Abstract
Background
Salmonella enterica subspecies enterica serovar Typhimurium is a Gram-negative pathogen causing salmonellosis. Salmonella Typhimurium-targeting bacteriophages have been proposed as an alternative biocontrol agent to antibiotics. To further understand infection and interaction mechanisms between the host strains and the bacteriophages, the receptor diversity of these phages needs to be elucidated.
Methodology/Principal Findings
Twenty-five Salmonella phages were isolated and their receptors were identified by screening a Tn5 random mutant library of S. Typhimurium SL1344. Among them, three types of receptors were identified flagella (11 phages), vitamin B12 uptake outer membrane protein, BtuB (7 phages) and lipopolysaccharide-related O-antigen (7 phages). TEM observation revealed that the phages using flagella (group F) or BtuB (group B) as a receptor belong to Siphoviridae family, and the phages using O-antigen of LPS as a receptor (group L) belong to Podoviridae family. Interestingly, while some of group F phages (F-I) target FliC host receptor, others (F-II) target both FliC and FljB receptors, suggesting that two subgroups are present in group F phages. Cross-resistance assay of group B and L revealed that group L phages could not infect group B phage-resistant strains and reversely group B phages could not infect group L SPN9TCW-resistant strain.
Conclusions/Significance
In this report, three receptor groups of 25 newly isolated S. Typhimurium-targeting phages were determined. Among them, two subgroups of group F phages interact with their host receptors in different manner. In addition, the host receptors of group B or group L SPN9TCW phages hinder other group phage infection, probably due to interaction between receptors of their groups. This study provides novel insights into phage-host receptor interaction for Salmonella phages and will inform development of optimal phage therapy for protection against Salmonella.
Introduction
Emergence of antibiotic-resistant pathogens due to abuse of various antibiotics is driving the development of alternative approaches to pathogen control. Bacteriophages are considered a possible alternative biocontrol agent for bacterial pathogens [1], [2]. This approach has advantages including narrow species specificity and safety for human applications [3]. As an example, a clinical trial in which volunteers were given oral doses of T4 phage indicated that it was safe [4]. In addition, a cocktail (ListShield™, Intralytix, Inc., Baltimore, MD, USA) of Listeria-infecting bacteriophages was approved by the US Food and Drug Administration in 2006, gaining the status of “Generally Recognized as Safe” [2], [5], supporting that bacteriophage may be a good candidate as a biocontrol agent for human applications.
Salmonella is a Gram-negative foodborne pathogen causing 1.4 million cases of salmonellosis including 17,000 hospitalization and 600 deaths every year in US [6], [7]. S. enterica serovar Typhimurium is common serotype in human infection and is frequently isolated from clinical and non-clinical samples from chicken sources. A large proportion of S. Typhimurium strains are resistant to several antimicrobial drugs, for example the multi-drug resistant S. Typhimurium phage type DT104 [8]. Therefore, use of S. Typhimurium bacteriophages is now getting more attractive as an alternative approach in the treatment for antibiotic-resistant pathogens.
Recent reports have described the isolation of new Salmonella bacteriophages and evaluation of their bactericidal effects [9]–[12]. For example, Salmonella-specific phage st104a or st104b reduced the bacterial cell number by up to 2 logs within 1 h of each phage infection [12]. Φ25 phage reduced S. Typhimurium viable cell number up to 2.19 logs within 24 h [13], [14]. However, the rapid emergence of phage-resistant Salmonella is an obstacle to effective biocontrol using phages [5], [14]–[17]. To reduce the impact of phage-resistance, phage cocktails have been developed and found to be effective in control of phage-resistant Salmonella [15], [18]–[20]. For example, a phage cocktail containing 45 different phages reduced Salmonella cell numbers up to 5 log in 2 h [15]. The phage cocktail approach can also broaden the host range, for example, one phage cocktail designed for serovar Typhimurium increased the host range to include S. enterica serovar Enteritidis and serovar Kentucky [21].
Because attachment of bacteriophage to the specific receptor of the host bacteria is the critical first step of phage infection [22], mutation of the receptor is the most frequent route to phage-resistance of the host. To date, several Salmonella phage receptors are known including FhuA [23], TolC [24], BtuB [25], [26], OmpC [27], Vi capsular antigen [28], lipopolysaccharide (LPS) [29], and flagella [13]. The study of phage receptors is expected to provide insight into the emergence of phage-resistance in Salmonella and guide optimization of phage cocktails for Salmonella control.
In this study, host receptors for 25 new Salmonella phages were determined using a phage-resistant Tn5-insertion random mutant library of S. Typhimurium. Cross infection studies with these phages and resistant strains revealed novel phage-host interactions and infection mechanisms. Further investigation of diversity of host receptors in Salmonella phages will increase our ability to circumvent phage resistance using phage cocktails and thus prevent food spoilage due to S. Typhimurium.
Materials and Methods
Bacterial Strains and Growth Conditions
Bacterial strains used in this study are listed in Table 1. All strains were grown in Luria-Bertani (LB) broth medium (Difco, Detroit, MI, USA) at 37°C with shaking for 12 h. Salmonella enterica serovar Typhimurium strain SL1344 was used for isolation of Salmonella-infecting phages from the collected samples, and prophage-free S. Typhimurium strain LT2C [30] (Cancer Research Center, Colombia, MO, USA) was used for purification of phages.
Table 1. Host range of bacteriophages isolated.
| Host | Lytic spectrumsa,b | Referencesd | |||||||||||
| GroupF-I | GroupF-II | Group B | Group L | ||||||||||
| I | II | III | IV | V | VI | VII | VIII | IX | X | XI | XII | ||
| Salmonella enterica | |||||||||||||
| subsp. enterica serovar Typhimurium SL1344 | T | T | T | T | T | C | C | C | C | C | T | C | NCTC |
| subsp. enterica serovar Typhimurium UK1, LT2, LT2Cc* | T | T | T | T | T | C | C | C | C | C | T | T | [66], [67], [30] |
| subsp. enterica serovar Typhimurium ATCC 14028 | – | – | – | T | I | T | T | T | T | T | T | T | ATCC |
| subsp. enterica serovar Typhimurium ATCC 19586 | C | T | C | T | T | C | C | C | C | T | T | C | ATCC |
| subsp. enterica serovar Typhimurium ATCC 43147 | T | T | T | T | T | – | I | – | – | I | T | C | ATCC |
| subsp. enterica serovar Typhimurium DT104 | T | T | T | T | T | – | – | – | – | – | T | C | [68] |
| subsp. enterica serovar Enteritidis ATCC 13078 | – | – | – | – | – | C | C | T | T | C | T | C | ATCC |
| subsp. enterica serovar Typhi Ty 2-b | – | – | – | – | – | – | T | – | – | T | – | – | IVI |
| subsp. enterica serovar Paratyphi A IB 211 | T | – | – | – | T | C | C | C | C | C | – | – | IVI |
| subsp. enterica serovar Paratyphi B IB 231 | – | – | – | – | – | T | T | T | T | T | T | C | IVI |
| subsp. enterica serovar Paratyphi C IB 216 | – | – | – | – | – | T | T | T | T | T | T | – | IVI |
| subsp. enterica serovar Dublin IB 2973 | – | – | – | – | – | – | T | T | T | C | – | – | IVI |
| subsp. arizonae ATCC 13314 | – | T | T | T | T | – | – | – | – | – | – | – | ATCC |
| subsp. arizonae ATCC 12324 | – | T | T | T | T | C | C | C | C | C | – | – | ATCC |
| subsp. salamae ATCC 15793 | T | T | T | T | T | – | – | – | – | – | – | – | ATCC |
| subsp. salamae ATCC 43972 | – | – | – | – | – | – | – | – | – | C | – | – | ATCC |
| subsp. indica ATCC 43976 | – | – | – | – | – | T | C | T | T | C | – | – | ATCC |
| subsp. houtenae ATCC 43974 | – | – | – | – | – | – | – | – | – | – | – | – | ATCC |
| subsp. diarizonae ATCC 43973 | – | – | – | – | – | T | T | T | C | T | – | – | ATCC |
| E. coli | |||||||||||||
| K-12, DH5α, DH10B | – | – | – | – | – | C | C | C | C | C | – | – | [69], ATCC, [70] |
| O157:H7 ATCC 43888 | – | – | – | – | – | – | – | C | – | – | – | – | ATCC |
| O157:H7 ATCC 43895 | – | – | – | – | – | – | – | T | – | – | – | – | ATCC |
| Gram-negative bacteria | |||||||||||||
| Shigella flexineri 2a strain 2457T | – | – | – | – | – | C | – | C | C | – | – | – | IVI |
| Shigella boydii IB 2474 | – | – | – | – | – | – | – | – | – | – | – | – | IVI |
| Vibrio fischeri ES-114 ATCC 700601 | – | – | – | – | – | – | – | – | – | – | – | – | ATCC |
| Pseudomonas aeruginosa ATCC 27853 | – | – | – | – | – | – | – | – | – | – | – | – | ATCC |
| Cronobacter sakazakii ATCC 29544 | – | – | – | – | – | – | – | – | – | – | – | – | ATCC |
| Gram-positive bacteria | |||||||||||||
| Enterococcus faecalis ATCC 29212 | – | – | – | – | – | – | – | – | – | – | – | – | ATCC |
| Staphylococcus aureus ATCC 29213 | – | – | – | – | – | – | – | – | – | – | – | – | ATCC |
| Bacillus cereus ATCC 14579 | – | – | – | – | – | – | – | – | – | – | – | – | ATCC |
| Listeria monocytogenes ATCC 19114 | – | – | – | – | – | – | – | – | – | – | – | – | ATCC |
Lytic spectrum: I contains SPN2T, SPN3C, and SPN13B; II contains SPN8T and SPN9T; III contains SPN11T, SPN16C; IV, SPN4S, and SPN19; V contains SPN5T and SPN6T; VI contains SPN7C and SPN9C, VII, SPN10H; VIII contains SPN12C and SPN17T; IX, SPN14; X, SPN18; XI contains SPN1S, SPN2TCW, SPN4B, SPN6TCW, SPN8TCW, and SPN13U; XII, SPN9TCW.
