Abstract
Live attenuated viruses make potent and effective vaccines. Despite the urgent need for an HIV vaccine, this approach has not been feasible, since it has not been possible to attenuate the virus reliably and guarantee vaccine safety. Instead, live viral vectors have been proposed that could present HIV vaccine antigens in the most immunogenic way, in the context of an active infection. We have adapted the rubella vaccine strain RA27/3 as a vector to express HIV and SIV antigens, and tested the effect of insert size and composition on vector stability and viral titer. We have identified an acceptor site in the rubella nonstructural gene region, where foreign genes can be expressed as a fusion protein with the nonstructural protein P150 without affecting essential viral functions. The inserts were expressed as early genes of rubella, under control of the rubella genomic promoter. At this site, HIV and SIV antigens were expressed stably for at least seven passages, as the rubella vectors reached high titers. Rubella readily infects rhesus macaques, and these animals will provide an ideal model for testing the new vectors for replication in vivo, immunogenicity, and protection against SIV or SHIV challenge.
Keywords: live viral vectors, rubella vaccine strain RA27/3, stable expression, HIV MPER, SIV Gag, vaccine antigen
1. Introduction
Many successful vaccines are based on live attenuated strains derived from viral pathogens. As they replicate in the host, they express exponentially increasing amounts of viral antigens. They present antigens in the most immunogenic way, in the context of an active infection. In the past, vaccine strains were derived from virulent viruses by repeated passage under selective conditions until virulence genes were mutated or lost, while retaining the ability to replicate and elicit an immune response in the host [1]. Unfortunately, this approach cannot be applied to all viruses.
Human immunodeficiency virus (HIV) infection often elicits a strong immune response, including cytolytic T lymphocytes (CTL) [2] and neutralizing antibodies [3–5]. Their targets have been identified as potential vaccine antigens. Similarly, in SIV infection, prior infection with a replicating, nef deleted simian immunodeficiency virus (SIV) can protect animals against a subsequent challenge with wild type virus [6]. However, it seems unlikely that HIV virus could be attenuated sufficiently for vaccine use [7]. This is due to the retroviral life cycle, with its obligatory integration into host DNA, as well as the high rate of mutation, with the risk of reversion to wild type [8]. In addition, virulence genes have not been identified that could be deleted to produce a reliably attenuated vaccine strain.
Instead of attenuating HIV directly, we and other groups have developed live attenuated viral vectors that combine the safety and immunogenicity of the vector with the antigenicity of HIV and SIV protein inserts. These have included DNA viruses, such as vaccinia virus and modified vaccinia Ankara [9], adenovirus [10–12] and cytomegalovirus (CMV) [13]. RNA viruses, such as Venezuelan equine encephalomyelitis replicons [14–16], attenuated vesicular stomatitis virus [17], and yellow fever vaccine [18, 19] have also been tested. Some vectors replicate poorly or not at all in vivo, while others continue to replicate until they are stopped by the immune response [20]. We have focused on the rubella vaccine strain RA27/3 because it is a licensed product with a safety record established in millions of children around the world [21, 22]. It is immunogenic: one dose protects for life against rubella infection. Full length, infectious cDNA clones are available both for wild type rubella virus [23] and for the RA 27/3 vaccine strain [24]. We have shown that rubella virus can be adapted for heterologous protein expression [25] by using the permissive deletion described by Tzeng et al. [26, 27] to make room for the insert.
Important questions for RNA viral vectors include the maximum insert size, vector stability, and viral titer that could be achieved by a small RNA virus carrying vaccine antigens[28]. In this paper, we report the first live rubella vectors expressing the HIV membrane-proximal external region (MPER) determinant targeted by cross-reactive neutralizing antibodies or multiple SIV Gag (sGag) epitopes targeted by T cells. The vectors grew to high titer while stably expressing their antigens for at least seven passages. Rubella readily infects rhesus macaques [29], and these will be the animal model of choice for demonstrating immunogenicity and protection against SIV or simian-human immunodeficiency virus (SHIV) challenge [11–13].
2. Materials and methods
2.1. Antibodies and antigens
Monoclonal antibodies 2F5 and 4E10 were obtained from the NIH AIDS Research and Reference Reagent Program, Division of AIDS, NIAID and from Dr. Hermann Katinger, Polymun Scientific (Klosterneuburg, Austria). Polyclonal goat antibodies to rubella structural proteins were purchased from Fitzgerald Industries International, Inc. (Concord, MA). Rabbit antibodies to rubella nonstructural protein P150 were provided by Dr. Tero Ahola (University of Helsinki, Finland) [30].
2.2. Construction of cDNA plasmids coding for infectious RNA
Plasmid p10RA coding for full-length infectious cDNA of the RA27/3 vaccine strain of rubella [24] was kindly provided by Dr. T. Frey (Georgia State University, Atlanta). Infectious rubella RNA was generated by transcribing from the SP6 promoter, followed by RNA capping.
For cloning purposes, a sub-clone of p10RA (from Hind III to Bgl II), pBR322-Hind- Bgl-RA was created in pBR322. To create space for potential inserts, a deletion was made between the two Not I sites at positions 3661 and 4168 in the non-structural protein region, as reported for wild type rubella [25, 26]. Hind III-Cla I fragment from the sub-clone carrying the Not I deletion was cloned back to p10RA, giving pBRA3226-dNotI plasmid. The constructs were verified by sequencing.
2.3. Construction of vectors with insertions in the nonstructural gene region
Recognition sequences for Avr II and Nsi I restriction enzymes were cloned into the Not I deletion site. These unique restriction sites were then used for directional cloning of inserts into the Not I-deletion site. In the case of MPERF, MPERE, SGag2L-A, SGag2L-B, SGag2L-C, and BC-SGag2, cloning was done using SpeI and Nsi I sites. Spe I and Avr II have compatible sticky ends. Each insert was PCR amplified using primers listed in Supplementary Table S1 and HIV-1 89.6 gp160 or SIV mac239 gag DNA as templates, cut with restriction enzymes, and ligated into the matching restriction sites. The amino acid sequences of these inserts are listed in Table 1.
