Abstract
Study Design
Serial, cross-sectional, nationally representative surveys of non-institutionalized adults.
Objective
To examine expenditures on common ambulatory health services for the management of back and neck conditions.
Summary of Background Data
Although it is well recognized that national costs associated with back and neck conditions have grown considerably in recent years, little is known about the costs of care for specific ambulatory health services that are used to manage this population.
Methods
We used the Medical Expenditure Panel Survey (MEPS) to examine adult (age ≥ 18 years) respondents from 1999 to 2008 who sought ambulatory health services for the management of back and neck conditions. We used complex survey design methods to make national estimates of mean inflation-adjusted annual expenditures on medical care, chiropractic care, and physical therapy per user for back and neck conditions.
Results
Approximately 6% of US adults reported an ambulatory visit for a primary diagnosis of a back or neck condition (13.6 million in 2008). Between 1999 and 2008, the mean inflation-adjusted annual expenditures on medical care for these patients increased by 95% (from $487 to $950); most of the increase was accounted for by increased costs for medical specialists, as opposed to primary care physicians. Over the study period, the mean inflation-adjusted annual expenditures on chiropractic care were relatively stable; while physical therapy was the most costly service overall, in recent years those costs have contracted.
Conclusion
Although this study did not explore the relative effectiveness of different ambulatory services, recent increasing costs associated with providing medical care for back and neck conditions (particularly subspecialty care) are contributing to the growing economic burden of managing these conditions.
Keywords: Medical Expenditure Panel Survey (MEPS), Spine Expenditures, Back Pain, Neck Pain
Introduction
Back and neck conditions are associated with considerable costs to the US economy both due to direct expenditures on their management and to indirect costs from losses in productivity. Between 49% and 70% of all adults will experience a back pain episode during their lifetime, and, at any given point in time, 12% to 30% of adults have an active back problem.1 Back pain is the second most common reason adults consult a primary care provider, following upper respiratory infections.2, 3 In recent years the prevalence and expenditures on spinal conditions in the US has increased significantly despite little change in the health status among people who suffer from these conditions.4,5 Estimates of the total expenditures on care vary, but the general consensus is that approximately $90 billion is spent on the diagnosis and management of low back pain, and an additional $10 to $20 billion is attributed to economic losses in productivity each year.4, 6, 7 However, little is known about the pattern of expenditures for different health services that manage this population.
It is generally accepted that medical care per unit (i.e. either per procedure or per episode) has gotten more expensive. Less is known about the cost of other non-medical services, such as chiropractic care and physical therapy, that manage a large percentage of back and neck cases in the US.8 Examining expenditures on the various ambulatory health services for back and neck conditions, particularly over time, is essential for health policy makers. Such information offers insight into the effects of health policy decisions and informs future strategies in regards to cost-containment efforts. As future health policy decisions will entail consideration of the overall cost and effectiveness of spinal interventions to improve population health, it is important to have a better understanding of spending patterns on health services.
Therefore we used the Medical Expenditure Panel Survey (MEPS) to examine US expenditures on common ambulatory health services for the management of back and neck conditions (spine conditions). We specifically examined expenditures on medical care, chiropractic care, and physical therapy—three of the most common ambulatory health services utilized by individuals with spine conditions.
Materials and Methods
The MEPS is a nationally representative survey of the non-institutionalized US population that is conducted annually by the Agency for Healthcare Research and Quality (AHRQ). 9 Information is gathered on healthcare utilization, expenditures, and health status. The MEPS utilizes an overlapping panel design consisting of a household component, medical provider component, and insurance provider component. For each year, personal and family level data obtained from the household, medical provider, and insurance provider are collected and aggregated. We used data from the MEPS consolidated annual files and the office-based and outpatient event files to gather information of ambulatory health services. Because our study used de-identified and publically available data it was granted an exemption from institutional board review by XX’s Committee for the Protection of Human Subjects.
Study Sample
We analyzed data from all adult (≥ 18 years) respondents to the MEPS survey from 1999 to 2008. The MEPS utilizes a sample frame of the previous year’s National Health Interview Survey to identify respondents. Sample sizes for the MEPS from these years ranged from a low of 23,565 individuals in 1999 to a high of 37,418 in 2002; response rates ranged from 56.9% in 2007 to 66.3% in 2001.
Respondents to the MEPS survey were asked if they had seen a healthcare provider in the past 6 months and, if so, what type of provider they visited, how many visits were made, and how much was spent on the service. Among the different healthcare provider types in the MEPS were “medical doctor,” “chiropractor,” or “physical therapist.” Starting in 2002, the MEPS recorded information on the specialty of the medical physician, allowing us to compare expenditures on primary care versus medical specialty services from 2002 to 2008. We operationally defined primary care as medical physicians identified as “family physicians,” “internal medicine,” or “general practice.”
For all visits, the MEPS reports the “best category for visit;” we used this variable to identify only visits made for “diagnosis and management” for this study.