C, clear plaque; T, turbid plaque; I, inhibition zone; –, no infection.
Prophage-cured strain of S. Typhimurium LT2.
NCTC, National Collection of Type Cultures; ATCC, American Type Culture Collection; IVI, International Vaccine Institute.
Bacteriophage Isolation and Propagation
Bacteriophages isolated in this study were listed in Table 2. No live chickens were used in this study. Seventy-six samples obtained from chicken feces collected from farms and commercially processed broiler skins obtained from markets were used as sources for isolation of Salmonella-specific bacteriophages. The chicken feces were collected with permissions from the farm owners and the samples were collected for the purpose of this research only. Twenty-five grams of each sample were mixed with 225 ml of sodium chloride–magnesium sulfate (SM) buffer (100 mM NaCl, 10 mM MgSO4·7H2O and 50 mM Tris·HCl, pH 7.5) without gelatin in sterile bags. Twenty-five milliliters of each homogenized sample were mixed with 25 ml of 2× concentrated LB broth and incubated with shaking at 37°C for 12 h. After centrifugation (5,000×g for 10 min), the supernatant was filtered using 0.22-µm pore size filters (Millipore, Billerica, MA, USA). Ten milliliters of each filtered sample were mixed with 50 ml LB broth with 107 CFU/ml of overnight cultured S. Typhimurium SL1344. The mixture was incubated with shaking at 37°C for 12 h. After centrifugation (5,000×g for 10 min), the supernatant was filtrated using 0.22 µm pore size filters. The presence of phages was assessed using a plaque forming assay with molten 0.4% LB soft agar containing 107 CFU/ml of S. Typhimurium SL1344. After incubation at 37°C for 12 h, individual plaques were picked and eluted with 1 ml of SM buffer without gelatin. Plaque isolation and elution were repeated more than five times for pure isolation of individual phages in S. Typhimurium LT2C. One liter of exponentially growing S. Typhimurium LT2C (OD600 nm = 1.0) was infected with each SPN phage at a multiplicity of infection (MOI) of approximately 1 and incubated with shaking at 37°C for 4 h. Cell debris was removed by centrifugation at 5,000×g for 10 min and filtered using 0.22-µm pore size filters. Phage particles were precipitated from the filtrate by addition of 10% polyethylene glycol 6,000 (Sigma, St. Louis, MO, USA). Finally, a stepped CsCl density ultracentrifugation (himac CP 100β, Hitachi, Japan) with step densities of 1.3, 1.45, 1.5, and 1.7 g/ml at 78,500×g for 2 h was conducted at 4°C. The bands of viral particles were withdrawn from the tube with a syringe and dialyzed using 1 L of SM buffer for 1 h and stored at 4°C.
Table 2. Characteristics of the isolated S. Typhimurium-specific bacteriophages and their identified receptors.
| Groupa (Family) | Phage | Source | Mutated genes of the phage-resistant strains |
| F-I (Siphoviridae) | SPN2T | Chicken feces1 | flgK, fliR b or fliC |
| SPN3C | Chicken feces2 | flgK, fliR or fliC | |
| SPN8T | Processed broiler skin1 | flgK, fliR or fliC | |
| SPN9T | Processed broiler skin2 | flgK, fliR or fliC | |
| SPN11T | Soil1 | flgK, fliR or fliC | |
| SPN13B | Water1 | flgK, fliR or fliC | |
| SPN16C | Chicken feces3 | flgK, fliR or fliC | |
| F-II (Siphoviridae) | SPN4S | Processed broiler skin3 | flgK or fliR |
| SPN5T | Processed broiler skin4 | flgK or fliR | |
| SPN6T | Processed broiler skin5 | flgK or fliR | |
| SPN19 | Processed broiler skin6 | flgK or fliR | |
| B (Siphoviridae) | SPN7C | Processed broiler skin7 | btuB c |
| SPN9C | Processed broiler skin2 | btuB | |
| SPN10H | Soil2 | btuB | |
| SPN12C | Soil3 | btuB | |
| SPN14 | Soil4 | btuB | |
| SPN17T | Silky fowl feces | btuB | |
| SPN18 | Processed broiler skin8 | btuB | |
| L (Podoviridae) | SPN1S | Water2 | rfaL d or rfbG |
| SPN2TCW | Chicken feces1 | rfaL or rfbG | |
| SPN4B | Processed broiler skin3 | rfaL or rfbG | |
| SPN6TCW | Processed broiler skin5 | rfaL or rfbG | |
| SPN8TCW | Processed broiler skin1 | rfaL or rfbG | |
| SPN13U | Water3 | rfaL or rfbG | |
| SPN9TCW | Processed broiler skin2 | rfaL or rfbG |
F-I and F-II, flagella-specific phage group; B, BtuB-specific phage group; L, LPS-specific phage group.
flgK, fliR mutations were complemented using pACYC184 vector expressing the flgK + or fliR + gene.
btuB mutation was complemented using pACYC184 vector expressing the btuB + gene.
rfaL mutation was complemented using pUHE21-lacI q vector expressing the rfaL + gene.
Transposon Mutagenesis and Receptor Screening
Random insertion mutagenesis of S. Typhimurium SL1344 was performed using the EZ-Tn5™ <R6Kγori/KAN-2>Tnp Transposome kit (Epicentre, Madison, WI, USA) according to manufacturer’s procedure. The transposon construct was obtained by treating pMOD3 with PvuII restriction enzyme, and gel purifying the fragment from a 1% agarose gel using the QIAquick Gel Extraction Kit (Qiagen, Valencia, CA, USA). Electrocompetent cells were prepared as follows: Fifty milliliter of LB broth inoculated at 1% with an overnight culture of S. Typhimurium SL1344 was incubated with shaking at 37°C for 1.5 h. Cells were then harvested by centrifugation at 5,000×g for 10 min, and the pellet was washed three times with 1 ml ice-cold molecular grade water and resuspended with 100 µl ice-cold molecular grade water. The complexes were electroporated into S. Typhimurium SL1344 using the Gene-Pulser Xcell system (Bio-Rad, Hercules, CA, USA) at 2.45 kV, 200 Ω and 25 µF in 2 mm electroporation cuvettes. Transformants were selected on LB agar plates containing kanamycin (Kan, 50 µg/ml), and individual colonies were cultured and stored in LB broth with Kan (50 µg/ml) containing 15% glycerol at −80°C.