Table 1.
Amino acid sequences of the HIV-1 MPER- and SIV Gag-derived inserts expressed at the Not I 3 site.
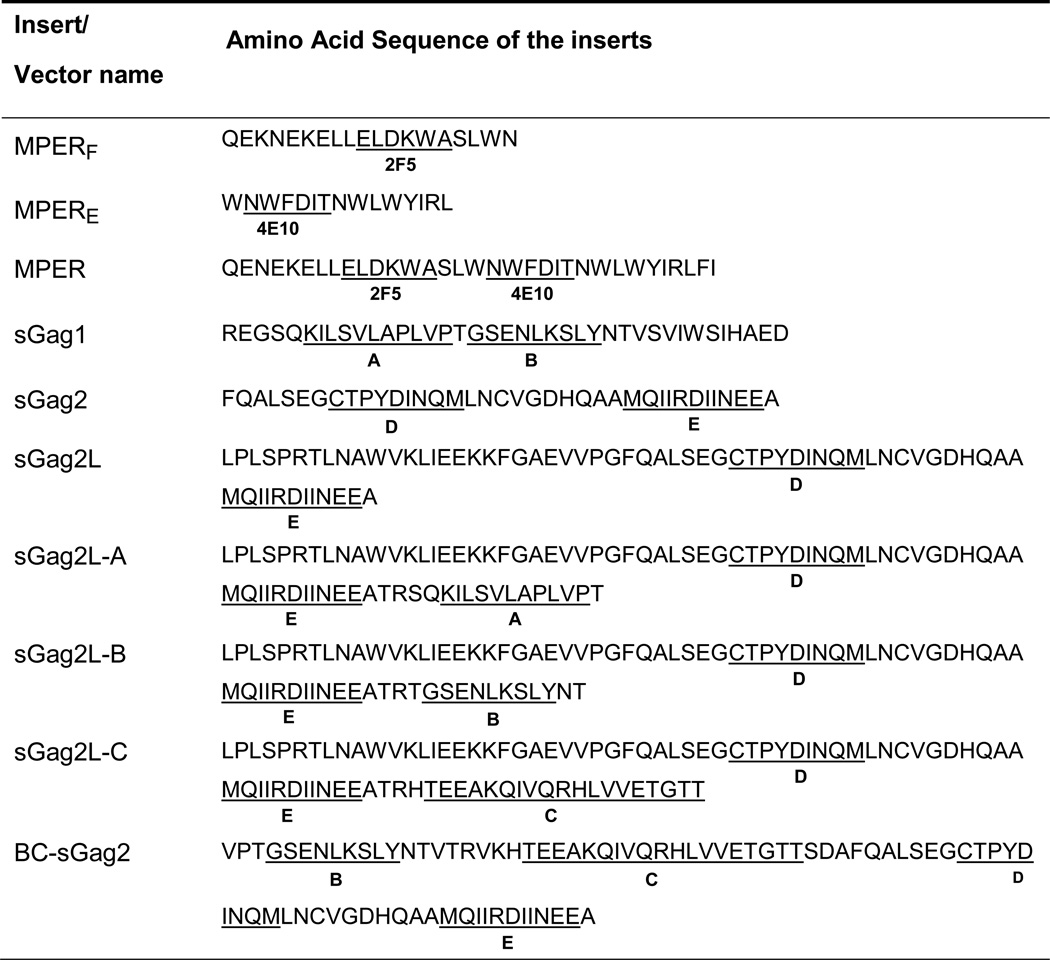 |
Underlined sequences show the core epitopes for broadly neutralizing antibodies 2F5 and 4E10, 5 and T cell epitopes in SIV Gag. All labeling is the same as in Fig. 1B.
2.4. Generation of rubella virus
The protocol for generation of capped, infectious rubella virus RNA from plasmid DNA and subsequent transfection of Vero cells was described previously [25]. After 7–10 days of infection, culture supernatant (P0) was centrifuged to produce cell-free supernatant and 0.1 mL was transferred onto fresh Vero cells to begin the next passage P1. Alternatively, in early passages, propagation efficiency could be increased by transferring virus via infected cells, rather than culture supernatants. After passages P3 or P4, we changed over to cell-free passage without loss of infectivity. This method was used to propagate vectors with inserts as large as BC- sGag2.
To estimate vector replication, we tested infected cells for expression of rubella structural proteins by Western blot. We also tested insert expression by Western blot, using specific antibodies. To produce a viral stock, virus from passage 4 or 5 was grown for 7 to 10 days on a Vero cell monolayer in a T75 flask. The yield of viral RNA was determined by quantitative RT- PCR, and multiple aliquots were frozen.
2.5. Detection of rubella proteins and MPER inserts by Western blot
Rubella structural proteins were detected by Western blot with goat anti-rubella antibodies to capsid protein C and envelope protein E1, as described previously [25]. Rubella non-structural protein P150 was detected using rabbit polyclonal antibodies at a dilution of 1:1000 [30]. Expression of the MPERF insert was detected with human monoclonal antibody 2F5 at 1 µg/ml. The second antibody was either horseradish peroxidase-conjugated rabbit anti-goat IgG, goat anti-rabbit IgG or goat anti-human IgG at 1:5000 dilution (Santa Cruz Biotechnology, CA). Blots were visualized with enhanced chemiluminescence (GE Healthcare).
2.6. Analysis of insert stability
To verify stability of the inserts in rubella, we sequenced the rubella flanking regions, as well as the entire insert, as described previously [25]. To PCR amplify cDNA we used oligonucleotide primers specific for rubella sequences flanking the Not I insertion site: Robo-seq67 (forward primer: 5’- gatgacgaggcgctcatcc) and Robo-seq6A (reverse primer: 5’-gagtgccgcgggcgtccgagtgc). The PCR products were analyzed by gel electrophoresis, purified from the gel using MinElute Gel Extraction Kit (Qiagen) and sequenced using the same primers.
