Abstract
Background
Depression and frailty both predict disability and morbidity in later life. However, it is unclear to what extent these common geriatric syndromes represent overlapping constructs.
Objective
To examine the joint relationship between the constructs of depression and frailty.
Methods
Data come from 2004/5 wave of the Baltimore Epidemiologic Catchment Area Study and analysis is limited to participants aged 40 and older with complete data on frailty and depression indicators (N = 683). Depression was measured using the Diagnostic Interview Schedule and frailty was indexed by modified Fried criteria. A series of confirmatory latent class analyses (LCA) were used to assess the degree to which depression and frailty syndromes identify the same populations. A latent Kappa coefficient (Кl) was also estimated between the constructs.
Results
Confirmatory LCA indicated that depression and frailty represent distinct syndromes rather than a single construct. The joint modeling of the two constructs supported a three class solution for depression and two class solution for frailty, with 2.9% categorized as severe depression, 19.4% as mild depression, and 77.7% as not depressed, and 21.1% categorized as frail and 78.9% as not frail. The chance-corrected agreement statistic indicated moderate correspondence between the depression and frailty constructs (Кl: 66, 95% CI: 0.58 – 0.74).
Conclusions
Results suggest that depression and frailty are interrelated concepts, yet their operational criteria identify substantively overlapping subpopulations. These findings have implications for understanding factors that contribute to the etiology and prognosis of depression and frailty in later life.
Keywords: depression, frailty, latent class analysis, aging
OBJECTIVES
Frailty is a syndrome in older adults characterized by vulnerability to physical and mental decline and is associated with risk of disability and mortality (1). Various operational and conceptual definitions of frailty have been proposed, and the three most prominent models focus on functional capacities, cumulative medical burden, and biological decline (2–4). In particular, depression shares many of the symptoms, risk factors, and predicts the same types of outcomes as frailty. The diagnosis of depression in mid- and late-life is often confounded by the presence of medical comorbidity and increased endorsement of medically-unexplained somatic symptoms (5), making it difficult for physicians to recognize depression or to differentiate its symptoms from physical illness (6). Depression in later life has been labeled “depression without sadness” (6) because empirical evidence suggests this syndrome is characterized by a relative lack of mood symptoms despite a high burden of cognitive and neurovegetative symptoms (6). Depression and frailty may therefore be related through a fundamental similarity and overlap of construct definition. Katz recently noted that “Depending on the definitions [of frailty] used, it is possible to make a case for each of these conditions [depression and frailty] as a cause, consequence, or comorbidity of the other. It is also possible to argue for their congruence” (7).
One current operational definition proposed by Fried and colleagues in the Cardiovascular Health Study (CHS) identifies frailty in terms of five dimensions: weight loss, exhaustion, low energy expenditure, slowness, and weakness (2). This definition has been cross-validated in other populations, and is consistent with the notion that frailty is a medical syndrome (2, 8, 9). This construction of frailty has several commonalities with symptoms of depression (e.g., psychomotor slowness, fatigue and weight change). As a clearly-defined and validated approach for identifying frailty, the CHS definition provides a useful measure with which to test assumptions regarding whether frailty and depression are distinct syndromes.
Tinetti and colleagues have explicitly called for a unified approach to conceptualizing syndromes in later life in acknowledgement of this difficulty (10); however few studies have explicitly adopted this approach to understanding health in later life. A notable exception is a recent study by Hajjar and colleagues (2009) in which they identified a novel clustering of slowness, executive function impairment, and depressive symptoms (11). They argue that this clustering of symptoms is indicative of subcortical changes in the brain, consistent with the notion of a common biology underlying this single syndrome.
The goal of this study is to evaluate the relationship and agreement between depression and frailty syndromes. Confirmatory latent class analysis (LCA) was used to examine the joint distributions of depression and frailty to assess the amount of agreement between the two constructs. If the latent constructs of depression and frailty can be described by a single latent construct, this supports Katz’s notion of the confluence of depression and frailty in mid- and late-life. Conversely, if the latent constructs of depression and frailty identify completely distinct populations, this suggests that epidemiologic studies treating them as independent ‘causes or consequences’ of the other are warranted. Finally, if the constructs of depression and frailty are distinct, but identify highly overlapping subpopulations, this indicates that the most appropriate model for understanding depression and frailty is one of comorbidity.
