Abstract
Intracranial germ cell tumors (GCTs) are relatively rare. Their incidence has been considered to be higher in East Asia than in the United States. This study estimates the incidence of CNS GCTs in Japan and the United States, investigates gender discrepancies in each country, and describes treatment outcomes. Data on primary CNS GCTs from 4 databases were utilized: population-based malignant incidence data from (1) the Japan Cancer Surveillance Research Group (2004–2006; 14 registries), malignant and nonmalignant incidence data from (2) the Surveillance, Epidemiology, and End Results Program (2004–2008; 17 registries), and hospital-based observed survival data from (3) the Brain Tumor Registry of Japan (1984–2000) and (4) the US National Cancer Data Base (1990–2003). Incidence rates per 100 000 for malignant GCTs were not statistically significantly different between Japan (males = 0.143, females = 0.046) and the United States (males = 0.118, females = 0.030). The malignant incidence-rate ratio was higher for pineal GCTs versus nonpineal (ie, the rest of the brain) GCTs in Japan (11.5:1 vs 1.9:1, respectively) and the United States (16.0:1 vs 1.7:1, respectively). In general, 5-year survival estimates were high: over 75% for all GCTs, and over 81% for germinomas, regardless of the type of treatment in either Japan or the United States. The incidence of primary GCTs is similar between Japan and the United States and has the same gender-based patterns by location. High rates of survival were observed in both countries.
Keywords: brain tumor, epidemiology, germ cell tumors, germinoma, mixed germ cell tumors, pineal gland, teratoma, tumor registry
The CNS is the second most common site of extragonadal germ cell tumors (GCTs), following the mediastinum.1 CNS GCTs are still relatively rare, occurring at an incidence rate of 0.10 per 100 000 person-years in the the United States (males = 0.13, females = 0.06).2 In East Asia, including Japan and South Korea, where many surgical and treatment investigations have originated, the incidence is thought to be higher—yet epidemiology studies demonstrating increased incidence are limited.3–5 A recent investigation of a prefecture by the Brain Tumor Registry of Japan (BTRJ) representing <1.5% of the population estimated an incidence rate of 0.17/100 000/year (males = 0.3, females = 0.07) from 1989 to 2004; but from 2005 to 2008, the incidence rate was 0.10/100 000/year (males = 0.13, females = 0.08), which is similar to the rates seen in the United States.6
Members of our group have published on CNS GCTs in the United States. Unexpectedly, a 15-fold increased incidence of GCTs in males over females in the pineal gland area was demonstrated.1 This small area represents occurrence of nearly half of CNS GCTs. The rest of CNS GCTs, being mostly in suprasellar areas, have a near even gender incidence.7 The reason for this gender discrepancy based on loction is unknown.
The goal of this study is to identify whether similar gender discrepancies are present in the historically increased incidence of an East Asian population and then to describe clinical and treatment outcomes. To accomplish this goal, 4 independent datasets were analyzed. Incidence rates were estimated from 2 population-based datasets: the Japan Cancer Surveillance Research Group (JCSRG) and the US National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) Program. In addition, 2 hospital-based follow-up datasets were used to estimate survival: the BTRJ and the US National Cancer Data Base (NCDB). Large studies of GCTs have not been performed, and although this is an infrequent CNS cancer, there is an added impetus for our investigation: it is highly curable and affects a young population.
Methods
Data Estimated by the Japan Cancer Surveillance Research Group
As the JCSRG only collects data on malignant tumors, incidence rates were estimated for all primary malignant brain and CNS tumors diagnosed during 2004 through 2006 in 14 population-based registries in Japan (Aichi, Chiba, Fukui, Hiroshima, Kanagawa, Kumamoto, Miyagi, Nagasaki, Niigata, Okayama, Saga, Tochigi, Tottori, and Yamagata). All 14 registries met the domestic quality criteria of registry data, representing 31.8% of the total population. All primary malignant brain and CNS tumors were identified using the International Classification of Diseases for Oncology, third edition (ICD-O-3) and were grouped by primary site as
(i) Pineal: C75.3 (pineal gland), or
(ii) Nonpineal: C70.0–C72.9; C75.1–C75.2 (meninges, brain, spinal cord, cranial nerves, and other parts of the CNS, pituitary gland, craniopharyngeal duct).
GCTs were further selected by using ICD-O-3 histology codes 9060–9091 and 9100. The cases that were identified were also grouped into the histologic categories of germinoma (9060, 9061, 9064, 9065), teratoma (9080, 9082, 9084), and mixed GCT (9081, 9085).
