Abstract
Endovascular embolization is being increasingly used to treat intracranial arteriovenous malformations (AVMs). However, we experienced two patients with retained microcatheters after AVM embolization using Onyx.
Keywords: Arteriovenous malformation, Onyx, Retained microcatheter
INTRODUCTION
Intracranial arteriovenous malformations (AVMs) are uncommonly encountered with a prevalence of 0.06 to 0.11% in the general population5,14). AVMs are treated by surgery, radiosurgery, endovascular embolization and their combination2,3,8). However, recent technical and material advances raised the status of the endovascular embolization of intracranial AVMs, particularly as an adjunct to surgery or radiosurgery.
Ethylene-vinyl alcohol copolymer (Onyx, ev3, CA, USA) is a new polymerizable liquid embolic material, which supplied in dimethyl-sulfoxide (DMSO). Unlike previous embolic material, theoretically it allows longer injection times and better control of injections because of its longer polymerization time, and thus, in addition to the lack of adherence mentioned above it also offers the advantage of better penetration4,11,15). Nevertheless, these advantages do not prevent a catheter being used for embolization being glued into an AVM, and a remnant catheter in an intracranial artery presents a risk of thromboembolic complications. Here, we report two patients in which a catheter was inadvertently glued into an intracranial AVM during Onyx embolization.
CASE REPORT
Case 1
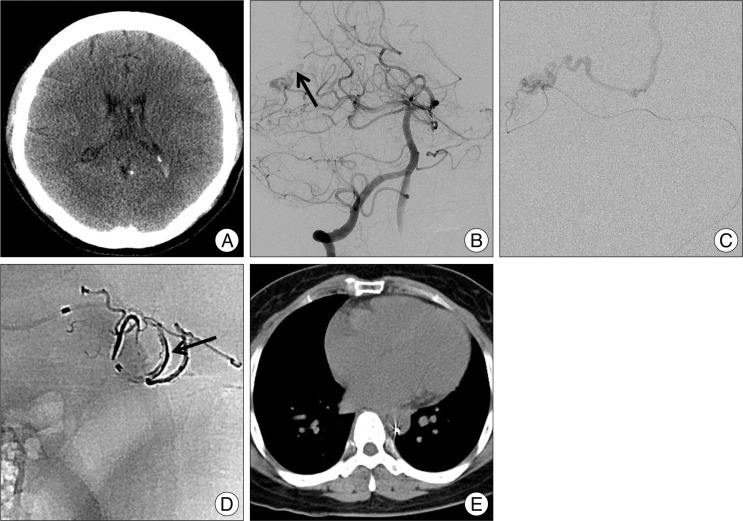
A 53-year-old woman presented with a headache. Brain computed tomography (CT) and magnetic resonance imaging revealed an intraventricular hemorrhage, a right temporal lobe AVM (Fig. 1A). Cerebral digital subtraction angiography (DSA) revealed a 10×6 mm sized AVM (Spetzler-Martin Grade II)13) filling from the superior cerebellar artery and draining through an internal cerebral vein without any feeding arterial aneurysm or venous stasis (Fig. 1B). The nidus was occluded with Onyx embolic material under local anesthesia at a biplane angiography unit. Vascular access was obtained using a 6F guiding catheter (Envoy, Cordis, FL, USA), and distal vascular access using a Silverspeed (ev3, Irvine, CA, USA) microwire. After the microcatheter tip was placed at the perinidal position, superselective angiography was performed to analyze the anatomy of the nidus (Fig. 1C). Embolization was conducted by flushing a microcatheter with normal saline and then filling it with DMSO. Onyx (0.25 mL) was then injected slowly (<0.1 mL/min) into the microcatheter, and injection from the catheter tip into the AVM was monitored fluoroscopically by road-mapping. When Onyx reflux of 1 cm was observed around the catheter tip, the injection of Onyx was temporarily discontinued for 1 minute to form a cast around the tip of the microcatheter, and subsequently, a second penetration into the nidus was made. The total amount of Onyx used in case 1 was 0.8 cc, the injection time was 25 minutes, and the distance between the catheter tip and Onyx reflux was about 13 mm (Fig. 1D). When we attempted to remove the microcatheter, its tip was found to be stuck to onyx mass, and could not be removed. Unsuccessful attempts were then made to withdraw the microcatheter over a period of 20 minutes. However, eventually the catheter was transected at the groin puncture site, and the remnant was left in the femoral artery. Anticoagulant therapy was administered for 2 days and the patient was maintained on antiplatelet agents. The patient also underwent gamma knife radiosurgery for a remnant AVM at 24 days after the procedure. At two years after the embolization treatment, contrast enhanced abdominopelvic CT depicted the retained microcatheter against the peripheral wall of the descending and abdominal aorta (Fig. 1E).
Fig. 1.
