Abstract
Objective Frontobasal fractures are relatively common traumas but surgical indications are still discussed. The authors report their results on patients showing anterior cranial fossa fractures; clinical data, surgical indications, and results are reported and critically analyzed.
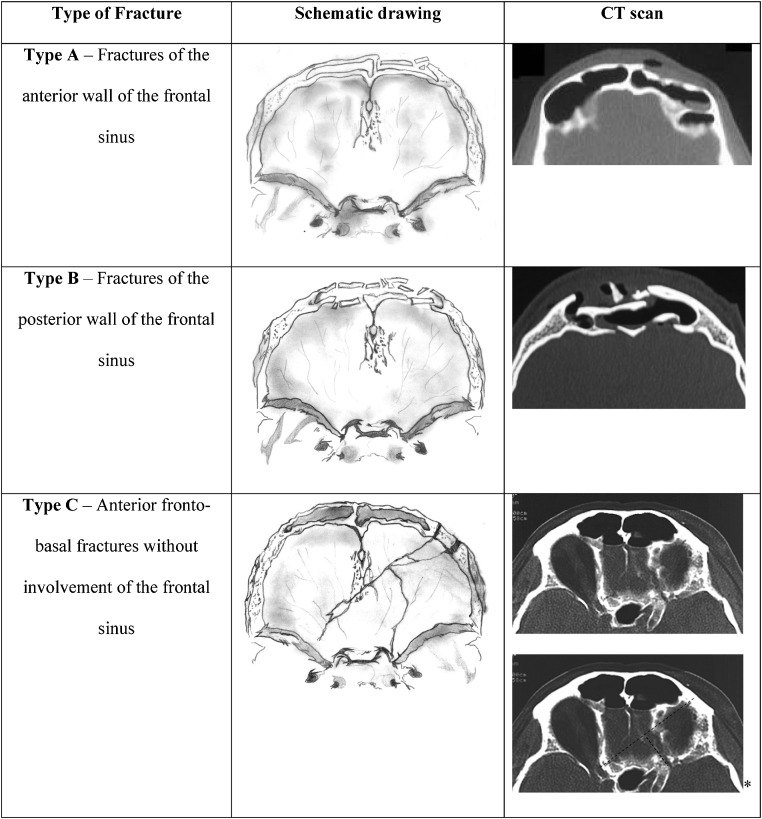
Methods From 1991 to 2010, 223 patients were admitted in our institution with diagnosis of anterior cranial fossa fracture. Fractures were classified as type A—fracture of the anterior wall of the frontal sinus; type B—fracture of the posterior wall of the frontal sinus; and type C—frontobasal traumas without involvement of the frontal sinus. All patients entered a follow-up program consisting in periodic controls.
Results A total of 105 patients were conservatively treated, while 118 patients underwent surgical intervention. The presence of pneumocephalus (p < 0.0001) and rhinoliquorrhea (p = 0.001) were the factors influencing the surgical indication. In the fractures of group B with signs of pneumocephalus and or rhinoliquorrhea, full sinus cranialization represents the variable mainly influencing the outcome (p < 0.001).
Conclusion Patients with frontobasal traumas should be carefully evaluated to choose the best treatment option. Clinical and radiological data suggest that patients with frontobasal fractures with massive pneumocephalus and/or rhinoliquorrhea should be always surgically treated.
Keywords: anterior cranial fossa, skull base fracture, head trauma, trauma
Introduction
Head injuries are one of the most common causes of treatment in the emergency and accidents ward. The first causes of head traumatology are still car or motorcycle accidents, followed by personal aggressions.1,2 Anterior skull base fractures are one of the most frequent consequences of head injury. This may present as bone fractures with or without intracranial involvement (epidural/subdural/intraparenchymal hematomas, cerebral contusion, or dural laceration).
Anterior intracranial base is formed by the ethmoid, sphenoid, and frontal bones. Due to anatomical, clinical, and radiological consideration, it has been divided in medial and lateral regions. Medial portion is formed by the cribriform plate of the ethmoid bone anteriorly and the planum of the sphenoid body posteriorly; its anterior limit is composed by the posterior wall of the frontal sinus. The lateral portion, which covers the orbit and the optic canal, is formed by the frontal bone and the lesser wing of the sphenoid bone, which blends medially into the anterior clinoid process.3 Several classifications of fractures of the frontal cranial base have been reported in the literature,4,5,6,7,8,9,10,11 but all series seem similar in one important point: the presence of fractures of anterior sinus wall, posterior sinus wall, and/or fronto-nasal duct are determinant for the choice of surgical treatment.12
Due to the complexity of anatomical relationships, these pathologies should be approached by a multidisciplinary team composed by a maxillofacial surgeon and a neurosurgeon.