If the individual reported having seen a healthcare provider, the MEPS proceeded to contact the individual’s provider and healthcare insurance to verify information regarding utilization (i.e. visit dates and details of office-based or outpatient visits) and expenditures. Our analysis used adult MEPS respondents who reported having seen any provider for an ambulatory health service for a primary diagnosis of spine condition, which ranged from 941 in 1999 to 1,607 in 2002.
Measures
Expenditures and Ambulatory Visits for Spine Conditions
The MEPS separates ambulatory visits to healthcare providers into either office-based or outpatient “events.” An outpatient event is defined as an ambulatory visit to an outpatient facility within a hospital; an office-based event, as a visit to healthcare provider’s office. We combined office-based and outpatient events to acquire information on the total number of annual ambulatory visits and expenditures on health services for spine conditions. For each respondent who reported an ambulatory visit for spine condition we aggregated their total expenditures and determined the mean total annual expenditures and expenditure per visit according to the health service.
The MEPS inquires about the health conditions and use of health services to address them. These self-reported conditions are then mapped to ICD-9-CM codes by trained MEPS coders. To identify ambulatory visits for spine conditions we used a combination of ICD-9-CM codes that have been demonstrated to capture the majority of such conditions (Appendix Table 1).7, 10 To ensure respondent confidentiality, the MEPS limits ICD-9-CM codes to 3 digits; therefore, the level of detail of spine condition diagnoses was somewhat limited. To ensure that the codes were similar across the health services we examined, we calculated the unweighted percent of ICD-9-CM codes by user type for 2008—which was comparable (Appendix Table 1). We did not include ICD-9-CM procedure codes because these were limited to 2 digits, rendering them unable to be attributed to spine conditions.
The MEPS reports up to 4 ICD-9-CM codes for each ambulatory visit. While previous reports that aimed to represent total utilization and expenditure related to spine conditions have used all 4 ICD-9-CM codes to identify visits,4, 5 we used only the primary diagnosis ICD-9-CM code (the first ICD-9-CM code reported). Because our study aimed to compare expenditures on common ambulatory services for the management of spine conditions (rather than estimate all use or expenditures), including only those visits made for a primary diagnosis of spine conditions provides a more direct comparison across the health services we examined.
Sociodemographic and Health Status Data
We examined sociodemographic data for individuals who had reported an ambulatory visit to a US provider for a primary diagnosis of a spine condition in 1999 and 2008 including: age, gender, race/ethnicity, healthcare insurance type, and education. To determine whether the health status of respondents who reported use of ambulatory health services changed over the 10-year time period, we examined self-reported health status measures. Since self-reported health status has been shown to be a strong predictor of health and mortality,11 we used this as our primary measure of respondent health status and collapsed this variable into “excellent,” “very good, or good” and “fair or poor.” We also determined the percentage of respondents with “any functional limitation” which is based on a combination of both physical and cognitive limitations collected by the MEPS.
Beginning in 2000 the MEPS collected information on body mass index (BMI), smoking status, and SF-12 scores. We determined the percentage of respondents who were obese (BMI ≥ 30 kg/m2) and who smoked, and we calculated the mean Physical and Mental Composite Summary12 from 2000 to 2008 (Appendix Table 2). To make data comparable across the study time period, we converted Physical and Mental Composite Summary scores for MEPS calendar years 2000 and 2001, during which time the MEPS used version 1, to version 2 scores, using standard methods.13
For measures that were acquired multiple times per year, we used the last measurement of the corresponding calendar year.
Analyses
To estimate expenditures on ambulatory visits for spine conditions, we converted all healthcare expenditure data to 2008 dollars using the Consumer Price Index (CPI) for professional medical services provided by the US Bureau of Labor Statistics.14 To determine whether the type of adults visiting providers changed over the ten-year study period, we performed univariate analyses comparing characteristics of respondents with spine conditions from 1999 to 2008 using a t-test for mean comparisons and a χ2 test for comparisons of proportions. To examine potential trends in mean annual expenditure per user from 1999 to 2008, we used linear regression adjusted for age, gender, healthcare insurance coverage, and other covariates. Specifically, we examined the statistical significance for the coefficient for year (as a categorical variable) in our linear regression models to test for trend.
We used complex survey design methods to generate all descriptive analyses (including national estimates, standard errors, and 95% confidence intervals) of the datasets using STATA version 11.1 statistical software (College Station, Texas), which account for a respondent’s probability of selection and sampling methodology.
Results
According to our estimates, in 1999, 11.9 million adults had an ambulatory visit for a primary diagnosis of a spine condition (Table 1). This number increased approximately 15% over the study period to 13.6 million in 2008; however, with population growth, the proportion of all US adults reporting a visit for a primary diagnosis of a spine condition remained constant at approximately 6%. The amount of overlap use of healthcare services among adults with spine conditions was remarkably stable over the ten year time period (84-86% used only one service, 13-14% used two different services, and 1-2% used all three of the ambulatory services we examined).