A : Non contrast enhanced brain computed tomography shows small amount of intraventricular hemorrhage in both lateral ventricle. B : Right vertebral artery angiography reveals small arteriovenous malformation (AVM) fed by right superior cerebellar artery braches and draining through internal cerebral vein (arrow). C : Superselective angiography demonstrates angioarchitecture of the AVM. D : Postprocedural radiography shows Onyx material. Black arrow indicates the cast of Onyx. E : Abdomino-pelvic computed tomography 2 years after embolization shows peripheral wall reposition of the retained microcatheter in descending aorta.
Case 2
Two years before this presentation, the patient, a 31-year-old male, experienced a seizure and was transferred to our hospital from a local clinic. Radiographic findings at that time revealed a 23 mm sized right temporal AVM fed by multiple branches of anterior temporal and posterior cerebral arteries, and he was treated by gamma knife radiosurgery. At this presentation, follow up DSA revealed no reduction in the size of the nidus.
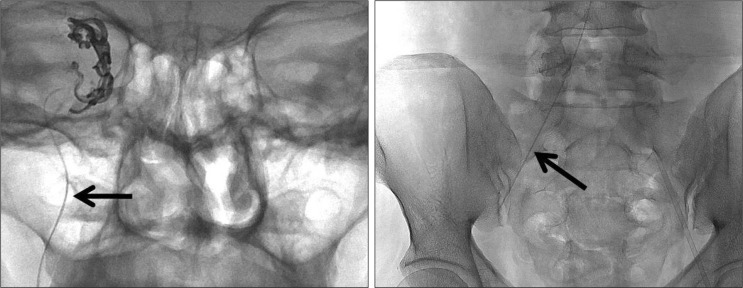
Accordingly, the AVM nidus and feeding arteries were occluded partially with Onyx under local anesthesia. Vascular access, microcatheter superselection, and embolization with Onyx were done as described above, but again, the catheter was adhered to Onyx mass and could not be removed. The catheter was transected at the groin puncture site and prescribed medications to prevent thromboembolic complications (Fig. 2). The patient underwent second gamma knife radiosurgery of the remnant nidus at 6 days after embolization.
Fig. 2.
Anterior-posterior view of plain X-ray of the skull and pelvis. Black arrows indicate a retained microcatheter in arteries.
DISCUSSION
The new liquid polymer Onyx allows longer embolization injection times, and therefore, provides better nidus penetration than n-BCA10). The complete obliteration rate of intracranial AVMs with Onyx is greater than the 10% rate of n-BCA9,10,16,17).
However, despite its non-adhesive nature, some reports have been issued about catheters glued into the cerebral circulation by Onyx4,9,17). On the other hand, little information is available about retained catheter rates in the arterial system or on subsequent complications. Weber et al.17) reported a retained catheter rate of 4% that for AVMs, but all complications encountered were without clinical consequences. The long-term courses of patients with a retained catheter have not been well documented. Although, it is evident that a retained catheter could cause local arterial injury, and that its mobile end could cause complications, such as, peripheral artery aneurysm formation or thromboembolism. Zoarski et al.18) reported a case of a chronically retained microcatheter in the carotid artery that was surgically removed, and in this case, the retained microcatheter caused thrombotic occlusion of the superficial femoral artery. Bingöl et al.1) also reported the successful surgical management of a femoral pseudoaneurysm caused by a retained catheter inadvertently glued into a cerebral AVM during embolization. In our two described cases, surgical management was not necessary because no vascular complications, such as, an aneurysm or thrombosis, arose. In the first case, serial follow up abdominopelvic CT demonstrated that the retained microcatheter had adopted a peripheral wall location in descending and abdominal aorta.
Ease of catheter removal depends on catheterized vessel tortuosity, vasospasm, the duration of precipitation, the distance of the reflux, and operator's experience. Some reports have described retrieval of a trapped microcatheter after Onyx embolization of an AVM. Santillan et al.12) used a balloon microcatheter (Hyperform™, eV3, CA, USA) to provide distal counter tension for trapped microcatheter retrieval, and Kelly et al.6) used a monorail snare technique to remove a microcatheter trapped in an occipital artery in an onyx treated case. However, great care must be taken when deciding whether to use these salvage techniques, especially for intracranial AVMs. The recent introduction of a microcatheter with a detachable tip (SONIC, Balt, France or Apollo, ev3, CA, USA) might overcome the complications associated with microcatheter retention and the risk of vessel wall rupture during microcatheter retrieval7).
CONCLUSION
The long-term courses of patients with a retained microcatheter have not been well characterized, but in our two cases, no vascular complications occurred during 3 years of follow up. We emphasize that great care must be taken when deciding whether to remove a retained intracranial microcatheter surgically.
Acknowledgements
This work was supported by clinical research grant from Pusan National University Hospital 2012.