3. Results
3.1. Insertion of foreign genes into the Not I site of rubella
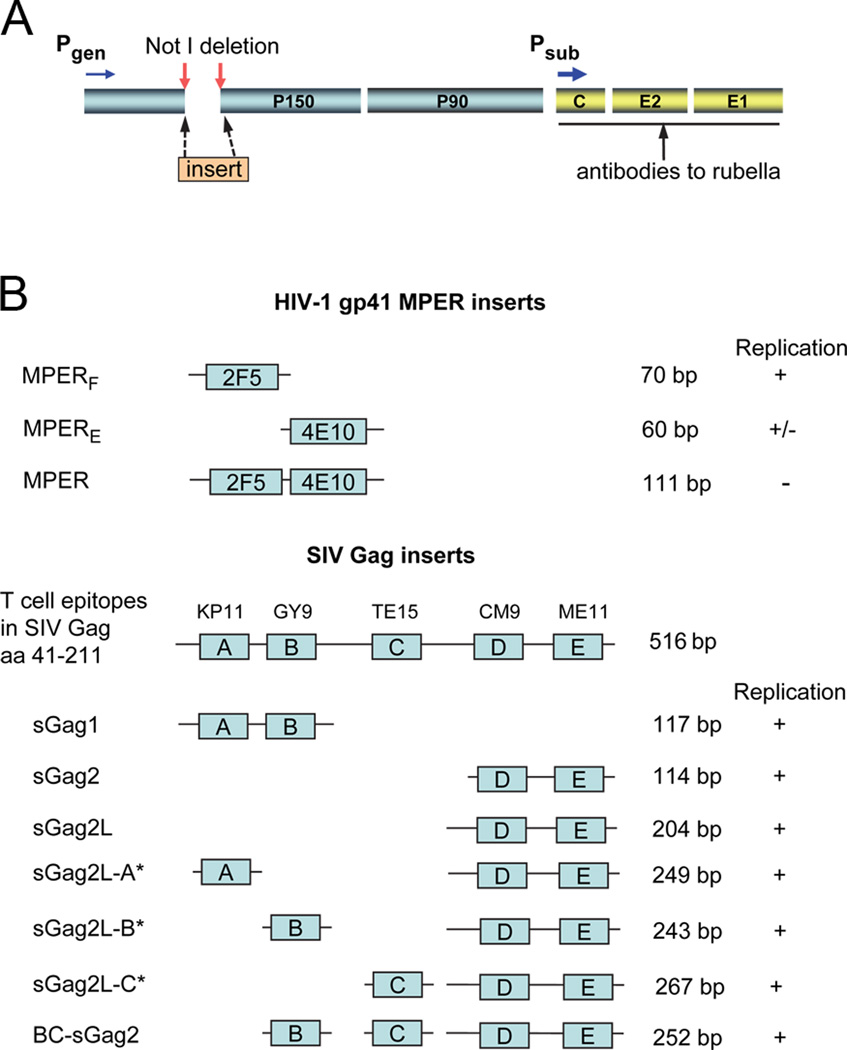
We have used a deletion/insertion strategy to construct rubella viral vectors carrying a foreign gene at the Not I site (Fig. 1A). This approach was employed in our previous study, where we deleted the 507 bp sequence between two Not I restriction sites in the nonstructural region and then inserted a zGFP reporter gene (792 bp) into the same site [25]. The resulting vector expressed zGFP (25 kDa) as a fusion protein with the rubella nonstructural protein P150 and replicated with nearly the same kinetics and yield as wild type rubella virus [25].
Figure 1. Deletion/insertion strategy for producing rubella vectors.
(A) Rubella genome, showing nonstructural proteins P150 and P90, structural proteins capsid, E2 and E1, and the genomic (Pgen) and subgenomic (Psub) promoters. A deletion between two Not I restriction sites in P150 allowed insertion of foreign genes at the same site. (B) HIV-1 gp41 inserts contained one or two epitopes of the membrane-proximal external region (MPER) targeted by broadly neutralizing antibodies 2F5 and 4E10. SIV Gag amino acids 41 to 211 contain five T cell epitopes, labeled A through E. The epitopes in each construct are shown schematically. In constructs denoted by an asterisk (*) one epitope at a time was added to the carboxyl end of sGag2L to produce sGag2L-A, -B, or -C. The vector BC-sGag2 contained four epitopes and replicated strongly for at least eight passages. Vector replication after 2 to 8 passages was detected with antibodies to the rubella structural proteins C and E1 and is indicated by + or −.
In this study, we have created ten new rubella vectors bearing HIV and SIV inserts at the Not I site (Fig. 1B). Three vectors contained HIV MPER-derived inserts and seven vectors carried SIV Gag antigens (called sGag). The full length MPER insert coded for 33 amino acids and included core epitopes recognized by human neutralizing monoclonal antibodies 2F5 (ELDKWA) and 4E10 (NWFDIT) (Fig. 1B, Table 1). Inserts MPERF and MPERE contained the 2F5 epitope [31] and the 4E10 epitope [32] separately.
The sGag inserts were derived from SIV Gag amino acids 41–211 (Fig. 1B). This region encodes the carboxyl half of matrix protein p17 and the amino half of capsid protein p27. It is rich in epitopes (at least 5) targeted by T cells during the immune response to SIV infection in rhesus macaques (Table 2) [33–35]. We started with small inserts coding for two epitopes, such as sGag1 and sGag2, and then added epitopes stepwise (Fig. 1B). The second largest insert BC-sGag2 contained four T cell epitopes: GY9, TE15, CM9, and ME11. The amino acid sequences of these inserts are shown in Table 1, with T cell epitopes underlined. Together, these constructs represent a series of rubella vectors expressing SIV Gag inserts of increasing size (114 to 267 bp) and antigenic complexity (one to four epitopes).
Table 2.