Surveillance, Epidemiology, and End Results Research Data
The SEER database for 17 population-based cancer registries covers 26% of the US population and collects incidence and survival data on all primary malignant and nonmalignant brain and CNS tumors.8 SEER research data available in April 2011 were used to analyze information on all primary malignant and nonmalignant GCTs located in brain or CNS diagnosed and reported during 2004 through 2008.8 Incidence estimates were presented separately for malignant and nonmalignant tumors for comparison of only malignant tumors with the Japanese incidence data described above while including some incidence data on nonmalignant tumors as a parallel to the data from the 2 hospital-based follow-up registries to be described. All primary malignant and nonmalignant brain and CNS tumors were identified using the ICD-O-3 and were grouped as previously described.
Brain Tumor Registry of Japan Data
All primary malignant and nonmalignant GCTs diagnosed from 1984 through 2000 and reported to the BTRJ were included in the data analyses. The BTRJ obtained data from 263 institutions, consisting primarily of universities, colleges, and hospitals, with authorization from the Japan Neurological Society; the data represent ∼25% of all primary brain tumors in Japan (personal communication, S.S.). Tumors were identified using the ICD-O-3 and were grouped as previously described. Cases were selected for the study if the tumor behavior was identified as malignant, benign, or borderline and if the tumor was the only or first primary tumor identified in the patient's lifetime. Comparative descriptive analyses grouped primary site, patient sex, age, surgery, and first course treatment. Follow-up of cases was to be pursued every 5 years following the initial year of diagnosis (eg, for a case diagnosed in 1990, follow-up would be done in 1995, 2000, etc, until death or loss to follow-up); therefore, survival outcomes of treatment were limited to patients with at least 5 years of follow-up data.
National Cancer Data Base
The NCDB, a joint program of the American College of Surgeons (ACS) and the American Cancer Society, contains cancer patient demographics, tumor identification characteristics, stage, treatment, and outcomes data. It captures nearly 75% of all newly diagnosed cancer cases in 49 of the United States from over 1450 hospitals accredited by the ACS Commission on Cancer.
This descriptive study reviewed 1652 GCTs, including 1262 germinomas diagnosed between January 1, 1990 and December 31, 2008 reported to the NCDB. Tumors were identified using the ICD-O-3 and were grouped as previously described. Cases were selected for the study if the tumor behavior was identified as malignant, benign, or borderline and if the tumor was the only or first primary tumor identified in the patient's lifetime. Data were abstracted according to the Facility Oncology Registry Data Standards manual. Follow-up of cases was to be pursued every 5 years as previously described.
Data reported to the NCDB are retrospective in nature. No patient or physician identifiers were collected as part of the study. Case identification information (facility identification number and local registry accession number) was collected for administrative purposes only. Analyses were reported only at the aggregate level to assist hospital cancer programs with quality assurance, rather than to be used to make decisions about individuals and their care. The ACS has executed a business associate agreement on data use with each hospital approved by the Commission on Cancer. Results reported in this study were in compliance with the privacy requirements of the Health Insurance Portability and Accountability Act of 1996 as reported in the Standards for Privacy of Individually Identifiable Health Information, Final Rule (45 CFR [Code of Federal Regulations] Parts 160 and 164).
Statistical Analysis
Population-based incidence data were available from the JCSRG for Japan and from SEER for the United States. Frequency and incidence rates, age adjusted to the 2000 US standard population, were estimated per 100 000 population for the data from the JCSRG using SAS v9.2, and for the SEER research data using SEER*Stat 7.0.5.9 Hospital-based follow-up data were available for survival analysis from the BTRJ and NCDB, with comparative descriptive analyses grouped by primary site, patient sex, age, surgery, and first course treatment. All data analyses for the BTRJ were conducted using Stata*12, and for the NCDB using SAS v9.2 or SPSS v18.0. Survival curves were estimated using the observed life-table method.
Results
Frequencies and Incidence-Rate Estimates from the 2 Population-based Incidence Registries
Data from 2004 through 2006 from the JCSRG included 122 primary malignant GCTs of the brain and the CNS. Males (0.143/100 000; 95% confidence interval [CI] = 0.113–0.172) had a statistically significantly higher incidence of all malignant GCTs than females (0.046/100 000; 95% CI = 0.029–0.064), with an overall male-to-female incidence-rate ratio (IRR) of 3.1:1 (Table 1). However, when stratified by site, the male-to-female IRR for tumors of the pineal region was 11.5:1 compared with a corresponding IRR of 1.9:1 for tumors located in a nonpineal region (ie, other brain or CNS site; data not shown). Over 50% of tumors were reported in the young adult age group (Table 1). About 40% of GCTs were located in the pineal region, while the remainder were located in a nonpineal region. The majority (82%) of tumors were categorized as germinomas (Table 1).