Surgical treatment of anterior skull base fractures is still debated. As far as the necessity for a treatment of a displaced fracture of the anterior wall is doubtlessly accepted, there is no agreement in the literature on indications for treatment of displaced or nondisplaced posterior wall fractures. In the present study, the authors perform a retrospective analysis of their experience both for patients who underwent surgery and the ones who were conservatively treated, to define and highlight the indications for the best treatment option for anterior frontobasal fractures.
Materials and Methods
The authors reviewed all clinical data of the patients with traumatic head injury and anterior frontobasal fractures that came to their observation from January 1991 to December 2010, in Policlinico Umberto I, University of Rome “Sapienza.” Only pure frontobasal injuries were considered and were defined as fractures confined to the anterior cranial fossa; patients with brain swelling, intracranial hematoma, or neurological impairment were excluded from this group.
A total number of 223 patients were observed; out of this, 105 patients underwent only clinical observation, while 118 patients were treated with surgical intervention. All patients were studied with computed tomography (CT) scan with axial, sagittal, and coronal reconstruction. Base on clinical, radiological, and surgical considerations, we divided population into three main types (Fig. 1).
Figure 1.
Classification of anterior frontobasal traumas. *Sectioned lines indicate the curse of fracture on computed tomography scan.
Type A: Fractures of the anterior wall of the frontal sinus. This group includes only patients with fracture confined to the anterior wall of the frontal sinus, with or without extension to another bone segment of the anterior cranial fossa, but without any impairment of the ethmoid bone and without any extension to the posterior wall of the frontal sinus.
Type B: Fractures of the anterior and posterior wall of the frontal sinus.
Type C: Anterior frontobasal fractures without involvement of the frontal sinus.
Retrospective analysis was performed on the three groups.
All patients entered a follow-up program consisting in periodic clinical controls at 2 weeks, 1 month, 6 months, and once a year for 3 years from surgery. All patients underwent a pre- and postoperative CT scan evaluation with three-dimensional reconstruction of the examination.
A multivariate statistical analysis has been performed (Fisher's exact test – JMP 5.1) comparing the clinical and radiological findings on the three groups. Primarily, the following signs were considered: the signs of abundant and persistent (>7 days) cerebrospinal fluid (CSF) leakage (rhinorrhea), presence of fracture displacement (>2 mm) and/or pneumocephalus on CT scan.
Results
Since 1991 to 2010, a total number of 223 patients with pure fronto-basal fractures came to our observation. Out of this, 105 patients underwent only clinical observation and follow-up, while 118 patients were treated with surgical intervention.
Clinical and radiological data are reported in Table 1.
Table 1. Clinical and Radiological Data of Patients with Pure Fronto-Basal Fractures.
| No Surgery | Surgery | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinic | CT Scan Findings | Age—Years (Range) | Sex | No. of Cases | Groups | No. of Cases | Sex | Age—Years (Range) | CT Scan Findings | Clinic | ||
| Signs of CSF Fistula | Intracranial Air | Fracture Displacement | 41 (9–75) | 33 M; 9 F | 46 | A | 37 | 26 M; 9 F | 32 (12–67) | Fracture Displacement | Intracranial Air | Signs of CSF Fistula |
| No | 0 | 1 | 35 | 0 | 0 | |||||||
| No | 0 | 0 | 41 (13–79) | 25 M; 8 F | 36 | B | 55 | 49 M; 6 F | 35 (18–77) | 40 | 35 | 10 |
| No | 0 | 2 | 40 (18–83) | 24 M; 6 F | 23 | C | 26 | 25 M; 3 F | 31 (14–69) | 22 | 6 | 8 |
| 105 | Total | 118 | ||||||||||
Group A counted 83 patients overall, 91 patients were included in group B, and 49 patients showed group C fractures.