T cell epitopes in SIV Gag (amino acids 41–211).
| sGag insert |
Gag epitope |
Sequence | Amino acids |
Gag protein |
MHC Class |
MHC Type |
Ref. |
|---|---|---|---|---|---|---|---|
| A | KP11 | KILSVLAPLVP | 59–70 | p17 MA | II | DPB1-06 | [35] |
| B | GY9 | GSENLKSLY | 71–79 | p17 MA | I | A02 | [45] |
| C | TE15/KT15 | TEEAKQIVQRHLVVE | 97–111 | p17 MA | II | DRB-W606 | [35] |
| D | CM9 | CTPYDINQM | 181–189 | p27 CA | I | A01 | [33] |
| E | ME11 | MQIIRDIINEE | 200–210 | p27 CA | II | DRB1-0306 | [35] |
3.2. Vector replication and expression of HIV MPER inserts
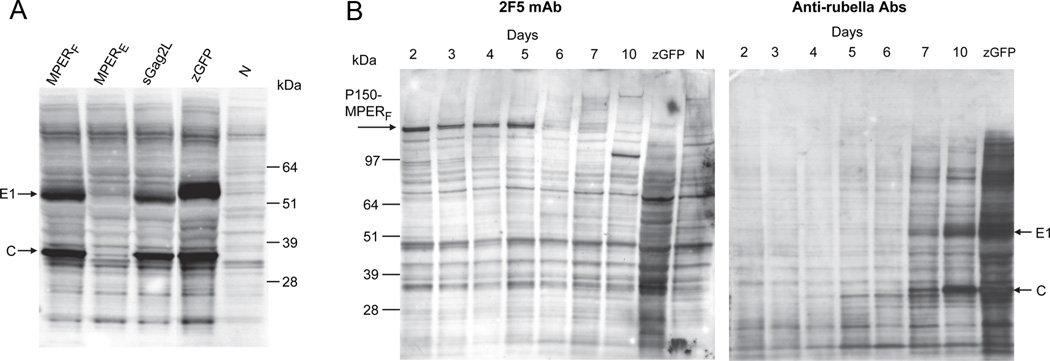
Replication of rubella vectors at an early passage was detected by Western blot with goat antibodies to rubella structural proteins. The vector expressing MPERF replicated strongly, while replication of the MPERE construct was barely detectable (Fig. 2A). Rubella virus bearing full length MPER (with both 2F5 and 4E10 epitopes) at the Not I site did not replicate. Vector sGag2L (with two SIV Gag epitopes) replicated nearly as well as the MPERF vector, but less well than the zGFP control vector constructed on the wild type rubella background (Fig. 2A). In these constructs, the MPER and Gag inserts were expressed as a fusion protein with P150 (Fig. 1A). As P150 is an essential cofactor for both plus and minus strand RNA synthesis [30, 36–38], this can place constraints on the insert. Any insert that reduced levels of functional P150 could be lethal for the virus. These estimates of viral replication, based on expression of rubella proteins, were generally borne out by measuring viral RNA titers at later passages (see below).
Figure 2. Vector replication and expression of HIV MPER determinants.
(A) Rubella vector replication at passage P0 was detected by Western blot with antibodies specific for rubella structural proteins C (33 kDa) and E1 (58 kDa). Strong vector replication was observed for the MPERF vector and for sGag2L, but not for MPERE (all in the vaccine strain). These were compared to a control vector expressing zGFP in wild type rubella or to uninfected cells (lane N). (B) Time course of MPERF expression (at passage P3), as detected by Western blot with monoclonal 2F5 (left panel) or with antibodies to rubella structural proteins (right panel). MPERF was expressed as a high molecular-weight fusion protein with P150 (arrow). Maximal expression was observed from day 2 to 5 after infection. In contrast, rubella structural proteins E1 and C first appeared on day 5 or 6 and were strongly expressed on days 7 to 10. The same samples were used for both gels.
Expression of the MPERF insert was monitored by Western blot with monoclonal antibody 2F5 (Fig. 2B, left panel). MPERF was detected as a high molecular weight band at the size expected for a P150-MPERF fusion protein (arrow). A time course showed that P150-MPERF was expressed strongly by day 2 of infection and continued at a high level until day 5. After that, MPERF expression quickly declined, even though viral infection persisted for at least 5 more days. In contrast, the rubella structural proteins C and E1 were expressed as late antigens on day 6 or 7 and increased steadily until day 10 post infection (Fig. 2B, right panel). These results indicate that MPERF was expressed as an early antigen under control of the rubella genomic promoter.
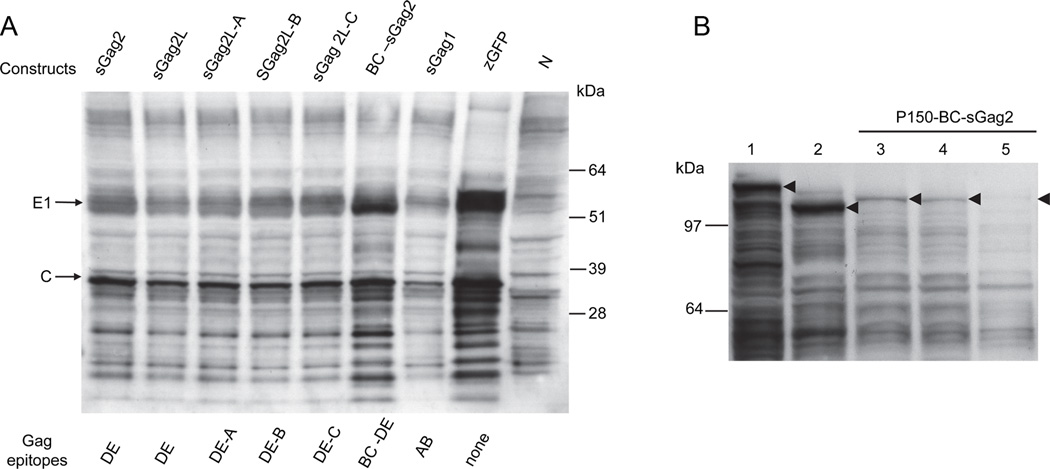
3.3. Vector replication and expression of SIV Gag inserts
The seven vectors with sGag inserts included five major Gag epitopes that are known targets of T cell immunity against SIV. Vectors bearing two to four sGag epitopes on inserts of 114 to 267 bp in size replicated strongly, as shown by Western blot of rubella structural proteins C and E1 (Fig. 3A). The second largest vector BC-sGag2, with four epitopes on the RA27/3 vaccine background, replicated nearly as well as a control vector expressing zGFP on a wild type rubella background (Fig. 3A, lanes BC-sGag2 and zGFP, respectively). Vector growth indicated that rubella could accommodate multiple T cell epitopes at the Not I site.
