SUMMARY
The Goto-Kakizaki (GK) rat is an inbred model of type 2 diabetes (T2D); GK rats are lean but have hyperglycemia and increased gluconeogenesis. However, fasting hyperglycemia in other commonly used rodent models of T2D is associated with increased corticosterone, and thus the underlying mechanism for hyperglycemia differs significantly from T2D in humans. Information regarding corticosterone in the GK rat is not readily available. We studied 14- to 16-week-old GK rats in comparison with age-matched control Wistar-Kyoto (WK) rats. GK rats had lower body weights (WK: 343±10 g vs GK: 286±9 g, P<0.01), but higher plasma glucose concentrations (WK: 132±1.5 mg/dl vs GK: 210±11.7 mg/dl, P<0.01). This was associated with an ∼twofold increase in PEPCK1 expression (P<0.05). However, these findings were also associated with elevations in plasma corticosterone and urinary corticosterone excretion. Ketoconazole (KTZ) treatment in GK rats reduced plasma corticosterone, fasting glucose (GK: 218±15 mg/dl vs GK-KTZ: 135±19 mg/dl, P<0.01) and rates of glucose production [GK: 16.5±0.6 mg/(kg-minute) vs GK-KTZ: 12.2±0.9 mg/(kg-minute), P<0.01]. This was associated with an ∼40% reduction in hepatic PEPCK1 expression as well as a 20% reduction in alanine turnover. Thus, hypercorticosteronemia might contribute to the diabetic phenotype of GK rats and should be considered as a potential confounder in rodent models of T2D.
INTRODUCTION
Animal models are indispensable in studying the mechanisms responsible for the pathogenesis and complications of type 2 diabetes (T2D), as well as preclinical testing for novel therapeutic agents. Early attempts to establish a hyperglycemic phenotype utilized experimental destruction of the pancreas, accomplished either surgically or chemically (e.g. streptozotocin, alloxan). Although both methods continue to be used, they are often criticized as not accurately reflecting the human T2D phenotype. Moreover, the induction of diabetes can be variable and labor intensive, as in the case of partial pancreatectomy. Thus, many investigators rely on specific rodent strains that model key features of T2D. These genetic models have been widely used to explore the pathophysiology of obesity and T2D, as well as in preclinical drug development.
Genetic rodent models can recapitulate several phenotypes of human T2D, including fasting hyperglycemia, increased rates of glucose production and increased gluconeogenesis. However, the underlying mechanisms for these changes could be very different. We recently reported that fasting hyperglycemia in Zucker diabetic fatty (ZDF)-[Leprfa] rats and db/db-[Leprdb] mice was associated with increased hepatic expression of phosphoenolpyruvate carboxykinase (PEPCK), a key gluconeogenic enzyme. In contrast, increased expression of PEPCK was not evident in other rodent models (e.g. streptozotocin-treated high-fat-fed rats) or in individuals with T2D (Samuel et al., 2009). One reason for this discrepancy is that many of the inbred T2D rodent strains also have elevated corticosterone, which can increase expression of gluconeogenic enzymes. T2D in humans is not associated with elevations in glucocorticoids (Veneziale et al., 1983; Robinson et al., 2000). Thus, although these common rodent models grossly manifest a similar phenotype as humans with T2D, the underlying mechanisms leading to that phenotype are markedly different.
Although less commonly utilized, the Goto-Kakizaki (GK) rat is also an established model of T2D. This rat strain was developed by selectively breeding Wistar rats for glucose intolerance over multiple generations (Goto et al., 1975; Goto and Kakizaki, 1981). The resulting animals are a polygenic strain and spontaneously develop hyperglycemia, have decreased β-cell function and manifest several complications of diabetes (Miyamoto et al., 1996; Vesely et al., 1999; Murakawa et al., 2002; Janssen et al., 2004). Fasting hyperglycemia in the GK rats is due to increased gluconeogenesis (Sena et al., 2007). However, there are no data regarding corticosterone production in these animals. Here, we determine whether increased corticosterone is associated with hyperglycemia in the GK rat.
RESULTS
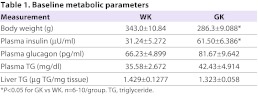
GK rats had lower body weights than age-matched Wistar-Kyoto (WK) rats (Table 1). As expected, the GK rats had increased fasting plasma glucose concentrations and rate of endogenous glucose production (Fig. 1A,B). Hyperglycemia was associated with an ∼twofold increase in fasting plasma insulin concentrations, suggesting insulin resistance. In contrast, fasting plasma glucagon concentrations were equivalent between the two rat strains (Table 1). mRNA expression of key gluconeogenic enzymes [cytosolic PEPCK (PEPCK1); glucose 6-phosphatase, catalytic (G6Pc) and T-1 translocase (G6Pt); and pyruvate carboxylase (PC)] were measured (Fig. 1C–F). PEPCK1 expression was increased twofold in GK rats (P=0.02). There was no difference in G6Pt expression between the two groups (Fig. 1D). In contrast, G6Pc and PC expression were decreased in the GK rats relative to the WK controls.