Conservative Treatment
The mean age of the patients was 41 years old (range 9 to 83 years); 82 patients were males (78%) and 23 females (22%). Group A counted 46 patients, group B 36, and group C 23.
The 46 patients of group A showed anterior frontal sinus fracture but no radiological signs of displacement and aesthetic deformity; they underwent bed rest, clinical observation, and symptomatic analgesic therapy.
Group B included 36 patients with linear or slightly displaced fracture (<2 mm) of the posterior wall of the frontal sinus, with no signs of pneumocephalus and/or rhinoliquorrhea; they were treated with bed rest, clinical observation, and symptomatic analgesic therapy.
The 23 patients of group C were treated the same way, that is, bed rest, clinical observation, and symptomatic analgesic therapy; no signs of pneumocephalus and or rhinoliquorrhea were observed in this group. There was no postinjury mortality. The median overall hospital stay was of 4 days ranging from 3 to 8. The following cases of morbidity were found: one case of scar retraction, one case of paresthesia along the V1 trigeminal branch, eight cases of anosmia, and spontaneously regressed in four patients at follow-up.
Surgery Group
The mean age of patients of the surgical group was 31.8 years old (range 12 to 77 years); 100 patients were males (84.7%) and 18 females (13.3%). Group A counted 37 patients, group B counted 55 patients, and group C counted 26 patients.
Skin incisions were divided as follows: 78 coronal incisions, 22 through an existing laceration, 10 emicoronal incisions, 6 eyebrow accesses, and 2 temporal incisions. Internal rigid fixation (titanium plates and screws) was used in every case except for patients in pediatric age; in these cases, reabsorbable devices were adopted.13
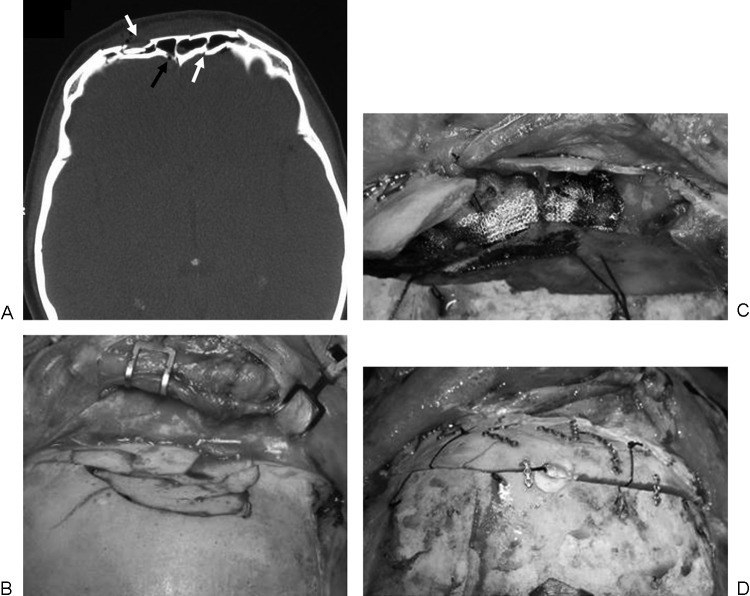
Patients of group A were treated with the reconstruction of anterior wall of the frontal sinus. When tear skin was present, we preferred to expose the fracture rim trough the existing wound; otherwise, we performed a bicoronal approach with wide exposition of the frontal bone. Every fracture has been reduced and fixed with titanium plates and screws (Fig. 2).
Figure 2.
Type A—Illustrative case: a 43-year-old man with fracture of the anterior wall of the frontal sinus. (a, b) Axial computed tomography (CT) scan and sagittal CT reconstruction show fracture of the anterior wall of the frontal sinus (white arrows) without evolvement of the posterior wall; (c) intraoperative findings: a bone graft taken from the mandible was placed to repair the fracture; (d) postoperative CT scan showing surgical repair of the anterior wall of the frontal sinus.