METHODS
Sample
Data come from the Baltimore Epidemiologic Catchment Area (ECA) Study, a longitudinal population-based survey of adults begun in 1981 as part of a multi-site study investigating prevalence of mental illness in the United States. Details concerning data collection procedures have been described previously (12, 13). The Baltimore ECA cohort was re-interviewed in 1982, 1993/6 and 2004/5. This analysis is limited to data collected during the fourth follow-up in 2004/5, in which interviews were conducted with 1,071 surviving participants over the age of 40 (age range: 41–96 years). Only the 2004/5 interview was used because the measures of frailty were not available in earlier waves. Of this sample, 683 participants had complete data concerning indicators of both depression and frailty and were included in the current analysis. Mid-life is an appropriate point in the life course for examining the relationship between depression and frailty because both are associated with increased mortality, and thus examinations of these relationships among older adults may be influenced by survivor bias (14). Recent studies have also suggested that indicators of frailty can occur as early as the third decade of life (15), however because frailty is more common in later life, a sensitivity analysis was conducted restricting the sample to those aged 55 and older (n=330).
The Baltimore ECA was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board and all participants provided informed consent. This study received an exempt status from Institutional Review Board at Virginia Commonwealth University.
MEASURES
Depression
Depressive symptoms were ascertained using the Diagnostic Interview Schedule (DIS; (16)), a fully-structured interview that reflects the criteria for major depression (MD) as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R; (17)). The DIS includes questions regarding the presence, onset, and recency of symptoms and other information relevant to the causal attribution and co-occurrence of symptoms. The DIS MD inventory consists of 26 individual symptom items which are organized into nine symptom groups: 1) dysphoria, 2) weight and appetite changes, 3) sleep disturbances, 4) fatigue, 5) psychomotor retardation or agitation 6) anhedonia, 7) feelings of guilt or worthlessness, 8) trouble concentrating or slowed thought, and 9) thoughts of death or suicide. All items were asked of all participants regardless of whether they endorsed the cardinal symptoms of dysphoria or anhedonia (that is, there are no screening items).
For the current study depression was modeled based on the occurrence of these nine symptom groups within the 6 months prior to interview to ensure that the symptoms clustered together in the same time period. Each individual symptom was coded dichotomously (present in past 6 months/not present), and these symptoms were then collapsed into the 9 symptom groups for analysis (Supplemental Table 1).
Frailty
Indicators of frailty were based on the CHS criteria, which include weight loss/low weight, exhaustion, slowness, weakness, and low energy expenditure (2); however the specific operationalization was adapted to the available data. Weight loss/low weight was indexed as the lowest 10% of BMI (<21.95 kg/m2). This cutoff was used because too few participants (N = 19, 1.8%) met the CHS criterion of BMI <18.5 kg/m2. A sensitivity analysis was conducted to determine if this decision influenced model fit. Exhaustion was indicated by endorsement of “feeling tired out all the time” and “not feeling full of energy,” from the DIS and General Health Questionnaire (GHQ), respectively. As a post-hoc sensitivity analysis we re-fit the frailty model using only the GHQ item to indicate fatigue. Low energy expenditure was defined as being concurrently in the lowest quartile of daily walking activity and not exercising at least once per week, both indicated by self-report. Slowness was defined as being either unable to complete a short (3 or 4 meters, depending on the space available to make the course) walking course, or among those who completed the course, having a walking speed in the highest quartile (>0.58 m/s) (2). CHS criteria define weakness as having poor grip strength (2), however because no equivalent measure of grip strength was available in the ECA, strength was instead based on ability to complete a series of timed chair-stands. Weakness was defined as being either unable to complete the five chair stands or being in the bottom 10% of completion speed (>17.6 seconds). All five frailty symptoms were coded as dichotomous (present/absent) indicator variables (Supplemental Table 1).
ANALYSIS
Initially, the bivariate relationship between MD status and demographic characteristics, frailty indicators, self-rated health, mini-mental status exam (MMSE) score, and disability status was examined using Fisher’s exact tests for categorical variables and t-tests for continuous variables.
Confirmatory latent class analysis (LCA) was used to determine the construct overlap between depression and frailty (18). In LCA, iterative maximum-likelihood estimation is used to fit a latent variable model in order to explain the association between a set of observed variables given membership in a discrete latent subpopulation (called classes). The goal of LCA is to identify distinct groups of people which share similar symptom endorsement profiles. Two sets of parameters from the latent class models were compared: i) the predicted probability of each class, and ii) the conditional probabilities of symptom endorsement given class membership. The predicted probability of each class represents the prevalence of each class in the population (19). Conditional on class membership, the predicted probability that any particular depressive symptom is endorsed describes the features of that class (e.g., a severely depressed class is likely characterized by very high predicted probabilities of endorsement of all depressive symptoms). These conditional probabilities of symptom endorsement are akin to factor loadings (19). This information was used to assess whether the best fitting models were consistent with previous research in terms of class prevalence and symptom endorsement patterns.
