Abstract
Purpose
Even though aural fullness is ubiquitous among patients presenting to otolaryngology clinics, the association between aural fullness and disease development has not yet been clearly determined.
Materials and Methods
Our study was performed on outpatients from June 2006 to February 2010 whose major complaint was "ear fullness", "aural fullness", or "ear pressure". We assessed their demographic and clinical characteristics, including sex, associated diseases, symptoms, otoscopic findings, audiology test results, and final diagnoses.
Results
Among 432 patients, 165 (38.2%) were males and 267 (61.8%) were females, with mean ages of 42±19 years and 47±17 years, respectively. Tinnitus, hearing disturbance, autophony (p<0.01) as well as nasal obstruction and sore throat (p<0.05) showed a statistically significant correlation with aural fullness. Among patients who complained of hearing fullness, tests and measures such as impedance audiometry, speech reception threshold, and pure tone audiometry generated statistically significant results (p<0.05). Ear fullness was most frequently diagnosed as Eustachian tube dysfunction (28.9%), followed by otitis media with effusion (13.4%) and chronic otitis media (7.2%). However, 13.4% of patients could not be definitively diagnosed.
Conclusion
Among patients complaining of ear fullness, Eustachian tube dysfunction, otitis media with effusion, chronic otitis media were most commonly observed. Performance of otoscopy, nasal endoscopy, the Valsalva maneuver, and additional audiological tests is necessary to exclude other diseases.
Keywords: Aural fullness, tinnitus, hearing, audiologic test, nasopharyngeal cancer
INTRODUCTION
Many patients complain of "ear pressure" or a "clogging sensation" of the ear, both of which suggest aural fullness. The underlying mechanisms of this widely overlooked symptom may involve any part of the peripheral hearing organ, from the external auditory canal to the inner ear. For instance, ear fullness is often reported in the early stages of Menière's disease1 and idiopathic sudden sensorineural hearing loss.2 Despite countless descriptions of ear diseases, only a few reports have attempted to unravel the clinical meaning of ear fullness as a chief complaint. Consequently, an objective diagnostic approach or treatment protocol for managing patients with aural fullness has yet to be developed. As a result, treatment tends to depend on a doctor's personal experience. In this study, patients in whom ear fullness was reported as a chief complaint were thoroughly investigated. Retrospective analysis was performed to investigate 1) the prevalence of aural fullness in an otolaryngology outpatient population, 2) symptoms associated with ear fullness, 3) audiological findings in individuals complaining of ear fullness and 4) identified final diagnoses.
MATERIALS AND METHODS
Patients & methods
We identified all outpatients who presented at our otolaryngology clinic between June 2006 and February 2010 with a chief complaint of "ear fullness", "aural fullness", or "ear pressure". Patients who complained of ear fullness as an associated rather than a major symptom were excluded. The final diagnoses were made by four professors of otolaryngology, each with more than 15 years of clinical experience. Cases diagnosed prior to or after the study period were also excluded. In other words, all final diagnoses were made during the study period. The average duration of patient follow-up was 4 months (range: 1 to 18 months), except for cases of nasopharyngeal cancer (range: 1 month to 10 years). From a chart review, we recorded each patient's age, sex, associated symptoms, diseases, eardrum findings, audiologic test results, and final diagnoses. The study protocol was approved by the Institutional Review Board of Kyung Hee University Medical Center.
Audiologic test
Audiological tests included otoscopic examinations, pure tone audiometry (PTA), impedance audiometry (IA), speech audiometry (SA), distortion product otoacoustic emissions (DPOAEs), auditory brainstem response (ABR), electrocochleography (ECoG), and tinnitogram. We calculated the pure tone threshold of patients with ear fullness by calculating the means of the thresholds over 500 Hz, 1 kHz, 2 kHz, and 4 kHz; patients with ear fullness on both sides were counted only once.
Statistical analyses
All data were analyzed statistically using Statistical Package for the Social Sciences (SPSS) software, version 12.0 (SPSS Inc., Chicago, IL, USA) and Microsoft Excel 2007 software. Student's t-test was used to analyze 1) age and sex, 2) pure tone threshold and sex, and 3) pure tone threshold and ear fullness. Chi-square analyses were used to assess 1) the relevance of diseases associated with ear fullness and 2) results of IA, DPOAEs, ABR, and ECoG. One way analysis of variance (ANOVA) was used to examine the relationship between ear fullness and the results of SA. p-values <0.05 were considered statistically significant.