Group B included 55 patients with fracture of the posterior wall of the frontal sinus; in all these patients there was evidence of one or more these findings: pneumocephalus, rhinoliquorrhea, displaced fracture. At the time of diagnosis, four patients showed CSF signs and/or displaced fractures (>2 mm), but it was attempted to treat them conservatively; all these patients were subsequently readmitted in our hospital with signs of persistent CSF fistula and also meningitis in three of them. They were all treated with surgical intervention.14
Patients of group B have been mostly approached with the coronal incision. Among those patients, 35 presented pneumocephalus at CT scan, 10 had rhinorrhea, and 15 showed both these findings. From 1991 to 2000, 26 patients underwent surgery; at that time, a wide frontal craniotomy was preferred to approach the posterior wall of the frontal sinus. From 2001 to 2010, 29 patients were treated with frontal craniotomy, while 9 patients were treated with a subcranial transsinusal Raveh approach to avoid retraction on the brain tissue.15,16,17 All these patients presented dura mater lining that was treated with suture, dural suspensions, Membrane evolution Tecnoss® (Tecnoss Medical Products, Turin, Italy) and fibrin glue (Tissucol; Baxter International, Deerfield, IL, USA). Since 2004, we replaced the previous bovine dura patch with the new one (i.e., Membrane evolution Tecnoss®) of equine nature to prevent CSF leaks. Galea pericranium sliding flap and Tissucol were used to perform frontal sinus cranialization and obliteration of the frontonasal duct, as reported in a previous report18 and in several works.19
Illustrative Case
A 45-year-old woman after a car accident showed displaced fracture of type B and signs of pneumocephalus on CT scan. She underwent surgical intervention with full sinus exposition, cranialization and fractures repair (Fig. 3).
Figure 3.
Type B—Illustrative case: a 45-year-old woman with fracture of anterior and posterior wall of the frontal sinus due to a frontal trauma in a car accident. (a) Axial computed tomography scan shows combined fractures of anterior and posterior walls of the frontal sinus (white arrows) with signs of pneumocephalus (black arrow); (b) intraoperative findings: fractures of the anterior wall of the frontal sinus; (c) wide exposition of the frontal sinus before its cranialization; (d) final surgical field; fractures were treated with microplates and screws.
Patients of group C had pneumocephalus in 14 cases, rhinoliquorrhea in 15 cases, both of them in 11 cases, displaced fractures in 22 cases; all these patients have been treated with a bicoronal craniotomy. Patients without any sign of CSF leakage were treated mainly for optic nerve compression or displacement of bone fragment on the brain tissue.
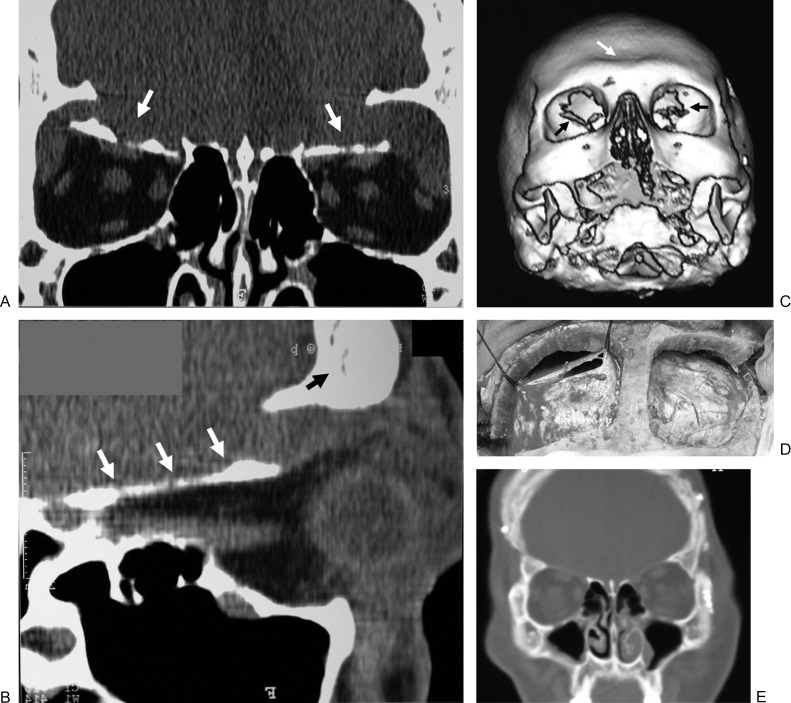
Illustrative Case
A 22-year-old man with motor car accident came to our observation complaining bilateral amaurosis; CT scan showed bilateral orbital blow-in fractures. Surgical intervention with coronal skin incision and two emicoronal craniotomies was performed. In this case, orbital roofs have been removed with decompression of the orbit and no further reconstruction has been performed. Patient showed a recovery of 5/10 for the right orbit and 7/10 for the left orbit after 5 months from surgery (Fig. 4).
