Abstract
Objective: we estimated the cost-effectiveness of a community falls prevention service compared with usual care from a National Health Service and personal social services perspective over the 12 month trial period.
Design: a cost-effectiveness and cost utility analysis alongside a randomised controlled trial
Setting: community.
Participants: people over 60 years of age living at home or in residential care who had fallen and called an emergency ambulance but were not taken to hospital.
Interventions: referral to community fall prevention services or usual health and social care.
Measurements: incremental cost per fall prevented and incremental cost per Quality-Adjusted Life Years (QALYs)
Results: a total of 157 participants (82 interventions and 75 controls) were used to perform the economic evaluation. The mean difference in NHS and personal social service costs between the groups was £-1,551 per patient over 1 year (95% CI: £-5,932 to £2,829) comparing the intervention and control groups. The intervention patients experienced on average 5.34 fewer falls over 12 months (95% CI: −7.06 to −3.62). The mean difference in QALYs was 0.070 (95% CI: −0.010 to 0.150) in favour of the intervention group.
Conclusion: the community falls prevention service was estimated to be cost-effective in this high-risk group. Current Controlled Trials ISRCTN67535605. (controlled-trials.com)
Keywords: economic evaluation, falls prevention, older people
Introduction
Falls are common among older people, can result in significant injury [1], and are associated with substantial health and social care resource use. A UK study estimated that in 1999 there were 647,721 A&E visits and 204,424 admissions resulting from injuries in people aged 60 years or above who had fallen. These falls were estimated to cost the UK government £981 million, of which around £581 million were NHS costs (2000 price year) [2]. People who have fallen in the UK often call the ambulance service that assesses the severity of the injury and need for medical care. Many such people are neither transferred to an emergency department, where they may get access to fall prevention services, nor are they routinely referred to falls services in the community. We have shown that routine referral of such people to a community falls prevention service has many health benefits including a reduction in falls, reduced fear of falling and increased activity [3].
A Cochrane review showed that the evidence that fall prevention strategies are cost saving is limited [4]. A different systematic review also showed that there is considerable uncertainty around the cost-effectiveness of multifactorial assessment and targeted intervention for preventing falls and injuries in community and emergency care settings among older people [5]. This study seeks to add to the evidence surrounding the cost-effectiveness of these types of interventions by reporting an economic evaluation of a community fall prevention rehabilitation service for older people who had called an ambulance because of a fall and who had not been taken to hospital.
Method
Details of the methods used in the randomised controlled trial have previously been published [3]. In brief, people were eligible for inclusion in the trial if they were aged >60 years and living at home or in care homes in four Nottinghamshire primary care trusts in the UK and had contacted the East Midlands Ambulance Service through the emergency telephone system because of a fall, but who had not been transported to hospital. People were excluded if they were unable to give consent, deemed too ill to participate (e.g. terminally ill) or were already in a falls prevention rehabilitation programme.
Participants allocated to the intervention group were referred to the community falls prevention service provided by four community fall prevention teams which included occupational therapists, physiotherapists and nurses. An individualised multi-factorial intervention programme was undertaken following the UK clinical falls guidelines [National Institute of Health and Clinical Excellence (NICE) 2004] [6]. The intervention was delivered primarily in the participants’ homes, but it also included group sessions held in community centres. Participants allocated to the control group continued to use existing social and medical services as usual. Further details of the interventions can be found on page 2 of the clinical paper [3].
Objective
To estimate the cost-effectiveness (defined as incremental cost per fall prevented) and cost utility [defined as incremental cost per Quality-Adjusted Life Years (QALYs) gained] of the community falls prevention service compared to usual care for the 12-month trial period from an NHS and social services perspective (as favoured by NICE [7]) in the base case.
Resource use and costing
Contacts with health and social services, including care home admissions, use of informal care, equipment provided and home modifications (For detailed list of resource items recorded, please see Table S1 in Supplementary data available in Age and Ageing online) were collected at an individual patient level primarily from questionnaires administered at baseline by a researcher face-to-face with the participants in their own home and at 6 and 12 months via a postal questionnaire. Different types of resource use data were collected for different time periods in the 6- and 12-month questionnaires to aid recall, reflecting the likely usage of the service, but all were adjusted to reflect a 12-month period. For instance, participants were asked to report at 6 and 12 months the number of GP visits in the past 3 months, at each time point these numbers were multiplied by 2 and summed to estimate the number of visits by the participant to the GP over 12 months.