Table 1.
Frequencies and incidence rates for all primary malignant brain and CNS germ cell tumors estimated by the Japan Cancer Surveillance Research Group (2004–2006; 14 registries) and Surveillance, Epidemiology, and End Results (2004–2008; 17 registries) data. Age-adjusted to the 2000 US Population
| Characteristics | JCSRG (malignant) |
SEER (malignant) |
||
|---|---|---|---|---|
| n (%) | Incidence (95% CI) | n (%) | Incidence (95% CI) | |
| All malignant GCTs | 122 (100.0) | 0.096 (0.079–0.114) | 289 (100.0) | 0.075 (0.067–0.084) |
| Male | 93 (76.2) | 0.143 (0.113–0.172) | 233 (80.6) | 0.118 (0.103–0.134) |
| Female | 29 (23.8) | 0.046 (0.029–0.064) | 56 (19.4) | 0.030 (0.023–0.039) |
| 00–14 ya | 43 (35.3) | 0.188 (0.132–0.244) | 119 (41.2) | 0.147 (0.122–0.176) |
| 15–29 ya | 65 (53.3) | 0.224 (0.169–0.278) | 141 (48.8) | 0.175 (0.147–0.207) |
| 30+ ya | 14 (11.5) | 0.013 (0.006–0.019) | 29 (10.0) | 0.014 (0.009–0.020) |
| Primary site | ||||
| Pineal (C75.3) | 49 (40.2) | 0.039 (0.028–0.049) | 134 (46.4) | 0.035 (0.029–0.041) |
| Nonpineal (C700–729, 751–752) | 73 (59.8) | 0.058 (0.044–0.071) | 155 (53.6) | 0.040 (0.034–0.047) |
| Suprasellar Regionb | 51 | 0.038 (0.027–0.049) | 88 | 0.023 (0.018–0.028) |
| Ventricle | – | – | 28 | 0.007 (0.005–0.010) |
| Brain, NOS | 36 | 0.027 (0.018–0.036) | 40 | 0.010 (0.007–0.014) |
| Pituitary gland | 13 | 0.010 (0.004–0.015) | 19 | 0.005 (0.003–0.008) |
| Cerebrum | 16 | 0.014 (0.007–0.021) | 29 | 0.007 (0.005–0.011) |
| All other sites | – | – | 38 | 0.010 (0.007–0.014) |
| Selected histologies | ||||
| Germinoma | 100 (82.0) | 0.078 (0.062–0.093) | 224 (77.5) | 0.058 (0.051–0.066) |
| Teratoma | 7 (5.7) | 0.006 (0.002–0.011) | 21 (7.3) | 0.005 (0.003–0.008) |
| Mixed GCT | 9 (7.4) | 0.007 (0.002–0.012) | 32 (11.1) | 0.008 (0.006–0.012) |
Dash indicates number too small to report. Abbreviation: NOS, not otherwise specified.
a Incidence rates are age specific, not standardized.
b Includes all tumors in site codes C71.5, 71.9, 72.9, and 75.1.
Using the SEER data for cases diagnosed from 2004 through 2008 from 17 registries, 289 primary malignant and 94 primary nonmalignant GCTs of the brain and CNS were reported. By behavior, the incidence rate for malignant GCTs in males (0.118/100 000 person-years; 95% CI = 0.103–0.134) was statistically significantly higher than for females (0.030/100 000 person-years; 95% CI = 0.023–0.039), with a male-to-female IRR of 3.9:1 (Table 1). The incidence of nonmalignant GCTs was not different between males and females (0.029 [95% CI = 0.021–0.037] and 0.020 [95% CI = 0.015–0.028]), respectively, with an IRR of 1.4:1 (data not shown). By site, the malignant male-to-female IRR for tumors of the pineal region was 16.0:1, as opposed to the male-to-female IRR for tumors located in a nonpineal region (ie, other brain or CNS site), which was only 2.1:1 (data not shown). The majority of malignant tumors in the SEER data were reported in the pediatric (41%) and young adult (49%) age groups (Table 1). Of malignant tumors, more than half (54%) were located in a nonpineal region, with the remainder located in the pineal region. Germinoma was the most frequently occurring (78%) malignant germ cell histology reported (Table 1). Teratoma was the only histology category where both malignant (18%) and nonmalignant tumors (82%) were reported (data not shown).