Figure 3. Vector replication and expression of SIV Gag epitopes.
(A) Replication of rubella vectors with a family of SIV Gag inserts was detected by Western blot with anti-rubella antibodies. These vectors replicated strongly while expressing two to four Gag epitopes. The vector with the second largest insert BC-sGag2 showed the strongest replication. Gag constructs are indicated above the gel (same as in Fig. 1B) and sGag epitopes are labeled below the gel.
Due to lack of a monoclonal antibody specific for the T cell epitopes of SIV Gag, we detected expression of BC-sGag2 at the Not I site indirectly, by measuring a shift in the P150 band to the size of the P150-BCs-Gag2 fusion protein (Fig. 3B). Western blot with antibodies to P150 showed that the size of P150 after Not I deletion (Fig. 3B, lane 2, arrowhead) shifted to a larger molecular weight following insertion of zGFP (lane 1, arrowhead) or BC-sGag2 (lanes 3 and 4, arrowheads). The size difference between P150 bands in lanes 3 and 4 vs. lane 2 indicates the presence of the BC-sGag2 insert. The P150-BC-sGag2 fusion protein was the major species of P150 in these cells. As with P150-MPERF, it was expressed at early times (lanes 3 and 4) but was undetectable by day 10 (lane 5), indicating control by the rubella genomic promoter.
3.4. Live rubella vector titers and stability
Rubella vectors would not be a practical vaccine platform unless they could achieve sufficiently high titers for vaccine production. After passage P6, we produced 20 ml stocks of rubella vectors with MPERF or BC-sGag2 inserts on the vaccine strain background (RA27/3). Viral RNA content of the stocks was measured by real time RT-PCR, as described previously [25], and the viral titer was estimated based on comparison to a rubella vaccine reference sample of known titer. As shown in Table 3, culture supernatants ranged from 106 to 107 RNA copies/ml, which correspond to infectious titers of about 105 to 106 PFU/ml.
Table 3.
Titers of rubella vector stocks of potential vaccine candidates.
| Viral vector | RNA copies/ml | Estimated titer, PFU/ml |
|---|---|---|
| MPERF in NotI site (P6) | 3.1 × 107 | 5.0 × 106 |
| BC-sGag2 in NotI site (P6) | 2.5 × 106 | 4.1 × 105 |
The viral RNA content of each vector was determined by real time RT-PCR. The titer was estimated by comparison to a vaccine standard of known infectious titer. Insert sequences were verified by viral genome sequencing.
For vectors that were considered vaccine candidates, such as BC-sGag2 and MPERF, stability was verified by sequencing viral RNA after seven passages in cell culture. Sequencing showed that the inserts were present in the correct reading frame. Continued growth of both vectors was demonstrated by Western blot through passage P7 or greater. Vector stability is important both for virus production in a fermentor and for vector expansion in the host during immunization.
4. Discussion
We have tested whether the rubella vaccine strain RA27/3 can be reprogrammed as a live viral vector to combine the safety and immunogenicity of rubella vaccine [21] with the antigenicity of SIV Gag and HIV MPER inserts. This is the first report showing that RA27/3 can stably express potential vaccine antigens, such as an MPER determinant targeted by broadly cross reactive neutralizing antibodies or up to four Gag epitopes targeted by CTLs. Insertion at the Not I site resulted in stable antigen expression that has persisted for at least seven passages. This would be sufficient for vector production in cell culture, followed by expansion in the host during immunization.
The Not I insertion site is located in the nonstructural region, and it can accommodate inserts ranging in size from 23 to 89 amino acids. The site is located in the middle of the gene coding for nonstructural protein P150. Thus, the insert protein (zGFP, BC-sGag2 or MPERF) is translated as a fusion protein with rubella P150. It is expressed as an early viral antigen between days 2 to 5 of infection. Based on prior results with P150-zGFP [25] and native P150 [30, 36, 37], the P150 fusion protein localizes to the cytoplasm, where it participates in viral replicative centers. This has a potential advantage for antigen presentation, since it is located near the entry point for proteasomal processing that leads to antigen presentation with MHC class I for induction of T cell immunity [39]. However, it may limit the choice of inserts, as P150 is an essential cofactor in viral RNA synthesis [40], and its functions must be preserved. Loss of P150 function could occur if an insert prevented normal P150 folding, blocked its interaction with viral RNA polymerase, or caused instability through proteolytic degradation or aggregation. Future studies will focus on finding alternative insertion sites, where insert size and composition have little or no effect on critical viral functions.
The MPER determinant is an important target of broadly cross reactive neutralizing antibodies [31, 32, 41]. However, these antibodies are found relatively rarely after infection, and they have not been elicited by immunization. Lack of immunogenicity may be due to several factors, including steric hindrance by gp120, lack of native conformation [42], or tolerance to self antigens [43]. Rubella vectors may help to overcome these problems by eliciting innate and adaptive immune responses to increase MPER potency.
The SIV Gag determinants were derived from a Gag region (amino acids 41–211) that is rich in targets of T cell immunity [33–35]. The CM9 and GY9 epitopes are restricted by Mamu A01 and A02, respectively. They are prominent CTL targets early after SIV infection [44, 45], and virus escape occurs late, if at all. These sites may be slow to mutate because they perform critical viral functions for SIV and require compensatory mutations before they can escape. By eliciting cytolytic T cells specific for these epitopes prior to infection, the BC-sGag2 vector could control a subsequent SIV infection, with limited risk of viral escape.
