Abstract
Objective The aim of this study was to assess the assumed advantage of endoscopic assistance to the standard subtemporal approach. The idea was to measure qualitatively and quantitatively visibility versus operability.
Design We performed eight subtemporal dissections on four cadaver heads. Our dissections integrated an operating microscope, endoscope, and neuronavigation. Comparison was made between visibility and operability afforded by the microscope alone or by the microscope–endoscope combination. Visibility was recorded as complete or incomplete and was quantified for key structures using linear measurements taken by the navigation system. Operability was determined by whichever maneuvers could be safely and comfortably accomplished in the space afforded.
Results From our survey, the structures whose visibility most benefitted from the addition of the endoscope include: contralateral third nerve, posterior perforated substance, mammillary bodies, and contralateral superior cerebellar artery. With regard to quantitative evaluation, we found increased visibility of both basilar artery and posterior cerebral artery. With regard to the operability, no objective advantage was afforded by the addition of the endoscope. Subjectively, the maneuvers were easier to perform while using the endoscope.
Conclusion Using the endoscope as an assistance tool during conducting classical subtemporal approach can help in overcome a lot of the classical subtemporal approach limitations.
Keywords: subtemporal, endoscope, endoscope-assisted, interpeduncular, operability
Introduction
The subtemporal approach is a classic approach commonly used in neurosurgery to access the interpeduncular fossa.1 This approach was initially used in the early 20th century for rhizotomy of the trigeminal nerve.2 This surgical route has been shown to be useful for accessing and treating a multitude of pathologies in the anterior and middle tentorial incisural spaces and has been altered to suit different surgical needs such as those encountered with retrochiasmatic craniopharyngiomas, arteriovenous malformations of the temporal lobe, anterior, or anterolateral lesions of the midbrain or pons.2,3,4,5,6,7 Although this approach has been variegated multiple times in several ways, the concept remains relatively unchanged from its inception. In 1968, Drake et al proposed this approach for treating basilar artery aneurysms and since then this indication has remained one of the most popular. Recently, endoscopic assistance has been suggested as an additive tool to augment this approach.8,9 In theory, the endoscope would allow increased exposure and surgical freedom while potentially minimizing bone resection such as the one needed in the Kawase approach.8
The aim of this study is to evaluate the visibility and operability afforded by performing the standard subtemporal approach using the endoscope–microscope combination and to compare it to the visibility and operability afforded by the microscope alone.
Materials and Methods
We used four silicone injected adult cadaveric heads. High-resolution volumetric computed tomography scans were obtained before the dissections on all the specimens. A Stryker neuronavigation system (Stryker Instruments, Kalamazoo, Michigan, USA) was also used with accompanying planning software (iNtellect Cranial, Stryker Instruments). A standard subtemporal approach was executed bilaterally in all the specimens using standard microsurgical instruments, a Moeller operating microscope, and Aesculap Hi-Definition rigid endoscope (2.7 mm) with both 0- and 30-degree lenses.
Once the exposure was completed, a comparison was made between the visibility and the operability afforded by the microscope alone or by the microscope–endoscope combination (Figs. 1–4). Visibility was determined by anatomic exposure. For structures requiring complete visibility to perform surgical manipulation, we recorded either complete visibility or incomplete visibility. The percentage of specimens in which the structure was completely visualized was recorded. For structures that can practically be operated on with only partial visibility, the visibility had to be quantified. To quantify visibility, linear measurements were taken using the navigation system. The XYZ coordinates delivered by the navigation system were then plugged into a formula, previously referenced in the reviewed literature, to determine the linear exposure.9
Figure 1.
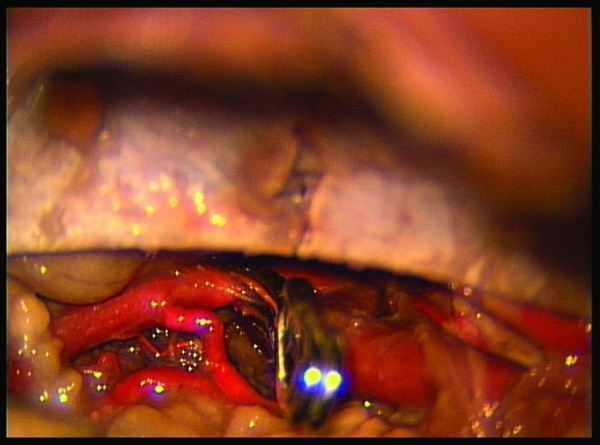
An aneurysmal clip placed on superior cerebellar artery under microscopic vision.