Participants were asked whether they had paid for any meals-at-home or for equipment and modifications made to their home in order that we could estimate the proportion paid for by social services. For equipment and modifications, we attached an average unit cost based on number of items of equipment used taken from a previous study [8]. We also measured the time costs of informal carers (regardless of whether they had to give up work or not) using the human capital approach, applying average net hourly or weekly earnings as appropriate (please see Supplementary data available in Age and Ageing online, Table S1). Patient and carer costs were excluded from the base case analysis because of controversy surrounding the methods used to value time [9], but were included separately in an additional analysis in line with the approach taken by NICE [7] and as recommended specifically in the area of economic evaluations of fall-prevention strategies [10].
In addition, some secondary care data (number of admissions, the length of stay and fall-related fractures) for the 12-month period was retrieved by a researcher blind to allocation from the Nottingham University Hospital computer system along with data on the number of emergency ambulance calls received for falls over 12 months and the proportion of these resulting in visits to emergency departments rather than the patient being left at home which were extracted from the East Midlands Ambulance Service computer system.
Baseline resource use was compared to check whether the intervention and usual care groups were comparable in terms of their prior health and social services usage. We estimated the overall change in costs per patient to the health service and personal social services (and separately incorporating the patient and carer costs) by summing the costs associated with delivering the intervention and the wider resource items. All unit costs and their sources are shown in Supplementary data available in Age and Ageing online, Table S1. All costs in this paper are presented in 2008–09 pounds sterling, discounting was not undertaken reflecting the timeframe for the analysis, and no price adjustments for inflation or currency conversion were necessary.
Outcomes
The number of falls was collected via a participant diary sent out by post each month. Participants were telephoned when diaries were not returned promptly.
To undertake a cost-utility analysis, we measured patient health-related quality of life using the EQ-5D (www.euroqol.org), which has five dimensions (mobility, self-care, usual activities, pain or discomfort, and anxiety or depression), each rated at one of three levels (none, some, severe problems) [11]. When combined, these levels create 243 possible health states, each of which has an empirically measured utility score from the York A1 tariff where scores range between −0.594 and 1.00 [12]. The EQ-5D was administered at baseline, 6 and 12 months, and used to construct patient-specific utility paths. The number of QALYs for the 12-month trial period was estimated for each patient using linear interpolation and area under the curve analysis taking account of baseline values. The mean difference in QALYs between the community falls prevention service and usual care was calculated.
Cost-effectiveness analysis
Cost-effectiveness was estimated from an NHS and personal social services perspective in the base case for a 12-month period. We present the incremental costs and benefits with 95% CIs computed using the bootstrap technique [13]. Neither costs nor benefits were discounted reflecting the 12-month analysis time frame. Current guidance produced by the NICE (2008) suggests an intervention is likely to be considered cost-effective if the incremental cost effectiveness ratio is within or lower than a cost-effectiveness threshold (λ) of £20,000–£30,000 per QALY [7]. In the case of incremental cost per fall prevented, there is no clear guideline as to what represents good value so we sought to compare it to previous cost-effectiveness studies reporting this outcome.
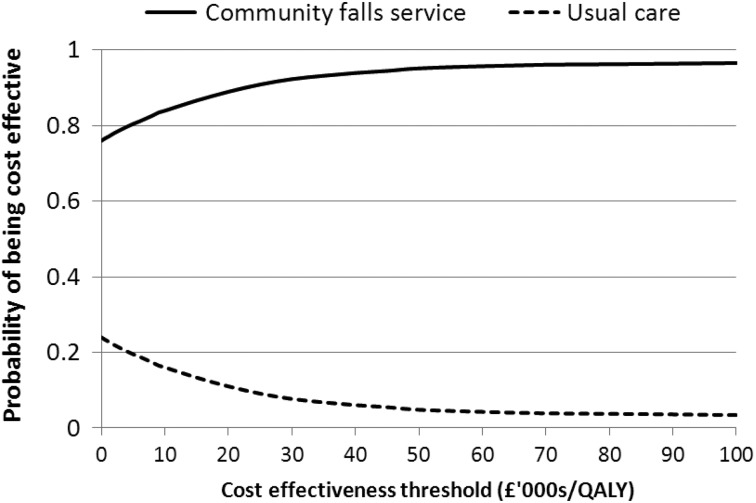
Decision uncertainty
To estimate the level of uncertainty associated with the decision as to whether the community falls prevention service or usual care was most cost-effective, we estimated the cost-effectiveness acceptability curves, which plot the probability of an intervention being cost-effective compared to an alternative for different levels of willingness to pay per QALY, and plotted these graphically [14, 15]. Unit costs were attached to resource use in Microsoft Excel and all statistical analysis was undertaken in STATA IC version 11.