Rubella’s biological properties favor its use as a vaccine platform. The safety of the RA27/3 vaccine strain has been demonstrated in millions of children around the world [21, 22]. The SIV Gag and HIV-1 MPER inserts were made on this background. These vectors replicate to high titers during vaccine production, yet rubella is known to immunize at the lowest dose of any vaccine, approximately 103 PFU [21]. If this dose can be extrapolated to the new rubella vectors, the titers we obtained in cell culture (Table 3) correspond to between 400 and 5,000 human doses per milliliter.
A rubella vector poses little risk of viral persistence, has no DNA intermediates and does not integrate into host genomes as retroviral vectors do [46]. Even if a vector lost its insert, it would revert to the vaccine strain. The vector does not interfere with antigen processing and presentation, as with CMV and adenovirus vectors [47]. Like any replicating viral vector, rubella will elicit antibodies to itself [17, 18]. This can be overcome by combining rubella vectors with another vaccine platform in a prime and boost strategy [20], or by giving rubella first, followed by a protein boost with virus-like particles [48, 49].
Rubella virus can readily infect rhesus macaques and immunizes them efficiently [29]. This will allow us to quickly evaluate rubella vectors expressing different vaccine antigens for growth and immunogenicity. Rhesus macaques are the model of choice for SIV and SHIV challenge studies. By comparing the immune response to each vector with the degree of protection against SIV or SHIV challenge, we can determine the correlates of protection. The same vectors replicate well in monkeys and man, so the results and immune correlates observed in monkeys could be readily translated into human vaccine design. Our study was focused on HIV and SIV, however, rubella viral vectors could be used to immunize against a variety of other infectious diseases.
Supplementary Material
Highlights.
We created live rubella vectors expressing HIV/SIV antigens in the non-structural gene region.
Inserts up to 267 bp were stably expressed for at least seven passages.
They were expressed as early antigens under control of the genomic promoter.
The vectors, based on the rubella vaccine strain, reached high titers in cell culture.
Acknowledgements
We thank Dr. David Watkins and Dr. Carol Weiss for many helpful discussions and Dr. Steven Feinstone for careful reading of the manuscript. We also thank Dr. Rajesh Gupta and Dr. Muhammad Shahabuddin of CBER for providing a titered reference sample of rubella vaccine.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Appendix A. Supplementary data
References
- 1.Chanock RM. Reminiscences of Albert Sabin and his successful strategy for the development of the live oral poliovirus vaccine. Proc Assoc Am Physicians. 1996 Mar;108(2):117–126. [PubMed] [Google Scholar]
- 2.Phillips RE, Rowland-Jones S, Nixon DF, Gotch FM, Edwards JP, Ogunlesi AO, et al. Human immunodeficiency virus genetic variation that can escape cytotoxic T cell recognition. Nature. 1991 Dec 12;354(6353):453–459. doi: 10.1038/354453a0. [DOI] [PubMed] [Google Scholar]
- 3.Berkower I, Murphy D, Smith CC, Smith GE. A predominant group-specific neutralizing epitope of human immunodeficiency virus type 1 maps to residues 342 to 511 of the envelope glycoprotein gp120. J Virol. 1991 Nov;65(11):5983–5990. doi: 10.1128/jvi.65.11.5983-5990.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu X, Zhou T, Zhu J, Zhang B, Georgiev I, Wang C, et al. Focused evolution of HIV-1 neutralizing antibodies revealed by structures and deep sequencing. Science. Sep 16;333(6049):1593–1602. doi: 10.1126/science.1207532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheid JF, Mouquet H, Ueberheide B, Diskin R, Klein F, Oliveira TY, et al. Sequence and structural convergence of broad and potent HIV antibodies that mimic CD4 binding. Science. Sep 16;333(6049):1633–1637. doi: 10.1126/science.1207227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daniel MD, Kirchhoff F, Czajak SC, Sehgal PK, Desrosiers RC. Protective effects of a live attenuated SIV vaccine with a deletion in the nef gene. Science. 1992 Dec 18;258(5090):1938–1941. doi: 10.1126/science.1470917. [DOI] [PubMed] [Google Scholar]
- 7.Baba TW, Liska V, Khimani AH, Ray NB, Dailey PJ, Penninck D, et al. Live attenuated, multiply deleted simian immunodeficiency virus causes AIDS in infant and adult macaques. Nat Med. 1999 Feb;5(2):194–203. doi: 10.1038/5557. [DOI] [PubMed] [Google Scholar]
- 8.Kirchhoff F, Kestler HW, 3rd, Desrosiers RC. Upstream U3 sequences in simian immunodeficiency virus are selectively deleted in vivo in the absence of an intact nef gene. J Virol. 1994 Mar;68(3):2031–2037. doi: 10.1128/jvi.68.3.2031-2037.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Earl PL, Wyatt LS, Montefiori DC, Bilska M, Woodward R, Markham PD, et al. Comparison of vaccine strategies using recombinant env-gag-pol MVA with or without an oligomeric Env protein boost in the SHIV rhesus macaque model. Virology. 2002 Mar 15;294(2):270–281. doi: 10.1006/viro.2001.1345. [DOI] [PubMed] [Google Scholar]