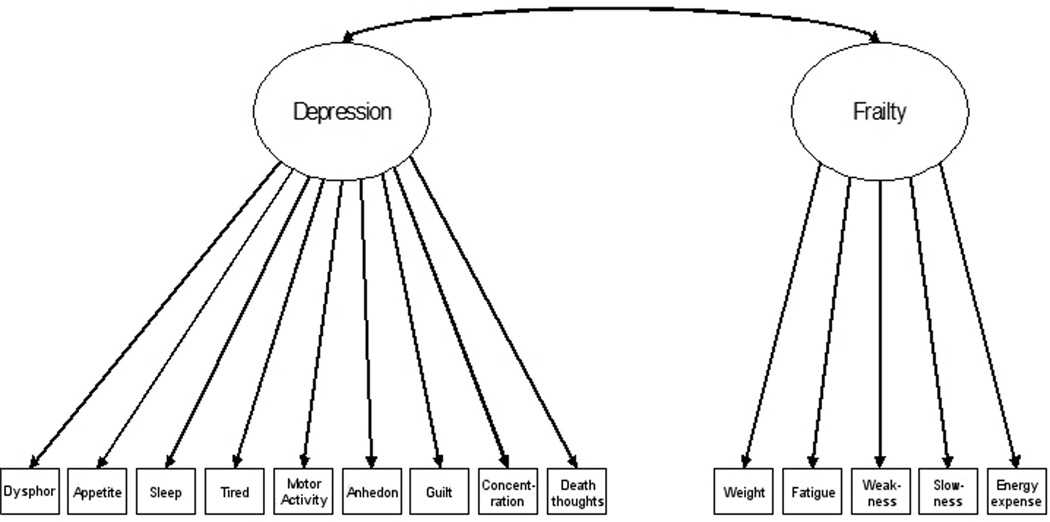
Two broad types of latent class models were fit: 1) a single discrete latent variable indicated by all 14 observed variables (9 from depression and 5 from frailty); and 2) separate but overlapping discrete latent variables representing depression and frailty, each defined by their respective indicator variables (Figure 1). The comparison of these two broad types of models indicates the degree to which the set of observed variables support a separation of frailty and depression as distinct latent constructs, as opposed to a single construct (i.e., lack of trait discrimination between depression and frailty). Using latent class analysis, four successive models were specified a priori, each extracting different numbers of latent classes for the frailty and depression constructs. These successive models were compared to determine the most appropriate number of latent classes for the depression and frailty constructs. The explanatory strengths of models assuming different numbers of latent classes were compared using goodness-of-fit statistics including Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and sample-size adjusted Bayesian Information Criterion (BICN); for each of these criteria, smaller values are indicative of better model fit. In addition to these statistical tests, whether additional classes were interpretable and clinically meaningful was used to determine the best fitting model.
Figure 1.
Conceptual model of depression and frailty agreement
Illustration of Table 2, Models 2 – 5. Observed indicators are binary (present/absent) variables.
Using the estimated class proportions, the latent Kappa coefficient (Кl; 20) was used to estimate the chance-corrected agreement between the two discrete constructs from the joint distributions of the overlapping latent classes (e.g. combinations of depression and frailty classes: depressed/frail, not depressed/frail, depressed/not frail, and not depressed/not frail) (Appendix A). While the conventional Kappa coefficient is usually used to represent the chance-corrected agreement between the two raters of a single observed variable (21), here it is used as a measure of the agreement between the two discrete latent variables representing depression and frailty (20). The Кl indicates to what degree those who were classified as depressed would also be classified as frail, and the degree to which those who were classified as not depressed would be classified as not frail when the number of depression and frailty classes are equal (e.g., three-class solution for both constructs, see Appendix B).
Analyses were conducted using STATA v.11 and MPlus statistical modeling software (22, 23).
RESULTS
Table 1 shows the demographic characteristics of the sample stratified by lifetime MD status. Consistent with previous research, individuals who met criteria for MD were younger and more likely to be female. The symptoms of frailty were fairly common (prevalence 8.5 to 27%), and with the exception of exhaustion, MD was not significantly associated with indicators of frailty.