RESULTS
Age and sex
Of the 28208 outpatients evaluated during the study period at our otolaryngology clinic, only 432 (1.53%) satisfied the inclusion criteria. Their mean age was 45±18 years. Among 432 patients, 165 (38.2%) were males and 267 (61.8%) were females, the mean ages of which were 42±19 years and 47±17 years, respectively.
Comorbidities
We found no association between laterality of aural fullness and other diseases such as diabetes mellitus, hypertension, allergic rhinitis, hepatitis, thyroid disease, cancer, migraines, depressive disorder, or chronic renal failure (p>0.05).
Associated symptoms
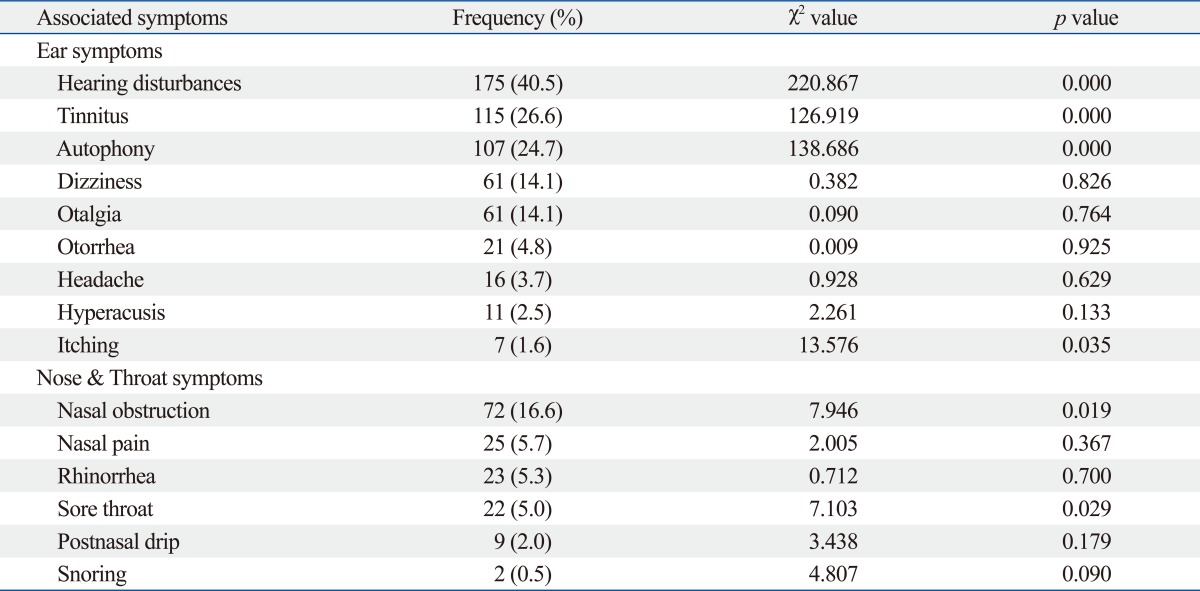
We examined the associations between ear fullness and the ear symptoms of tinnitus, hearing disturbances, dizziness, headaches, otalgia, otorrhea, itching, autophony, and hyperacusis, as well as the associations between aural fullness and the nasal symptoms of nasal obstruction, nasal pain, rhinorrhea, postnasal drip, snoring, and sore throat (Table 1). On the affected side, tinnitus, hearing disturbances, autophony were significantly related to ear fullness (p<0.001). In regards to nasal symptoms, nasal obstruction and sore throat were significantly related to bilateral ear fullness (p<0.05). Otalgia, otorrhea and hyperacusis were not significantly related to ear fullness (p>0.05).
Table 1.
Symptoms Associated with Ear Fullness
Audiologic test results
Otoscopic examination showed that the eardrums of 281 patients (65%) were normal; however, eardrum conditions were not significantly related to ear fullness (p=0.188).
