | (0.21, 119.96) |
| Procedure: pancreatectomy | 1.70* | (1.09, 2.66) |
| Postoperative complication | 4.20* | (2.89, 6.13) |
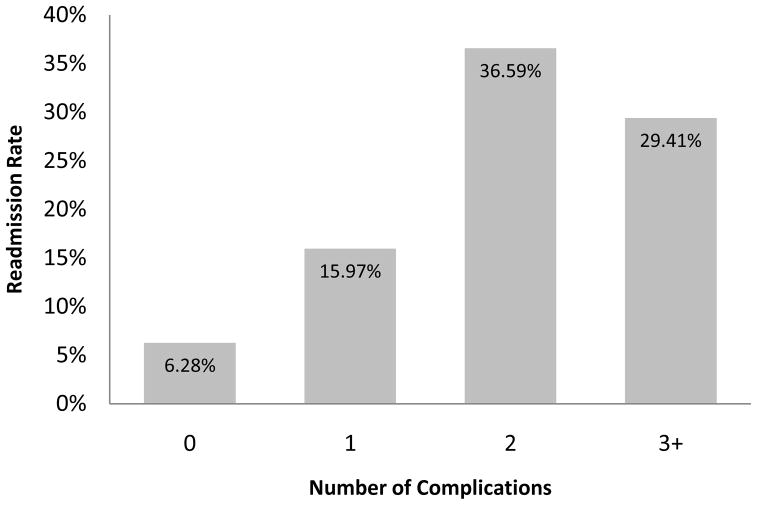
Figure 2 further demonstrates that the risk of readmission increases based on the number of complications that a patient experienced. Patients with the highest rate of readmission are those that had two postoperative complications. Although there is a small decrease in the readmission rate for patients with 3 or more complications, calculation of this relationship with the Cochran-Armitage trend test demonstrates a significant trend of increasing readmission rate with the number of complications that occur (p<0.0001). Furthermore, the median hospital length of stay was 5 days for patients with no complications, 9 days for patients with one complication, 12 days for patients with two complications, and 24 days for three or more complications.
Figure 2.
Rate of readmissions by number of complications. Cochran-Armitage trend test demonstrates a significant increasing trend in rate of readmission as more complications occur (p<0.0001).
The specific complications which occurred in patients who were readmitted are listed in Table 1. Wound complications were the most common complication within the readmission cohort (28.8%). The second-most-frequent postoperative occurrence associated with readmission was blood transfusion within 72 hours of a surgical procedure (26.4%). The next most common occurrences were sepsis/shock (21.5%), PPC (14.7%), and UTI (9.2%). Patients who experienced a complication after discharge had two times the readmission rate compared to those whose complication occurred during the index admission (37.8% vs. 17.9%, p=<0.0001).
While wound complications were the most common occurrence seen in patients that were readmitted, analysis demonstrates that these patients were three and a half times more likely to be readmitted (OR 3.52, 95%CI 2.40–5.17). In contrast, however, postoperative UTI was a relatively uncommon occurrence in patients who were readmitted, yet it was associated with the highest risk for readmission (OR 5.08, 95%CI 2.62–9.86).
Discussion
In April of 2012, the CMS proposed a new methodology for adjusting hospital reimbursements based upon the number of readmissions, with excessive readmissions leading to decreased payments.16 Furthermore, the Agency for Healthcare Research and Quality has recently funded a program entitled Project RED (re-engineered discharge) which focuses upon patient education that facilitates successful hospital discharge.17 With the increased attention placed upon readmissions in our current healthcare climate, it is essential to understand risk factors and how readmissions might be prevented.
The reasons for readmission following a General Surgery procedure are multi-factorial. However, the common denominator which appears in our data, as well as other studies in the literature, is that of postoperative complications. Studies examining patients who were readmitted following colon resection cite postoperative blood transfusion, dehydration, and infection as being the complications leading to significant rates of readmission.9,11,12,18 Similarly, among patients undergoing pancreatic resections, postoperative wound infections, pancreatic fistulas, and delayed gastric emptying have been reported to be associated with increased risk of readmission.4,8,19,20
Our study provides further evidence that postoperative complications are the most significant independent risk factor leading to hospital readmissions. Our analysis shows that any postoperative complication, independent of patient- and procedure-specific risk factors, increases risk of readmission by a factor of four. Furthermore, patients with postoperative sepsis or UTI were around five times more likely to be readmitted than those patients without, and postoperative wound infections and postoperative pulmonary complications both carried an approximate three and a half-fold increase in readmission rates.