Table 1.
Baseline metabolic parameters
Fig. 1.
Comparison between WK and GK rats after an overnight fast. (A) Fasting plasma glucose concentration. (B) Endogenous glucose production. (C–F) Expression of gluconeogenic enzymes. (G) Fasting plasma corticosterone. (H) 24-hour urine corticosterone normalized to creatinine. *P<0.05, **P<0.01, ***P<0.001. n=7–10/group.
Increased corticosterone has been documented in other rodent models of T2D. To determine whether or not hypercorticosteronemia plays a role in the phenotype of GK rats, we measured plasma and urinary corticosterone concentrations. Plasma corticosterone was measured after an overnight fast from rodents with indwelling catheters. Plasma corticosterone was elevated approximately threefold (Fig. 1G). There was no detectable difference in plasma adrenocorticotropic hormone (ACTH) concentrations (WK: 29.0±6.2 ng/ml vs GK: 30.1±6.3 ng/ml, P=0.90). Because a single time point might not accurately reflect the entire exposure of the animal to corticosterone, we also measured 24-hour urinary corticosterone excretion, normalized to urinary creatinine. Urinary corticosterone excretion was ∼eightfold higher in the GK rats in comparison with the WK rats (Fig. 1H). Finally, corticosterone might be regenerated through the action of the 11β-hydroxysteroid dehydrogenase type 1 (11βHSD1). However, neither hepatic nor adipose 11βHSD1 mRNA expression differed between WK and GK rats [liver WK: 0.57±0.11 relative abundance (RA) vs liver GK: 0.81±0.26 RA, P=0.55; white adipose tissue (WAT) WK: 0.57±0.22 RA vs GK: 0.88±0.13 RA, P=0.32].
To determine whether decreasing the corticosterone levels would correct the phenotype, GK rats were treated with ketoconazole (KTZ), a piperazine antifungal agent that inhibits 11β-hydroxylase (Loose et al., 1983). GK rats were gavaged either with KTZ (175 mg/kg body weight) or water for 3 days, followed by a 6-hour fast on the morning of the study. Body weight was unaltered (GK-Water: 266±8 g vs GK-KTZ: 276±7 g). KTZ treatment lowered plasma corticosterone (Fig. 2A). This was associated with an ∼40% reduction in plasma glucose concentration (Fig. 2B) and a 25% reduction in the basal rate of glucose production (Fig. 2C). KTZ treatment reduced plasma insulin concentration (GK-Water: 84.06±7.55 μU/ml vs GK-KTZ: 31.04±6.51 μU/ml, P=0.0003) without any change in plasma glucagon concentration (GK-Water: 65.7±11.3 ng/ml vs GK-KTZ: 109.4±21.5 ng/ml, P=0.12), suggesting an improvement in insulin sensitivity. These changes were associated with reductions in PEPCK1 mRNA and protein (Fig. 2E,F). PC mRNA was also reduced (GK-Water: 2.2±0.3 RA vs GK-KTZ: 0.8±0.2 RA, P=0.004), but not G6Pc (P=0.06) or G6Pt (P=0.10). Previous studies in these rats suggested that increased Cori cycling (glucose-alanine cycle) might also be a determinant of increased glucose production. Alanine turnover was decreased ∼20% in GT-KTZ rats (Fig. 2D), and might represent another mechanism for the reduction in glucose production following KTZ treatment in these animals.
Fig. 2.
Effect of KTZ treatment in GK rats. KTZ treatment in GK rats reduces (A) fasting plasma corticosterone, (B) fasting plasma glucose, (C) rate of endogenous glucose production, (D) rate of alanine turnover, (E) PEPCK1 mRNA expression and (F) PEPCK1 protein expression in cytosolic fraction (representative blots shown below). *P<0.05, **P<0.01. n=5–7/group.