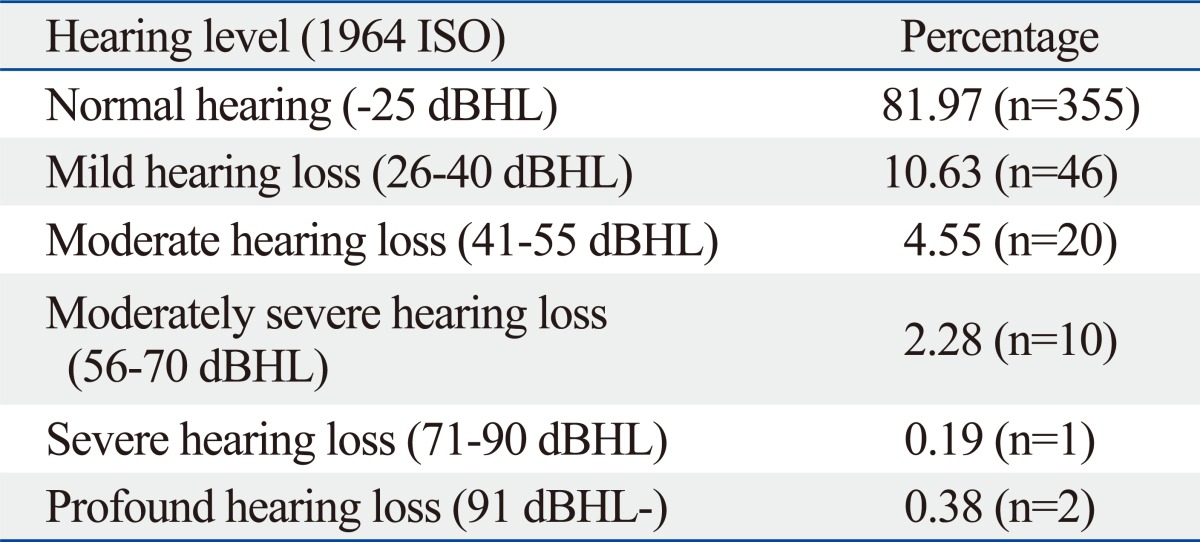
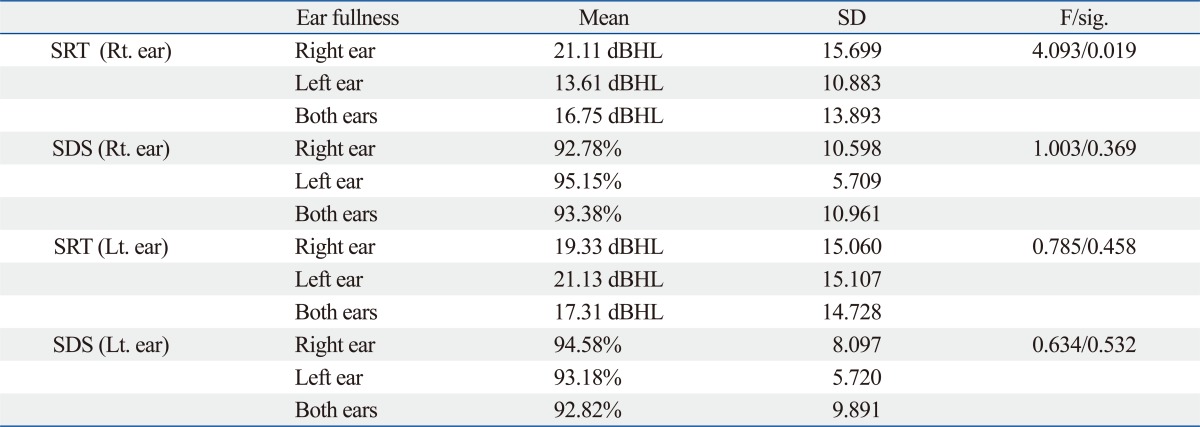
Patients were categorized according to 1964 International Organization for Standardization (ISO) (Table 2). The average pure tone threshold was 13.6 dBHL±16.6 (range: -2.50 dB to 119.17 dB). Impedance audiometry results for ear fullness in either a single or both ears mainly showed type A (p<0.05). On speech audiometry, only the right sided speech reception thresholds varied, depending on the direction of ear fullness. Patients with right sided ear fullness showed a threshold of right ear speech recognition of 21.11±15.69 dBHL (p<0.05). In contrast, word recognition scores and speech recognition thresholds were not correlated with ear fullness (p>0.05) (Table 3).
Table 2.
Hearing Level of Patients with Ear Fullness
dBHL, decibel hearing level; ISO, International Organization for Standardization.
Table 3.
Speech Audiometry and Ear Fullness
SRT, speech reception test; SDS, speech discrimination test; Rt., right; Lt., left; dBHL, decibel hearing level.
The results of distortion product otoacoustic emission (p=0.071), auditory brainstem response (p=0.870), and electrocochleography tests (p=0.850) were not significantly associated with ear fullness.