Table 1.
Participant characteristics by lifetime history of major depression
| Overall (N = 683) |
Lifetime MD (N = 88) |
Never MD (N = 595) |
p-Value | |
|---|---|---|---|---|
| % or Mean (SD) | ||||
| Demographics | ||||
| Female | 62.52 | 77.27 | 60.34 | 0.002 |
| Race | 0.134 | |||
| White | 62.08 | 70.45 | 60.84 | |
| Black | 34.26 | 25.00 | 35.63 | |
| Other | 3.66 | 4.55 | 3.53 | |
| Age (years) | 56.77 (11.10) | 53.31 (7.82) | 57.29 (11.42) | 0.008 |
| Education (years) | 12.67 (2.61) | 13.30 (2.64) | 12.58 (2.59) | 0.017 |
| Currently Employed | 63.98 | 69.32 | 63.19 | 0.286 |
| Health Indicators | ||||
| MMSE | 28.53 (1.91) | 28.94 (1.47) | 28.46 (1.96) | 0.028 |
| Any IADL disability | 8.64 | 21.59 | 6.72 | <.001 |
| Any ADL disability | 3.37 | 5.68 | 3.03 | 0.202 |
| Self-rated health (poor/fair) | 31.33 | 42.05 | 29.75 | 0.026 |
| Frailty Symptoms | ||||
| Low BMI | 8.49 | 11.36 | 8.07 | 0.306 |
| Exhaustion | 12.15 | 38.64 | 8.24 | <.001 |
| Low energy expenditure | 16.54 | 13.64 | 16.97 | 0.539 |
| Slow movement | 27.09 | 23.86 | 27.56 | 0.522 |
| Weakness | 14.49 | 12.50 | 14.79 | 0.630 |
| Frail* | 6.44 | 10.23 | 5.88 | 0.158 |
| Intermediately frail** | 46.27 | 55.68 | 44.87 | 0.067 |
Lifetime MD status based on DIS/DSM-III-R criteria.
p-value for Fisher exact tests (1 df) for categorical variables and t-tests (681 df) for continuous variables.
MMSE: Mini-mental status exam. IADL: Instrumental activities of daily living. ADL: Activities of daily living.
Indicates a person has 3 or more frailty indicators, defined in the CHS as frail (9)
Indicates a person has 1 or 2 frailty indicators, defined in the CHS as intermediately frail (9).
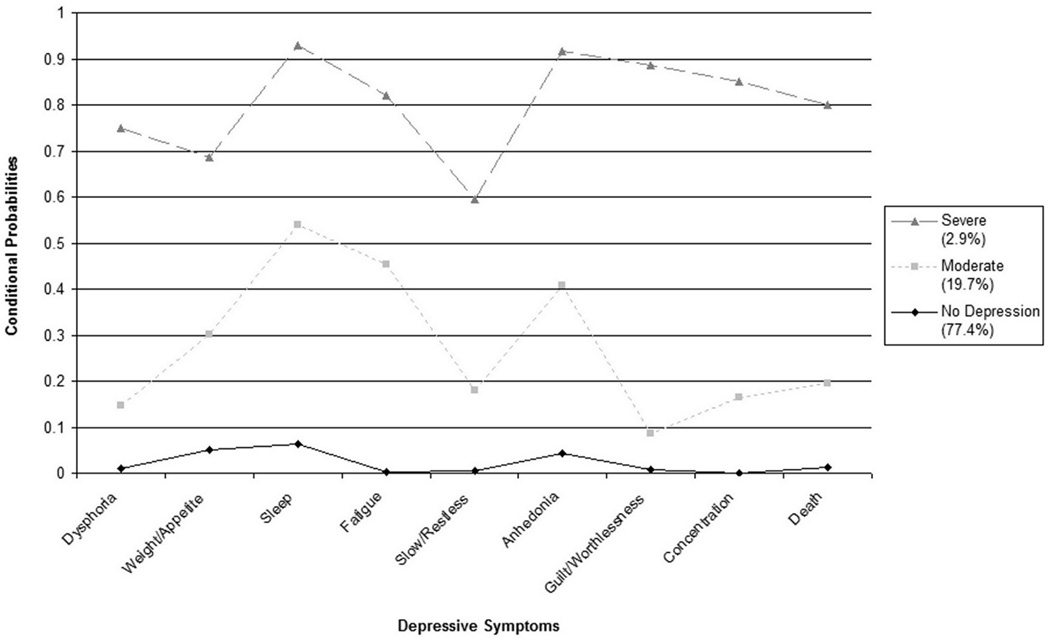
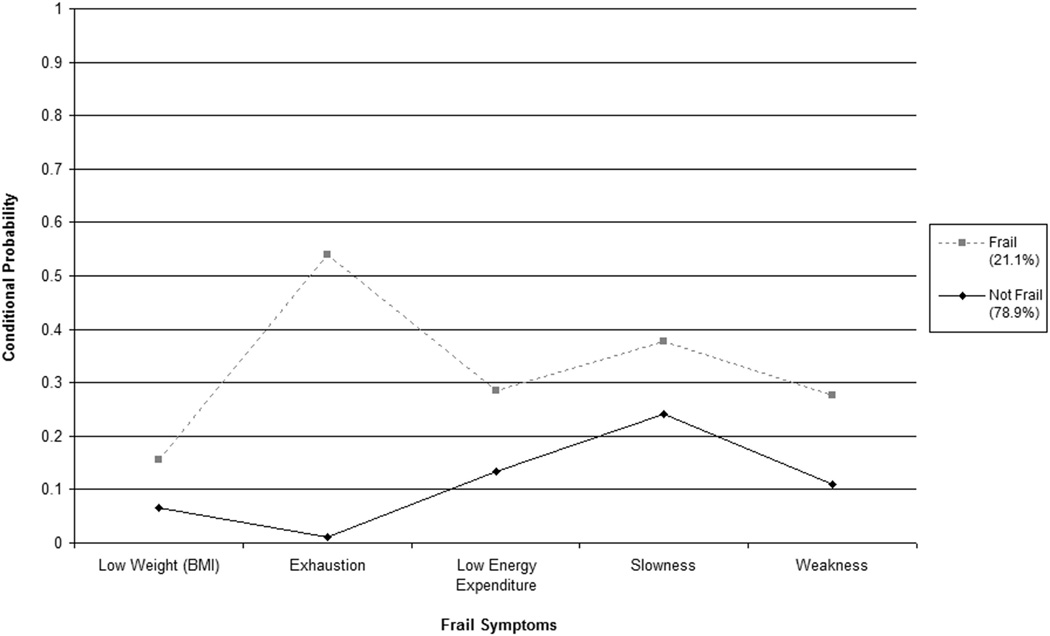