To screen mutant strains resistant to each SPN phage, the mutant library was duplicated in the 96-well plates containing LB broth supplemented with 50 µg/ml of Kan. The SPN phage was added to one of those duplicated 96-well plates (MOI = 10) after shaking at 37°C for 1.5 h and growth inhibition was compared with the corresponding 96-well plate not inoculated with phage. All plates were incubated at 37°C for an additional 3 h. Phage resistance mutants were identified by comparing the optical density at 600 nm of the plates with and without phage using an iMark microplate absorbance reader (Bio-Rad). Rescue cloning of transposed genomic DNA and partial sequencing was conducted to identify the Tn5 transposon insertion sites according to the manufacturer’s protocol.
Construction of Deletion Mutants and Complementation Plasmids
S. Typhimurium SL1344 derivatives with deletions of flgK, fliR, fliC, fljB, fliC/fljB or rfaL genes were constructed using the lambda red recombination method [31]. The kanamycin resistance (KanR) cassette from plasmid pKD13 was amplified using primers specific for each gene, for example, flgK-lamb-F1 and flgK -lamb-R1 for flgK. Sequences of all primers for these constructs are provided in Table S1. The polymerase chain reaction (PCR) products were transformed into S. Typhimurium SL1344 harboring pKD46 and integrated into the chromosomal flgK, fliR, fliC, fljB or rfaL genes. Finally, the KanR cassette was removed using pCP20 plasmid following the procedure of Cherepanov et al. [32]. For construction of SL1344 ΔfliC ΔfljB, phage P22-mediated transductions were performed as described previously [19]. For complementation of the flgK, fliR or rfaL deletion mutations, the flgK, fliR and rfaL genes were amplified from S. Typhimurium SL1344 using the primers flgK-pACYC-F and flgK-pACYC-R for flgK, fliR-pACYC-F and fliR-pACYC-R for fliR, rfaL-pUHE-F and rfaL-pUHE-R for rfaL. The PCR products were digested with BamHI and EcoRI and ligated into BamHI/EcoRI-digested pACYC184 [33] or pUHE21-lacI q expression vector [34]. Plasmid constructs were confirmed by sequencing, and then transformed into deletion mutant strains selecting for ampicillin (Amp)-resistant transformants on LB with 50 µg/ml of Amp. Transformants were confirmed by colony PCR and susceptibility to SPN phages was tested.
Electron Microscopy
The morphology of CsCl-purified SPN phages was determined using transmission electron microscopy (TEM). Concentrated viral samples were diluted with SM buffer without gelatin and 5 µl of each phage sample was applied to the surface of carbon coated copper grids. Excess volume was removed by carefully touching the side of grid with filter paper and 5 µl 2% uranyl acetate (pH 4.0) was spotted on the grid for negative staining and removed after a short interval. The prepared samples were observed using TEM (LIBRA 120, Carl Zeiss, Switzerland) at 80 kV. Taxonomy of the SPN phages was determined according to the guidelines of the International Committee on Taxonomy of Viruses [35].
Host Range Determination by Spotting Assay
A 100-µl aliquot of bacterial culture was added to 6 ml molten 0.4% LB agar and then poured on a 1.5% LB agar plate. After solidification of the top agar, 10 µl serially diluted phage suspension ranging from 102 to 105 plaque forming unit/ml was spotted on the top agar and the plates were incubated at 37°C for 12 h. After incubation, the sensitivity of indicator strains to the tested phages was determined by degrees of clearing in the spots or plaques (Table 1). The plaque assay was performed in triplicate.
Isolation of Phage-resistant Strains and Determination of Cross Resistance
To investigate influence of resistance against one type of receptor to infection by phages using different receptors, resistance strains were developed against phages and then they were used for the infections by phages using different host receptors. Group L phage-resistant strains showing resistance to re-infection were isolated using high-titer overlay assay following modified Kim and Ryu’s protocol [26]. In this modified protocol, separate colonies of group L phage-resistant strains were obtained by additional streaking on LB agar plate. Because high-titer overlay assay did not work for isolation of transiently phage-resistant strains by group F, group B, and group L SPN9TCW phage infections, they were isolated using high-titer broth assay to increase the yield of the phage-resistant strains and to maintain resistance in the presence of phages. For the high-titer broth assay, phages were added to an LB broth culture of S. Typhimurium LT2C (OD600 nm = 1.0) at MOI = 100, and the culture was incubated with shaking at 37°C until the OD600 nm reached 1.0, again. To remove excessive phages, the phage-infected cells were then harvested by centrifugation at 5,000×g for 10 min, resuspended in 200 µl ice-cold molecular grade water and used as a host for the second infection of SPN phages using different host receptors. The host resistance to the second infection was monitored using plaquing assays as described above.
Lysogen Induction
All phage-resistant strains of S. Typhimurium LT2C were cultivated at 37°C until OD600 nm reached to 1.0 and 0.5 µg/ml of mitomycin C (Sigma) was added to the cultures. Then, these cultures were additionally incubated at 37°C for 2 h. After incubation, the cells were removed by centrifugation and filtration and the supernatant was collected. The spotting assay of this supernatant with S. Typhimurium LT2C was conducted to confirm the lysogen formation. To confirm the unstable lysogen formation of group F phage-resistant strains, the group F, B, L-SPN9TCW phage-resistant strains were plate in green plate (Evans blue uranine agar plate, 0.5% NaCl, 1% Tryptone, 0.5% Yeast extract, 0.5% K2HPO4, 0.04 M Glucose, 0.04% Evans blue, 0.04% Uranine, and 1.5% Micro agar, final concentration) as the procedure developed by Chan et al. [19].
Real-time Reverse Transcription (RT)-PCR
Total RNA was isolated from S. Typhimurium using the RNeasy Mini Kit (Qiagen) and converted to cDNA using the Omniscript RT Kit (Qiagen) and random hexamers (Invitrogen, Carlsbad, CA, USA) using manufacturer’s instructions. Quantitative real-time RT-PCR was performed as previously described [36] with primers listed in Table S1.
Sodium Dodecyl Sulfate-polyacrylamide Gel Electrophoresis (SDS-PAGE)
Flagellin of S. Typhimurium was isolated as previously described [37], and suspended in loading buffer (0.05 M Tris·HCl pH 8.0, 1.6% SDS, 25% glycerol, 5% 2-mercaptoethanol, 0.003% bromophenol blue, final concentration). Samples were heated in boiling water for 3 min, and then loaded in a well of a 12% Ready Gel Tris·HCl gel (Bio-Rad) in 1X Tank Buffer (0.025 M Tris, 0.192 M glycine, and 0.1% SDS, final concentration). Gel electrophoresis was performed using Mini-PROTEAN 3 (Bio-Rad) at 20 mA for 45 min. The gel was stained in a staining solution containing 0.25% Coomassie Brilliant Blue R250 and destained with a destaining solution containing 30% methanol and 10% glacial acetic acid.
Results
Bacteriophage Isolation
Between September and December 2009, 25 bacteriophages were newly isolated from 18 of 76 samples (23.7% phage recovery frequency). All phages in Table 2 were designated as Salmonella Phage Number (SPN) and specific numbers were used to indicate the sample sources and sometimes characters were used to differentiate the isolated phages from the same samples, respectively.