Table 1.
The Characteristics of US Adults with and without Spine Conditions in 1998 and 2008
| 1999 | 2008 |
P-value for Difference between Adults with Spine Conditions 1999 to 2008c |
|||||
|---|---|---|---|---|---|---|---|
| Spine Conditions |
No Spine Conditions |
P-valueb,c | Spine Conditions |
No Spine Conditions |
P-valueb,c | ||
| No. of MEPS Respondents (sample) | 941 | 16,457 | 1,110 | 22,269 | |||
| Projected National Estimates | |||||||
| No. of US adults (millions) | 11.9 | 192.0 | 13.6 | 216.8 | |||
| % of US adult population | 5.8 | 94.2 | 5.9 | 94.1 | |||
| US Region (%) | |||||||
| Northeast | 19.0 | 20.9 | 18.5 | 16.3 | |||
| Midwest | 22.6 | 25.3 | 0.17 | 21.4 | 30.0 | <0.001 | 0.03 |
| South | 35.9 | 33.9 | 37.0 | 28.1 | |||
| West | 22.5 | 19.9 | 23.0 | 25.6 | |||
| Sociodemographic Characteristics | |||||||
| Age (mean) | 44.9 | 47.7 | <0.001 | 46.0 | 49.9 | <0.001 | 0.03 |
| % female | 51.9 | 58.0 | 0.01 | 51.2 | 56.4 | 0.01 | 0.53 |
| Race/Ethnicity (%) | |||||||
| Hispanic | 10.8 | 5.7 | 14.1 | 5.9 | |||
| Non-Hispanic White | 73.2 | 86.7 | <0.001 | 67.3 | 83.8 | <0.001 | 0.06 |
| Non-Hispanic Black or African American | 11.9 | 5.4 | 11.9 | 5.7 | |||
| Other or multiple races | 4.1 | 2.2 | 6.7 | 4.7 | |||
| Marital status (%) | |||||||
| married | 55.6 | 63.4 | 53.5 | 59.1 | |||
| divorced, separated, or widowed | 20.1 | 21.4 | <0.001 | 20.3 | 23.4 | <0.001 | 0.28 |
| never married | 24.3 | 15.1 | 26.2 | 17.5 | |||
| Employment status (%) | |||||||
| ever unemployed (or retired) during year? | 38.5 | 37.2 | 0.55 | 42.2 | 40.5 | 0.32 | 0.24 |
| employed | 61.5 | 62.8 | 57.8 | 59.5 | |||
| Education (%) | |||||||
| high school graduate or less | 70.9 | 67.7 | 66.6 | 59.6 | |||
| some college or associate’s degree | 15.4 | 17.2 | 0.24 | 16.7 | 20.1 | 0.01 | <0.01 |
| bachelor s or graduate degree | 13.7 | 15.1 | 16.6 | 20.3 | |||
| Health Insurance Coverage (%) | |||||||
| private | 74.3 | 82.4 | 67.5 | 76.3 | |||
| public | 13.4 | 11.7 | <0.001 | 16.7 | 15.9 | <0.001 | 0.02 |
| uninsured | 12.3 | 5.8 | 15.8 | 7.8 | |||
| Health Status Measures | |||||||
| “fair” or “poor” self-reported health status (%) | 21.8 | 10.9 | <0.001 | 19.0 | 13.0 | <0.001 | 0.17 |
| any self-reported limitaion (%) | 38.7 | 22.0 | <0.001 | 41.7 | 26.4 | <0.001 | 0.28 |
| any social limitation (%) | 6.4 | 3.9 | 0.01 | 8.1 | 4.5 | <0.001 | 0.23 |
| any work, school, or home limitation (%) | 12.8 | 6.6 | <0.001 | 15.4 | 8.4 | <0.001 | 0.14 |
| any limitation in physical functioning (%) | 16.7 | 8.3 | <0.001 | 23.7 | 11.4 | <0.001 | <0.01 |
Abbreviations: MEPS, Medical Expenditure Panel Survey
No. of MEPS respondents includes adult (age ≥ 18 years) who were inscope and reported an ambulatory visit for primary ICD-9-CM condition related to spine conditions
P-values compare those adults with Spine Conditions to those No Spine Conditions
t-test used in comparison of means and χ2 statistic used in comparison of proportions
Ambulatory Visits
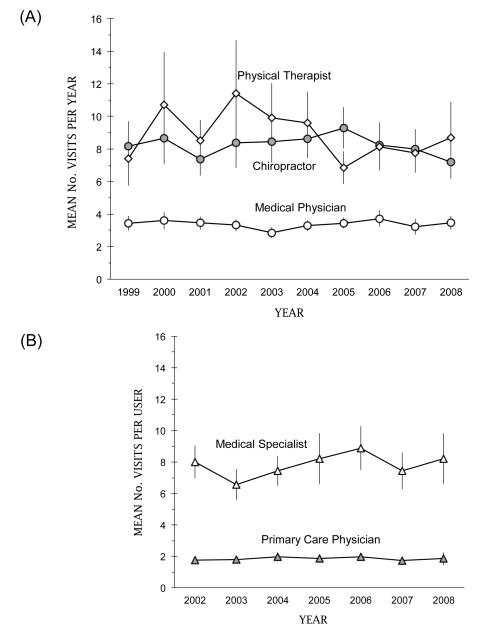
The mean number of ambulatory visits to medical physicians for a primary diagnosis of a spine condition fluctuated between approximately 2.9 and 3.7 visits per year from 1999 to 2008 (Figure 1A). The mean number of visits for chiropractic fluctuated between 7.2 and 9.3 visits per year. We found the most variability in service use among adult users of physical therapy, with the mean number of visits per year ranging between a high of 11.4 in 2002 to a low of 6.8 in 2005; nevertheless, the differences we saw were not statistically significant.