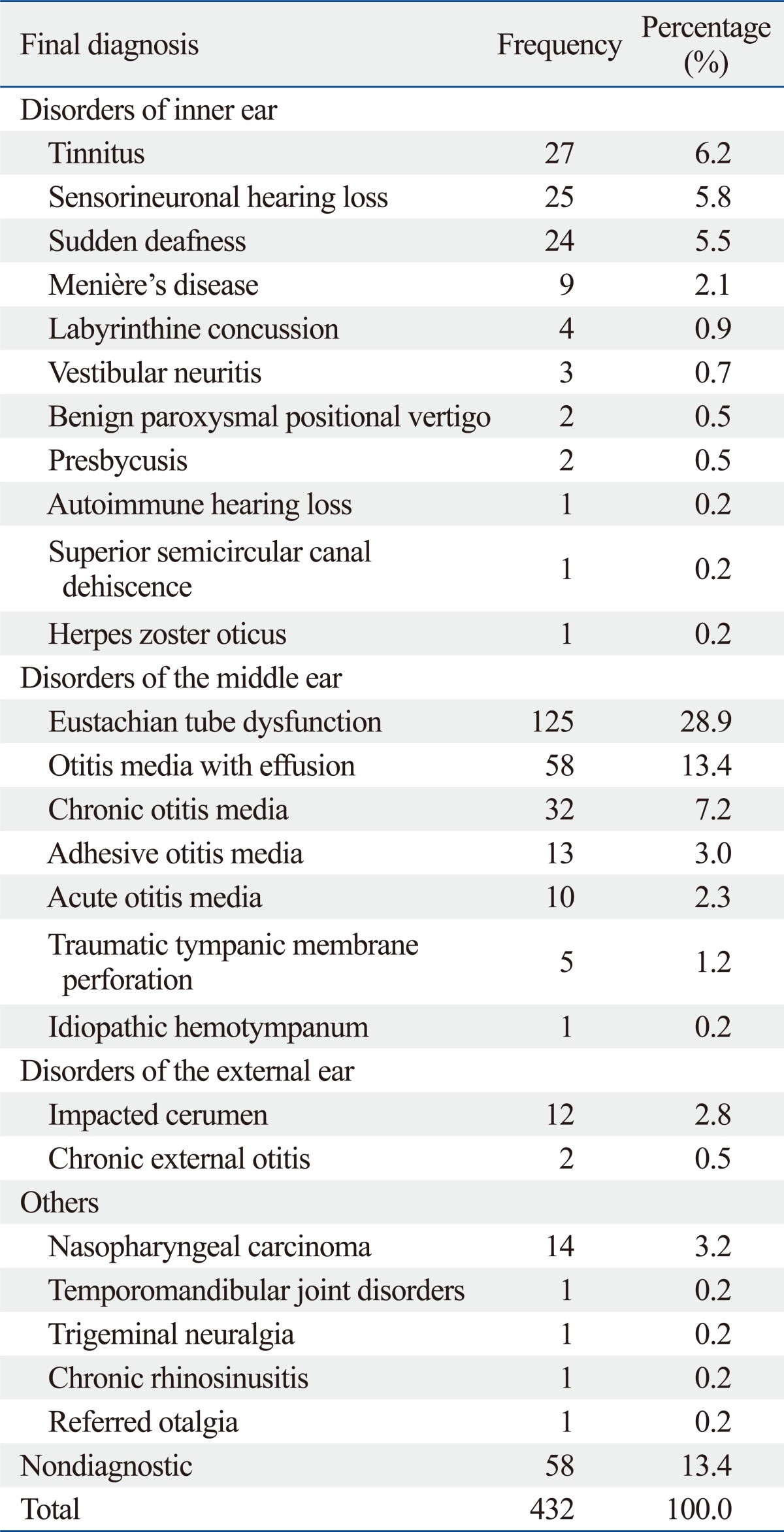
Final diagnosis and ear fullness
Eustachian tube dysfunction was ultimately diagnosed in 28.9% of these patients. The next largest group, 13.4% of patients, could not be definitively diagnosed. Other major diagnoses included otitis media with effusion, chronic otitis media and tinnitus. Patients with Eustachian tube dysfunction comprised Patulous Eustachian tubes, Eustachian tube obstruction, and Eustachian tube salpingitis. Of the 58 patients who could not be diagnosed, 22 (37.9%) underwent thorough examinations, which were insufficient in leading to a final diagnosis; 27 (46.6%) were lost to follow-up; and eight (13.8%) showed normal functioning on every examination. Insufficient medical record keeping was observed in some of these patients' charts (Table 4).
Table 4.