Figure 2.
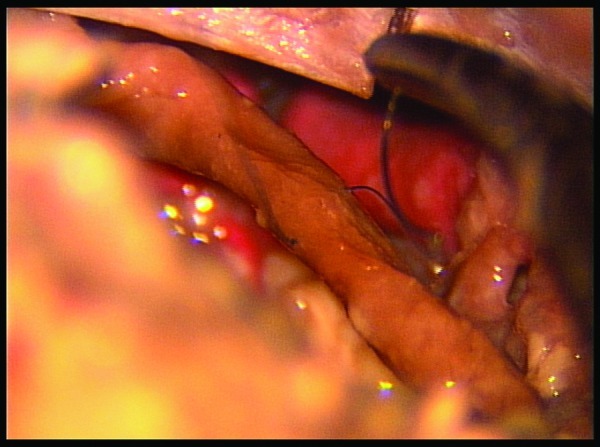
Suture thrown in cranial nerve III under microscopic vision.
Figure 3.
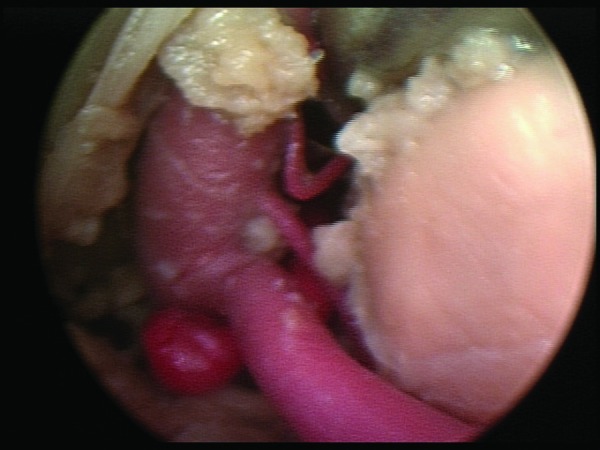
Basilar tip aneurysm seen under endoscopic vision.
Figure 4.
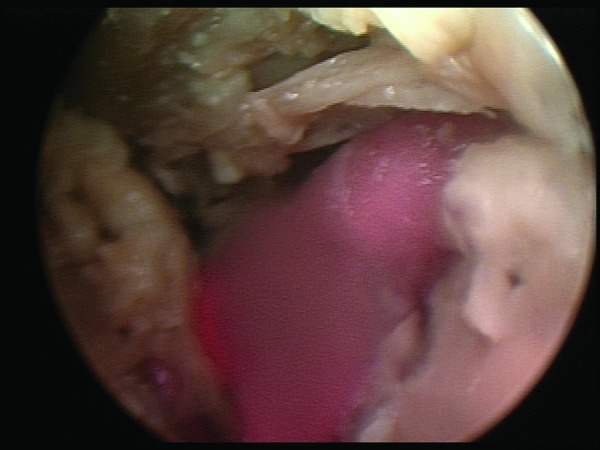
Cranial nerve IV easily seen with the endoscope.
The same determining factors were used to assess the visibility afforded by the addition of the endoscope. The measurements taken using the endoscope were done with both 0- and 30-degree rod lenses. Both video and digital images were taken to document dissections.
Surgical maneuverability was assessed in a manner similar to that done in several previous publications.6,7,8,9,10 That is, whichever maneuvers could be safely and comfortably accomplished in the space afforded by the microscope or the endoscope.
Results
From our survey, the structures that most benefitted from the addition of the endoscope include the contralateral third nerve, the posterior perforated substance, the mammillary bodies, and the contralateral superior cerebellar artery (Tables 1 and 2).