- 10.Demberg T, Florese RH, Heath MJ, Larsen K, Kalisz I, Kalyanaraman VS, et al. A replication-competent adenovirus-human immunodeficiency virus (Ad-HIV) tat and Ad-HIV env priming/Tat and envelope protein boosting regimen elicits enhanced protective efficacy against simian/human immunodeficiency virus SHIV89.6P challenge in rhesus macaques. J Virol. 2007 Apr;81(7):3414–3427. doi: 10.1128/JVI.02453-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patterson LJ, Malkevitch N, Venzon D, Pinczewski J, Gomez-Roman VR, Wang L, et al. Protection against mucosal simian immunodeficiency virus SIV(mac251) challenge by using replicating adenovirus-SIV multigene vaccine priming and subunit boosting. J Virol. 2004 Mar;78(5):2212–2221. doi: 10.1128/JVI.78.5.2212-2221.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shiver JW, Fu TM, Chen L, Casimiro DR, Davies ME, Evans RK, et al. Replication- incompetent adenoviral vaccine vector elicits effective anti-immunodeficiency-virus immunity. Nature. 2002 Jan 17;415(6869):331–335. doi: 10.1038/415331a. [DOI] [PubMed] [Google Scholar]
- 13.Hansen SG, Ford JC, Lewis MS, Ventura AB, Hughes CM, Coyne-Johnson L, et al. Profound early control of highly pathogenic SIV by an effector memory T-cell vaccine. Nature. 2011 May 26;473(7348):523–527. doi: 10.1038/nature10003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnston RE, Johnson PR, Connell MJ, Montefiori DC, West A, Collier ML, et al. Vaccination of macaques with SIV immunogens delivered by Venezuelan equine encephalitis virus replicon particle vectors followed by a mucosal challenge with SIVsmE660. Vaccine. 2005 Oct 10;23(42):4969–4979. doi: 10.1016/j.vaccine.2005.05.034. [DOI] [PubMed] [Google Scholar]
- 15.MacDonald GH, Johnston RE. Role of dendritic cell targeting in Venezuelan equine encephalitis virus pathogenesis. J Virol. 2000 Jan;74(2):914–922. doi: 10.1128/jvi.74.2.914-922.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pushko P, Parker M, Ludwig GV, Davis NL, Johnston RE, Smith JF. Replicon-helper systems from attenuated Venezuelan equine encephalitis virus: expression of heterologous genes in vitro and immunization against heterologous pathogens in vivo. Virology. 1997 Dec 22;239(2):389–401. doi: 10.1006/viro.1997.8878. [DOI] [PubMed] [Google Scholar]
- 17.Rose NF, Marx PA, Luckay A, Nixon DF, Moretto WJ, Donahoe SM, et al. An effective AIDS vaccine based on live attenuated vesicular stomatitis virus recombinants. Cell. 2001 Sep 7;106(5):539–549. doi: 10.1016/s0092-8674(01)00482-2. [DOI] [PubMed] [Google Scholar]
- 18.Bonaldo MC, Martins MA, Rudersdorf R, Mudd PA, Sacha JB, Piaskowski SM, et al. Recombinant yellow fever vaccine virus 17D expressing simian immunodeficiency virus SIVmac239 gag induces SIV-specific CD8+ T-cell responses in rhesus macaques. J Virol. 2010 Apr;84(7):3699–3706. doi: 10.1128/JVI.02255-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonaldo MC, Mello SM, Trindade GF, Rangel AA, Duarte AS, Oliveira PJ, et al. Construction and characterization of recombinant flaviviruses bearing insertions between E and NS1 genes. Virol J. 2007;4:115. doi: 10.1186/1743-422X-4-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robert-Guroff M. Replicating and non-replicating viral vectors for vaccine development. Curr Opin Biotechnol. 2007 Dec;18(6):546–556. doi: 10.1016/j.copbio.2007.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Plotkin SA, Reef S. Rubella Vaccine. In: Plotkin SA, Orenstein WA, editors. Vaccines. 4th ed. Philadelphia: Saunders; 2004. pp. 707–743. [Google Scholar]
- 22.Watson JC, Hadler SC, Dykewicz CA, Reef S, Phillips L. Measles, mumps, and rubella--vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 1998 May 22;47(RR-8):1–57. [PubMed] [Google Scholar]
- 23.Pugachev KV, Abernathy ES, Frey TK. Improvement of the specific infectivity of the rubella virus (RUB) infectious clone: determinants of cytopathogenicity induced by RUB map to the nonstructural proteins. J Virol. 1997 Jan;71(1):562–568. doi: 10.1128/jvi.71.1.562-568.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pugachev KV, Galinski MS, Frey TK. Infectious cDNA clone of the RA27/3 vaccine strain of Rubella virus. Virology. 2000 Jul 20;273(1):189–197. doi: 10.1006/viro.2000.0408. [DOI] [PubMed] [Google Scholar]
- 25.Spadaccini A, Virnik K, Ni Y, Prutzman K, Berkower I. Stable expression of a foreign protein by a replication-competent rubella viral vector. Vaccine. 2010 Feb 3;28(5):1181–1187. doi: 10.1016/j.vaccine.2009.11.037. [DOI] [PubMed] [Google Scholar]
- 26.Tzeng WP, Chen MH, Derdeyn CA, Frey TK. Rubella virus DI RNAs and replicons: requirement for nonstructural proteins acting in cis for amplification by helper virus. Virology. 2001 Oct 10;289(1):63–73. doi: 10.1006/viro.2001.1088. [DOI] [PubMed] [Google Scholar]
- 27.Tzeng WP, Frey TK. Complementation of a deletion in the rubella virus p150 nonstructural protein by the viral capsid protein. J Virol. 2003 Sep;77(17):9502–9510. doi: 10.1128/JVI.77.17.9502-9510.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pugachev KV, Tzeng WP, Frey TK. Development of a rubella virus vaccine expression vector: use of a picornavirus internal ribosome entry site increases stability of expression. J Virol. 2000 Nov;74(22):10811–10815. doi: 10.1128/jvi.74.22.10811-10815.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parkman PD, Phillips PE, Kirschstein RL, Meyer HM., Jr Experimental rubella virus infection in the rhesus monkey. J Immunol. 1965 Oct;95(4):743–752. [PubMed] [Google Scholar]
- 30.Kujala P, Ahola T, Ehsani N, Auvinen P, Vihinen H, Kaariainen L. Intracellular distribution of rubella virus nonstructural protein P150. J Virol. 1999 Sep;73(9):7805–7811. doi: 10.1128/jvi.73.9.7805-7811.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Purtscher M, Trkola A, Gruber G, Buchacher A, Predl R, Steindl F, et al. A broadly neutralizing human monoclonal antibody against gp41 of human immunodeficiency virus type 1. AIDS Res Hum Retroviruses. 1994 Dec;10(12):1651–1658. doi: 10.1089/aid.1994.10.1651. [DOI] [PubMed] [Google Scholar]