Frequencies from the 2 Hospital-based Follow-up Registries
Both the BTRJ and the NCDB are hospital-based registries, whose frequency results are presented in Table 2. Within the BTRJ, the frequencies of pineal (48%) and nonpineal (50%) GCTs were similar to each other. In the NCDB, the frequency of all GCTs located in the pineal gland was much higher than nonpineal GCTs (79% vs 21%). The frequencies of pineal GCTs in males were 11.7 and 14.4 times higher than the frequencies of pineal GCTs in females for the BTRJ and NCDB, respectively. For tumors of the nonpineal region, the frequencies of tumors were 1.8 and 1.1 times higher in males than females in the BTRJ and NCDB, respectively.
Table 2.
Description of first primary germinomas and all CNS germ cell tumors from the Brain Tumor Registry of Japan (1984–2000) and the National Cancer Data Base (1990–2008) by tumor location, extent of surgical resection, radiation treatment, and chemotherapy
| Total | Germinoma, n (%) |
All Germ Cell Tumors, n (%) |
||
|---|---|---|---|---|
| BTRJ | NCDB | BTRJ | NCDB | |
| 1258 (100) | 1262 (100) | 1815 (100) | 1652 (100) | |
| Tumor locationa | ||||
| Pineal gland | 585 (46.5) | 1034 (81.9) | 871 (48.0) | 1300 (78.7) |
| Male | 542/585 (92.6) | 971 (93.9) | 802/871 (92.1) | 1216 (93.5) |
| Female | 43/585 (7.4) | 63 (6.1) | 69/871 (7.9) | 84 (6.5) |
| Nonpineal gland | 645 (51.3) | 228 (18.1) | 910 (50.1) | 352 (21.3) |
| Male | 429/645 (66.5) | 129 (56.6) | 589/910 (64.7) | 188 (53.4) |
| Female | 216/645 (33.5) | 99 (43.4) | 321/910 (35.3) | 164 (46.6) |
| Age at diagnosisa | ||||
| 0–9 y | 105 (8.3) | 95 (7.5) | 245 (13.5) | 186 (11.3) |
| 10–14 y | 357 (28.4) | 321 (25.4) | 509 (28.0) | 433 (26.2) |
| 15–19 y | 339 (26.9) | 360 (28.5) | 460 (25.3) | 431 (26.1) |
| 20–24 y | 220 (17.5) | 240 (19.0) | 284 (15.6) | 273 (16.5) |
| 25+ y | 225 (17.9) | 246 (19.5) | 300 (16.5) | 329 (19.9) |
| Surgical procedurea | ||||
| None | 400 (31.8) | 704 (55.8) | 491 (27.1) | 792 (47.9) |
| Biopsy, local, or partial removal | 795 (63.2) | 331 (26.2) | 1133 (62.4) | 500 (30.3) |
| Total surgical removal | 47 (3.7) | 148 (11.7) | 169 (9.3) | 256 (15.5) |
| Radiation treatmenta | ||||
| No | 133 (10.6) | 235 (18.6) | 332 (18.3) | 399 (24.2) |
| Yes | 1113 (88.5) | 937 (74.3) | 1470 (81.0) | 1116 (67.6) |
| Mode for first coursea | ||||
| Linac | 849/1113 (76.3) | NA | 1123/1470 (76.4) | NA |
| Co60 | 216/1113 (19.4) | NA | 282/1470 (19.2) | NA |
| Other | 17/1113 (1.5) | NA | 23/1470 (1.6) | NA |
| Chemotherapya | ||||
| No | 717 (57.0) | 642 (50.9) | 913 (50.3) | 801 (48.5) |
| Yes | 519 (41.3) | 577 (45.7) | 872 (48.0) | 795 (48.1) |
| Agent for first coursea | ||||
| Cisplatin | 253/519 (48.7) | NA | 456/872 (52.3) | NA |
| VP-16 | 103/519 (19.8) | NA | 149/872 (17.1) | NA |
| Other | 149/519 (28.7) | NA | 246/872 (28.2) | NA |
Abbreviation: NA, data not available.
a Counts may not add to total number due to subgroup category unknown or not presented here.
In the NCDB, almost half (48%) of all GCTs and 56% of germinomas were recorded as having no surgical treatment as the first course of therapy. Conversely, 68% of all GCTs and 74% of germinomas received radiation treatment as a first course of therapy. Chemotherapy was used in the first course of treatment in 46% of germinomas and 48% of all GCTs. In the BTRJ, 62% of all GCTs and 63% of germinomas received surgical treatment consisting of biopsy, local or partial removal, while less than one-third of tumors were not treated with a surgical procedure for the first course of treatment. Radiation treatment was performed more frequently in the BTRJ (81% for all GCTs and 89% for germinomas) than in the NCDB. However, chemotherapy was utilized in the first course of treatment (48% for all GCTs and 41% for germinomas) at a frequency similar to the NCDB.