Grouping of Bacteriophages Based on their Receptors
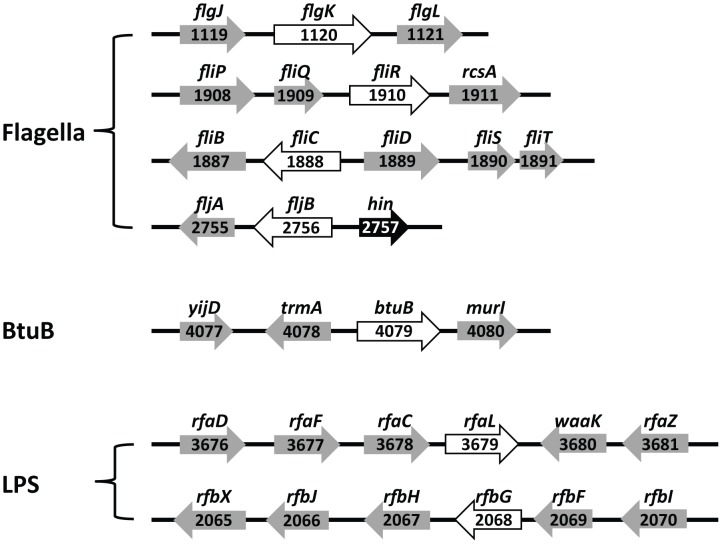
To determine the host receptors for 25 phages, a Tn5 random mutant library of S. Typhimurium SL1344 containing thousands of Tn5-inserted mutants was constructed and mutant strains resistant to each phage via inactivation of host receptor genes by Tn5 insertions were screened. Interestingly, sequence analysis of the Tn5 insertions in the phage-resistant mutants revealed only three different types of genes: flagellar production genes, the gene encoding the vitamin B12 uptake outer membrane protein, and genes involved in LPS-related O-antigen production. The Tn5 random mutant library screening results were confirmed by targeted inactivation of the identified genes by lambda red recombination method and complementation experiments. The host receptor genes deleted by the lambda red recombination method are indicated in the receptor gene clusters presented in Fig. 1. Based on the deleted specific genes for formation of phage receptors, 25 phages were grouped into group F, group B, and group L phages, respectively (Table 2 and Fig. 2A).
Figure 1. Genetic map of the receptor gene clusters and the mutated genes of resistant strains.
Genes involved in the synthesis of flagella (flgK, fliQ, fliC and fljB), BtuB (btuB), and LPS (rfaL and rfbG) inactivated by transposon insertion were indicated by open arrows. Black arrow marked with hin is a promoter that transcribes the fljB gene. The numbers are locus-tag numbers indicating the locations of the genes in the genome sequence.
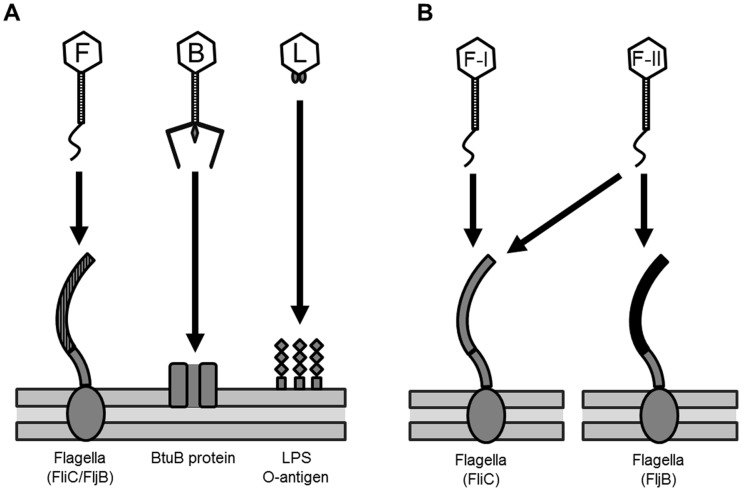
Figure 2. Host receptors of SPN phages.
F, F-I, F-II, B, and L marked in the phage heads indicate group F, group F-I, group F-II, group B, and group L phages, respectively. (A) Group F, group B, and group L phages use flagella (FliC/FljB), BtuB, and O-antigen of LPS as host receptors, respectively. (B) Group F-I and group F-II phages use FliC (grey-colored) and FliC/FljB (black-colored) in the host flagella.
The deleted genes involved in flagella production included genes encoding the flagella hook-filament junction protein (flgK), a putative component of the type III flagella export apparatus (fliR), and the gene encoding flagellin (fliC). Because S. Typhimurium expresses either one of two flagellin genes, fliC or fljB [38], we tested whether the group F phages can use both flagellins by phage infection analysis of fliC and fljB deletion mutants. The group F phages can be categorized into two groups, F-I and F-II, as shown on Table 3 and Fig. 2B. The group F-I phage could not infect the fliC mutant or the fliC/fljB double mutant, but could infect the fljB mutant, suggesting that the group F-I phage can only use FliC as a receptor. Group F-II phage could not infect the fliC/fljB double mutant but could infect the fliC and the fljB single mutants, suggesting that the group F-II phage can use either FliC or FljB as a receptor (Table 3 and Fig. 2B).
Table 3. Flagellin-targeting phages: receptor and sensitivity patterns based on specific gene mutation.
| Strain genotype | Receptor present | Resistance profilesa,b | |
| F-I phage | F-II phage | ||
| ΔfliC | FljB only | R | S |
| ΔfljB | FliC only | S | S |
| ΔfliC ΔfljB | neither | R | R |
F-I, flagella-targeting phage group I; F-II, flagella-targeting phage group II.
S, sensitive to infection; R, resistant to infection.
One group of resistant mutants has deletion mutations in the btuB gene encoding the membrane transporter for vitamin B12, suggesting that BtuB is a group B phage receptor. The mutated genes in the O-antigen biosynthesis are O-antigen ligase (rfaL) and CDP glucose 4,6-dehydratase (rfbG). Complementation of the deleted genes with pACYC184 and pUHE21-lacq expression vectors containing the wild-type genes restored susceptibility, supporting that O-antigen is a receptor for group L phage infection. Overall, 11 out of 25 phages use flagella (group F phage), seven out of 25 use BtuB (group B phage), and another seven out of 25 use LPS-related O-antigen (group L phage) as receptors. Although the Salmonella outer membrane proteins (OMPs) such as TolC [24], FhuA [23] and OmpC [27] are known receptors for some phages, no phages using those receptors was present in this set of 25 phages. It is not clear why BtuB was the only OMP detected as a receptor in this study.
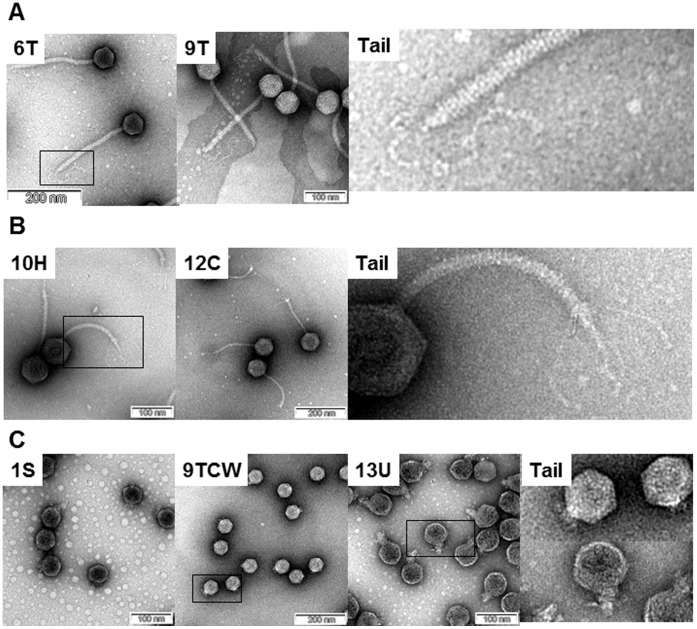
Morphology
All 25 phages could be categorized into three morphological groups (Fig. 3). Interestingly, this morphological grouping is correlated with the grouping of Salmonella-specific phages based on their receptors (Table 2). All of the group F and B phages have isometric heads and non-contractile, cross-banded tails that are longer than the tails of the group L phages (Fig. 3). These phages can be classified into the B1 morphotype of the Siphoviridae family, although the group F phages have a single, long, kinky tail fiber structure and the group B phages have four or five L-shaped fibers (Fig. 1A and 1B). The group L phages are classified as members of the Podoviridae family. They have isometric heads with very short tails that are distinct from other groups.
