Abstract
Background
External beam radiotherapy (EBRT) for retinoblastoma has traditionally been done with conventional radiotherapy techniques which resulted high doses to the surrounding normal tissues.
Case report
A 20 month-old girl with group D bilateral retinoblastoma underwent intensity modulated radiotherapy (IMRT) to both eyes after failing chemoreduction and focal therapies including cryotherapy and transpupillary thermotherapy. In this report, we discuss the use of IMRT as a method for reducing doses to adjacent normal tissues while delivering therapeutic doses to the tumour tissues compared with 3-dimensional conformal radiotherapy (3DCRT). At one year follow-up, the patient remained free of any obvious radiation complications.
Conclusions
Image guided IMRT provides better dose distribution than 3DCRT in retinoblastoma eyes, delivering the therapeutic dose to the tumours and minimizing adjacent tissue damage.
Keywords: retinoblastoma, radiotherapy, intensity modulated radiotherapy
Introduction
Retinoblastoma is the most common intraocular malignant tumour encountered in children. In most patients, retinoblastoma remains confined to the eye. However, in advanced cases, retinoblastoma can secondarily invade the orbit and metastasize to the central nervous system and other distant organs. Untreated retinoblastoma is nearly always fatal. Therefore, the early diagnosis and treatment is critical in saving lives of retinoblastoma patients and preserving a visual function of the affected eyes. Retinoblastoma occurs with an estimated frequency of 1/14000–1/34000 live births.1 In the United States, approximately 200 to 300 new cases are diagnosed each year. About 2/3 of the patients have unilateral and 1/3 have bilateral disease. More than 90% of the patients are diagnosed before the age of 5 years.2 Bilateral patients are generally discovered in the first year of life and unilateral ones are diagnosed later in the second year.1,3
Chemoreduction has changed the approach to the management of retinoblastoma. The dogma of enucleating the worse eye and irradiating the least affected eye in bilateral disease has largely been replaced by chemoreduction as a first step for both eyes. For the unilateral retinoblastoma chemoreduction is appropriate for those with Group A to C disease, but much less successful for those children with Group D or E retinoblastoma, which is usually treated by enucleation.
External beam radiation therapy (EBRT) is used less often today. It is used for moderately advanced tumours, multiple tumours, especially those with vitreous or subretinal seeds that fail chemoreduction. The external beam radiation dose is 35–45 Gy delivered over 4–5 weeks. An anterior lens-sparing, relative lens-sparing or modified lateral beam technique can be used. The anterior lens-sparing technique compared to the modified lateral beam technique leads to a higher tumour recurrence rate because the anterior retina is undertreated. On the other hand, the relative lens-sparing and modified lateral beam techniques yield similar eye conservation rates with subsequent salvage therapy. Much higher doses (from 50 Gy to 100 Gy) have been used in the past decades and it is quite possible that some second cancers have been due to the high radiation dose. The external beam radiation therapy can lead to significant complications such as facial hypoplasia from orbital bone atrophy, radiation cataract, and retinopathy.
The aim of this study was to compare the dose distribution of intensity modulated radiotherapy (IMRT) with the conventional external beam radiotherapy in terms of target and normal tissue doses in a recurrent bilateral retinoblastoma patient.
Case report
An 8 month-old girl was referred to the Department of Ophthalmology, Ankara University Faculty of Medicine with the complaint of strabismus in the left eye. The examination under anaesthesia revealed bilateral group D retinoblastoma in both eyes. There was an exudative retinal detachment in both eyes with extensive subretinal seeds. There was no evidence of systemic involvement on bone marrow biopsy, spinal tap, and cranial MRI. The patient was initially treated with 6 cycles of intravenous carboplatin, etoposide and vincristine chemotherapy. Initially, the tumours in both eyes responded well to chemotherapy with resolution of SRF. The patient received several cryotherapy and transpupillary thermotherapy applications to recurrent and new tumours in both eyes over a period of approximately 12 months. However, the massive recurrence developed both eyes at 12 month follow-up and it was felt that either EBRT or enucleation was necessary at this point. The family opted for EBRT. The patient was seen in the Department of Radiation Oncology, Acibadem University, Istanbul for IMRT. A thermoplastic mask was prepared for the immobilization under anaesthesia and thereafter she underwent Computerized Tomography (CT) imaging with 1-mm slices for treatment planning purposes. Target tumour volumes and organs at risk (OAR) such as orbital bone, cornea, lens, lacrimal gland and optic nerve were delineated.