The results of our analysis also demonstrate that certain complications represent a disproportionately large portion of readmissions. For example, postoperative blood transfusions doubled a patient’s risk for readmission and represented over 25% of our readmitted patient population. On the other hand, postoperative UTIs accounted only for 9.2% of readmissions, but they actually carried the highest risk for readmission of all complications studied (OR=5.08). Understanding which postoperative complications carry larger risks will be helpful in determining how to allocate resources in order to prevent the complications, and readmission, following surgery.
We also show that the number of complications, along with their timing, influence the risk of readmission. Patients with one complication were over two times likely to be readmitted than those without any postoperative complications. Furthermore, patients with two complications were over twice as likely to be readmitted as patients with only one complication, and over five times as likely when compared to patients without complications. Our data reveal, however, that patients who have three or more complications have a slightly lower risk of readmission than those who only have two complications. There could be several ways to interpret this finding. First, we demonstrate that patients with a three or more complications have substantially longer lengths of stay (24 days compared to 12 days or less for two or fewer complications), and are thus less likely to be discharged prematurely before the complications are completely treated and/or appropriate transition of care has been arranged. This reasoning is further supported by the fact that patients whose complications occur during, not after, their index admission are more than half as likely to be readmitted. Finally, it could be that the severity of the complications, not the actual number, is driving the rate of readmission. Future prospective analysis will be needed to clarify this result.
In addition to postoperative complications, certain risk factors such as procedure type and preoperative length of stay were associated with readmission risk. While these variables cannot be changed in and of themselves, we do have an opportunity to intervene pre- and postoperatively if we know ahead of time that specific patients are at increased risk for readmission. Hendren and colleagues report that patients at risk for readmission following colectomy for colon cancer are more likely to be elderly, male, African American, and from a lower socioeconomic status.9 While our study did not find any significant association between age, race, gender and readmission, we do reveal that patients who undergo complex gastrointestinal surgery (pancreatectomy, hepatectomy, and colectomy), and have a preoperative length of stay greater than 24 hours are more likely to be readmitted than other patients.
Intra-abdominal General Surgery procedures are much more likely to be associated with postoperative complications than those outside the abdomen all together (e.g. mastectomy, parathyroidectomy, and thyroidectomy), and our study results further support this notion.21 Additionally, patients who are in the hospital for at least 24 hours prior to their surgery are likely to have greater exposure to nosocomial bacteria, further increasing the risk of an infectious complication following surgery. Multidisciplinary efforts by physicians, nurses, therapists and social workers, should be focused on these specific patient populations during preoperative clinic visits and throughout their hospital stay in order to minimize the risk of postoperative complications and readmission.
There are a few comorbidities which significantly affect the risk of readmission. Patients with disseminated cancer and open wounds are at nearly double the risk of readmission than those without. Patients with dyspnea are at further risk for readmission. When you compare preoperative comorbidities to the postoperative complications associated with readmission, they are undoubtedly related. Patients who are immunosuppressed, poor wound healers, and who have baseline pulmonary disease are vulnerable to complications which will increase the likelihood of postoperative readmission. There is an abundance of evidence within the literature to support that comorbidities such as diabetes, smoking, and immunosuppresion increase the risk of surgical site infections and postoperative pulmonary complications.22,23 However, our analysis underscores the notion that postoperative complications, independent of patient comorbidity, are associated with a four-fold increase in risk of readmission. Multiple comorbidities such as acute renal failure, ventilator dependence, and ascites, while associated with a high rate of readmission, were not statistically significant risk factors within our study. This is likely due to the small number of patients with these comorbidities within our cohort. Only three patients had preoperative renal failure, 11 were ventilator dependent, and 26 had ascites.