Figure 3. TEM morphology of representative SPN phages.
Each phage name is indicated in the upper left corner of the picture. The representative tails of each group of phage were marked with boxes and the enlarged pictures were shown on the right. (A) Phages using flagella as a receptor. (B) Phages using BtuB as a receptor. (C) Phages using LPS as a receptor.
Host Range of the Isolated Bacteriophages
Infection analysis of 25 Salmonella-specific bacteriophages was conducted with 21 Salmonella strains, five E. coli strains and nine other species of Gram-negative and Gram-positive bacteria (summarized in Table 1). In general, SPN bacteriophages infect S. Typhimurium strains but not other Gram-negative and Gram-positive bacteria, suggesting that they are specific to S. Typhimurium. The group F phages also infect S. enterica subsp. arizonae and subsp. salamae, and the group B phages can infect several strains of E. coli, indicating that these bacteriophages have a host range that extends to other Salmonella subspecies or E. coli strains. In addition, group L phages and some group F phages infect S. Paratyphi. The group B phages have much broader host range than the group F and L phages. They can infect E. coli and Shigella flexneri strains as well as Salmonella (Table 1), suggesting that the BtuB proteins of S. Typhimurium, E. coli, and Shigella flexneri are similar. Comparative sequence analysis of BtuB proteins in the group B phage susceptible strains S. Typhimurium LT2, E. coli MG1655 and Shigella flexineri 2a strain 2457T revealed >87% identity at the amino acid level between S. Typhimurium and the other two species, whereas S. Typhimurium and Vibrio fischeri ES-114, which is not susceptible to group B phage, share <35% identity at the amino acid level. These findings support the hypothesis that the group B phage receptor motifs are shared among Salmonella, E. coli and Shigella. Comparative host range analysis of group F-I and F-II phages revealed that F-II phages infect a larger number of S. Typhimurium isolates (data not shown), probably because the F-II phages can use either the FliC or the FljB flagellin as a receptor while the F-I phages can only use FliC (Table 3 and Fig. 2B).
Lysogenization
It is intriguing that while the group F and L phages generally make turbid plaques, and thus may be temperate phages, the group B phages make clear plaques and may be virulent phages [39]. Induction experiments in which mitomycin C was used to induce lytic growth indicate that the group L phage-resistant S. Typhimurium LT2C strains carry an inducible prophage. In contrast, mitomycin C treatment of the group L SPN9TCW phage-resistant and group B phage-resistant Salmonella strains did not yield phage, indicating that these phages do not make lysogens in the LT2C strain consistent with the clear plaque morphology (Table 1 and 3). Most of the group F phage-resistant Salmonella strains did not yield phage after treatment with mitomycin C even though they make turbid plaques. Five percent of the group F phage-resistant Salmonella made phage in response to mitomycin C, but they also lose resistance easily upon subculturing in the absence of the phages, suggesting the possibility of formation of unstable lysogens or pseudolysogens [40] (Table 4). To confirm if transient resistance is due to unstable lysogeny or pseudolysogeny, we conducted the green plate (Evans blue uranine agar plate) experiment (Fig. S1). In the green plate experiment, only the cells lysed by phage induction make blue colonies due to pH change. It revealed that while the resistant strains to the virulent phages in group B and group L-SPN9TCW did not show any blue colony, the resistant strains to group F phages did show small number of blue colonies (approximately 5% of all colonies) in the green plates. These results indicate that a few of the strains resistant to group F phages were lysed, suggesting that group F phages do not form stable lysogens.
Table 4. Cross resistance of phage-resistant strains.
| Resistant strain | Phage sensitivity patterna | Mitomycin C inductionb | ||
| Group F (Flagella) | Group B (BtuB) | Group L (LPS) | ||
| Group F | R1 | S | S | Nc |
| Group B | S | R1 | R1 | N |
| Group L (SPN9TCW) | S | R1 | R1 | N |
| Group L (Other) | S | S | R2 | I |
R1, transiently resistant; R2, stably resistant; S, sensitive.
N, not induced; I, induced.
Although most of the group F phage-resistant Salmonella were not induced, <5% of the resistant Salmonella were induced by mitomycin C.
Cross-resistance of Phage-resistant Salmonella to the Different Receptor Group Phages
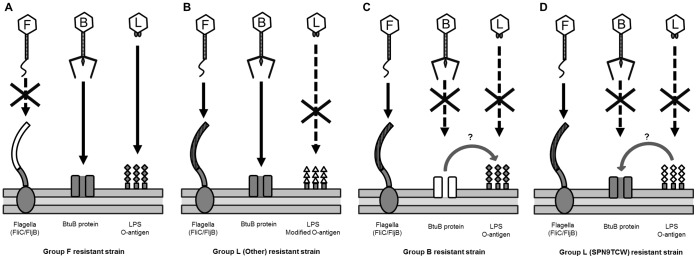
To understand the interaction of phage with the specific host receptors, derivatives of S. Typhimurium LT2C that are resistant to the group F, group B and group L phages described here were isolated and characterized. Group B phage-resistant Salmonella [26] were transiently resistant to re-infection with group B phages, and most group F phage-resistant and group L SPN9TCW phage-resistant strains also showed transient resistance to re-infection with phages from their own group. All group L phage-resistant strains, except for the strain resistant to phage SPN9TCW, showed stable phage resistance to group L phages. Interestingly, all group L phage-resistant strains except those resistant to SPN9TCW were lysogens, suggesting that the resistance for the group L phages is due to prevention of superinfection by a stable prophage (Table 4 and Fig. 4B) [41], [42]. Cross-infection of group F phages on other phage-resistant strains showed sensitivity to these phages, suggesting no mutual influence between flagellin and other phage receptors on the sensitivity to the phages (Table 4 and Fig. 4). However, cross-infection of group B phages on group L phage-resistant strains yielded two different patterns. While the group L phage-resistant strains are sensitive, the SPN9TCW phage-resistant strain is resistant to group B phage infection, depending on the formation of lysogen (Table 4 and Fig. 4BD). Furthermore, group L phages were not able to infect group B phage-resistant strains, suggesting a possible influence between the BtuB and LPS receptors on the sensitivity to the phages (Table 4 and Fig. 4C).
Figure 4. Cross-resistance of phage-resistant Salmonella to the different receptor group phages.
F, B, and L marked in the phage heads indicate group F, group B, and group L phages, respectively. Each receptor in the phage-resistant strains is white-colored. (A) Group F phage-resistant strain is sensitive to group B and group L phages. (B) Group L phage-resistant strain is sensitive to group F and group B phages, but resistant to group L phages, due to modification of O-antigen of LPS. Modified O-antigen is indicated by white triangles. (C) Group B phage-resistant strain is sensitive to group F, but resistant to group B as well as group L phages, probably due to putative interaction between BtuB and O-antigen of LPS. (D) Group L (SPN9TCW phage)-resistant strain is sensitive to group F, but resistant to group B as well as group L phages, probably due to putative interaction between BtuB and O-antigen of LPS.
Discussion
The details of the molecular interactions between phages and their host receptors that determine host specificity are not fully understood yet. Here, we isolated 25 Salmonella-specific phages, identified their receptors, studied their host specificity, and examined cross-resistance among the phages and phage resistant hosts. Although this study on Salmonella phage receptors using 25 phages does not represent the complete range of infection mechanisms used by Salmonella-infecting bacteriophages, the results provide novel insights into general host-phage interactions of typical Salmonella-infecting bacteriophages.