Table 1. Visibility.
| Structure | Without Endoscope | 0 Degree | 30 Degree |
|---|---|---|---|
| Basilar | 12.395 mm | 19.618 mm | 22.526 mm |
| Posterior cerebral artery | 17.042 mm | 22.613 mm | 24.309 mm |
| Ipsilateral third nerve | 100% seen | 100% seen | 100% seen |
| Contralateral third nerve | 0% seen | 100% seen | 100% seen |
| Mammillary bodies | 0% seen | 100% seen | 100% seen |
| Posterior perforated substance | 0% seen | 62.5% seen | 87.5% seen |
| Ipsilateral superior cerebellar artery | 50% seen | 87.5% seen | 100% seen |
| Contralateral superior cerebellar artery | 37.5% seen | 87.5% seen | 100% seen |
Table 2. Surgical Maneuverability.
| Structure | Without Endoscope | 0 Degree | 30 Degree |
|---|---|---|---|
| Basilar artery clipping | 100% | 100% | 100% |
| Ipsilateral posterior communicating artery clipping | 100% | 100% | 100% |
| Contralateral posterior communicating artery clipping | 100% | 100% | 100% |
| Ipsilateral posterior cerebral artery clipping | 100% | 100% | 100% |
| Contralateral posterior cerebral artery clipping | 100% | 100% | 100% |
| Third nerve suture | 100% | 100% | 100% |
With regard to quantitative evaluation, we chose to measure the linear exposure imparted by the microscope (the usual method of the subtemporal approach) and that obtained by the addition of the endoscope using the 0- and 30-degree lenses. The result was increased visibility of both the basilar artery and the posterior cerebral artery (Table 2).
Regarding the basilar artery, linear exposure with the 0-degree endoscope was on average 58.27% greater than that without the endoscope. The addition of the 30-degree endoscope increased linear exposure by 81.7% as compared with the traditional view with the microscope (Table 2).
Concerning the posterior cerebral artery, the linear exposure afforded by the 0-degree endoscope is 32.7% greater than that without it. That afforded by the 30-degree endoscope is 42.6% greater than with the microscope alone (Table 2).
The advantages of the addition of the endoscope were not as pronounced with regard to the operability. Concerning the capacity to actually perform the functions tested, there seemed to be no extra advantage afforded by the addition of the endoscope whether the 0 degree or the 30 degrees.
Subjectively, though, the authors felt that the maneuvers were easier to perform while using the endoscope. With the endoscope, utilizing the 0- or 30-degree lenses, the increased visibility was useful in performing the functions. Movements were more purposeful and therefore more efficient.
Discussion
The subtemporal approach has been used for ~100 years and hence, it has been well documented in the literature, together with its possible complications. Some of these include damage to the temporal lobe including edema, hemorrhage, and venous infarction.4,5,11
From our investigation, it seems relatively evident that the endoscope adds to the structures visibility. There is also subjective increased operability afforded by the addition of the endoscope.
As in previous cadaveric studies, the actual distance in mm exposed by each approach is useful. In contrast to older studies in the literature which used a ruler to quantify this, our measurements were taken using the Stryker navigation system described earlier. The authors feel that this allows for more precise measurements and therefore a more accurate picture of the exposure afforded.
The authors chose to express the linear exposure in this way also to limit bias. That is, the limitations encountered by taking measurements with a ruler may naturally accommodate bias. This is because the ruler when inserted will either alter the anatomy or take measurements at an angle–in either case bias is likely introduced. The possibility of observer bias is also increased with the use of these measuring devices. This is minimized by the use of navigation.
The usefulness of the endoscope as an adjunct to the microscope has been discussed in the literature.8,9 The small size endoscope (2.7 mm) allows deep visualization in areas otherwise limited by anatomy. It also reduces the amount of retraction needed of normal tissue when trying to access deep structures.3,6,7,8
When considering operability and comparing it to visibility, the importance of the former cannot be minimized. In clinical medicine, the patient expects the surgeon to influence the pathology witnessed and as such visibility alone offers little advantage in terms of potential patients' outcome. Manipulation of pathology is the purpose of surgery. Being such, visibility without increased operability is akin to a peephole in a door; that is, its usefulness is limited.