Final Diagnoses of Patients Mainly Complaining of Ear Fullness
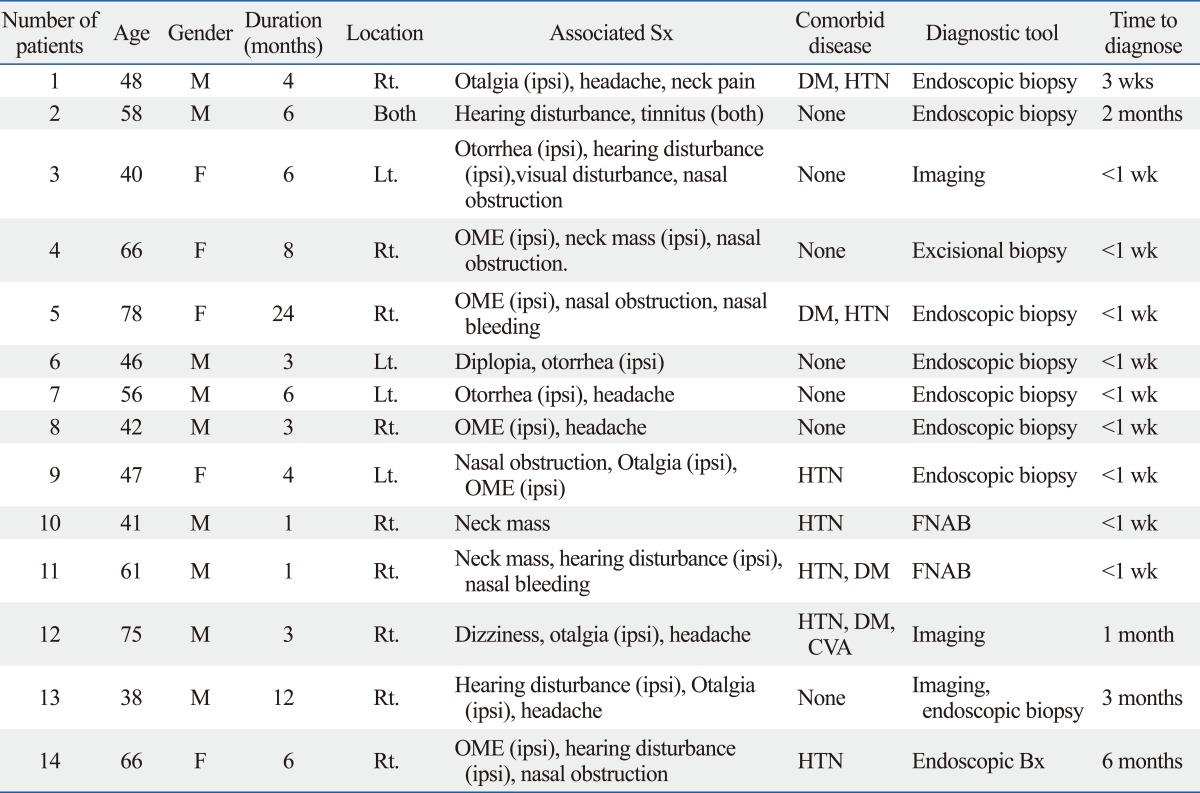
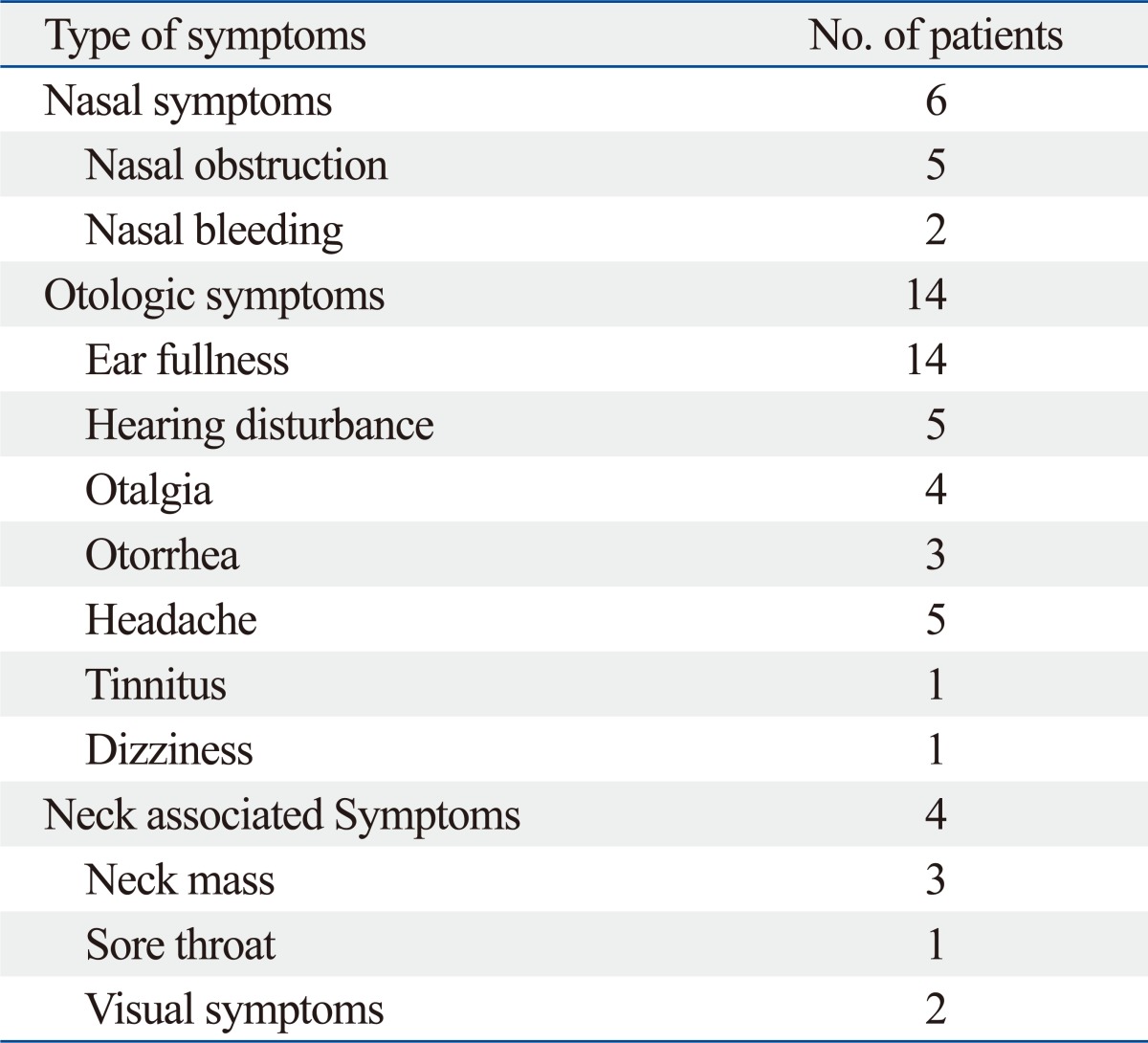
In addition, 14 (3.2%) of the 432 patients were finally diagnosed with nasopharyngeal cancer upon fulfilling the following criteria: more than 1 month of persistent symptoms and confirmation by medical imaging and histological examination within 1 week of the first visit. Unlike most patients, four patients originally complained of otologic symptoms only. For those patients, it took more than 1 month after the first visit to be finally diagnosed (Table 5). Other accompanying symptoms with nasopharyngeal cancer in patients with ear fullness included non-specific symptoms including nasal obstruction, nasal bleeding, rhinorrhea, headache and so on (Table 6). Briefly, among the associated symptoms with ear fullness in nasopharyngeal cancer, otologic symptoms were the most common at 64.3%. Among other symptoms, visual disturbances or headaches were presented in 50%, nasal symptoms in 42.9%, and neck associated symptoms in 28.5% of patients.
Table 5.
Characteristics of Nasopharyngeal Cancer in Patients with Ear Fullness
Ipsi, ipsilateral side; OME, otitis media with effusion; FNAB, fine needle aspiration biopsy; DM, diabetes mellitus; HTN, hypertension; CVA, cerebrovascular accident; Rt., right; Lt., left.
Table 6.
Accompanying Symptoms of Nasopharyngeal Cancer in Patients with Ear Fullness
DISCUSSION