Bacteriophages tend to use structures exposed on the outer membrane of the host bacteria as a receptor because they are easily accessible. Unexpectedly, only three kinds of receptors were identified in this study, flagella, O-antigen, and the outer membrane protein BtuB, although several other outer membrane proteins, including FhuA, TolC, and OmpC, are characterized as phage receptors of Salmonella. One possible reason may be the complex nature of Salmonella Typhimurium LPS [43], [44], which may block access of phage to some outer membrane proteins, making it more challenging to isolate those phages. In a seeming contradiction, LPS may help attachment of group B phage to BtuB on a S. Typhimurium host. T5 phage, for example, has both a receptor-binding tail protein Pb5 and a L-shaped tail fiber protein on the phage tail that targets the host outer membrane protein and LPS, respectively [45], [46]. The Pb5 as a major host specificity protein is reported to mediate irreversible binding to a specific outer membrane protein and the L-shaped tail fiber protein as a helper protein provides reversible binding to LPS. Therefore, the L-shaped tail fiber protein increases the infection rate of T5 phage by stabilization of binding between phage and an outer membrane receptor via Pb5. Group B phages are in the same family as T5 phage, Siphoviridae, and have a similar tail structure containing an Pb5-like protein possibly targeting BtuB and an L-shaped tail fiber protein possibly targeting LPS (Fig. 3). Due to this similarity between T5 and group B phages, it is suggested that this tail fiber protein may help the binding of Pb5-like protein to BtuB to increase the infection rate of group B phages, but this proposed binding mechanism needs further study.
Morphological characterization of the group F and group L bacteriophages also provided insight into the interaction of these phages with host receptors. The group F phages have relatively long, non-contractile and cross-banded tails with a single and twisted tail fiber structure. This structure is very similar to that of chi phage that infects E. coli, Salmonella and Serratia through flagella filament receptors [47], [48], suggesting possible interaction between the group F twisted tail fibers and bacterial flagella. Group L phages are morphologically belong to Podoviridae and use LPS as a main receptor like other phages including ε15 [49], [50], P22 [51] and T7 [52], which all interact with LPS via major host specificity proteins. However, Salmonella phages of Myoviridae family were not isolated in this study. It is not clear why we failed to isolate phages of Myoviridae family. The standard phage isolation protocol employed in our study may not be suitable for isolation of Salmonella phages in Myoviridae family because the genome sizes of Salmonella phages of Myoviridae family except for Pedovirinae subfamily are generally bigger than those of other family phages [53]–[57]. Otherwise, there might be unknown bias in the phage isolation.
Host range analysis of group F-I phages showed that they successfully infected all S. Typhimurium strains tested except strain ATCC 14028. It is not clear why the group F-I phages that use only FliC as a receptor could not infect ATCC 14028 while the group F-II phages could. The complete genome sequence of strain ATCC 14028 (GenBank accession number CP001363) showed that it has a fliC gene and multiple sequence alignment with the fliC genes of susceptible Salmonella strains revealed no sequence differences. Real-time RT-PCR and SDS-PAGE analysis confirmed that the fliC gene is expressed and translated for flagella formation, indicating that FliC in the strain ATCC 14028 is functional (data not shown). The group B phages also infected all S. Typhimurium strains except one, strain DT104. Sequencing and real-time RT-PCR analyses of the btuB gene in strain DT104 showed that it is expressed (data not shown), so it is not clear why the strain is resistant. These two examples imply that there may be an additional unknown factor(s) that makes the phage and host receptor interaction more specific and complicated. However, only S. Typhimurium ATCC 14028 has Gifsy-3 prophage, so this prophage could cause superinfection exclusion to group F-I phages.
The phages that can make lysogen normally make turbid plaques but many other factors are involved in turbid plaque formation that it is not simple to distinguish lysogen formation based on plaque turbidity. While the lysogen generally resists superinfection by expression of the phage genes, acquisition of phage resistance by host mutation has been hardly found in lysogen.
Therefore, the aim of this lysogenization experiment was to test whether the resistance against phage infection was due to lysogenization or other factors related with a host receptor. To confirm their lysogen formation, mitomycin C was treated to induce the prophages. Group L phages except for SPN9TCW did yield phage after mitomycin C induction, substantiating the lysogen formation by most of group L phage infection. However, most of group F phage-resistant strains did not yield phage by mitomycin C induction, even though these phages make turbid plaques, suggesting that these phages may make unstable lysogen, resulting in very low frequency of mitomycin C induction (approximately 5%) in the resistant strains. It has been known that Mu-like prophages were generally not induced by mitomycin C treatment [58], suggesting the possibility that group F phage may be mitomycin C-insensitive phage. To verify this, we performed PCR detection of group F phage genomes in the resistant hosts and the green plate experiment. Recently, we sequenced completely the genomes of four phages in group F and phage-specific primers were designed. Using these phage-specific primers, PCR was conducted to detect group F phage genomes in the genomes of group F phage-resistant S. Typhimurium LT2C strains. Interestingly, very low number of group F phage-resistant strains (approximately 5%) showed the presence of group F phage genomes in the host genomes, suggesting the formation of very unstable lysogens, supporting our observation of low mitomycin C induction with group F phage-resistant strains (data not shown). And green plate experiments also showed that most of group F phage infection does not make stable lysogens. We still do not understand this very distinct feature of group F phages for unstable lysogen formation and it needs to be elucidated soon.
Analysis of cross resistance among phage-resistant strains revealed that group F phage-resistant strains are sensitive to group L or B phages (Table 4 and Fig. 4A). This sensitivity indicates that the host resistance of group F phages does not disrupt the interactions between these other phages and the cell surface receptors. In contrast, group B phage-resistant strains are resistant to their phages as well as group L phages (Table 4 and Fig. 4C). The concurrent resistance to both group B and group L phages imply that BtuB may influence the interaction between LPS and phage, as in the case of E. coli phage T5 [45], [46]. The interaction between LPS and phage has been reported to accelerate adsorption of phage T5 to E. coli even though an outer membrane protein is the cell surface receptor.
All but one group L phage-resistant strain was sensitive to infection by group B phages (Table 4 and Fig. 4B). The group L SPN9TCW phage-resistant strain was resistant to group B phages (Table 4 and Fig. 4D), even though phage SPN9TCW uses LPS as a receptor and the resistant strain does not appear to be a lysogen. Therefore stable lysogen formation of group L phages may be a key to determine the host resistance against group B phages (Table 4). Further analyses of group B phage-resistant Salmonella strains are required to elucidate the mechanism of cross-resistance observed against the group B and L phages.
Many Salmonella-specific phages that use LPS as a receptor modify LPS as a mechanism to protect from superinfection when they lysogenize a host [59], [60]. The recent complete genome sequence analysis of a lysogenic SPN1S phage in group L revealed that the phage genome encodes a GtrA and two copies of lipopolysaccharide modification acyltransferase, supporting this [61]. Even though the LPS modification protects the lysogen from a superinfection by other group L phages, the lysogen is still sensitive to phages that target other receptors such as flagella and BtuB (Table 4 and Fig. 4B). Furthermore, group F, group B and group L SPN9TCW phage-resistant strains showed transient resistance to re-infection of the same phages (Table 4). These resistant strains were collected for the cross resistant experiment after the bacterial growth resumed in the presence of the phage. In this case, these collected phage-resistant strains are probably not lysogens, suggesting that host defense mechanisms such as CRISPR [62], [63] or restriction-modification systems [64], [65] or still unknown host defense mechanisms are probably activated during growth recovery.
Supporting Information
Green plate experiment of representative phages in three phage groups. (A) Group B SPN10H-resistant strain (B) Group L SPN9TCW-resistant strain (C) Group F SPN19-resistant strain. Red triangles indicate blue colonies on green plate.
(TIF)
Primers used in this study.