In early 2011, Atul Gawande introduced the idea of “hot spots” within the American healthcare system.24 Based upon healthcare utilization research, Gawande suggests that the sickest, most “difficult” patients account for the largest expenditure of healthcare dollars. Thus, if resources can be focused upon certain high-risk patient populations undergoing complex inpatient procedures, the number of postoperative complications could be considerably reduced and incidence of hospital readmission could be less frequent. As a result, the potential for healthcare savings could be quite significant.
Our data demonstrate that postoperative complications, in particular, drive readmission rates at our institution. Consequently, focusing our efforts on effectively preventing and appropriately managing postoperative complications in high-risk patients could greatly impact the number of readmissions following surgical procedures. Patients who experience postoperative complications are likely to have a more complex discharge plan involving wound care instructions, antibiotic regimens, and/or rehabilitation therapy, each of which could lead to a readmission if not properly executed following discharge from the hospital.25
There are at least three weaknesses to our study. First, the data were collected locally for a single institution, and the small study size leads to deficiencies in gaining statistical power. While large multi-institutional databases such as the NSQIP Participant User Files are extremely valuable, the data are de-identified, thus limiting the ability to capture patient readmissions. What is important to appreciate, however, is the impact that local data can have on quality improvement within single medical centers. It can be difficult to determine an institution’s quality risks using large-powered, multi-institutional studies, while here we show the value of local data.
Second, we utilized encounter-specific NSQIP variable to analyze the risk of readmission. It is possible that other factors which are not captured by the NSQIP database could be contributing to hospital readmissions. Furthermore, we should note that our method of detecting readmissions by linking our NSQIP data to our clinical data warehouse leaves the study vulnerable to underestimating readmissions. It is plausible that a patient might seek treatment for follow-up care at an outside institution. However, due to the fact that we are a regional tertiary care referral center, the majority of patients treated at our institution for their index admission are directed back here for care if a subsequent complication arises. In future studies, it might be possible to link multiple data sets which could capture patient readmissions at multiple institutions.
Finally, this study is exploratory with the aim of identifying factors associated with readmission following a general surgical procedure. Future studies with larger sample sizes should be utilized to build and validate predictive models for the risk of 30-day readmission. The results we have presented, however, offer a framework for institutions to think about when trying to address and prevent unplanned patient readmissions to the hospital.
Conclusion
In conclusion, better understanding the predictors of readmission for General Surgery patients will allow hospitals to develop programs to decrease readmission rates. We demonstrate that patients with multiple medical comorbidities who undergo inpatient abdominal procedures, especially those admitted 24 hours or more prior to surgery, are at risk for readmission. This increased risk, however, is manifested through the development of postoperative complications. Future studies should focus on specifically targeting these high-risk patients in order to decrease the rate of 30-day readmission.
There is certainly an acceptable baseline readmission rate for each surgical procedure that needs to be defined. However, given the current healthcare environment, reducing readmissions by just a small amount will have a large impact on hospital budgets and operations. With the utilization of local data, individual institutions have the ability to analyze areas of weakness and re-focus their efforts on reducing readmissions and cutting costs. And most importantly, there is the patient. Each complication averted or readmission prevented is one less burden for our patients to bear during an already trying and difficult time.
Acknowledgments
This work was supported in part by National Institutes of Health/National Institute of Aging Grant 1RC4AG039071 (to Drs Sweeney and Cox).
Footnotes
Disclosure Information: Nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.The Patient Protection and Affordable Care Act. 111th United States Congress. March 23, 2010.