For details of the sensitivity analysis undertaken, please see Supplementary data available in Age and Ageing online, Appendix 3.
Results
In total, 204 patients were randomised equally between the intervention and control groups. In total, 35 patients died (16 intervention vs. 19 control), and 12 withdrew (4 intervention vs. 8 control) before 12-month data could be elicited. Therefore, data from 157 participants (82 intervention and 75 control) were included in the base case economic analysis using only complete cases (one participant did not complete the 6-month follow-up resource use questionnaire, so for this patient, we based the annual costs only on answers to their 12-month questionnaire).
Resource use and costs
Baseline resource use was similar for intervention versus control participants (data not shown but available from corresponding author).
Tables 1 and 2 show the resource use and associated costs in the two groups over 12 months. There were significantly fewer GP and practice nurse visits, subsequent ambulance journeys to the emergency department and meals-at-home paid for by the patient in the intervention group compared with the control group. The mean total NHS and personal social service cost per participant during the 12-month follow-up period (excluding patient and carer costs) was £15,266 (SD £13,504) in the intervention group compared to £16,818 (SD £14,210) in the control group giving a mean difference of £-1,551 (95% CI: £-5,932 to £2,829).
Table 1.
Mean (standard deviation) resource use and mean difference in resource use per patient (95% CI)
| Resource use item | Community falls prevention service (n = 82) | Usual care (n = 75) | Mean difference (95% CI) |
|---|---|---|---|
| Intervention | |||
| Rehabilitation programme (number of hours) | 12.02 (12.51) | NA | 12.02 (9.25 to 14.78) |
| Primary health care | |||
| GP (number of visits) | 8.00 (10.54) | 11.95 (12.22) | −3.95 (−7.56 to −0.33) |
| Practice nurse (number of visits) | 3.22 (6.74) | 7.09 (11.94) | −3.87 (−6.98 to −0.77) |
| District nurse (number of visits) | 12.10 (45.56) | 12.45 (30.74) | −0.36 (−12.53 to 11.82) |
| NHS walk in centre (number of visits) | 0.10 (0.43) | 0.29 (1.26) | −0.20 (−0.50 to 0.11) |
| Secondary health care | |||
| Ambulance call out (leaving the person at home) (number) | 1.83 (5.20) | 2.57 (4.19) | −0.74 (−2.23 to 0.74) |
| Ambulance call out (taking the person to ED) (number) | 0.55 (0.74) | 1.01 (1.44) | −0.46 (−0.83 to −0.10) |
| Fractures (number) | 0.10 (0.43) | 0.11 (0.45) | −0.01 (−0.15 to 0.013) |
| Inpatients (number of bed days) | 13.24 (19.53) | 11.41 (17.97) | 1.83 (−4.08 to 7.74) |
| A&E (number of visits) | 0.93 (1.81) | 1.65 (3.19) | −0.73 (−1.56 to 0.10) |
| Outpatients first and follow-up visit (number) | 2.45 (5.28) | 1.356 (4.26) | 1.09 (−0.42 to 2.60) |
| Day hospital visits (number) | 1.32 (6.02) | 0.53 (2.82) | 0.78 (−0.68 to 2.25) |
| NHS funded travel (number of trips) | 1.44 (1.64) | 1.39 (1.771) | 0.05 (−0.48 to 0.58) |
| Personal social services | |||
| LA home care worker (number of hours | 192.99 (297.33) | 184.00 (252.33) | 8.99 (−77.03 to 95.71) |
| Day centre (number of visits) | 21.88 (78.95) | 15.25 (41.68) | 6.62 (−13.09 to 26.33) |
| Residential care (number of days resident) | 14.43 (48.25) | 30.05 (75.81) | −15.62 (−35.91 to 4.67) |