(DOC)
Funding Statement
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Ministry of Education, Science and Technology (No. 20090078983) and the Agriculture Research Center program of the Ministry for Food, Agriculture, Forestry and Fisheries, Republic of Korea. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. García P, Martínez B, Obeso JM, Rodríguez A (2008) Bacteriophages and their application in food safety. Lett Appl Microbiol 47: 479–485. [DOI] [PubMed] [Google Scholar]
- 2. O'Flaherty S, Ross RP, Coffey A (2009) Bacteriophage and their lysins for elimination of infectious bacteria. FEMS Microbiol Rev 33: 801–819. [DOI] [PubMed] [Google Scholar]
- 3.Cann AJ (1993) Principles of Molecular Virology. New York: Harcourt Brace and Co. Publ. 224 p.
- 4. Bruttin A, Brussow H (2005) Human volunteers receiving Escherichia coli phage T4 orally: a safety test of phage therapy. Antimicrob Agents Chemother 49: 2874–2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cairns BJ, Payne RJH (2008) Bacteriophage Therapy and the Mutant Selection Window. Antimicrob Agents Chemother 52: 4344–4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC (2007) Bacterial Foodborne and Diarrheal Disease National Case Surveillance, Annual Report 2005. US Department of Health and Human Services, CDC.
- 7.Mead PS, Slutsker L, Dietz V, McCaig LF, Bresee JS, et al.. (1999) Food-related illness and death in the United States. US Department of Health and Human Services, CDC. [DOI] [PMC free article] [PubMed]
- 8.CDC (2008) Salmonella Surveillance: Annual Summary, 2006. US Department of Health and Human Services, CDC.
- 9. McLaughlin MR, King RA (2008) Characterization of Salmonella bacteriophages isolated from swine lagoon effluent. Curr Microbiol 56: 208–213. [DOI] [PubMed] [Google Scholar]
- 10. Higgins JP, Andreatti Filho RL, Higgins SE, Wolfenden AD, Tellez G, et al. (2008) Evaluation of Salmonella-lytic properties of bacteriophages isolated from commercial broiler houses. Avian Dis 52: 139–142. [DOI] [PubMed] [Google Scholar]
- 11. McLaughlin MR, Balaa MF, Sims J, King R (2006) Isolation of Salmonella bacteriophages from swine effluent lagoons. J Environ Qual 35: 522–528. [DOI] [PubMed] [Google Scholar]
- 12. O'Flynn G, Coffey A, Fitzgerald GF, Ross RP (2006) The newly isolated lytic bacteriophages st104a and st104b are highly virulent against Salmonella enterica . J Appl Microbiol 101: 251–259. [DOI] [PubMed] [Google Scholar]
- 13. Kagawa H, Ono N, Enomoto M, Komeda Y (1984) Bacteriophage chi sensitivity and motility of Escherichia coli K-12 and Salmonella typhimurium Fla- mutants possessing the hook structure. J Bacteriol 157: 649–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Atterbury RJ, Van Bergen MAP, Ortiz F, Lovell MA, Harris JA, et al. (2007) Bacteriophage therapy to reduce Salmonella colonization of broiler chickens. Appl Environ Microbiol 73: 4543–4549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Andreatti Filho RL, Higgins JP, Higgins SE, Gaona G, Wolfenden AD, et al. (2007) Ability of bacteriophages isolated from different sources to reduce Salmonella enterica serovar Enteritidis in vitro and in vivo. Poult Sci 86: 1904–1909. [DOI] [PubMed] [Google Scholar]
- 16. Greer GG (2005) Bacteriophage control of foodborne bacteria. J Food Prot 68: 1102–1111. [DOI] [PubMed] [Google Scholar]
- 17. Carey-Smith GV, Billington C, Cornelius AJ, Hudson JA, Heinemann JA (2006) Isolation and characterization of bacteriophages infecting Salmonella spp. FEMS Microbiol Lett 258: 182–186. [DOI] [PubMed] [Google Scholar]
- 18. Ye J, Kostrzynska M, Dunfield K, Warriner K (2010) Control of Salmonella on sprouting mung bean and alfalfa seeds by using a biocontrol preparation based on antagonistic bacteria and lytic bacteriophages. J Food Prot 73: 9–17. [DOI] [PubMed] [Google Scholar]
- 19. Chan RK, Botstein D, Watanabe T, Ogata Y (1972) Specialized transduction of tetracycline resistance by phage P22 in Salmonella typhimurium : II. Properties of a high-frequency-transducing lysate. Virol 50: 883–898. [DOI] [PubMed] [Google Scholar]
- 20. Hudson JA, Billington C, Carey-Smith G, Greening G (2005) Bacteriophages as biocontrol agents in food. J Food Prot 68: 426–437. [DOI] [PubMed] [Google Scholar]
- 21. Zhang J, Kraft BL, Pan Y, Wall SK, Saez AC, et al. (2010) Development of an anti-Salmonella phage cocktail with increased host range. Foodborne Pathog Dis 7: 1415–1419. [DOI] [PubMed] [Google Scholar]
- 22. Mahichi F, Synnott AJ, Yamamichi K, Osada T, Tanji Y (2009) Site-specific recombination of T2 phage using IP008 long tail fiber genes provides a targeted method for expanding host range while retaining lytic activity. FEMS Microbiol Lett 295: 211–217. [DOI] [PubMed] [Google Scholar]
- 23. Casjens SR, Gilcrease EB, Winn-Stapley DA, Schicklmaier P, Schmieger H, et al. (2005) The generalized transducing Salmonella bacteriophage es18: complete genome sequence and dna packaging strategy. J Bacteriol 187: 1091–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ricci V, Piddock LJV (2010) Exploiting the role of TolC in pathogenicity: identification of a bacteriophage for eradication of Salmonella serovars from poultry. Appl Environ Microbiol 76: 1704–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hong J, Kim K-P, Heu S, Lee SJ, Adhya S, et al. (2008) Identification of host receptor and receptor-binding module of a newly sequenced T5-like phage EPS7. FEMS Microbiol Lett 289: 202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim M, Ryu S (2011) Characterization of a T5-like coliphage SPC35 and differential development of resistance to SPC35 in Salmonella Typhimurium and Escherichia coli . Appl Environ Microbiol 77: 2042–2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ho TD, Slauch JM (2001) OmpC is the receptor for Gifsy-1 and Gifsy-2 bacteriophages of Salmonella . J Bacteriol 183: 1495–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pickard D, Toribio AL, Petty NK, de Tonder A, Yu L, et al. (2010) A conserved acetyl esterase domain targets diverse bacteriophage to the Vi capsular receptor of Salmonella enterica serovar Typhi. J Bacteriol 192: 5746–5754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Salgado CJ, Zayas M, Villafane R (2004) Homology Between Two Different Salmonella phages: Salmonella enterica serovar Typhimurium phage P22 and Salmonella enterica serovar Anatum var. 15+ phage ε34. Virus Genes 29: 87–98. [DOI] [PubMed] [Google Scholar]
- 30. Erickson M, Newman D, Helm RA, Dino A, Calcutt M, et al. (2009) Competition among isolates of Salmonella enterica ssp. enterica serovar Typhimurium: role of prophage/phage in archived cultures. FEMS Microbiol Lett 294: 37–44. [DOI] [PubMed] [Google Scholar]
- 31. Datsenko KA, Wanner BL (2000) One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc Natl Acad Sci U S A 97: 6640–6645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cherepanov PP, Wackernagel W (1995) Gene disruption in Escherichia coli: TcR and KmR cassettes with the option of Flp-catalyzed excision of the antibiotic-resistance determinant. Gene 158: 9–14. [DOI] [PubMed] [Google Scholar]
- 33. Chang AC, Cohen SN (1978) Construction and characterization of amplifiable multicopy DNA cloning vehicles derived from the P15A cryptic miniplasmid. J Bacteriol 134: 1141–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Soncini FC, Vescovi EG, Groisman EA (1995) Transcriptional autoregulation of the Salmonella typhimurium phoPQ operon. J Bacteriol 177: 4364–4371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fauquet C (2005) Virus taxonomy : classification and nomenclature of viruses: 8th report of the International Committee on the Taxonomy of Viruses. San Diego: Elsevier Academic Press.