Figure 4.
Type C—Illustrative case: a 22-year-old man with bilateral fractures of the orbital roof and a little parietal fracture. (a) Coronal computed tomography (CT) scan showing bilateral depression of the orbital roof (white arrows); (b) sagittal CT reconstruction showing fracture of the orbital roof (white arrows) without evolvement of the frontal sinus (black arrow); (c) three-dimensional reconstruction showing bilateral dislocation of the orbital roof (black arrows) without fracture of the anterior wall of the frontal sinus (white arrow); (d) intraoperative field: bone fragments have been removed, dural laceration was repaired and suspended; (e) postoperative CT scan.
In 20 patients, frontal sinus was preserved to avoid consequent reconstructive maneuvers and increasing risk of infection; however, in the remnant eight patients, due to the large size of the sinus, it was opened and cranialized.
Patients were dismissed within a median period of 5 days, ranging from 3 to 8 days. There was no perioperative mortality. Follow-up controls documented that 107/118 patients showed no complications after 6 months, 1 year, 2, and 3 years. Early postoperative CT scans showed obliteration of the frontal sinus and good reduction of the fractures without any pathological sing.
A total of 11 patients presented the following complications. Of this, two patients complained rhinorrhea, despite cranialization of frontal sinus; they were treated with a second surgical intervention, which showed the presence of unsatisfactory dural closure with CSF fistula. One case of scar retraction; two cases of extrinsic muscles of the eye impairment were also noted; four patients presented with anosmia that regressed spontaneously in four of them with a mean period of 1 year; one patient presented a posttraumatic insipid diabetes, treated with antidiuretic hormone; his symptoms showed a complete regression after 4 days; and last one patient presented epifora.
Discussion
The first step in the treatment of anterior skull base trauma or upper third fractures is to perform an accurate clinical evaluation. A primary inspection of forehead integrity should be performed. The surgeon should look for hematomas or skin laceration, evaluate bone integrity by observing any possible bone deformity or tenderness, fragments mobility, or periorbital edema.20 A characteristic clinical sign is the periorbital hematoma also known as “raccoon eyes”; it is associated with anterior skull base fractures in more than 70% of cases.21 The clinical inspection must always test the presence of rhinoliquorrhea, also making the patient bend the head forward. The β2 transferrin test is helpful to obtain a certain differential diagnosis from mucous or serous secretions from the nose. X-rays imaging could be a useful step in diagnosis of anterior skull base but, although used in the past, today we almost abandoned them, preferring CT scan, which shows a better resolution for the study of pneumocephalus, fracture rim, and nervous structures compression.
Anterior skull base traumas' treatment is still object of many controversies. In the international literature, there is no agreement on guidelines for conservative or surgical indications and approaches. The crucial point is whether to treat or not an anterior skull base fracture even if favorable without any trace of cerebral involvement.
According to fractures type A, the main reason for surgical treatment is the patient's face aesthetic reconstruction, which has to be performed in the great majority of displaced fractures. The simple fracture of the anterior wall of the frontal sinus, if linear, can be treated conservatively without a surgical intervention.
For patients of group B, some authors assess that nondisplaced posterior wall fractures can be treated conservatively with antibiotic therapy and closed follow-up10,12 and this is exactly our conduct. Conversely, patients with displaced fractures, signs of pneumocephalus and/or rhinoliquorrhea show high risk of posttraumatic infections and should be promptly treated with surgical intervention and antibiotic therapy. As shown in the results section, four patients were initially discharged then readmitted with signs of rhinoliquorrhea and also meningitis in three of them.14
Dealing with this aspect, we use to perform a surgical treatment with frontal sinus cranialization in all patients with these signs. Our experience suggests that some patients can show symptoms of CSF fistula after a variable period from the trauma. In a previous work, our team reported that 50 to 85% of traumatic CSF fistulae occurring within 48 hours after injury cease spontaneously14,22,23,24; however, dural tear could not be definitely sealed and recurrent rhinorrhea or late intracranial infections may develop.14,25,26,27,28,29 It seems possible that dural tissue, previously impaired for a traumatic stretching due to sudden dislocation of the frontal bone, could lacerate as a consequence of efforts or little traumas after the first surgical intervention. Delayed or recurrent CSF rhinorrhea almost never stops without operative treatment and the risk of meningitis becomes higher.14,23,24,30,31 In our opinion, surgical treatment described should be always performed even in nondisplaced fractures when CT findings of pneumocephalus are present because they are highly predictive of dural laceration; in the previous report, we also proposed a treatment algorithm for posttraumatic fistula management.14 According to our experience, after frontal sinus cranialization, to avoid the risk of infection, it is mandatory to change all the operative tools previously used before dural opening and suture.