Table 2 shows the model fit statistics and class proportion estimates for the series of confirmatory LCA models described above. All models performed better than the independence model, which specifies no latent structure for the observed symptom patterns. Model 1 fit a single binary latent variable indicated by all 14 observed variables, which represents the hypothesis that all indicators measure the same latent construct with two classes: one class with generally high symptom endorsement on all items of both depression and frailty (class prevalence: 17.8%) and one with low symptom endorsement (class prevalence: 82.2%). This model did not provide as good a fit to the data as those which treated depression and frailty as distinct but overlapping discrete latent constructs represented by their respective indicators (Figure 1). Models 2 – 5 represent successive confirmatory LCA models with increasing numbers of extracted classes. The BIC was similar for Models 4 and 5, but Model 4 had more interpretable parameter estimates and was therefore selected as the final model. Figures 2 illustrate the conditional probabilities of symptom endorsement for depression (Panel A) and frailty (Panel B) derived from the three class model of depression and the two class model of frailty, respectively. Sensitivity analyses using the BMI cutpoint of 18.5 kg/m2 and restricting the analysis to those aged 55 and older produced similar results (see Supplemental Tables 2 and 3). Post-hoc analysis using only the GHQ item to indicate fatigue produced similar results, but as expected because of the use of a less-stringent measure of this indicator, the prevalence of moderate frailty in Models 3 and 5 was higher using this specification (Supplemental Table 4). There were no significant differences in the interpretation of the relationship between depression and frailty across these different specifications of frailty.
Table 2.