Gross tumour volume (GTV)4 dose was not specified in this case, only the recurrent tumours in both eyes were delineated as tumour in order to not to lower the dose in those areas; clinical tumour volume (CTV) was defined as both right and left retina and planning target volume (PTV) was generated from CTV plus 1 mm margin. Dose to OAR was defined according to previously reported data.5–9
Comparison of 3DCRT and IMRT
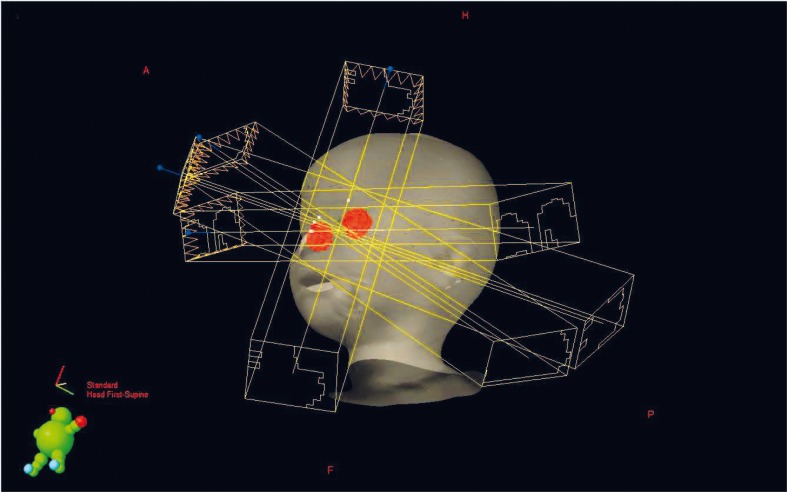
In order to provide dose constraints for OAR we performed 4 different IMRT plans and a conformal plan. Of these IMRT plans the best isodose distribution and the dose volume histogram were provided with a noncoplanar 4-field technique (Figure 1); when compared to a conformal plan there was no significant difference for cornea, lens and optic nerve doses. The patient was treated with 4-field noncoplanar IMRT plan to a total dose of 40 Gy, 2 Gy per fraction under general anaesthesia. According to our department’s image guided radiotherapy (IGRT) protocol, daily kilovoltage images were taken from anteroposterior and lateral fields before each treatment and corrections were done by matching pretreatment images with digitally reconstructed radiographs.
FIGURE 1.
Four-field noncoplanar IMRT plan
Radiation doses to the orbital bones and lacrimal glands were apparently lower while the tumour dose was higher in the IMRT plan. As a result of using multiple non coplanar beams; there were low dose areas in brain, brainstem and hypophysis with IMRT plan whereas no dose with 3DCRT, but these doses were below 5 Gy which was a safe dose for the affected areas. The comparison of doses between conformal and IMRT plan is detailed in Table 1.
Table 1.
Comparison of doses for 3DCRT and IMRT plan of our patient
|
3DCRT
|
IMRT
|
|||||
|---|---|---|---|---|---|---|
| Mean (cGy) | Max. (cGy) | Vol/dose | Mean (cGy) | Max. (cGy) | Vol/dose | |
| R. Lens | 3304 | 3676 | 2763 | 3134 | ||
| L. Lens | 2657 | 3299 | 2639 | 3270 | ||
| R. Cornea | 3228 | V26.5<78% | 2609 | V26.5<70.6% | ||
| L. Cornea | 2874 | V26.5<67% | 2909 | V26.5<50.6% | ||
| R. Optic nerve | 3830 | 4147 | ||||
| L. Optic nerve | 3841 | 4063 | ||||
| R. Lac. Gland | 3807 | V34<99% | 2527 | V34<5% | ||
| L. Lac. Gland | 3741 | V34<100% | 2456 | V34<0% | ||
| Orbital Bones | 2204 | V20<56.8% | 1965 | V20<49.7% | ||
V20 (volume received above 20 Gy), V34 (volume received above 34 Gy), V26.5 (volume received above 26.5 Gy)
At one year follow-up, the patient remained free of any obvious radiation complications.