In patients of group C, surgical treatment is reserved for those fractures that are displaced and/or when patients show sings of rhinorrhea or hypertensive pneumocephalus. All patients included in the present study showed one or both these findings. In the majority of these patients, frontal sinus was preserved. Our experience suggests that frontal sinus has to be opened only when it seems too wide to avoid its invasion; in this case, full cranialization is mandatory.
The access to the fractures of the anterior skull base poses a challenge to the surgeon. Some classic approaches to lesions of the anterior skull base have been described by Ketcham et al, who reported, in 1963, a combination of the transfrontal and the transfacial approaches. This approach is preferable when fracture shows a big diastasis and a wider exposition is required; however, when brain parenchyma is intact, the intracranial approach is characterized by stressing maneuvers on the frontal lobes; some existing risks related to this approach are postoperative brain swelling and/or contusion and frontal lobe retraction.32,33
The subcranial approach instead has proved to be a safe and effective method treating complex frontobasal fractures giving an access that is quick to realize and that provides a wide visibility of the anterior skull base.14,15,16,34,35 It allows to widely expose the posterior wall of the frontal sinus avoiding traumatisms of the cerebral tissue but, as we said before, it should not be performed when sinus is not well represented or when fracture is extended or associated with significant intracranial hematomas.
Conclusion
Concluding, in patients with frontobasal traumas it is mandatory to estimate the necessity of a surgical intervention. Main complications of frontobasal fractures are CSF fistula and/or infections; both these risks seem to be higher if the posterior wall of the frontal sinus is involved (group B). Radiological and clinical signs of fracture of the posterior wall of the frontal sinus should be carefully considered and treated with full cranialization of the frontal sinus. Isolated fractures of the anterior wall of the frontal sinus (group A) require only reduction for aesthetic issues. When frontobasal fractures show no involvement of the frontal sinus (group C) surgeon should not open it, if possible and according to its size, to avoid the risks of infections.
Acknowledgments
The authors would like to thank Silvia Anichini, who is the author of the drawings in Fig. 1. The authors would also dedicate the present work to the memory of our colleague, teacher, and friend Giovanni Rocchi, died on February 13, 2009, who dedicated his life to head trauma and treated almost half of the patients of the present series.
References
- 1.Rocchi G, Fadda M T, Marianetti T M, Reale G, Iannetti G. Craniofacial trauma in adolescents: incidence, etiology, and prevention. J Trauma. 2007;62(2):404–409. doi: 10.1097/01.ta.0000197627.05242.a4. [DOI] [PubMed] [Google Scholar]
- 2.Servadei F, Verlicchi A, Soldano F, Zanotti B, Piffer S. Descriptive epidemiology of head injury in Romagna and Trentino. Comparison between two geographically different Italian regions. Neuroepidemiology. 2002;21(6):297–304. doi: 10.1159/000065523. [DOI] [PubMed] [Google Scholar]
- 3.Rhoton A L. The anterior and middle cranial base. Neurosurgery. 2002;51(4, Suppl):S273–S302. [PubMed] [Google Scholar]