One important increase in operability we have noted is the ease with which maneuvers can be performed. This cannot be understated, yet is difficult to quantify. This ease can translate into shorter, safer, and more efficient procedures.
The second important factor that affects operability is the reduction in brain retraction. Because of the increase in visibility and the small size of the endoscope, less retraction of the temporal lobe is needed to accomplish the same feats. Considering the inherent dangers of the subtemporal approach, this is a big advantage afforded by the addition of the endoscope.
Another factor of note is the type of maneuver the surgeon is attempting. The maneuvers attempted with this study tended to demand a great deal of space for their execution. This is not true for all procedures. For example, if a soft tumor was noted in the area, the extra visibility afforded by the endoscope would offer a great advantage when using suction for this tumor. The added illumination and visibility would offer just enough advantage to increase resection of a deep tumor, for example. In itself, illumination is a great advantage that is noteworthy.
Conclusion
Our study demonstrates that the endoscope, as an adjuvant tool to the microscope, does not objectively increase surgical maneuverability in our subtemporal approach model. However, the increased visibility afforded by the endoscope helps in performing microscopic maneuvers because it creates an image in the surgeon's mind of where critical structures, albeit not visible with the microscope, are located in the microsurgical environment.
References
- 1.Hernesniemi J Ishii K Karatas A et al. Surgical technique to retract the tentorial edge during subtemporal approach: technical note Neurosurgery 2005734E408, discussion E408 [DOI] [PubMed] [Google Scholar]
- 2.Spiller W G, Frazier C H. The division of the sensory root of the trigeminus for relief of tic douloureaux: an experimental pathological and clinical study with a preliminary report of one surgical successful case. Phila Med J. 1901;73:1039–1049. [Google Scholar]
- 3.Wen D Y, Heros R C. Surgical approaches to the brain stem. Neurosurg Clin N Am. 1993;73(4):457–468. [PubMed] [Google Scholar]
- 4.Rhoton A L. Tentorial incisura. Neurosurgery. 2000;73:131–153. doi: 10.1097/00006123-200009001-00015. [DOI] [PubMed] [Google Scholar]
- 5.Knosp E, Tschabitscher M, Matula C, Koos W T. Modifications of temporal approaches: anatomical aspects of a microsurgical approach. Acta Neurochir (Wien) 1991;73:159–165. doi: 10.1007/978-3-7091-9183-5_26. [DOI] [PubMed] [Google Scholar]
- 6.Ardeshiri A Ardeshiri A Wenger E Holtmannspötter M Winkler P A Subtemporal approach to the tentorial incisura: normative morphometric data based on magnetic resonance imaging scans Neurosurgery 2006734ONS22–ONS28., discussion ONS22–ONS28 [DOI] [PubMed] [Google Scholar]
- 7.Hernesniemi J, Ishii K, Niemelä M, Kivipelto L, Fujiki M, Shen H. Subtemporal approach to basilar bifurcation aneurysms: advanced technique and clinical experience. Acta Neurochir Suppl (Wien) 2005;73(4):31–38. doi: 10.1007/3-211-27911-3_6. [DOI] [PubMed] [Google Scholar]
- 8.Pichierri A D'Avella E Ruggeri A Tschabitscher M Delfini R Endoscopic assistance in the epidural subtemporal approach and Kawase approach: anatomic study Neurosurgery 2010734ons29–ons37., discussion ons37 [DOI] [PubMed] [Google Scholar]
- 9.Salma A Wang S Ammirati M Extradural endoscope-assisted subtemporal posterior clinoidectomy: a cadaver investigation study Neurosurgery 2010734ons43–ons48., discussion ons48 [DOI] [PubMed] [Google Scholar]
- 10.Ammirati M, Ma J, Becker D, Black K, Cheatham M, Bloch J. Transzygomatic approach to the tentorial incisura: surgical anatomy. Skull Base Surg. 1992;73(4):161–166. doi: 10.1055/s-2008-1057128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonzalez L F, Amin-Hanjani S, Bambakidis N C, Spetzler R F. Skull base approaches to the basilar artery. Neurosurg Focus. 2005;73(4):E3. doi: 10.3171/foc.2005.19.2.4. [DOI] [PubMed] [Google Scholar]