- 2.Adeyemo D, Radley S. Unplanned general surgical re-admissions - how many, which patients and why? Ann R Coll Surg Engl. 2007;89:363–367. doi: 10.1308/003588407X183409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman B, Basu J. The rate and cost of hospital readmissions for preventable conditions. Med Care Res Rev. 2004;61:225–240. doi: 10.1177/1077558704263799. [DOI] [PubMed] [Google Scholar]
- 4.Kent TS, Sachs TE, Callery MP, Vollmer CM., Jr Readmission after major pancreatic resection: a necessary evil? J Am Coll Surg. 2011;213:515–523. doi: 10.1016/j.jamcollsurg.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:326–341. doi: 10.1097/01.sla.0000179621.33268.83. discussion 341–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson GF, Steinberg EP. Hospital readmissions in the Medicare population. N Engl J Med. 1984;311:1349–1353. doi: 10.1056/NEJM198411223112105. [DOI] [PubMed] [Google Scholar]
- 7.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 8.Emick DM, Riall TS, Cameron JL, et al. Hospital readmission after pancreaticoduodenectomy. J Gastrointest Surg. 2006;10:1243–1252. doi: 10.1016/j.gassur.2006.08.016. discussion 1252–1253. [DOI] [PubMed] [Google Scholar]
- 9.Hendren S, Morris AM, Zhang W, Dimick J. Early discharge and hospital readmission after colectomy for cancer. Dis Colon Rectum. 2011;54:1362–1367. doi: 10.1097/DCR.0b013e31822b72d3. [DOI] [PubMed] [Google Scholar]
- 10.Kellogg TA, Swan T, Leslie DA, et al. Patterns of readmission and reoperation within 90 days after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2009;5:416–423. doi: 10.1016/j.soard.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 11.Schneider EB, Hyder O, Brooke BS, et al. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J Am Coll Surg. 2012 doi: 10.1016/j.jamcollsurg.2011.12.025. [DOI] [PubMed] [Google Scholar]
- 12.Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis Colon Rectum. 2011;54:1475–1479. doi: 10.1097/DCR.0b013e31822ff8f0. [DOI] [PubMed] [Google Scholar]
- 13.Hannan EL, Zhong Y, Lahey SJ, et al. 30-day readmissions after coronary artery bypass graft surgery in New York State. JACC Cardiovasc Interv. 2011;4:569–576. doi: 10.1016/j.jcin.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 14. [Accessed January 10, 2012.];American College of Surgeons National Surgical Quality Improvement Program. Available online: www.acsnsqip.org.
- 15.Schilling PL, Dimick JB, Birkmeyer JD. Prioritizing quality improvement in general surgery. J Am Coll Surg. 2008;207:698–704. doi: 10.1016/j.jamcollsurg.2008.06.138. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Medicare and Medicaid Services. [Accessed 16 May 2012.];“FY 2013 Hospital Readmissions Reduction Program Supplemental Data File.” Inpatient Prospective Payment System. Available online: http://www.cms.gov.
- 17.Agency for Healthcare Research and Quality. [Accessed 16 May 2012.];Re-engineered discharge project dramatically reduces return trips to the hospital. Available online: http://www.ahrq.gov/research/mar11/0311RA1.htm.
- 18.Guinier D, Mantion GA, Alves A, et al. Risk factors of unplanned readmission after colorectal surgery: a prospective, multicenter study. Dis Colon Rectum. 2007;50:1316–1323. doi: 10.1007/s10350-007-0310-x. [DOI] [PubMed] [Google Scholar]
- 19.Halloran CM, Ghaneh P, Bosonnet L, et al. Complications of pancreatic cancer resection. Dig Surg. 2002;19:138–146. doi: 10.1159/000052029. [DOI] [PubMed] [Google Scholar]
- 20.McPhee JT, Hill JS, Whalen GF, et al. Perioperative mortality for pancreatectomy: a national perspective. Ann Surg. 2007;246:246–253. doi: 10.1097/01.sla.0000259993.17350.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aust JB, Henderson W, Khuri S, Page CP. The impact of operative complexity on patient risk factors. Ann Surg. 2005;241:1024–1027. doi: 10.1097/01.sla.0000165196.32207.dd. discussion 1027–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheadle WG. Risk factors for surgical site infection. Surg Infect (Larchmt) 2006;7 (Suppl 1):S7–11. doi: 10.1089/sur.2006.7.s1-7. [DOI] [PubMed] [Google Scholar]
- 23.Sachdev G, Napolitano LM. Postoperative pulmonary complications: pneumonia and acute respiratory failure. Surg Clin North Am. 2012;92:321–344. doi: 10.1016/j.suc.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 24.Gawande A. The hot spotters: can we lower medical costs by giving the neediest patients better care? New Yorker. 2011:40–51. [PubMed] [Google Scholar]
- 25.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]