| Nursing home care (number of days resident) | 16.09 (58.82) | 29.39 (79.99) | −13.30 (−35.63 to 9.04) |
| Meals at home (number of meals) | 42.64 (104.21) | 66.89 (146.08) | −24.25 (−65.64 to 16.14) |
| Special equipment (number of items) | 3.89 (4.41) | 2.64 (3.50) | 1.25 (−0.005 to 2.50) |
| Patient and carer | |||
| Meals at home (number of meals) | 40.11 (80.85) | 88.42 (153.96) | −48.30 (−87.73 to −8.88) |
| Travel (number of trips)a | 1.28 (3.76) | 0.71 (2.34) | 0.57 (−0.40 to 1.55) |
| Home care—live in (number of hours) | 81.13 (304.40) | 44.07 (148.761) | 37.06 (−37.69 to 111.80) |
| Home care—live out (number of hours) | 160.50 (485.06) | 152.37 (188.79) | 8.13 (−106.52 to 122.78) |
| Time—relative/friend gave up work partially (number of hours) | 45.98 (232.60) | 7.63 (46.58) | 38.35 (−13.80 to 90.50) |
| Time costs—relative/friend gave up work completely for all or part of the year (number of people) | 0.05 (0.22) | 0.00 (0.00) | 0.05 (−0.001 to 0.10) |
aThe number of trips was estimated by adding up the number of inpatient, outpatient and A&E visits minus the number of ambulance trips. This may overestimate costs if patients attended multiple outpatient visits at once.
Table 2.
Mean (standard deviation) cost and cost difference (95% CI) per patient over the 12 months for community falls prevention service compared to usual care (in 2008–09 pounds sterling)
| Resource use item | Community falls prevention service (n = 82): mean (SD) £'s | Usual care (n = 75): mean (SD) £'s | Mean difference (95% CI) £'s |
|---|---|---|---|
| Intervention | |||
| Rehabilitation programme | 262.44 (245.04) | NA | 262.44 (208.60 to 316.28) |
| Primary health care | |||
| GP | 288.00 (379.30) | 430.08 (440.03) | −142.08 (−172.22 to −11.94) |
| Practice nurse | 35.41 (74.12) | 78.03 (131.37) | −42.61 (−76.76 to −8.47) |
| District nurse | 314.54 (1,184.68) | 323.79 (799.32) | −9.25 (−325.73 to 307.23) |
| NHS walk in centre | 7.61 (33.81) | 22.88 (98.31) | −15.27 (−39.01 to 8.47) |
| Total primary health care | 645.56 (1,258.18) | 854.77 (1,070.21) | −209.21 (−576.55 to 158.12) |
| Secondary health care | |||
| Ambulance call out (leaving the person at home) | 477.89 (1,368.23) | 676.79 (1,102.47) | −198.90 (−589.23 to 191.44) |
| Ambulance call out (taking the person to A&E) | 205.24 (276.60) | 378.99 (537.75) | −173.74 (−310.91 to −36.58) |
| Cost of fractures | 37.95 (168.62) | 41.49 (15.99) | −3.54 (−58.00 to 50.91) |
| Cost of inpatients | 5,576.03 (8,299.44) | 4,859.00 (7,649.41) | 717.03 (−1,797.38 to 3,231.41) |
| A&E | 62.30 (168.28) | 88.85 (159.05) | −26.55 (−78.16 to 25.06) |
| Outpatients first and follow-up visit | 187.43 (332.34) | 117.84 (266.30) | 69.59 (−25.01 to 164.18) |
| Day hospital visits | 181.76 (831.08) | 73.60 (388.56) | 108.16 (−94.16 to 310.47) |
| NHS funded travel | 77.71 (88.63) | 74.88 (92.21) | 2.83 (−25.75 to 31.40) |
| Total secondary health care | 6,806.31 (8,474.43) | 6,311,44 (7,681.01) | 494.87 (−12,052.12 to 3,041.85) |
| Personal social services | |||
| LA home care worker | 3,474.04 (5,351.79) | 3,312.08 (4,541.34) | 161.96 (−1,398.88 to 1,722.79) |
| Day centre visits | 765.73 (2763.39) | 533.87 (1458.87) | 231.87 (−457.939 to 921.712) |
| Residential care | 1,030.27 (3,433.51) | 2,150.26 (5,412.20) | −1,119.99 (−2,566.89 to 326.90) |
| Nursing home care | 1,644.46 (6,016.53) | 3,005.41 (8,180.65) | −1,360.95 (−3,644.93 to 923.03) |