Fit statistics and class proportions for competing confirmatory latent class models
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Model Fit Statistics | |||||
| AIC | 5883.19 | 5876.93 | 5835.38 | 5799.24 | 5761.91 |
| BIC | 6014.46 | 6017.25 | 6007.38 | 5989.35 | 5988.23 |
| BICN | 5922.38 | 5918.82 | 5886.73 | 5856.00 | 5829.48 |
| Class Proportions | |||||
| Single Latent Variable | |||||
| Class 1 | .822 | -- | -- | -- | -- |
| Class 2 | .178 | -- | -- | -- | -- |
| Multiple Latent Variable | |||||
| Depression (2 class) | |||||
| Not Depressed | -- | .824 | .825 | -- | -- |
| Depressed | -- | .176 | .175 | -- | -- |
| Frailty (2 class) | |||||
| Not Frail | -- | .814 | -- | .789 | -- |
| Frail | -- | .186 | -- | .211 | -- |
| Depression (3 class) | |||||
| Not depressed | -- | -- | -- | .774 | .777 |
| Moderately depressed | -- | -- | -- | .197 | .194 |
| Severely depressed | -- | -- | -- | .029 | .029 |
| Frailty (3 class) | |||||
| Not frail | -- | -- | .781 | -- | .764 |
| Moderately frail | -- | -- | .138 | -- | .151 |
| Severely frail | -- | -- | .081 | -- | .085 |
Model 1: Single latent variable with 2 classes indicated by all 14 observed variables from depression and frailty. Model 2: Two correlated latent variables (depression and frailty) each indicated by their specific observed variables (2 class model for depression and 2 class model for frailty). Model 3: Two correlated latent variables each indicated by their specific observed variables (2 class model for depression and 3 class model for frailty). Model 4: Two correlated latent variables each indicated by their specific observed variables (3 class model for depression and 2 class model for frailty). Model 5: Two correlated latent variables each indicated by their specific observed variables (3 class model for depression and 3 class model for frailty). AIC: Akaike Information Criterion. BIC: Bayesian Information Criterion. BICN: sample-size adjusted Bayesian Information Criterion.
Figure 2.
Panel A: Conditional probabilities of symptom endorsement for the depression classes
Conditional probabilities estimated from the joint modeling of depression and frailty (Table 2, Model 4).
Panel B: Conditional probabilities of symptom endorsement for the frailty classes
In order to further evaluate the conceptual overlap of depression and frailty, overlapping class proportions resulting from the best fitting model (Model 4) were compared. Class proportions showed that, among those classified as not depressed, 5.9% were considered frail, among those classified as moderately depressed, 69.0% were considered frail, and among those considered severely depressed, 100% were considered frail. To account for chance agreement between latent constructs, a Кl was estimated from the two models that fit equal numbers of depression and frailty classes (Table 2, Models 2 and 5), with a range of 0.66 (95% Confidence Interval (CI): 0.58 – 0.74) for Model 2 to 0.68 (95% CI: 0.62 – 0.75) for Model 5, indicating high level of agreement between the latent constructs (25).
DISCUSSION
This study empirically evaluated the construct overlap between two common syndromes in later life, depression and frailty. The primary finding is that the operational criteria of these constructs identify distinct, but highly overlapping, subpopulations. The overlap between these constructs is substantial as suggested by the Кl, and indicates that these syndromes should be considered jointly in studies aimed at identifying predictors and consequences of health and disability in later life.
This study extends previous LCA reports on depression and frailty. The classes that identified both depression and frailty were characterized by high or low endorsement of all indicator symptoms (and high, moderate, and low endorsement for depression), indicative of a medical syndrome as opposed to distinct biologic processes or random symptom aggregation (9). Our estimates of symptom endorsement were consistent with previous LCA models of these constructs (9, 24). Previous LCA of the CHS frailty criteria assuming two classes estimated a prevalence of 26.7% for the frail class (2, 9); in this study the prevalence of this class was approximately 21%. While similar, the lower proportion in this study may reflect the different operational construction of some indicator variables and the younger age of the sample, although the sensitivity analyses indicated these differences did not substantially impact the final estimated model. Recent studies suggest that frailty can indeed manifest in earlier ages where, as in older adults, it is associated with higher risk of mortality (15). Regarding depression, the current study exhibited slightly higher proportions of individuals in the mild depressive class relative to previous reports (21). This difference might be due to the relatively older age of the sample, as older adults are more likely to endorse higher overall numbers of symptoms yet less likely to meet criteria for major depressive disorder (6, 26). Nonetheless, the similarity between latent class proportions obtained in this study and those obtained in previous studies using similar operational criteria lend validity to the operationalization of these constructs as defined in this study.