Discussion
Retinoblastoma is a radiosensitive tumour. There is a wide spectrum of techniques used for retinoblastoma ranging from single fields to complex fields such as anterior lens sparing technique, lateral oblique fields, multiple non coplanar arcs, single anterior electron fields, stereotactic radiotherapy, conformal and intensity modulated radiotherapy plans. Even protons were used to perform homogeneous dose coverage of retina while sparing the lens and bony anatomy.5,10–13 IMRT for retinoblastoma was first reported by Krasin et al.5 Subsequently, Reisner et al. published a comparative analysis of external radiotherapy techniques with IMRT in a case report of unilateral retinoblastoma.8 Previous reports on IMRT planning for retinoblastoma revealed greater sparing of the surrounding bony orbit and lacrimal gland as in our study.
High doses affecting bony orbital structures may cause growth arrest of orbital fossa and facial asymmetry.7 IMRT leads to lower doses in orbital bones, while not reducing retinal doses. In our bilateral IMRT plan, doses in both orbital bones were higher when compared to unilateral cases of Reisner et al.8 These relatively high doses can be explained by the location of recurrent tumours; which were in the posterior poles of both eyes. Plans were done in order to have an optimal dose in these regions. In cases where the tumour is located medially or anteriorly, a lower dose may be delivered to the orbital bones using IMRT.
Dry-eye syndrome, because of lacrimal gland exposure to radiation, is also another important and irreversible complication for this patient group threatening life quality. One of the main advantages of IMRT is to reduce lacrimal gland dose without lowering retinal doses. Our patient’s mean lacrimal gland doses were less than 30Gy. Dry eye is quite unlikely to develop with these radiation doses as reported by Parson et al.6
The optic nerve is also affected in the radiotherapy of retinoblastoma. Doses exceeding 54 Gy may lead to the development of radiation optic neuropathy leading to irreversible visual impairment. Reisner et al. reported maximum doses as high as 48 Gy for the optic nerve dose with several techniques including their IMRT planning.8 In our setting the optic nerve received a maximum dose of 40–41 Gy which is a safe dose for optic neuropathy. The reduction in the optic nerve dose may prevent visual problems in the future life of the patient.
Corneal injury after EBRT has also been reported previously. The critical dosage was considered 50 Gy as the 50% risk at 5 years for cornea.14 Reisner et al. considered V26.5 for the evaluation of corneal injury probability based on the study of Jiang et al.9,10 Our plan delivered less than 50 Gy to the cornea region (mean dose for right and left cornea was 32 Gy and 28.7 Gy respectively) but the V26.5 dose was relatively higher especially on the right side, where a tumour was located more anteriorly.
The lens is the most radiosensitive tissue in the eye.15 Lens preservation was always been an important target in radiotherapy planning for the treatment of tumours around the eye region. Doses exceeding 12 Gy usually results cataract. Lens sparing techniques with EBRT also caused cataract in 28% of patients.16 However, a good outcome after the cataract surgery with phacoemulsification was reported even in young ages.17 Therefore, we preferred to achieve therapeutic doses in the entire to avoid the recurrence of the tumour rather than delivering subtherapeutic doses to the retina in an effort to preserve the lens from the cataract development.
Technologic developments improved outcomes enormously in the last 10 years for EBRT. The capability of protecting normal tissue around tumour became available. IMRT with image guidance, so called IGRT-IMRT, is the superior technique that allows us to do the best and safe treatment. Outcomes of IMRT were successful with the more common cancers including prostate, head and neck, breast cancers in terms of the increased local control and normal tissue protection. Even with lung cancer, where a significant organ and tumour movement may be a problem in radiotherapy, IMRT proved to be successful. The outcomes of IMRT in rarer tumours such as retinoblastoma are not widely known because of the paucity of publications in this area.