Survival Estimates from 2 Hospital-based Follow-up Registries
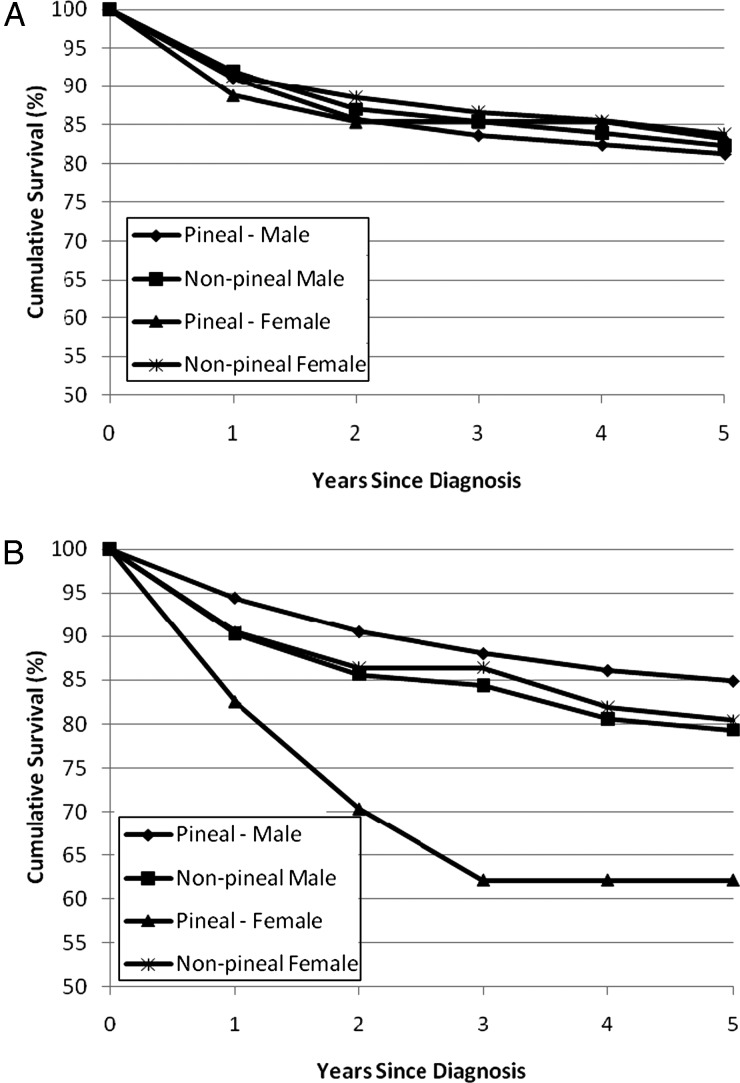
No statistically significant differences in survival were observed in the BTRJ between males and females for tumors located in the pineal or nonpineal regions (Fig. 1A; 5-year cumulative survival estimates for males = pineal: 81.3%, nonpineal: 82.3%; females = pineal: 83.2%, nonpineal: 83.8%). Using data from the NCDB, females with a pineal GCT (62.1%; 95% CI = 48.6–75.6) had statistically significantly worse 5-year observed survival than males with a pineal GCT (84.9%; 95% CI = 82.3–87.5); no other differences in 5-year observed survival were seen (Fig. 1B; 5-year cumulative survival estimates: male = nonpineal: 79.3%; females = nonpineal: 80.4%). In general, 5-year survival estimates were high for all germ cell tumors: over 75% in both datasets (NCDB and BTRJ), regardless of radiation therapy, chemotherapy, or surgery status (Table 3). Similarly, cumulative survival estimates for germinomas were over 81% at 5 years in both datasets regardless of the type of treatment received.
Fig. 1.
Five-year cumulative survival for all CNS germ cell tumors by primary site and gender. Data from (A) the Brain Tumor Registry of Japan (1984–2000) and (B) the National Cancer Data Base (1990–2003).
Table 3.