Figure 1.
(A) Mean Number of Annual Ambulatory Visits per User to US Medical Physicians, Physical Therapists, and Chiropractors from 1999 to 2008 for Spine Conditions and (B) Mean Number of Annual Ambulatory Visits to Medical Physicians according to Specialty from 2002 to 2008 for Spine Conditions
The mean number of annual visits per user of primary care was stable while the mean annual number of visits to specialists varied but increased from 6.6 in 2003 to 8.9 in 2006 (Figure 1B).
Annual Expenditures on Ambulatory Health Services
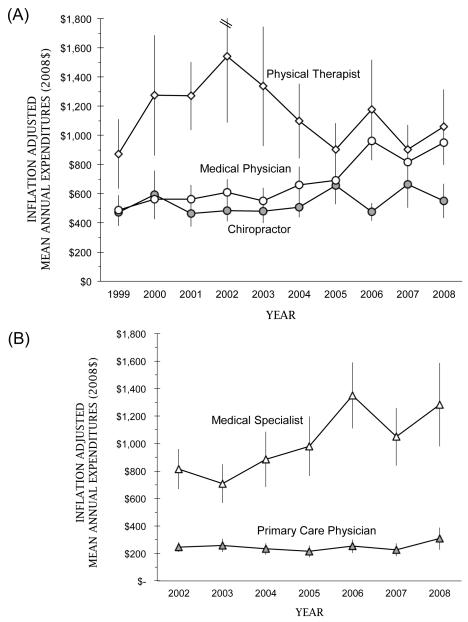
We found inconsistent trends in expenditures per user across the health services we examined. The most consistent trend was observed for expenditure on medical care (Figure 2A). Among adults who reported any expenditure on medical care for a primary diagnosis of a spine condition, the mean inflation-adjusted expenditure increased by 95% (from $487 in 1999 to $950 in 2008). We found a contraction in expenditures on medical care in 2007 and 2008, possibly due to the coinciding economic recession.15 For chiropractic care, the mean expenditure varied much less, fluctuating between a low of $473 in 1999 and a high of $662 in 2007. The annual inflation-adjusted mean expenditure per user on physical therapy peaked in 2002 at $1,543 and apparently contracted thereafter; however, the confidence intervals for physical therapy were large, implying considerable variation in expenditures among physical therapy users.
Figure 2.
(A) Inflation-adjusted Mean Annual Expenditure per User for Ambulatory Visits to US Medical Physicians, Physical Therapists, and Chiropractors from 1999 to 2008 for Spine Conditions and (B) Inflation Adjusted Mean Annual Expenditures for Ambulatory Visits to Medical Physicians according to Specialty from 2002 to 2008 for Spine Conditions
We found significant increases in expenditures on specialty care with little change in inflation-adjusted expenditures on services provided by primary care physicians (Figure 2B).
In our linear regression models, time was predictive in explaining inflation-adjusted expenditures on medical care and chiropractic care when adjusted for sociodemographic and health status covariates (the coefficient for year in our model was 1.04 (95% CI 1.02, 1.05) for medical care and 1.02 (95% CI 1.00, 1.04) for chiropractic care for predicting an incremental increase in $100 2008 dollars) (Table 2). Across all health services we examined, having “any limitation” was strongly predictive of health spending. In particular, poorer health status (both “fair” or “poor” health status and reporting “any limitation”) was most predictive of medical care expenditures. However, interaction terms between time and health status measures were insignificant suggesting differences in patients’ health status over time do not explain expenditure trends on medical care. Being privately insured and living in an MSA was predictive of higher healthcare spending among adult users of medical and chiropractic care.
Table 2.