It has been concluded that any genotoxic therapy can induce second neoplasms after long latent times and the risk is slightly higher with radiotherapy but the side effects of radiotherapy have less impact on the patients’ quality of life when compared with other therapies.18 In the pediatric setting the risk could be significant due to a higher inherent susceptibility of tissues. However, as the risk of secondary cancers as sarcomas, related with IMRT estimated to be 2% compared with 1% for 3DCRT, the use of protons became actual to reduce risk of radiation-induced carcinogenesis.19 The efficacy of IMRT in reducing the acute and late toxicity in children with nasopharyngeal carcinoma (NPC) was reported by two centres recently.20,21 Louis et al. found no difference with IMRT in terms of late toxicity such as hypothyroidism, xerostomia, hearing loss, and dental disease.20 On the other hand Laskar et al. concluded that IMRT significantly reduces and delays the onset of the acute toxicity compared to EBRT, resulting in the improved tolerance and treatment compliance for children with NPC.21 However, the number of studies with IMRT in pediatric tumours was very limited and other centre experience should be awaited.
In conclusion; image guided IMRT provides better dose distribution than 3DCRT in retinoblastoma eyes, delivering the therapeutic dose to the tumours and minimizing adjacent tissue damage. In terms of avoiding radiation complications including dry eye syndrome, facial deformity, cataract, radiation retinopathy and radiation papillopathy, IMRT planning should always be taken into consideration for patients that are referred for radiotherapy.
References
- 1.Halperin EG, Kirkpatrick JP. Retinoblastoma. In: Halperin EG, Constine LS, Tarbell NJ, Kun LE, editors. Pediatric Radiation Oncology. 4th edition. Philadelphia: Lippincott Williams & Wilkins; 2004. pp. 135–78. [Google Scholar]
- 2.Kachanov DY, Dobrenkov KV, Shamanskaya TV, Abdullaev RT, Inushkina EV, Varfolomeeva SR, et al. Solid tumors in young children in Moscow Region of Russian Federation. Radiol Oncol. 2008;42:39–44. [Google Scholar]
- 3.McDaid C, Hartley S, Bagnall AM, Ritchie G, Light K, Riemsma R. Systematic review of effectiveness of different treatments for childhood retinoblastoma. Health Technol Assess. 2005;48:1–145. doi: 10.3310/hta9480. [DOI] [PubMed] [Google Scholar]
- 4.Stavrev P, Schinkel C, Stavreva N, Fallone BG. How well are clinical gross tumor volume DVHs approximated by an analytical function? Radiol Oncol. 2009;43:132–5. [Google Scholar]
- 5.Krasin MJ, Crawford BT, Zhu Y, Evans ES, Sontag MR, Kun LE, et al. Intensity-modulated radiation therapy for children with intraocular retinoblastoma: Potential sparing of the bone orbit. Clin Oncol. 2004;16:215–22. doi: 10.1016/j.clon.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Parsons JT, Bova FJ, Fitzgerald CR, Mendenhall WM, Million RR. Severe dry-eye syndrome following external beam irradiation. Int J Radiat Oncol Biol Phys. 1994;30:775–80. doi: 10.1016/0360-3016(94)90348-4. [DOI] [PubMed] [Google Scholar]
- 7.Eifel PJ, Donaldson SS, Thomas PRM. Response of growing bone to irradiation: A proposed late effects scoring system. Int J Radiat Oncol Biol Phys. 1995;31:1301–7. doi: 10.1016/0360-3016(94)00420-P. [DOI] [PubMed] [Google Scholar]