- 4.Buitrago-Téllez C H, Schilli W, Bohnert M, Alt K, Kimmig M. A comprehensive classification of craniofacial fractures: postmortem and clinical studies with two- and three-dimensional computed tomography. Injury. 2002;33(8):651–668. doi: 10.1016/s0020-1383(02)00119-5. [DOI] [PubMed] [Google Scholar]
- 5.Gerbino G, Roccia F, Benech A, Caldarelli C. Analysis of 158 frontal sinus fractures: current surgical management and complications. J Craniomaxillofac Surg. 2000;28(3):133–139. doi: 10.1054/jcms.2000.0134. [DOI] [PubMed] [Google Scholar]
- 6.Ioannides C Freihofer H P Vrieus J Friens J [corrected to Vrieus J]. Fractures of the frontal sinus: a rationale of treatment Br J Plast Surg 1993463208–214. [DOI] [PubMed] [Google Scholar]
- 7.Lee T T, Ratzker P A, Galarza M, Villanueva P A. Early combined management of frontal sinus and orbital and facial fractures. J Trauma. 1998;44(4):665–669. doi: 10.1097/00005373-199804000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Madhusudan G, Sharma R K, Khandelwal N, Tewari M K. Nomenclature of frontobasal trauma: a new clinicoradiographic classification. Plast Reconstr Surg. 2006;117(7):2382–2388. doi: 10.1097/01.prs.0000218794.28670.07. [DOI] [PubMed] [Google Scholar]
- 9.Manson P N, Stanwix M G, Yaremchuk M J, Nam A J, Hui-Chou H, Rodriguez E D. Frontobasal fractures: anatomical classification and clinical significance. Plast Reconstr Surg. 2009;124(6):2096–2106. doi: 10.1097/PRS.0b013e3181bf8394. [DOI] [PubMed] [Google Scholar]
- 10.Rohrich R J, Hollier L H. Management of frontal sinus fractures. Changing concepts. Clin Plast Surg. 1992;19(1):219–232. [PubMed] [Google Scholar]
- 11.Wilson B C, Davidson B, Corey J P, Haydon R C. Comparison of complications following frontal sinus fractures managed with exploration with or without obliteration over 10 years. Laryngoscope. 1988;98(5):516–520. doi: 10.1288/00005537-198805000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Yavuzer R Sari A Kelly C P et al. Management of frontal sinus fractures Plast Reconstr Surg 2005115679e–93e., discussion 94e–95e [DOI] [PubMed] [Google Scholar]
- 13.Clauser L, Dallera V, Sarti E, Tieghi R. Frontobasilar fractures in children. Childs Nerv Syst. 2004;20(3):168–175. doi: 10.1007/s00381-003-0868-0. [DOI] [PubMed] [Google Scholar]
- 14.Rocchi G Caroli E Belli E Salvati M Cimatti M Delfini R Severe craniofacial fractures with frontobasal involvement and cerebrospinal fluid fistula: indications for surgical repair Surg Neurol 2005636559–563., discussion 563–564 [DOI] [PubMed] [Google Scholar]
- 15.Raveh J, Laedrach K, Speiser M. et al. The subcranial approach for fronto-orbital and anteroposterior skull-base tumors. Arch Otolaryngol Head Neck Surg. 1993;119(4):385–393. doi: 10.1001/archotol.1993.01880160029006. [DOI] [PubMed] [Google Scholar]
- 16.Raveh J, Vuillemin T. The surgical one-stage management of combined cranio-maxillo-facial and frontobasal fractures. Advantages of the subcranial approach in 374 cases. J Craniomaxillofac Surg. 1988;16(4):160–172. doi: 10.1016/s1010-5182(88)80042-8. [DOI] [PubMed] [Google Scholar]
- 17.Raveh J, Vuillemin T, Sutter F. Subcranial management of 395 combined frontobasal-midface fractures. Arch Otolaryngol Head Neck Surg. 1988;114(10):1114–1122. doi: 10.1001/archotol.1988.01860220048022. [DOI] [PubMed] [Google Scholar]
- 18.Caroli E, Rocchi G, D'Andrea G, Delfini R. Management of the entered frontal sinus. Neurosurg Rev. 2004;27(4):286–288. doi: 10.1007/s10143-004-0335-8. [DOI] [PubMed] [Google Scholar]
- 19.Donath A, Sindwani R. Frontal sinus cranialization using the pericranial flap: an added layer of protection. Laryngoscope. 2006;116(9):1585–1588. doi: 10.1097/01.mlg.0000232514.31101.39. [DOI] [PubMed] [Google Scholar]