Linear Regression Models to Predict Annual Expenditures (2008$)a on Ambulatory Visits to US Medical Physicians, Chiropractors, and Physical Therapists for Spine Conditions
| Medical Care | Chiropractic Care | Physical Therapy | ||||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) |
P- value |
Coefficient (95% CI) |
P- value |
Coefficient (95% CI) 1,358 |
P- value |
|
| No. of MEPS Respondents in Sample | 7,647 | 4,507 | 1,358 | |||
| Yearb | 1.04 (1.02, 1.05) | <0.001 | 1.02 (1.00, 1.04) | 0.06 | 0.99 (0.96, 1.01) | 0.31 |
| Age | 1.00 (1.00, 1.00) | 0.45 | 1.00 (1.00, 1.00) | 0.72 | 1.01 (1.00, 1.01) | 0.00 |
| Gender | ||||||
| male | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| female | 0.99 (0.92, 1.06) | 0.70 | 1.16 (1.07, 1.27) | 0.00 | 1.22 (1.05, 1.41) | 0.01 |
| US Region | ||||||
| Northeast | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| Midwest | 0.90 (0.80, 1.02) | 0.09 | 0.89 (0.78, 1.03) | 0.11 | 0.94 (0.75, 1.18) | 0.61 |
| South | 0.87 (0.78, 0.97) | 0.01 | 1.02, 0.89, 1.17) | 0.81 | 0.93 (0.75, 1.15) | 0.51 |
| West | 0.91 (0.80, 1.03) | 0.15 | 0.90 (0.79, 1.03) | 0.13 | 0.82 (0.65, 1.02) | 0.08 |
| Rurality | ||||||
| Non-MSA | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| MSA | 1.03 (0.94, 1.13) | 0.46 | 1.44 (1.28, 1.61) | <0.001 | 1.03 (0.85, 1.24) | 0.79 |
| Race/Ethnicity | ||||||
| Hispanic | 1.01 (0.88, 1.16) | 0.89 | 0.98 (0.78, 1.23) | 0.87 | 0.73 (0.55, 0.98) | 0.04 |
| Non-Hispanic White | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| Non-Hispanic Black or African American | 0.96 (0.85, 1.08) | 0.46 | 1.18 (0.94, 1.47) | 0.15 | 1.02 (0.78, 1.34) | 0.87 |
| Other or multiple races | 0.89 (0.74, 1.08) | 0.24 | 1.25 (0.99, 1.59) | 0.06 | 1.23 (0.86, 1.75) | 0.27 |
| Marital status | ||||||
| married | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| divorced, separated, or widowed | 0.95 (0.87, 1.04) | 0.30 | 1.03 (0.92, 1.16) | 0.57 | 0.97 (0.81, 1.15) | 0.71 |
| never married | 0.94 (0.83, 1.07) | 0.36 | 1.02 (0.89, 1.17) | 0.78 | 1.07 (0.84, 1.35) | 0.59 |
| Employment status | ||||||
| employed | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| ever unemployed (or retired) during year | 1.03 (0.94, 1.13) | 0.56 | 1.00 (0.90, 1.09) | 0.92 | 0.92 (0.77, 1.11) | 0.38 |
| Education | ||||||
| high school graduate or less | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| some college or associate's degree | 1.05 (0.94, 1.18) | 0.37 | 1.06 (0.94, 1.19) | 0.33 | 0.88 (0.71, 1.10) | 0.27 |
| bachelor’s or graduate degree | 1.11 (1.01, 1.23) | 0.04 | 1.04 (0.93, 1.17) | 0.49 | 0.99 (0.82, 1.19) | 0.91 |
| Health Insurance Coverage | ||||||
| private | 1.36 (1.18, 1.57) | <0.001 | 1.21 (1.03, 1.43) | 0.20 | 1.02 (0.66,1.57) | 0.95 |
| public | 1.06 (0.90, 1.25) | 0.46 | 0.97 (0.79, 1.18) | 0.74 | 0.66 (0.41, 1.05) | 0.08 |
| uninsured | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| Any Limitation | ||||||
| No | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| Yes | 1.52 (1.40, 1.65) | <0.001 | 1.21 (1.10, 1.34) | <0.001 | 1.23 (1.06, 1.42) | 0.07 |
| Self-reported Health Status | ||||||
| Excellent, Very Good, or Good | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | |||
| Fair or Poor | 1.36 (1.23, 1.50) | <0.001 | 1.06 (0.94, 1.20) | 0.34 | 1.12 (0.92, 1.36) | 0.25 |
Abbreviations: MEPS, Medical Expenditure Panel Survey; CI, Confidence Interval
Linear regression models predict annual expenditures in hundreds (2008$, log transformed)
Test of trend (Year included in models as a categorical variable)
Discussion
We used the MEPS to examine expenditures on common ambulatory health services for the management of spine conditions between 1999 and 2008. According to our estimates, the total annual expenditures on medical care for the management of spine conditions has grown significantly in recent years while expenditures on chiropractic care and physical therapy have not experienced the same growth. Our study suggests that this growth in medical care is due primarily to increases in expenditures on specialty care services (expenditures on primary care physician services were remarkably stable over the ten years we examined). Consistent with previous reports,4,5 we also found that the health status of adults with a primary diagnosis of a spine condition has not improved despite increasing costs over time.