While it is clear that symptoms of depression and frailty tend to co-aggregate, the factors that drive this overlap are unclear. In certain instances it is evident that indicator symptoms for frailty and depression measure similar phenomena but in different ways. For instance, the MD symptom group of fatigue is undoubtedly related to the exhaustion criterion of the CHS frailty operationalization. On the other hand, co-occurrence of symptoms such as slowness in frailty and concentration difficulties in MD may be a sign of general progressive decline in underlying mental and physiologic systems. Consistent with this notion, Hajjar and colleagues have identified a phenotype among older adults characterized by the aggregation of impairment in executive functioning, high depressive symptoms, and slowed gait speed, which is independently associated with hypertension and other cardiovascular conditions (11). They argue that this aggregation may be a manifestation of pathological vascular processes in subcortical regions of the brain (11). A third possibility is that symptoms of depression lead causally to symptoms of frailty and vice-versa, potentially in a positive feedback loop (27, 28, 29). Without longitudinal data on both depression and frailty we cannot determine the predictive relationship between these conditions. Our findings indicate that the construct of frailty is highly overlapping with that of depression in mid- and later-life, which has implications for the design and interpretation of epidemiologic and clinical studies of these conditions. These results indicate that future attempts to estimate the predictive relationship between depression and frailty explicitly account for the substantial correlation in these constructs identified here.
These findings should be interpreted in light of study limitations. The operationalization of the CHS frailty criteria was limited by the measures collected and differed some from previous reports. There are also other established criteria for frailty that were not examined, which may show a different relationship to depression. The sample was relatively young (mean age: 57 years), which may have influenced our results and therefore these findings should be replicated for adults over the age of 65. Also, due to the sample size some of the cells in the LCA were small and the number of classes that could be reliably extracted was limited; these analyses should be replicated in a larger sample. This study also has several strengths, notably the community-based sample which limits the influence of selection bias. The DIS depression module assesses all symptoms of depression regardless of endorsement of dysphoria or anhedonia, and is thus an apt instrument for examining the clustering of depression and frailty symptoms in the general population.
The results of this study underscore the need for interdisciplinary research which acknowledges the conceptual and empirical overlap of physical and mental health in aging (7). From a theoretical standpoint depression and frailty should be looked upon less as distinct concepts and more as interrelated syndromes. These findings indicate that previous efforts to examine frailty independently from depression, as has been done in previous studies by excluding individuals with depressive symptomology from the analysis (1), may imply an artificial and unwarranted distinction between these syndromes, at least concerning epidemiologic investigations of the predictors of disability, morbidity, and mortality in later life. This study supports the conjecture by Tinetti and colleagues to adopt a unified approach to conceptualizing geriatric syndromes, both in research and clinical care.
Supplementary Material
Acknowledgements
B. Mezuk is supported by the VCU Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) Program (K12-HD055881). The Baltimore ECA Study is supported by the National Institute on Drug Abuse (R01-DA026652). This project was also supported by award number UL1RR031990 from the National Center for Research Resources and NIH Roadmap for Medical Research and R03-MH64474 from National Institute of Mental Health, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Appendix A: Kappa for 2 × 2 Class Latent Variable Model
The symbols represent joint distributions from Table 2, Model 2 for those categorized as frail and depressed and those categorized as neither frail nor depressed, respectfully. The πD and πF symbols represent the marginal distributions of latent classes (subscripts: 1 = severe or moderate symptoms; 0 = low or no symptoms; superscripts: F = frail classes; D = depression classes).