- 8.Reisner ML, Viégas CM, Grazziotin RZ, Santos Batista DV, Carneiro TM, Mendonça de Araújo CM, et al. Retinoblastoma-comparative analysis of external radiotherapy techniques, including an IMRT technique. Int J Radiat Oncol Biol Phys. 2007;67:933–41. doi: 10.1016/j.ijrobp.2006.09.057. [DOI] [PubMed] [Google Scholar]
- 9.Jiang GL, Tucker SL, Guttenberger R, Peters LJ, Morrison WH, Garden AS, et al. Radiation induced injury to the visual pathway. Radiother Oncol. 1994;30:17–25. doi: 10.1016/0167-8140(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 10.Blach LE, McCormick B, Abramson DH. External beam radiation therapy and retinoblastoma: long term results in the comparison of two techniques. Int J Radiat Oncol Biol Phys. 1996;35:45–51. doi: 10.1016/s0360-3016(96)85010-3. [DOI] [PubMed] [Google Scholar]
- 11.Cormack RA, Kooy HM, Bellerive MR, Loeffler JS, Petersen RA, Tarbell NJ. A stereotactic radiation therapy device for retinoblastoma using a noncircular collimator and intensity filter. Med Phys. 1998;25:1438–42. doi: 10.1118/1.598317. [DOI] [PubMed] [Google Scholar]
- 12.McCormick B, Ellsworth R, Abramson D, LoSasso T, Grabowski E. Results of external beam radiation for children with retinoblastoma: A comparison of two techniques. J Pediatr Ophthalmol Strabismus. 1989;26:239–43. doi: 10.3928/0191-3913-19890901-09. [DOI] [PubMed] [Google Scholar]
- 13.Schipper J. An accurate and simple method for megavoltage irradiation therapy of retinoblastoma. Radiother Oncol. 1983;1:31–41. doi: 10.1016/s0167-8140(83)80005-x. [DOI] [PubMed] [Google Scholar]
- 14.Constine LS, Williams JP, Morris M, Rubin P, Okunie FF. Late effects of cancer treatment. In: Chao CKS, Perez CA, Brady LW, editors. Radiation Oncology Management Decisions. 2nd edition. Philadelphia: Lippincott Williams & Wilkins; 1999. pp. 103–10. [Google Scholar]
- 15.Constine LS, Williams JP, Morris M, Rubin P, Okunieff P. Late effects of cancer treatment on normal tissues. In: Perez CA, Brady LW, Halperin CE, Schmidt-Ullrich RK, editors. Principles and practice of radiation oncology. 4th edition. Philedelphia: Lippincott Williams&Wilkins; 2004. pp. 357–90. [Google Scholar]
- 16.Foote RL, Garretson BR, Schomberg PJ, Buskirk SJ, Robertson DM, Earle JD. External beam irradiation for retinoblastoma: patterns of failure and dose-response analysis. Int J Radiat Oncol Biol Phys. 1989;16:823–30. doi: 10.1016/0360-3016(89)90502-6. [DOI] [PubMed] [Google Scholar]
- 17.Honavar SG, Shields CL, Shields JA, Demirci H, Naduvilath TJ. Intraocular surgery after treatment of retinoblastoma. Arch Ophthalmol. 2001;119:1613–21. doi: 10.1001/archopht.119.11.1613. [DOI] [PubMed] [Google Scholar]
- 18.Dörr W, Herrmann T. Second tumors after oncologic treatment. Strahlenther Onkol. 2008;184:67–72. doi: 10.1007/s00066-008-1807-5. [DOI] [PubMed] [Google Scholar]
- 19.Greco C, Wolden S. Current status of radiotherapy with proton and light ion beams. Cancer. 2007;109:1227–38. doi: 10.1002/cncr.22542. [DOI] [PubMed] [Google Scholar]
- 20.Louis CU, Paulino AC, Gottschalk S, Bertuch AA, Chintagumpala M, Heslop HE, et al. A single institution experience with pediatric nasopharyngeal carcinoma: high incidence of toxicity associated with platinum-based chemotherapy plus IMRT. J Pediatr Hematol Oncol. 2007;29:500–5. doi: 10.1097/MPH.0b013e3180959af4. [DOI] [PubMed] [Google Scholar]
- 21.Laskar S, Bahl G, Muckaden M, Pai SK, Gupta T, Banavali S, et al. Nasopharyngeal carcinoma in children: comparison of conventional and intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2008;72:728–36. doi: 10.1016/j.ijrobp.2008.01.032. [DOI] [PubMed] [Google Scholar]