The information provided by our study is particularly important for examining the effects of health policy decisions that aim to control cost. The effects of health policy decisions pertaining to reimbursement of health services for spine condition management have observable effects over time. For example, our analyses on the per user level suggest stability in expenditures on health services such as chiropractic care.8 From 2005 to 2007 the Centers for Medicare and Medicaid Services’ (CMS) Office of Research Development and Information conducted a study to examine the economic impacts of expansion of reimbursable services (i.e. coverage of diagnostic and examination) treatment of neuromuscular conditions by chiropractors and concluded that such expansion would result in higher costs.16 The stability in expenditures on chiropractic care is likely due to health policy decisions to limit chiropractors’ reimbursable practices whereas medical specialists rely more heavily on reimbursable advanced technologies (which are more subject to increased expenditures).
There are important decisions on the horizon regarding the US healthcare system pertaining to cost and cost-effectiveness of health services. Our findings imply that medical care, specifically specialty care, rather than primary care, chiropractic care, or physical therapy, is responsible for rising ambulatory care costs for spine conditions. Increases in expenditures on specialty care are likely influenced by collaborative markets such as producers of medical supplies as well as the growth in technological dependence overall, while physical therapy and chiropractic care are less influenced by technologically-based innovations.18 In addition, resistance to shrinking reimbursement from third party sources among larger groups with more leverage such as medical specialists may partially explain the trends we observed.17 While our study did not explicitly consider the relative effectiveness of different health services (which is likely dependent on the specific spine condition), our findings do imply that strategies aimed at reducing dependency on specialty care would mitigate national spending on spine conditions. In light of some evidence that specialists provide services that could be performed in a primary care setting,19, 20 national efforts to substitute primary care for management by specialists may have cost-containment benefits for this population.
To inform overall value and future health policy decisions, it will be critical to determine the relative effectiveness of these different health services as our analyses clearly demonstrate differences in expenditures.
Study Limitations
Our study has several limitations that must be acknowledged. First, we investigated only treatment patterns, utilization, and expenditures for common health services among non-institutionalized US adult (≥ 18 years) citizens. Including inpatient services and expenditures on pharmaceuticals would significantly increase our estimates on medical care, and findings for children or institutionalized adults may differ. Second, the MEPS data on healthcare utilization and expenditures are self-reported by patients, potentially causing inaccuracies; however, the MEPS attempts to correct self-reported errors by verifying response data with the respondent’s healthcare providers and healthcare insurance providers. Finally, our analyses did not separate expenditures on diagnostic procedures from expenditures on consultations—differences in the location where services were provided (i.e. office-based versus outpatient) among health services could have affected our results. We did perform all analyses excluding ambulatory visits that included a diagnostic procedure and while the overall expenditures dropped slightly, trends in expenditures among specific ambulatory services were unaffected.
Despite the inherent limitations of our study, our findings offer important information regarding expenditures on health services for spine conditions. Therefore our findings will help inform future studies that examine the relative cost-effectiveness these services. Health policy makers should consider these finding when developing national strategies to manage the large population of Americans with spine conditions.
Key Points.
It is well known that national expenditures on spine conditions have increased in recent years in the absence in improvement in the health status of the spine condition population.
Among the most common ambulatory health services that manage spine conditions, expenditures on medical care has increased mostly due to expenditures related to providing specialty care.
Non-technologically based ambulatory health services that manage spine conditions such as chiropractic care and physical therapy have not experienced the same increases in expenditures per user.
Future health policy decisions must be informed by the relative cost-effectiveness of ambulatory health services that manage the spine condition population.
Mini Abstract.
We used the Medical Expenditure Panel Survey to examine expenditures on health services that manage back and neck conditions from 1999 to 2008. Recent increasing costs associated with providing medical care for back and neck conditions (particularly subspecialty care) are contributing to the growing economic burden of managing these conditions.
Acknowledgments
Funding and Disclaimer
The manuscript submitted does not contain information about medical device(s)/drugs(s). NIH grant funds were received to support this work. One or more of the author(s) has/have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this manuscript: e.g., honoraria, gifts, consultancies, royalties, stocks, stock options, decision making position.