| Meals at home | 183.36 (448.12) | 287.63 (628.16) | −104.27 (−277.95 to 69.42) |
| Special equipment | 454.34 (395.76) | 362.32 (407.50) | 92.02 (−34.85 to 218.89) |
| Total personal social services | 7,552.21 (9,536.96) | 9,651.58 (11,044.15) | −2,099.37 (−5,367.95 to 1,169.20) |
| Patient and carer | |||
| Meals at home | 175.63 (352.57) | 452.40 (935.26) | −276.77 (−504.74 to −48.81) |
| Travel costs | 28.52 (112.06) | 10.55 (42.42) | 17.98 (−8.41 to 44.37) |
| Home care—live in | 735.10 (2,758.20) | 399.34 (1,347.93) | 335.76 (−341.49 to 1,013.03) |
| Home care—live out | 1,454 (4,395.6) | 1,380.64 (1,710.67) | 73.67 (−965.15 to 1,112.5) |
| Time costs—relative/friend gave up work partially | 416.59 (2,107.57) | 69.11 (422.09) | 347.48 (−125.07 to 820.03) |
| Time costs—relative/friend gave up work completely | 956.23 (495.82) | 0 (0) | 956.23 (−30.30 to 1,942.77) |
| Total patient and carer | 3,766.39 (10,031.45) | 2,312.04 (2,462.31) | 1,454.35 (−817.26 to 3,725.96) |
| Total NHS and PSS costs | 15,266.52 (13,504.44) | 16,817.79 (14,210.42) | −1,551.28 (−5,932.02 to 2,829.47) |
| Total costs | 19,032.9 (17, 055.79) | 19,129.83 (14,930.35) | −96.92 (−5,140.92 to 4,947.07) |
Cost-effectiveness
The mean number of falls per patient during the 12-month follow-up period in the 157 participants included in the base case economic analysis was 2.61 (SD 4.13) for community falls prevention service participants and 7.95 (SD: 6.61) for the control group (difference −5.34; 95% CI: −7.06 to −3.62, P < 0.001). These are similar to the figures presented in the effectiveness paper that included all participants, not only those with resource use data [8]. The cost-effectiveness analysis estimates that the intervention was the dominant strategy as it had lower costs and falls compared to the control group, therefore an incremental cost-effectiveness ratio is not required and the intervention is cost-effective.
Cost utility results without carer time costs included
The mean utility per patient at baseline, 6 and 12 months was 0.438, 0.366 and 0.344 for the intervention group and 0.481, 0.334 and 0.263 for the control group, respectively. The mean QALYs per patient for the community falls prevention service group was −0.059 (SD: 0.269), while the mean QALYs for the control group was −0.129 (SD: 0.238), giving a mean difference of 0.070 (95% CI: −0.010 to 0.150; p = 0.086). Since the mean cost per patient was lower for the intervention group and the intervention group saw a lower fall in QALYs over the trial period, we conclude that the intervention is dominant and therefore cost-effective such that there is no need to estimate an incremental cost-effectiveness ratio for the community falls prevention service in the base case and no need for value judgements about its cost-effectiveness. Figure 1 shows the cost-effectiveness acceptability curves for the 12-month trial period. At a willingness to pay of £20,000 (£30,000) per QALY there is a 89.0% (92.3%) chance of the community falls prevention service group being cost-effective in this population.
Figure 1.
Decision uncertainty: Cost Effectiveness Acceptability Curves for intervention and usual care when patient and carer costs are included.
For details of the results of the sensitivity analysis undertaken, please see Supplementary data available in Age and Ageing online, Appendix 4.