Although many studies on patients with hearing loss and tinnitus have focused on aspects of pathophysiology and treatment, there have been no studies to date on the clinical manifestations of ear fullness, despite similarities between these audiological symptoms. Ear fullness has been regarded as an associated symptom of Menière's disease and otitis media with effusion. In this study, 1.44% of outpatients at the otolaryngology clinic complained of ear fullness as a primary symptom.
Ear fullness was more prevalent in females than in males, perhaps due to do hormonal changes accompanying menstrual cycles, and was especially prevalent in patients in their early forties.3 We also assessed the associations between aural fullness and diseases such as diabetes, hypertension, hepatitis, head and neck cancer, malignancies throughout the body, migraines, thyroid disease, chronic renal failure, depressive disorder, and allergic rhinitis, all of which might have some influence on hearing. For example, diabetes is frequently accompanied by sensorineuronal hearing loss, which may hinder both hearing and cognitive functioning.4,5 In addition, a study based of DPOAE and PTA found that hypertension was a high risk factor for hearing loss.6 Other studies also showed a possible association between aural fullness and other diseases, such as delayed neural conduction of the auditory pathway during chronic renal failure and numerous cases of hearing loss among phonophobia patients with migraines.7,8 Depression has also been linked to hearing loss and vision impairments.9,10 In contrast with these reported associations, we found no relationship between aural fullness and any of these diseases.