- 32.Stiegler G, Kunert R, Purtscher M, Wolbank S, Voglauer R, Steindl F, et al. A potent cross-clade neutralizing human monoclonal antibody against a novel epitope on gp41 of human immunodeficiency virus type 1. AIDS Res Hum Retroviruses. 2001 Dec 10;17(18):1757–1765. doi: 10.1089/08892220152741450. [DOI] [PubMed] [Google Scholar]
- 33.Allen TM, Mothe BR, Sidney J, Jing P, Dzuris JL, Liebl ME, et al. CD8(+) lymphocytes from simian immunodeficiency virus-infected rhesus macaques recognize 14 different epitopes bound by the major histocompatibility complex class I molecule mamu-A*01: implications for vaccine design and testing. J Virol. 2001 Jan;75(2):738–749. doi: 10.1128/JVI.75.2.738-749.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Loffredo JT, Sidney J, Wojewoda C, Dodds E, Reynolds MR, Napoe G, et al. Identification of seventeen new simian immunodeficiency virus-derived CD8+ T cell epitopes restricted by the high frequency molecule, Mamu-A*02, and potential escape from CTL recognition. J Immunol. 2004 Oct 15;173(8):5064–5076. doi: 10.4049/jimmunol.173.8.5064. [DOI] [PubMed] [Google Scholar]
- 35.Sacha JB, Giraldo-Vela JP, Buechler MB, Martins MA, Maness NJ, Chung C, et al. Gag- and Nef-specific CD4+ T cells recognize and inhibit SIV replication in infected macrophages early after infection. Proc Natl Acad Sci U S A. 2009 Jun 16;106(24):9791–9796. doi: 10.1073/pnas.0813106106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Froshauer S, Kartenbeck J, Helenius A. Alphavirus RNA replicase is located on the cytoplasmic surface of endosomes and lysosomes. J Cell Biol. 1988 Dec;107(6 Pt 1):2075–2086. doi: 10.1083/jcb.107.6.2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee JY, Marshall JA, Bowden DS. Replication complexes associated with the morphogenesis of rubella virus. Arch Virol. 1992;122(1–2):95–106. doi: 10.1007/BF01321120. [DOI] [PubMed] [Google Scholar]
- 38.Liang Y, Gillam S. Rubella virus RNA replication is cis-preferential and synthesis of negative- and positive-strand RNAs is regulated by the processing of nonstructural protein. Virology. 2001 Apr 10;282(2):307–319. doi: 10.1006/viro.2001.0862. [DOI] [PubMed] [Google Scholar]
- 39.Berzofsky J, Berkower IJ. Immunogenicity and Antigen Structure. In: Paul WE, editor. Fundamental immunology. 6th ed. Philadelphia: Wolters Kluwer / Lippincott Williams & Wilkins; 2008. pp. 631–683. [Google Scholar]
- 40.Frey TK. Molecular biology of rubella virus. Adv Virus Res. 1994;44:69–160. doi: 10.1016/S0065-3527(08)60328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nelson JD, Brunel FM, Jensen R, Crooks ET, Cardoso RM, Wang M, et al. An affinity- enhanced neutralizing antibody against the membrane-proximal external region of human immunodeficiency virus type 1 gp41 recognizes an epitope between those of 2F5 and 4E10. J Virol. 2007 Apr;81(8):4033–4043. doi: 10.1128/JVI.02588-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Montero M, van Houten NE, Wang X, Scott JK. The membrane-proximal external region of the human immunodeficiency virus type 1 envelope: dominant site of antibody neutralization and target for vaccine design. Microbiol Mol Biol Rev. 2008 Mar;72(1):54–84. doi: 10.1128/MMBR.00020-07. table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Verkoczy L, Diaz M, Holl TM, Ouyang YB, Bouton-Verville H, Alam SM, et al. Autoreactivity in an HIV-1 broadly reactive neutralizing antibody variable region heavy chain induces immunologic tolerance. Proc Natl Acad Sci U S A. 2010 Jan 5;107(1):181–186. doi: 10.1073/pnas.0912914107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mothe BR, Horton H, Carter DK, Allen TM, Liebl ME, Skinner P, et al. Dominance of CD8 responses specific for epitopes bound by a single major histocompatibility complex class I molecule during the acute phase of viral infection. J Virol. 2002 Jan;76(2):875–884. doi: 10.1128/JVI.76.2.875-884.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vogel TU, Friedrich TC, O'Connor DH, Rehrauer W, Dodds EJ, Hickman H, et al. Escape in one of two cytotoxic T-lymphocyte epitopes bound by a high-frequency major histocompatibility complex class I molecule, Mamu-A*02: a paradigm for virus evolution and persistence? J Virol. 2002 Nov;76(22):11623–11636. doi: 10.1128/JVI.76.22.11623-11636.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Levine BL, Humeau LM, Boyer J, MacGregor RR, Rebello T, Lu X, et al. Gene transfer in humans using a conditionally replicating lentiviral vector. Proc Natl Acad Sci U S A. 2006 Nov 14;103(46):17372–17377. doi: 10.1073/pnas.0608138103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ploegh HL. Viral strategies of immune evasion. Science. 1998 Apr 10;280(5361):248–253. doi: 10.1126/science.280.5361.248. [DOI] [PubMed] [Google Scholar]
- 48.Phogat S, Svehla K, Tang M, Spadaccini A, Muller J, Mascola J, et al. Analysis of the human immunodeficiency virus type 1 gp41 membrane proximal external region arrayed on hepatitis B surface antigen particles. Virology. 2008 Mar 30;373(1):72–84. doi: 10.1016/j.virol.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Berkower I, Spadaccini A, Chen H, Al-Awadi D, Muller J, Gao Y, et al. Hepatitis B virus surface antigen assembly function persists when entire transmembrane domains 1 and 3 are replaced by a heterologous transmembrane sequence. J Virol. 2011 Mar;85(5):2439–2448. doi: 10.1128/JVI.02061-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.