Discussion
We have estimated that the community falls preventions service, as delivered in this trial, was both cost saving and improved outcomes (both in terms of number of falls and QALYs), suggesting it is highly cost-effective in this group of people. Exploring the decision uncertainty surrounding this result showed that the probability that the intervention was cost-effective was high >89% from an NHS and personal social services perspective and slightly less certain (>71%) when patient and carer costs were incorporated. The results are robust to changes in (i) large increases in the cost of the intervention; (ii) taking a wider perspective; or (iii) where one considers only the cost of the intervention i.e. excluding the wider costs associated with the intervention (although in the latter scenario the intervention group on average cost more but was cost-effective when considering the change in QALYs).
Comparison with other studies
Previous studies of strategies to reduce falls in older people in the community have shown a range of costs per fall prevented, but none has found an intervention that is both cost saving and reduces falls [4]. This may be explained by the differences in the target populations since previous studies have suggested that cost-effectiveness can be improved by better targeting of interventions. For instance, Irvine et al. identified older people via GP practices and had to contact more than five thousand people in order to identify those at high risk of falling and ended up with 364 suitable patients [16]. They calculated an incremental cost-effectiveness ratio of £3,320 per fall averted, with a fall rate of 2.85 among controls over a 12-month follow-up. Salkeld et al. found that a home hazard reduction programme to reduce falls was cost saving for only those that had fallen in the 12 months prior to randomisation [17]. Therefore, cost-effectiveness seems to depend on the background fall rate of the population targeted by a fall prevention intervention. In the current study, we identified high-risk older people at the point at which they had fallen and called the emergency services, the targeting of this intervention to a group who had all fallen and who had a particularly high fall rate during follow-up (mean of 7.95 among controls) may explain why we find it to be so cost-effective relative to previous studies in the area.
Strengths and weaknesses
The major strength of this study is that it was conducted alongside a randomised controlled trial. The inclusion of a cost utility analysis, measuring outcomes in terms of QALYs, in this study will aid value for money comparisons across diverse health interventions and should help raise the priority attached to care of this vulnerable group of people. However, potential limitations include the possibility of respondent bias since respondents knew if they were in the intervention arm or not and this may have influenced how they recorded resource use, although notably most secondary care data and ambulance resource use data came from computerised records rather than patients directly. The study time frame was 12 months, thus we did not estimate the long-term costs and benefits of the intervention compared to usual care. Finally, the 95% CIs around the mean differences in costs and QALYs span zero, suggesting that it is possible that the intervention is associated with additional costs or less QALYs. This reflects the fact that clinical studies are rarely powered to find statistically significant differences in economic costs or outcomes, this is one reason why economists generally focus on estimation (of incremental cost effectiveness) and the uncertainty surrounding this estimate (as illustrated in this paper using cost-effectiveness acceptability curves) rather than on hypothesis testing [18].
Implications and future research
The provision of a community falls prevention service targeted at those calling ambulance services following a fall is likely to represent a cost-effective use of NHS and personal social services resources. However, future research should be conducted to test the generalisability of the findings from this study to investigate whether similar levels of cost-effectiveness can be found across multiple study sites.
Conclusion
The community falls prevention service delivered in this trial was cost-effective with little decision uncertainty. This study further justifies the development of clinical pathways linking the emergency ambulance services to community therapy services.
Key points.
Many people fall and call an ambulance and are not transported to hospital. This group is at high risk of falls.
A community-based falls prevention service reduces the falls rate, fear of falling and increases activity in these people.
Few economic evaluations of strategies to prevent falls in older people have been conducted, particularly in the UK.
The community-based falls prevention service was estimated to be a cost-effective intervention for this patient group.
Authors’ contributions
T.H.S.: contributed to the writing and design of the protocol, analysed and wrote the economic paper. Guarantor: P.A.L.: PI for the study, designed the protocol, secured funding, recruited participants, collected data, contributed to writing the paper. Had scholarly thoughts about the interpretation of results. Guarantor: C.A.C.C.: contributed to writing the paper and the interpretation of results. J.R.F.G.: contributed to the writing and design of the protocol and grant application, contributed to analysis and writing paper and scholarly thoughts about the results. O.S.: contributed to the writing and design of the protocol and grant application, contributed to writing the paper and scholarly thoughts about application of the results. V.S.-H.: contributed to the writing and design of the protocol and grant application, collected data, contributed to the scholarly discussions about the paper writing. K.R.: contributed to the writing and design of the protocol and grant application, collected data, checked data, contributed to the scholarly discussions about the paper writing. V.T.: contributed to the writing and design of the protocol and grant application, collected data, checked data and inputted data, contributed to the scholarly discussions about the paper writing. M.W.: contributed to the research process and writing the paper with clinical observations. A.A.: contributed to the writing and design of the protocol and grant application, contributed to writing the paper and scholarly thoughts about application of the results. C.L. Fellows: initially contacted participants through the ambulance service. C. Simms-Jones: contributed to data collection from the ambulance service.