Five-year cumulative survival for all CNS germ cell tumors and germinomas by radiation therapy status, chemotherapy status, and surgery status; data from the National Cancer Data Base (1990–2003) and the Brain Tumor Registry of Japan (1984–2000)
| National Cancer DataBase (NCDB) |
Brain Tumor Registry of Japan (BTRJ) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1-y | 2-y | 3-y | 4-y | 5-y | 1-y | 2-y | 3-y | 4-y | 5-y | |
| All GCTs | ||||||||||
| Radiation therapy status | ||||||||||
| Yes | 95.2 | 90.6 | 88.3 | 85.8 | 84.4 | 93.0 | 88.2 | 86.5 | 85.3 | 83.9 |
| No | 89.9 | 86.0 | 83.5 | 81.0 | 79.3 | 84.4 | 80.7 | 78.7 | 77.8 | 75.3 |
| Chemotherapy status | ||||||||||
| Yes | 93.5 | 87.3 | 84.6 | 82.0 | 80.5 | 88.0 | 81.0 | 78.7 | 77.3 | 75.2 |
| No | 93.1 | 90.2 | 87.7 | 86.3 | 85.3 | 94.9 | 92.6 | 91.3 | 90.4 | 89.5 |
| Surgery status | ||||||||||
| Total | 87.0 | 83.2 | 82.4 | 78.4 | 77.6 | 90.0 | 87.3 | 85.9 | 83.6 | 82.0 |
| Partial | 94.4 | 90.5 | 87.6 | 84.5 | 83.0 | 91.0 | 86.0 | 83.8 | 82.8 | 81.0 |
| None | 93.7 | 88.9 | 85.9 | 85.0 | 84.0 | 93.9 | 90.0 | 88.9 | 88.0 | 86.7 |
| Germinoma only | ||||||||||
| Radiation therapy status | ||||||||||
| Yes | 97.0 | 94.3 | 92.2 | 89.7 | 88.4 | 96.9 | 93.9 | 93.1 | 91.9 | 91.0 |
| No | 93.4 | 91.4 | 90.0 | 87.1 | 85.6 | 87.7 | 85.8 | 84.8 | 83.7 | 81.2 |
| Chemotherapy status | ||||||||||
| Yes | 96.2 | 93.0 | 90.8 | 88.1 | 86.7 | 96.2 | 91.8 | 90.6 | 88.7 | 87.0 |
| No | 95.1 | 93.1 | 91.0 | 89.7 | 88.8 | 95.7 | 94.0 | 93.5 | 92.9 | 92.5 |
| Surgery status | ||||||||||
| Total | 91.8 | 90.8 | 90.8 | 85.1 | 83.9 | 93.3 | 93.3 | 93.3 | 90.5 | 90.5 |
| Partial | 96.5 | 94.8 | 92.1 | 89.2 | 88.6 | 96.1 | 93.3 | 92.1 | 91.1 | 90.0 |
| None | 95.9 | 92.7 | 90.2 | 89.1 | 88.0 | 96.2 | 93.1 | 92.8 | 91.6 | 90.4 |
Discussion
Descriptions of incidence, outcomes, and treatment of care are important for a highly curable disease, especially one affecting primarily pediatric and young adult populations. International comparisons, although inherently complicated, can provide insightful direction in the management of such conditions. Our study is the largest international comparison to date on primary CNS GCTs, and our findings are noteworthy.
The observed incidence data for Japan and the United States were not statistically different in this study. This was largely unexpected, as previous literature demonstrated an increased incidence in East Asia, including Japan and South Korea.3–5 We also demonstrated that the differences in anatomic site and incidence of primary CNS GCTs by gender found in the United States paralleled those observed in the Japanese population. This likely reflects inherent biological differences based on gender. Finally, and importantly, clinical variables such as treatment and outcomes were similar in both countries.
Our study verifies the findings of a recent but small registry study in Japan.6 In the Japanese registry study, the incidence of CNS GCTs decreased over time, but only from males, as the incidence in females remained the same. In the United States, an overlapping time period shows incidence rates for malignant GCTs increased slightly, but not statistically significantly, for tumors diagnosed from 2000 through 2008 (annual percent change = 1.11; 95%CI =−3.18 to 5.59).10,11 These rates indicate that CNS GCTs are an uncommon tumor. It would be of interest to know if other parts of East Asia have a similar incidence rate as Japan.
Our previous finding of differences in anatomic site and incidence of primary CNS GCTs based by gender was unexpected in the United States.1,12 Finding the same results in Japan affirms the gender-based biology of this disease. To highlight, the difference in incidence of GCTs in the pineal region is the largest gender difference for any cancer besides gender-based endocrine organs. The biological basis is unknown, but the findings are remarkable.