- 36. Hwang S, Kim M, Ryu S, Jeon B (2011) Regulation of oxidative stress response by CosR, an essential response regulator in Campylobacter jejuni . PLoS ONE 6: e22300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ogushi K-I, Wada A, Niidome T, Mori N, Oishi K, et al. (2001) Salmonella enteritidis FliC (flagella filament protein) induces human β-defensin-2 mRNA production by caco-2 cells. J Biol Chem 276: 30521–30526. [DOI] [PubMed] [Google Scholar]
- 38. Kutsukake K, Nakashima H, Tominaga A, Abo T (2006) Two DNA invertases contribute to flagellar phase variation in Salmonella enterica serovar Typhimurium strain LT2. J Bacteriol 188: 950–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Jiang SC, Kellogg CA, Paul JH (1998) Characterization of marine temperate phage-host systems isolated from Mamala bay, Oahu, Hawaii. Appl Environ Microbiol 64: 535–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ackermann HW, DuBow MS (1987) Viruses of prokaryotes, vol. 1. General properties of bacteriophages. CRC Press, Boca Raton, FL.
- 41. Hofer B, Ruge M, Dreiseikelmann B (1995) The superinfection exclusion gene (sieA) of bacteriophage P22: identification and overexpression of the gene and localization of the gene product. J Bacteriol 177: 3080–3086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Berngruber TW, Weissing FJ, Gandon S (2010) Inhibition of superinfection and the evolution of viral latency. J Virol 84: 10200–10208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Guo L, Lim KB, Gunn JS, Bainbridge B, Darveau RP, et al. (1997) Regulation of lipid a modifications by Salmonella typhimurium virulence genes phoP-phoQ. Science 276: 250–253. [DOI] [PubMed] [Google Scholar]
- 44. Ernst RK, Guina T, Miller SI (2001) Salmonella typhimurium outer membrane remodeling: role in resistance to host innate immunity. Microbes Infect 3: 1327–1334. [DOI] [PubMed] [Google Scholar]
- 45. Heller K, Braun V (1982) Polymannose O-antigens of Escherichia coli, the binding sites for the reversible adsorption of bacteriophage T5+ via the L-shaped tail fibers. J Virol 41: 222–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wang J, Jiang Y, Vincent M, Sun Y, Yu H, et al. (2005) Complete genome sequence of bacteriophage T5. Virology 332: 45–65. [DOI] [PubMed] [Google Scholar]
- 47. Samuel ADT, Pitta TP, Ryu WS, Danese PN, Leung ECW, et al. (1999) Flagellar determinants of bacterial sensitivity to x-phage. Proc Natl Acad Sci U S A 96: 9863–9866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Schade SZ, Adler J, Ris H (1967) How bacteriophage chi attacks motile bacteria. J Virol 1: 599–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chang JT, Schmid MF, Haase-Pettingell C, Weigele PR, King JA, et al. (2010) Visualizing the structural changes of bacteriophage epsilon15 and its Salmonella host during infection. J Mol Biol 402: 731–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Jiang W, Chang J, Jakana J, Weigele P, King J, et al. (2006) Structure of epsilon15 bacteriophage reveals genome organization and DNA packaging/injection apparatus. Nature 439: 612–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Israel V, Rosen H, Levine M (1972) Binding of bacteriophage P22 tail parts to cells. J Virol 10: 1152–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kruger DH, Schroeder C (1981) Bacteriophage T3 and bacteriophage T7 virus-host cell interactions. Microbiol Rev 45: 9–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Serwer P, Hayes SJ, Thomas JA, Demeler B, Hardies SC (2009) Isolation of novel large and aggregating bacteriophages. Methods Mol Biol 501: 55–66. [DOI] [PubMed] [Google Scholar]
- 54. Lee J-H, Shin H, Kim H, Ryu S (2011) Complete genome sequence of Salmonella bacteriophage SPN3US. J Virol 85: 13470–13471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Santos SB, Kropinski AM, Ceyssens P-J, Ackermann H-W, Villegas A, et al. (2011) Genomic and proteomic characterization of the broad-host-range Salmonella phage PVP-SE1: creation of a new phage genus. J Virol 85: 11265–11273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Park M, Lee J-H, Shin H, Kim M, Choi J, et al. (2012) Characterization and comparative genomic analysis of a novel bacteriophage, SFP10, simultaneously inhibiting both Salmonella enterica and Escherichia coli O157: H7. Appl Environ Microbiol 78: 58–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Anany H, Lingohr E, Villegas A, Ackermann H-W, She Y-M, et al. (2011) A Shigella boydii bacteriophage which resembles Salmonella phage ViI. Virol J 8: 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Paul JH (2008) Prophages in marine bacteria: dangerous molecular time bombs or the key to survival in the seas? ISME J 2: 579–589. [DOI] [PubMed] [Google Scholar]
- 59. Villafane R, Zayas M, Gilcrease E, Kropinski A, Casjens S (2008) Genomic analysis of bacteriophage ε34 of Salmonella enterica serovar Anatum (15+). BMC Microbiol 8: 227–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kropinski AM, Kovalyova IV, Billington SJ, Patrick AN, Butts BD, et al. (2007) The genome of ε15, a serotype-converting, Group E1 Salmonella enterica-specific bacteriophage. Virol 369: 234–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Shin H, Lee J-H, Lim JA, Kim H, Ryu S (2012) Complete genome sequence of Salmonella enterica serovar typhimurium bacteriophage SPN1S. J Virol 86: 1284–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Labrie SJ, Samson JE, Moineau S (2010) Bacteriophage resistance mechanisms. Nat Rev Micro 8: 317–327. [DOI] [PubMed] [Google Scholar]
- 63. Deveau H, Barrangou R, Garneau JE, Labonté J, Fremaux C, et al. (2008) Phage response to CRISPR-encoded resistance in Streptococcus thermophilus . J Bacteriol 190: 1390–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Wilson GG, Murray NE (1991) Restriction and modification systems. Annu Rev Genet 25: 585–627. [DOI] [PubMed] [Google Scholar]
- 65. Hill C, Pierce K, Klaenhammer TR (1989) The conjugative plasmid pTR2030 encodes two bacteriophage defense mechanisms in lactococci, restriction modification (R+/M+) and abortive infection (Hsp+). Appl Environ Microb 55: 2416–2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Zhang X, Kelly SM, Bollen WS, Curtiss R (1997) Characterization and immunogenicity of Salmonella typhimurium SL1344 and UK-1 Δcrp and Δcdt deletion mutants. Infect Immun 65: 5381–5387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. McClelland M, Sanderson KE, Spieth J, Clifton SW, Latreille P, et al. (2001) Complete genome sequence of Salmonella enterica serovar Typhimurium LT2. Nature 413: 852–856. [DOI] [PubMed] [Google Scholar]
- 68. Poppe C, Smart N, Khakhria R, Johnson W, Spika J, et al. (1998) Salmonella typhimurium DT104: a virulent and drug-resistant pathogen. Can Vet J 39: 559–565. [PMC free article] [PubMed] [Google Scholar]
- 69. Hayashi K, Morooka N, Yamamoto Y, Fujita K, Isono K, et al. (2006) Highly accurate genome sequences of Escherichia coli K-12 strains MG1655 and W3110. Mol Syst Biol 2: 2006.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Durfee T, Nelson R, Baldwin S, Plunkett G, Burland V, et al. (2008) The complete genome sequence of Escherichia coli DH10B: Insights into the biology of a laboratory workhorse. J Bacteriol 190: 2597–2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Green plate experiment of representative phages in three phage groups. (A) Group B SPN10H-resistant strain (B) Group L SPN9TCW-resistant strain (C) Group F SPN19-resistant strain. Red triangles indicate blue colonies on green plate.
(TIF)
Primers used in this study.
(DOC)