Appendix 1. The ICD-9-CM Diagnosis Codes used in this study to identify Ambulatory Visits for Spine Conditions
| Percent of Ambulatory Visits for Spinal Conditions in 2008 |
|||||
|---|---|---|---|---|---|
| ICD-9-CM Code | Description | All | Medical Care |
Chiropractic Care |
Physical Therapy |
| 720 | Ankylosing spondylitis and other inflammatory spondylopathies | 0.0 | 0.1 | 0.0 | 0.0 |
| 721 | Spondylosis and allied disorders | 2.1 | 1.5 | 2.7 | 2.4 |
| 722 | Intervertebral disk disorders | 18.7 | 19.7 | 15.1 | 27.0 |
| 723 | Other disorders of the cervical spine region | 10.7 | 8.1 | 12.4 | 11.3 |
| 724 | Other and unspecified disorders of the back | 53.1 | 56.0 | 54.1 | 40.9 |
| 724.0 | Spinal stenosis, other than of cervical spine | ||||
| 724.1 | Pain in thoracic spine | ||||
| 724.2 | Lumbago | ||||
| 724.3 | Sciatica, excluding lesion | ||||
| 724.4 | Thoracic or lumbosacral neuritis or radiculitis | ||||
| 724.5 | Backache, unspecified | ||||
| 724.6 | Disorders of sacrum | ||||
| 724.7 | Disorders of coccyx | ||||
| 724.8 | Other symptoms referable to back | ||||
| 724.9 | Other unspecified back disorders | ||||
| 737 | Curvature of spine | 2.8 | 2.1 | 3.3 | 3.9 |
| 805 | Fracture of vertebral column without mention of spinal cord injury | 1.0 | 1.2 | 1.0 | 0.3 |
| 806 | Fracture of vertebral column with spinal cord injury | 0.0 | 0.0 | 0.0 | 0.0 |
| 839 | Other, multiple, and ill-defined dislocations of spine | 3.9 | 3.3 | 6.1 | 0.0 |
| 846 | Sprains and strains of sacroiliac region | 0.7 | 0.6 | 0.3 | 2.2 |
| 847 | Sprains and strains of other and unspecified parts of back | 7.0 | 7.4 | 5.2 | 12.1 |
Abbreviations: ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification
Appendix 2. The Health Status of US Adults with Spine Conditions from 1999 to 2008
| Mean or % (95% Confidence Interval) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
| No. MEPS Respondentsa | 941 | 944 | 1,286 | 1,607 | 1,419 | 1,490 | 1,512 | 1,535 | 1,274 | 1,110 |
| Estimated No. Adults (millions) | 11.9 | 11.7 | 12.9 | 14.2 | 15.3 | 16.0 | 16.9 | 16.7 | 14.7 | 13.6 |
| Any Limitation (%) | 38.7 (34.7,42.7) |
38.2 (34.7,41.7) |
41.8 (38.5,45.1) |
44.8 (41.6,48.1) |
45.5 (42.1,48.9) |
45.9 (42.8,49.0) |
45.8 (42.5,49.0) |
43.7 (40.4,47.1) |
43.9 (40.6,47.2) |
41.7 (38.2,45.1) |
| Any social limitation (%) | 6.4 (4.3,6.3) |
9.5 (7.2,11.8) |
8.9 (7.1,10.7) |
9.1 (7.4,10.8) |
12.0 (10.0,14.1) |
13.2 (11.2,15.2) |
11.3 (9.4,13.1) |
9.0 (7.3,10.6) |
9.7 (7.8,11.6) |
8.1 (6.1,10.1) |
| Any work, school, or home limitation (%) | 12.8 (10.3,15.3) |
15.7 (13.2,18.2) |
16.9 (14.4,19.5) |
17.0 (14.7,19.2) |
18.3 (15.9,20.8) |
18.7 (16.5,20.9) |
18.1 (16.0,20.1) |
15.7 (13.6,17.8) |
16.1 (13.8,18.3) |
15.4 (12.9,18.0) |
| Any limitation in physical functioning (%) | 16.7 (13.8,19.6) |
19.1 (16.5,21.8) |
23.8 (20.9,26.7) |
24.3 (21.6,27.0) |
25.9 (23.1,28.7) |
25.1 (22.5,27.8) |
25.0 (22.5,27.6) |
22.0 (19.2,24.8) |
24.3 (21.4,27.2) |
23.7 (20.7,26.7) |
| Summary Score (mean)b | ||||||||||
| PCS | -- | 44.5 (43.5,45.5) |
44.6 (43.8,45.5) |
45.2 (44.5,45.9) |
44.2 (43.4,45.0) |
44.0 (43.3,44.7) |
44.2 (43.4,45.0) |
44.3 (43.6,45.0) |
44.3 (43.5,45.1) |
44.9 (44.0,45.9) |
| MCS | -- | 49.9 (49.1,50.7) |
50.5 (49.9,51.1) |
49.3 (48.7,50.0) |
49.7 (49.1,50.3) |
49.5 (48.8,50.1) |
49.9 (49.3,50.5) |
49.8 (49.3,50.4) |
50.3 (49.6,51.0) |
50.2 (49.5,51.0) |
| “Fair” or“ Poor” Self-reported Health Status (%) | 21.8 (18.8,24.8) |
19.6 (16.4,22.7) |
21.0 (18.5,23.6) |
21.2 (18.7,23.6) |
21.8 (19.3,24.4) |
22.8 (20.4,25.2) |
21.1 (18.6,23.6) |
19.0 (16.8,21.2) |
18.9 (16.6,21.2) |
19.0 (16.4,21.7) |
| Obese (body mass index ≥ 30.0kg/m2) (%) | -- | 23.3 (19.9,26.7) |
23.1 (20.1,26.1) |
27.3 (24.5,30.1) |
28.3 (25.4,31.2) |
29.7 (27.0,32.4) |
30.6 (27.9,33.4) |
31.4 (38.9,34.0) |
30.4 (27.6,33.2) |
32.9 (29.8,35.9) |
| Smoking Status (%) | -- | 21.6 (17.5,25.7) |
21.8 (19.1,24.4) |
20.0 (17.6,22.3) |
24.6 (21.9,27.3) |
20.9 (18.1,23.8) |
19.0 (16.8,21.3) |
20.3 (18.0,22.6) |
17.7 (15.1,20.3) |
17.6 (14.6,20.6) |
Abbreviations: MEPS, Medical Expenditure Panel Survey; PCS, Physical Composite Summary; MCS, Mental Composite Summary
No. of MEPS respondents includes adult (age ≥ 18 years) who were inscope and reported an ambulatory visit for primary ICD-9-CM condition related to the spine
PCS and MCS scores range from 0-100 with higher scores indicating better functioning. PCS and MCS version 1 scores (MEPS years 2000 and 2001) were converted to version 2 scores (MEPS years 2003-2008).