Although treatment and outcomes were largely similar, there were exceptions. There were higher rates of surgical procedures in Japan compared with the United States. Neurosurgical procedures in the pineal and suprasellar areas are challenging, as these areas are near the center of the brain.13 In clinical studies, radiation therapy is the standard of care for CNS germinomas, with demonstration of 5-year survival of over 90%.12 Although there are positive results from studies involving sequential chemotherapy and radiation therapy,10,11,14,15 no randomized trial has yet compared the combined modality treatment with radiotherapy alone. However, results from the Societé Internationale de Oncologie Pédiatrique CNS GCT 96 protocol are expected to be reported soon, which will allow physicians to choose either combined sequential therapy or radiation therapy alone.16
Another notable difference between the US and Japanese data includes lower survival in pineal region GCTs in females in the United States. These differences in survival rates are likely attributable to the limited number of cases and possibly differences in surgical practice or, less likely, inherent racial differences. Ethnic variability affecting disease biology has been demonstrated between the United States and Japan, including the location, treatment, and outcome of gastric cancer17–19 and incidence of epidermal growth factor receptor mutant allele lung cancer.20,21
An important similarity between the US and Japanese data is the predominance of germinoma histology and overall high rates of survival. Outcomes, with the exception previously discussed on lower survival of pineal region germ cell cancers in females in the United States, based on location in the brain and gender did not influence survival.
Limitations of our study were expected concerns for database analysis, including the complexity of analyzing from 2 different countries and 4 distinct databases that are not directly comparable. The structure and quality of these databases are certainly different, which needs to be taken into consideration when evaluating our results. Also, as there were 4 independent analyses done (one for each database), there were differences in the analyses performed. For comparison purposes, we analyzed and presented the incidence of GCTs in the SEER data by gender for both malignant and nonmalignant GCTs separately. The data from the NCDB and BTRJ were hospital or clinic-based and were therefore not representative of the entire population. Although this database analysis is based on large amounts of data and a large number of cases, generalizations on the success of individual treatments should be cautioned against, especially given that this is not a clinical trial. Survival rates were presented as observed survival as opposed to relative survival, which can adjust for survival in the general population by age and gender. In addition, other clinical variables that may influence survival (ie, those not presented here) were not available for inclusion in the analysis and may have influenced the results.
In conclusion, we found that the incidence of primary GCTs is similar between Japan and the United States and that there is the same high incidence of GCTs predominantly in males in the pineal region, with more balanced gender incidence in the remaining brain locations. Finally, outcomes are similar in the United States and Japan for this uncommon but curable primary CNS tumor.
Conflict of interest statement. None declared.
Funding
This work was supported by the Central Brain Tumor Registry of the United States (CBTRUS), which is supported by the American Brain Tumor Association, the National Brain Tumor Society, the Pediatric Brain Tumor Foundation, the Division of Cancer Control and Population Sciences, National Cancer Institute, National Institutes of Health, Department of Health and Human Services (HHSN261201000576P), and Centers for Disease Control and Prevention (Cooperative Agreement 1U58DP003831) to T. D. and B. M. The Valerie Landis Fund of the University of Illinois, Chicago also provided support. Contents of this work are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
References
- 1.Villano JL, Propp JM, Porter KR, et al. Malignant pineal germ-cell tumors: an analysis of cases from three tumor registries. Neuro Oncol. 2008;10:121–30. doi: 10.1215/15228517-2007-054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Published by the Central Brain Tumor Registry of the United States; 2011. CBTRUS: Statistical report: Primary brain tumors in the United States, 2004–2007. [Google Scholar]
- 3.Kuratsu J, Ushio Y. Epidemiological study of primary intracranial tumors: a regional survey in Kumamoto Prefecture in the southern part of Japan. J Neurosurg. 1996;84:946–50. doi: 10.3171/jns.1996.84.6.0946. [DOI] [PubMed] [Google Scholar]
- 4.Kuratsu J, Takeshima H, Ushio Y. Trends in the incidence of primary intracranial tumors in Kumamoto, Japan. Int J Clin Oncol. 2001;6:183–91. doi: 10.1007/pl00023928. [DOI] [PubMed] [Google Scholar]
- 5.Jennings MT, Gelman R, Hochberg F. Intracranial germ-cell tumors: natural history and pathogenesis. J Neurosurg. 1985;63:155–67. doi: 10.3171/jns.1985.63.2.0155. [DOI] [PubMed] [Google Scholar]
- 6.Nakamura H, Makino K, Yano S, et al. Epidemiological study of primary intracranial tumors: a regional survey in Kumamoto prefecture in southern Japan–20-year study. Int J Clin Oncol. 16:314–21. doi: 10.1007/s10147-010-0178-y. [DOI] [PubMed] [Google Scholar]
- 7.Villano JL, Virk IY, Ramirez V, et al. Descriptive epidemiology of central nervous system germ cell tumors: nonpineal analysis. Neuro Oncol. 0000;12:257–64. doi: 10.1093/neuonc/nop029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Surveillance E, and End Results (SEER) Program. SEER*Stat Database: Incidence - SEER 13 Regs Limited-Use, Nov 2007 Sub (1992–2005)<Katrina/Rita Population Adjustment> - Linked To County Attributes - Total United States., 1969–2005 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2008, based on the November 2007 submission. 2008 http://seer.cancer.gov . [Google Scholar]
- 9.Surveillance Research Program. National Cancer Institute SEER*Stat software (seer.cancer.gov/seerstat) version 7.0.5 (ed version 6.4.4.), National Cancer Institute. 2011.