In this study, symptoms significantly associated with ear fullness included hearing disturbances (43.0%), tinnitus (28.3%), autophony (26.3%), nasal obstruction (17.7%), and sore throat (5.4%), suggesting that outpatients complaining of ear fullness should be examined for these symptoms in order to arrive at a final diagnosis. Physical examination should include the Valsalva test; nasal examinations should include endoscopy; and audiological tests should include PTA. The highest incidence of hearing disturbances was due to the subjective similarity between hearing loss and ear fullness, making it important to determine whether these symptoms are due only to "ear fullness". The results of audiological tests showed that the A type was most prevalent in patients with aural fullness, followed by the B and C types. This result was not surprising, since 69.0% of these patients had normal functioning eardrums. About 20% of patients suffered from severe or profoundly severe hearing loss, indicating that subjective hearing loss can coexist with ear fullness, regardless of hearing capacity.
Patients who present with ear fullness should undergo basic hearing threshold evaluations, such as PTA. This is more important in assessing the possibility of Menière's disease and dysfunction of the inner ear in the early stages, when ear fullness may present.
The most prevalent final diagnoses in patients complaining chiefly of ear fullness were Eustachian tube dysfunction, followed by otitis media with effusion and chronic otitis media. Eustachian tube dysfunction may be accompanied by ear fullness due to the failure of pressure control. Ear fullness in patients with otitis media with effusion or disorders of sound transmission or resonance may be due to fluid filling the middle ear.
Eustachian tube dysfunction may be triggered by many causes, the most common being viral infection, chronic sinusitis, allergic rhinitis, adenoid hypertrophy, tobacco smoke, reflux, cleft palate, reduced mastoid air cell system, and nitrous oxide.11 There may also be an association between Eustachian tube dysfunction and allergic rhinitis.12 In general, there is no single test that can precisely evaluate the functioning of the Eustachian tube.13 Therefore, in order to accurately diagnose Eustachian tube dysfunction, it is necessary to examine nasal and Eustachian tube conditions by taking a detailed history and by performing otoscopic and nasal endoscopic examinations. Moreover, the Toynbee and Valsalva maneuver, while frequently used for examination, cannot be used in quantitative analyses. To compensate, sonotubometry has been introduced for the evaluation of Eustachian tube function, regardless of eardrum conditions. This test, however, remains unpopular.14
Finally, clinicians should not overlook the possibility of nasopharyngeal carcinoma. Although usually occurring in fewer than 1 per 100000 persons, its incidence is 30-times higher in Chinese individuals. It is also well-known that low socioeconomic status, Epstein Barr virus infection, and exposure to croton and tung oil increase the risk of nasopharyngeal carcinoma; an association between HLA-A2 and HLA-B17 has also been shown.15-18 In addition, 3.2% of patients with ear fullness in this study were diagnosed with nasopharyngeal cancer, a higher rate than that for the total rate of nasopharyngeal cancer.15 This can be explained by the fact that many patients are referred from either a primary or a secondary hospital for more accurate diagnosis and suspicious cancer treatment. After analyzing patients with nasopharyngeal cancer, many complained of otologic symptoms upon visitation to the outpatient clinic, among which ear fullness was most frequently reported, followed by sinonasal symptoms and head and neck symptoms.