References
- 1.Bingöl H, Sirin G, Akay HT, Ilyem H, Demirkilic U, Tatar H. Management of a retained catheter in an arteriovenous malformation. Case report. J Neurosurg. 2007;106:481–483. doi: 10.3171/jns.2007.106.3.481. [DOI] [PubMed] [Google Scholar]
- 2.Frizzel RT, Fisher WS., 3rd Cure, morbidity, and mortality associated with embolization of brain arteriovenous malformations : a review of 1246 patients in 32 series over a 35-year period. Neurosurgery. 1995;37:1031–1039. doi: 10.1227/00006123-199512000-00001. discussion 1039-1040. [DOI] [PubMed] [Google Scholar]
- 3.Jafar JJ, Davis AJ, Berenstein A, Choi IS, Kupersmith MJ. The effect of embolization with N-butyl cyanoacrylate prior to surgical resection of cerebral arteriovenous malformations. J Neurosurg. 1993;78:60–69. doi: 10.3171/jns.1993.78.1.0060. [DOI] [PubMed] [Google Scholar]
- 4.Jahan R, Murayama Y, Gobin YP, Duckwiler GR, Vinters HV, Viñuela F. Embolization of arteriovenous malformations with Onyx : clinicopathological experience in 23 patients. Neurosurgery. 2001;48:984–995. doi: 10.1097/00006123-200105000-00003. discussion 995-997. [DOI] [PubMed] [Google Scholar]
- 5.Jellinger K. Vascular malformations of the central nervous system : a morphological overview. Neurosurg Rev. 1986;9:177–216. doi: 10.1007/BF01743136. [DOI] [PubMed] [Google Scholar]
- 6.Kelly ME, Turner R, 4th, Gonugunta V, Rasmussen PA, Woo HH, Fiorella D. Monorail snare technique for the retrieval of an adherent microcatheter from an onyx cast : technical case report. Neurosurgery. 2008;63:ONSE89. doi: 10.1227/01.neu.0000335018.68369.e8. discussion ONSE89. [DOI] [PubMed] [Google Scholar]
- 7.Maimon S, Strauss I, Frolov V, Margalit N, Ram Z. Brain arteriovenous malformation treatment using a combination of Onyx and a new detachable tip microcatheter, SONIC : short-term results. AJNR Am J Neuroradiol. 2010;31:947–954. doi: 10.3174/ajnr.A1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Natarajan SK, Ghodke B, Britz GW, Born DE, Sekhar LN. Multimodality treatment of brain arteriovenous malformations with microsurgery after embolization with onyx : single-center experience and technical nuances. Neurosurgery. 2008;62:1213–1225. doi: 10.1227/01.neu.0000333293.74986.e5. discussion 1225-1226. [DOI] [PubMed] [Google Scholar]
- 9.Panagiotopoulos V, Gizewski E, Asgari S, Regel J, Forsting M, Wanke I. Embolization of intracranial arteriovenous malformations with ethylene-vinyl alcohol copolymer (Onyx) AJNR Am J Neuroradiol. 2009;30:99–106. doi: 10.3174/ajnr.A1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pérez-Higueras A, López RR, Tapia DQ. Endovascular treatment of cerebral AVM : our experience with Onyx. Interv Neuroradiol. 2005;11:141–157. doi: 10.1177/15910199050110S118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pierot L, Januel AC, Herbreteau D, Barreau X, Drouineau J, Berge J, et al. Endovascular treatment of brain arteriovenous malformations using onyx : preliminary results of a prospective multicenter study. Interv Neuroradiol. 2005;11:159–164. doi: 10.1177/15910199050110S119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santillan A, Zink W, Knopman J, Riina H, Gobin YP. Balloon-assisted technique for trapped microcatheter retrieval following onyx embolization. A case report. Interv Neuroradiol. 2009;15:453–455. doi: 10.1177/159101990901500414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986;65:476–483. doi: 10.3171/jns.1986.65.4.0476. [DOI] [PubMed] [Google Scholar]
- 14.Stapf C, Mast H, Sciacca RR, Berenstein A, Nelson PK, Gobin YP, et al. The New York Islands AVM Study : design, study progress, and initial results. Stroke. 2003;34:e29–e33. doi: 10.1161/01.STR.0000068784.36838.19. [DOI] [PubMed] [Google Scholar]
- 15.van Rooij WJ, Sluzewski M, Beute GN. Brain AVM embolization with Onyx. AJNR Am J Neuroradiol. 2007;28:172–177. discussion 178. [PMC free article] [PubMed] [Google Scholar]
- 16.Velat GJ, Reavey-Cantwell JF, Sistrom C, Smullen D, Fautheree GL, Whiting J, et al. Comparison of N-butyl cyanoacrylate and onyx for the embolization of intracranial arteriovenous malformations : analysis of fluoroscopy and procedure times. Neurosurgery. 2008;63:ONS73–ONS78. doi: 10.1227/01.neu.0000335015.83616.12. discussion ONS78-ONS80. [DOI] [PubMed] [Google Scholar]
- 17.Weber W, Kis B, Siekmann R, Kuehne D. Endovascular treatment of intracranial arteriovenous malformations with onyx : technical aspects. AJNR Am J Neuroradiol. 2007;28:371–377. [PMC free article] [PubMed] [Google Scholar]
- 18.Zoarski GH, Lilly MP, Sperling JS, Mathis JM. Surgically confirmed incorporation of a chronically retained neurointerventional microcatheter in the carotid artery. AJNR Am J Neuroradiol. 1999;20:177–178. [PubMed] [Google Scholar]