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Koes BW, van Tulder MW, Ostelo R, Kim Burton A, Waddell G. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine (Phila Pa 1976) 2001;26(22):2504–2513. doi: 10.1097/00007632-200111150-00022. discussion 2513-2504. [DOI] [PubMed] [Google Scholar]
- 2.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581–585. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 3.Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine (Phila Pa 1976) 1995;20(1):11–19. doi: 10.1097/00007632-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299(6):656–664. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 5.Martin BI, Turner JA, Mirza SK, Lee MJ, Comstock BA, Deyo RA. Trends in Health Care Expenditures, Utilization, and Health Status Among US Adults With Spine Problems, 1997-2006. Spine (Phila Pa 1976) 2009;34:2077–2084. doi: 10.1097/BRS.0b013e3181b1fad1. [DOI] [PubMed] [Google Scholar]
- 6.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Cherkin DC, Deyo RA, Volinn E, Loeser JD. Use of the International Classification of Diseases (ICD-9-CM) to identify hospitalizations for mechanical low back problems in administrative databases. Spine (Phila Pa 1976) 1992;17(7):817–825. doi: 10.1097/00007632-199207000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Davis MA, Sirovich BE, Weeks WB. Utilization and expenditures on chiropractic care in the United States from 1997 to 2006. Health Serv Res. 2010;45(3):748–761. doi: 10.1111/j.1475-6773.2009.01067.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Medical Expenditure Panel Survey [Accessed March 5, 2011];Agency for Health Care Policy and Research, Household Component Full Year Files. 2008 http://www.meps.ahrq.gov/mepsweb/data_stats/download_data_files.jsp.
- 10.Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976) 2004;29(1):79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 11.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ware J, Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Ware JE, Kosinksi M, Turner-Bowker DM, Gandek B. How to Score Version 2 of the SF-12 (r) Health Survey. Quality Metrics Inc.; Lincon, RI: 2002. [Google Scholar]
- 14.United States Bureau of Labor Statistics [Accessed September 5, 2011];Consumer Price Index. http://www.bls.gov/cpi.
- 15.Martin A, Lassman D, Whittle L, Catlin A. Recession contributes to slowest annual rate of increase in health spending in five decades. Health Aff (Millwood) 2011;30(1):11–22. doi: 10.1377/hlthaff.2010.1032. [DOI] [PubMed] [Google Scholar]
- 16.Statson WB, Shepard DS, Ritter G, Tompkins C. Analysis of buget neutrality of the demonstration of coverage of chiropractic services under Medicare. 2009. [Google Scholar]
- 17.Robinson JC. Hospital market concentration, pricing, and profitability in orthopedic surgery and interventional cardiology. Am J Manag Care. 2011;17(6 Spec No.):e241–248. [PubMed] [Google Scholar]
- 18.Meeker WC, Haldeman S. Chiropractic: a profession at the crossroads of mainstream and alternative medicine. Ann Intern Med. 2002;136(3):216–227. doi: 10.7326/0003-4819-136-3-200202050-00010. [DOI] [PubMed] [Google Scholar]
- 19.Starfield B, Chang HY, Lemke KW, Weiner JP. Ambulatory specialist use by nonhospitalized patients in us health plans: correlates and consequences. J Ambul Care Manage. 2009;32(3):216–225. doi: 10.1097/JAC.0b013e3181ac9ca2. [DOI] [PubMed] [Google Scholar]
- 20.Valderas JM, Starfield B, Forrest CB, Sibbald B, Roland M. Ambulatory care provided by office-based specialists in the United States. Ann Fam Med. 2009;7(2):104–111. doi: 10.1370/afm.949. [DOI] [PMC free article] [PubMed] [Google Scholar]