Appendix B: Kappa for 3 × 3 Class Latent Variable Model
The πDF symbols represent the joint distributions from Table 2, Model 5: those categorized as severely frail and severely depressed (), those categorized as moderately depressed and moderately frail (), and those categorized as neither frail nor depressed (). The πD and πF symbols represent the marginal distributions of latent classes (subscripts: 2 = severe symptom levels; 1 = moderate symptom levels; 0 = low or no symptoms; superscripts: F = frail classes; D = depression classes).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Cigolle C, Ofstedal M, Tian Z, et al. Comparing models of frailty: the Health and Retirement Study. J Am Geriatr Soc. 2009;57:830–839. doi: 10.1111/j.1532-5415.2009.02225.x. [DOI] [PubMed] [Google Scholar]
- 2.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M157. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 3.Strawbridge WJ, Shema SJ, Balfour JL, et al. Antecedents of frailty over three decades in an older cohort. J Gerontol B Psychol Sci Soc Sci. 1998;53:S9–S16. doi: 10.1093/geronb/53b.1.s9. [DOI] [PubMed] [Google Scholar]
- 4.Rockwood K, Andrew M, Mitnitski A. A comparison of two approaches to measuring frailty in elderly people. J Gerontol B Psychol Sci Soc Sci. 2007;62:738–743. doi: 10.1093/gerona/62.7.738. [DOI] [PubMed] [Google Scholar]
- 5.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–1970. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 6.Gallo JJ, Rabins PV. Depression without sadness: alternative presentations of depression in late life. Am Fam Physician. 1999;60:820–826. [PubMed] [Google Scholar]
- 7.Katz I. Depression and frailty: the need for multidisciplinary research. Am J Geriatr Psychiatry. 2004;12:1–6. [PubMed] [Google Scholar]
- 8.Fried L, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 9.Bandeen Roche K, Xue Q, Ferrucci L, et al. Phenotype of frailty: characterization in the women's health and aging studies. J Gerontol A Biol Sci Med Sci. 2006;61:262–266. doi: 10.1093/gerona/61.3.262. [DOI] [PubMed] [Google Scholar]
- 10.Tinetti ME, Inouye SK, Gill TM, et al. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA (Chicago, Ill.) 1995;273:1348–1353. [PubMed] [Google Scholar]
- 11.Hajjar I, Yang F, Sorond F, et al. A novel aging phenotype of slow gait, impaired executive function, and depressive symptoms: relationship to blood pressure and other cardiovascular risks. J Gerontol A Biol Sci Med Sci. 2009;64:994–1001. doi: 10.1093/gerona/glp075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eaton WW, Kessler LG. Epidemiologic field methods in psychiatry: the NIMH epidemiologic catchment area program. New York: Academic Press; 1985. [Google Scholar]
- 13.Eaton WW, Kalaydjian A, Scharfstein DO, et al. Prevalence and incidence of depressive disorder: the Baltimore ECA follow-up, 1981–2004. Acta Psychiatr Scand. 2007;116:182–188. doi: 10.1111/j.1600-0447.2007.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Szklo M, Nieto FJ. Epidemiology: beyond the basics. Jones and Bartlett Publishers; 2000. [Google Scholar]
- 15.Rockwood K, Song X, Mitnitski A. Changes in relative fitness and frailty across the adult lifespan: evidence from the Canadian National Population Health Survey. CMAJ. 2011:E487–E494. doi: 10.1503/cmaj.101271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robins LN, Helzer JE, Croughan J, et al. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association: Diagnostic and statistical manual of mental disorders, DSM-III. 3rd ed. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- 18.Goodman L. Exploratory latent structure-analysis using both indentifiable and unidentifiable models. Biometrika. 1974;61:215–231. [Google Scholar]
- 19.Chen L, Eaton WW, Gallo JJ, et al. Understanding the heterogeneity of depression through the triad of symptoms, course and risk factors: a longitudinal, population-based study. J Affect Disord. 2000;59:1–11. doi: 10.1016/s0165-0327(99)00132-9. [DOI] [PubMed] [Google Scholar]
- 20.Dumenci L. The Psychometric Latent Agreement Model (PLAM) for discrete latent variables measured by multiple items. Organ Res Methods. 2011;14:91–115. doi: 10.1177/1094428110374649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:213–220. [Google Scholar]
- 22.Muthén LK, Muthén BO. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; [Google Scholar]
- 23.Stata Statistical Software: Release 11 [computer program] College Station, TX: StataCorp LP.: StataCorp; 2009. [Google Scholar]
- 24.Eaton WW, Dryman A, Sorenson A, et al. DSM-III major depressive disorder in the community. A latent class analysis of data from the NIMH epidemiologic catchment area programme. Br J Psychiatry. 1989;155:48–54. doi: 10.1192/bjp.155.1.48. [DOI] [PubMed] [Google Scholar]
- 25.Altman DG. Practical statistics for medical research. Chapman and Hall; 1991. [Google Scholar]
- 26.Fiske A, Wetherell J, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mezuk B, Eaton WW, Golden SH. Depression and osteoporosis: epidemiology and potential mediating pathways. Osteoporosis Int. 2008;19:1–12. doi: 10.1007/s00198-007-0449-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mezuk B, Edwards L, Lohman M, Choi M, Lapane K. Depression and frailty in later life: A synthetic review. Int J Geriatr Psychiatr. 2011 doi: 10.1002/gps.2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barry LC, Murphy TE, Gill TM. Depressive symptoms and functional transitions over time in older persons. Am J Geriatr Psychiatr. 2011;19:783–791. doi: 10.1097/JGP.0b013e3181ff6669. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.