Conflicts of interest
None declared.
Data
All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Ethics committee approval
Ethical approval was granted from the North Nottinghamshire, UK Local Research Ethic Committee and NHS R&D approval from Nottinghamshire Primary Care Trusts, UK. 05/Q2402/53.
Funding
This study was funded by a post doctoral training scholarship awarded to Dr Philippa Logan from the UK NHS National Institute of Health Research. The funding source provided an external peer review of the study protocol but did not have any role in the data collection, analysis, report writing or in the decision to publish this paper.
Supplementary data
Supplementary data mentioned in the text is available to subscribers in Age and Ageing online.
References
- 1.Tinetti M, Speechley M, Ginter S. Risk factors for falls among elderly persons living within the community. N Engl J Med. 1988;319:1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 2.Scuffman P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health. 2003;57:740–4. doi: 10.1136/jech.57.9.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Logan PA, Coupland CAC, Gladman JRF, et al. Community falls prevention for people who call an emergency ambulance after a fall: randomised controlled trial. BMJ. 2010;340:c2102. doi: 10.1136/bmj.c2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009;2:CD007146. doi: 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Gates S, Fisher JD, Cooke MW, Carter YH, Lamb SE. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: systematic review and meta-analysis. BMJ. 2008;336:130–3. doi: 10.1136/bmj.39412.525243.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NICE. Falls: the assessment and prevention of falls in older people. 2004. www.nice.org.uk/cg21 .
- 7.National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. URL www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdateJune2008.pdf . [PubMed]
- 8.Logan PA, Murphy A, Drummond AE, et al. The cost of assistive devices for people who have fallen. Br J Occupat Therapy. 2007;70:475. [Google Scholar]
- 9.Sach TH, Whynes DK. Measuring indirect costs: is there a problem? Appl Health Econ Health Policy. 2003;2:135–9. [PubMed] [Google Scholar]
- 10.Davis JC, Robertson MC, Comans T, Scuffham PA. Guidelines for conducting and reporting economic evaluation of fall prevention strategies. Osteoporos Int. 2011;22:2449–59. doi: 10.1007/s00198-010-1482-0. [DOI] [PubMed] [Google Scholar]
- 11.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 12.Dolan P. Modelling valuations for EuroQol health states. Med Care. 1997;35:1095–108. doi: 10.1097/00005650-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ. 1997;6:327–40. doi: 10.1002/(sici)1099-1050(199707)6:4<327::aid-hec282>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 14.Fenwick E, Claxton K, Sculpher MJ. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ. 2001;10:779–87. doi: 10.1002/hec.635. [DOI] [PubMed] [Google Scholar]
- 15.Barton GR, Briggs AH, Fenwick EA. Optimal cost-effective decisions: the role of the cost-effectiveness acceptability curve (CEAC), cost effectiveness acceptability frontier (CEAF) and expected value of perfect information (EVPI) Value Health. 2008;11:886–97. doi: 10.1111/j.1524-4733.2008.00358.x. [DOI] [PubMed] [Google Scholar]
- 16.Irvine L, Conroy SP, Sach T, et al. Cost-effectiveness of a day hospital falls prevention programme for screened community-dwelling older people at high risk of falls. Age Ageing. 2010;39:710–6. doi: 10.1093/ageing/afq108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salkeld G, Cumming RG, O'Neill E, et al. The cost effectiveness of a home hazard reduction program to reduce falls among older persons. Aust N Z J Public Health. 2000;24:265–71. doi: 10.1111/j.1467-842x.2000.tb01566.x. [DOI] [PubMed] [Google Scholar]
- 18.Briggs AH, O'Brien BJ. The death of cost-minization studies? Health Econ. 2001;10:179–84. doi: 10.1002/hec.584. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.