- 10.Buckner JC, Peethambaram PP, Smithson WA, et al. Phase II trial of primary chemotherapy followed by reduced-dose radiation for CNS germ cell tumors. J Clin Oncol. 1999;17:933–40. doi: 10.1200/JCO.1999.17.3.933. [DOI] [PubMed] [Google Scholar]
- 11.Matsutani M. Combined chemotherapy and radiation therapy for CNS germ cell tumors—the Japanese experience. J Neurooncol. 2001;54:311–6. doi: 10.1023/a:1012743707883. [DOI] [PubMed] [Google Scholar]
- 12.Bamberg M, Kortmann RD, Calaminus G, et al. Radiation therapy for intracranial germinoma: results of the German cooperative prospective trials MAKEI 83/86/89. J Clin Oncol. 1999;17:2585–92. doi: 10.1200/JCO.1999.17.8.2585. [DOI] [PubMed] [Google Scholar]
- 13.Bruce JN, Ogden AT. Surgical strategies for treating patients with pineal region tumors. J Neurooncol. 2004;69:221–36. doi: 10.1023/b:neon.0000041885.09226.2d. [DOI] [PubMed] [Google Scholar]
- 14.Bouffet E, Baranzelli MC, Patte C, et al. Combined treatment modality for intracranial germinomas: results of a multicentre SFOP experience. Societe Francaise d'Oncologie Pediatrique. Br J Cancer. 1999;79:1199–204. doi: 10.1038/sj.bjc.6690192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aoyama H, Shirato H, Ikeda J, et al. Induction chemotherapy followed by low-dose involved-field radiotherapy for intracranial germ cell tumors. J Clin Oncol. 2002;20:857–65. doi: 10.1200/JCO.2002.20.3.857. [DOI] [PubMed] [Google Scholar]
- 16.National Cancer Institute. Combination Chemotherapy and Radiation Therapy in Treating Patients With Germ Cell Tumors in the Brain. ClinicalTrials.gov Bethesda, MD: National Library of Medicine (US) http://clinicaltrials.gov/ct2/show/NCT00293358. NLM Identifier: NCT00293358, 2009. [Google Scholar]
- 17.Isobe Y, Nashimoto A, Akazawa K, et al. Gastric cancer treatment in Japan: 2008 annual report of the JGCA nationwide registry. Gastric Cancer. 14:301–16. doi: 10.1007/s10120-011-0085-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sasako M, Sakuramoto S, Katai H, et al. Five-year outcomes of a randomized phase III trial Comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 29:4387–93. doi: 10.1200/JCO.2011.36.5908. [DOI] [PubMed] [Google Scholar]
- 19.Ohtsu A, Shah MA, Van Cutsem E, et al. Bevacizumab in combination with chemotherapy as first-line therapy in advanced gastric cancer: a randomized, double-blind, placebo-controlled phase III study. J Clin Oncol. 2011;29:3968–76. doi: 10.1200/JCO.2011.36.2236. [DOI] [PubMed] [Google Scholar]
- 20.Mitsudomi T, Yatabe Y. Mutations of the epidermal growth factor receptor gene and related genes as determinants of epidermal growth factor receptor tyrosine kinase inhibitors sensitivity in lung cancer. Cancer Sci. 2007;98:1817–24. doi: 10.1111/j.1349-7006.2007.00607.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sone T, Kasahara K, Kimura H, et al. Comparative analysis of epidermal growth factor receptor mutations and gene amplification as predictors of gefitinib efficacy in Japanese patients with nonsmall cell lung cancer. Cancer. 2007;109:1836–44. doi: 10.1002/cncr.22593. [DOI] [PubMed] [Google Scholar]