Of particular importance, patients that first complained of otologic symptoms only took longer to be finally diagnosed with nasopharyngeal cancer. Since ear fullness was only considered as a simple otologic symptom, the lack of endoscopic and histological examination may have delayed the diagnosis for nasopharyngeal cancer. Thus, ear fullness should not be considered as a simple otologic symptom, and should be carefully examined along with other accompanying symptoms. In conclusion, in examining outpatients whose main complaint was ear fullness, we found that the predominant final diagnosis was Eustachian tube dysfunction, followed by otitis media with effusion and chronic otitis media. These patients should be examined by otoscopy, nasal endoscopy, the Valsalva maneuver, and additional audiological tests. Since many of our patients could not be initially diagnosed, it is necessary to take a detailed history, as well as perform thorough examinations and sustained observations of patients in order to arrive at a final diagnosis.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Tokumasu K, Fujino A, Naganuma H, Hoshino I, Arai M. Initial symptoms and retrospective evaluation of prognosis in Menière's disease. Acta Otolaryngol Suppl. 1996;524:43–49. doi: 10.3109/00016489609124348. [DOI] [PubMed] [Google Scholar]
- 2.Westerlaken BO, Stokroos RJ, Dhooge IJ, Wit HP, Albers FW. Treatment of idiopathic sudden sensorineural hearing loss with antiviral therapy: a prospective, randomized, double-blind clinical trial. Ann Otol Rhinol Laryngol. 2003;112:993–1000. doi: 10.1177/000348940311201113. [DOI] [PubMed] [Google Scholar]
- 3.Nir D, Weissman A, Drugan A, Zimmer EZ, Danino J, Shenhav R, et al. Effect of estrogen on eustachian tube performance. Am J Otol. 1991;12:119–121. [PubMed] [Google Scholar]
- 4.Kakarlapudi V, Sawyer R, Staecker H. The effect of diabetes on sensorineural hearing loss. Otol Neurotol. 2003;24:382–386. doi: 10.1097/00129492-200305000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Cukierman T, Gerstein HC, Williamson JD. Cognitive decline and dementia in diabetes--systematic overview of prospective observational studies. Diabetologia. 2005;48:2460–2469. doi: 10.1007/s00125-005-0023-4. [DOI] [PubMed] [Google Scholar]
- 6.Zhang J, Zhou H, Zhang G, Xu Y. [A study on early hearing impairment with essential hypertension] Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2009;23:731–733. [PubMed] [Google Scholar]
- 7.Aspris AK, Thodi CD, Balatsouras DG, Thodis ED, Vargemezis V, Danielides V. Auditory brainstem responses in patients under treatment of hemodialysis. Ren Fail. 2008;30:383–390. doi: 10.1080/08860220801947405. [DOI] [PubMed] [Google Scholar]
- 8.Baloh RW. Neurotology of migraine. Headache. 1997;37:615–621. doi: 10.1046/j.1526-4610.1997.3710615.x. [DOI] [PubMed] [Google Scholar]
- 9.Capella-McDonnall ME. The effects of single and dual sensory loss on symptoms of depression in the elderly. Int J Geriatr Psychiatry. 2005;20:855–861. doi: 10.1002/gps.1368. [DOI] [PubMed] [Google Scholar]
- 10.Chia EM, Mitchell P, Rochtchina E, Foran S, Golding M, Wang JJ. Association between vision and hearing impairments and their combined effects on quality of life. Arch Ophthalmol. 2006;124:1465–1470. doi: 10.1001/archopht.124.10.1465. [DOI] [PubMed] [Google Scholar]
- 11.Seibert JW, Danner CJ. Eustachian tube function and the middle ear. Otolaryngol Clin North Am. 2006;39:1221–1235. doi: 10.1016/j.otc.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 12.Yeo SG, Park DC, Eun YG, Cha CI. The role of allergic rhinitis in the development of otitis media with effusion: effect on eustachian tube function. Am J Otolaryngol. 2007;28:148–152. doi: 10.1016/j.amjoto.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 13.Westerman ST. Tasting instilled otologic drops is not a reliable test of eustachian tube function. Arch Otolaryngol Head Neck Surg. 2000;126:1042. doi: 10.1001/archotol.126.8.1042. [DOI] [PubMed] [Google Scholar]
- 14.van der Avoort SJ, van Heerbeek N, Zielhuis GA, Cremers CW. Sonotubometry: eustachian tube ventilatory function test: a state-of-the-art review. Otol Neurotol. 2005;26:538–543. doi: 10.1097/01.mao.0000169765.00798.cd. [DOI] [PubMed] [Google Scholar]
- 15.Shanmugaratnam K. Nasopharyngeal carcinoma: epidemiology, histopathology and aetiology. Ann Acad Med Singapore. 1980;9:289–295. [PubMed] [Google Scholar]
- 16.Yu WM, Hussain SS. Incidence of nasopharyngeal carcinoma in Chinese immigrants, compared with Chinese in China and South East Asia: review. J Laryngol Otol. 2009;123:1067–1074. doi: 10.1017/S0022215109005623. [DOI] [PubMed] [Google Scholar]
- 17.Li X, Fasano R, Wang E, Yao KT, Marincola FM. HLA associations with nasopharyngeal carcinoma. Curr Mol Med. 2009;9:751–765. doi: 10.2174/156652409788970698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skinner DW, Van Hasselt CA, Tsao SY. Nasopharyngeal carcinoma: modes of presentation. Ann Otol Rhinol Laryngol. 1991;100:544–551. doi: 10.1177/000348949110000705. [DOI] [PubMed] [Google Scholar]