- 20.Katzen J T, Jarrahy R, Eby J B, Mathiasen R A, Margulies D R, Shahinian H K. Craniofacial and skull base trauma. J Trauma. 2003;54(5):1026–1034. doi: 10.1097/01.TA.0000066180.14666.8B. [DOI] [PubMed] [Google Scholar]
- 21.Herbella F A, Mudo M, Delmonti C, Braga F M, Del Grande J C. 'Raccoon eyes' (periorbital haematoma) as a sign of skull base fracture. Injury. 2001;32(10):745–747. doi: 10.1016/s0020-1383(01)00144-9. [DOI] [PubMed] [Google Scholar]
- 22.Griffith H B. CSF fistula and the surgeon. Br J Neurosurg. 1990;4(5):369–371. doi: 10.3109/02688699008992757. [DOI] [PubMed] [Google Scholar]
- 23.Talamonti G, Fontana R A, Versari P P. et al. Delayed complications of ethmoid fractures: a “growing fracture” phenomenon. Acta Neurochir (Wien) 1995;137(3-4):164–173. doi: 10.1007/BF02187189. [DOI] [PubMed] [Google Scholar]
- 24.Talamonti G, Fontana R, Villa F. et al. “High risk” anterior basal skull fractures. Surgical treatment of 64 consecutive cases. J Neurosurg Sci. 1995;39(3):191–197. [PubMed] [Google Scholar]
- 25.Eljamel M S. Liverpool: University of Liverpool; 1993. The Role of Surgery and h2-Transferrin in the Management of CSF Fistulas [MD thesis] pp. 207–219. [Google Scholar]
- 26.Eljamel M S, Foy P M. Post-traumatic CSF fistulae, the case for surgical repair. Br J Neurosurg. 1990;4(6):479–483. doi: 10.3109/02688699008993796. [DOI] [PubMed] [Google Scholar]
- 27.Eljamel M S, Pidgeon C N. Localization of inactive cerebrospinal fluid fistulas. J Neurosurg. 1995;83(5):795–798. doi: 10.3171/jns.1995.83.5.0795. [DOI] [PubMed] [Google Scholar]
- 28.El Gammal T, Sobol W, Wadlington V R. et al. Cerebrospinal fluid fistula: detection with MR cisternography. AJNR Am J Neuroradiol. 1998;19(4):627–631. [PMC free article] [PubMed] [Google Scholar]
- 29.Lewin W. Cerebrospinal fluid rhinorrhoea in closed head injuries. Br J Surg. 1954;42(171):1–18. doi: 10.1002/bjs.18004217102. [DOI] [PubMed] [Google Scholar]
- 30.Manelfe C, Cellerier P, Sobel D, Prevost C, Bonafé A. Cerebrospinal fluid rhinorrhea: evaluation with metrizamide cisternography. AJR Am J Roentgenol. 1982;138(3):471–476. doi: 10.2214/ajr.138.3.471. [DOI] [PubMed] [Google Scholar]
- 31.Yilmazlar S, Arslan E, Kocaeli H. et al. Cerebrospinal fluid leakage complicating skull base fractures: analysis of 81 cases. Neurosurg Rev. 2006;29(1):64–71. doi: 10.1007/s10143-005-0396-3. [DOI] [PubMed] [Google Scholar]
- 32.Ketcham A S, Wilkins R H, Vanburen J M, Smith R R. A combined intracranial facial approach to the paranasal sinuses. Am J Surg. 1963;106:698–703. doi: 10.1016/0002-9610(63)90387-8. [DOI] [PubMed] [Google Scholar]
- 33.Shah J P, Kraus D H, Bilsky M H, Gutin P H, Harrison L H, Strong E W. Craniofacial resection for malignant tumors involving the anterior skull base. Arch Otolaryngol Head Neck Surg. 1997;123(12):1312–1317. doi: 10.1001/archotol.1997.01900120062010. [DOI] [PubMed] [Google Scholar]
- 34.Fliss D M, Zucker G, Cohen J T, Gatot A. The subcranial approach for the treatment of cerebrospinal fluid rhinorrhea: a report of 10 cases. J Oral Maxillofac Surg. 2001;59(10):1171–1175. doi: 10.1053/joms.2001.26720. [DOI] [PubMed] [Google Scholar]
- 35.Kinnunen I, Aitasalo K. A review of 59 consecutive patients with lesions of the anterior cranial base operated on using the subcranial approach. J Craniomaxillofac Surg. 2006;34(7):405–411. doi: 10.1016/j.jcms.2006.04.007. [DOI] [PubMed] [Google Scholar]