DISCUSSION
Rodent models are essential for exploring the mechanisms underlying the pathogenesis of T2D and for preclinical testing of novel therapies. Although increased corticosterone has been described in these models (Saito and Bray, 1984; Shimomura et al., 1987; Takeshita et al., 2000; Bates et al., 2008), this remains an underappreciated confounder. Disrupting the increased corticosterone production in these models can ameliorate the phenotype in these strains, either by adrenalectomy (Saito and Bray, 1984), inhibition of 11βHSD1 (Tomlinson and Stewart, 2005) or knockdown of the glucocorticoid receptor (Watts et al., 2005). The GK rat model differs from these more common models in several aspects. This non-obese strain is thought to have polygenic diabetes (Galli et al., 1996; Gauguier et al., 1996). The exact genetic defects remain unclear, although linkage studies have identified a region of chromosome 1 that contains genes for UCP2, UCP3 and Tub (Kaisaki et al., 1998). GK rats are not known to have mutations in leptin or the leptin receptor genes; one study has reported that these animals do seem to have some degree of leptin resistance (Maekawa et al., 2006).
To ascertain whether the increased corticosterone contributes to the diabetic phenotype in this model, we performed a set of metabolic measurements in GK rats in comparison with WK control rats. We confirmed previous findings demonstrating that GK rats had increased fasting glucose and increased rates of glucose production (Farese et al., 1994; O’Rourke et al., 1997). Recently, studies utilizing a combination of U-13C glucose and 2H2O to quantify the pathways contributing to glucose production demonstrated that GK rats have increased rates of gluconeogenesis that are largely attributable to increased gluconeogenesis from phosphoenolpyruvate, consistent with our finding of increased PEPCK1 expression (Sena et al., 2007). In addition, this study reported an increased contribution of the Cori cycle to glucose production.
In the present study, we found an increased rate of glucose production in GK rats compared with WK rats, and this was associated with increased expression of PEPCK1 mRNA. In contrast, the expression of other gluconeogenic enzymes was not significantly different. Hypercorticosteronemia per se might account for many of these findings because the promoter elements of the genes encoding these enzymes contain glucocorticoid receptor elements (Imai et al., 1990; Hall et al., 1995; Vander Kooi et al., 2005). We observed increases in both fasting plasma corticosterone concentration and 24-hour urinary corticosterone excretion in the GK rat, relative to the WK rat. The increase in plasma corticosterone concentration seemed to be independent of changes in hepatic or adipose 11βHSD1 mRNA expression. Fasting plasma ACTH concentrations were identical, which could suggest that the hypothalamic-pituitary-adrenal axis might have an altered set point for cortisol production, although this is difficult to judge accurately with a single time point.
We further examined the role of corticosterone in the development of the hyperglycemic phenotype in GK rats using KTZ to decrease corticosterone synthesis. Treatment with KTZ decreased plasma corticosterone concentration, and lowered fasting plasma glucose and insulin concentrations. This was associated with a reduction in the basal rate of glucose production and a decrease in the expression of PEPCK1. However, the ability of this enzyme to regulate gluconeogenic flux is much less than previously thought, with a metabolic control coefficient of 0.18, a low value for a ‘rate-controlling’ enzyme (Burgess et al., 2007). Although we also observed a reduction in hepatic PC mRNA, there might be other mechanisms accounting for decreased fasting glucose following KTZ. Sena et al. reported that Cori cycle flux was ∼twofold higher in the GK rats compared with WK rats (Sena et al., 2007). Thus, the increased delivery of alanine to the livers of GK rats might contribute to increased gluconeogenesis. Here, we demonstrate that KTZ treatment reduced alanine turnover, suggesting that a decrease in Cori cycling with KTZ treatment might also contribute to the reduction in glucose production.
The present study has some limitations. Suppressing corticosterone production, even in normal rodents, could decrease glucose production. Additionally, the selective inbreeding of the GK rats might have created a strain that has sufficient genetic differences from the WK rat such that a direct comparison is not ideal. Despite this concern, the WK rats remain the best comparator group for these studies. Taken together, these data suggest that increased corticosterone might play a role in the development of the hyperglycemic phenotype in the GK rat by both increasing the gluconeogenic capacity of the liver as well as enhancing substrate delivery. Future studies should examine the underlying mechanisms leading to increased corticosterone in this strain.
There is evidence that tissue-specific production of cortisol contributes to the various features of the metabolic syndrome, for example, through the 11βHSD1 pathway. However, a frank increase in plasma glucocorticoid concentration is not a typical feature in humans with T2D (Veneziale et al., 1983; Robinson et al., 2000). Thus, the increased corticosterone that is present in several rodent models might lead to erroneous conclusions about the pathophysiology of T2D and efficacy of treatments tested in preclinical models. For example, increased gluconeogenesis in these models had been largely ascribed to increased expression of PEPCK, leading to the view that this was a mechanism for increased gluconeogenesis in humans with T2D. However, no relationship between PEPCK and glucose production was seen in models without increased corticosterone or in humans with T2D (Samuel et al., 2009). Thus, although the ‘ideal’ rodent models of T2D will probably remain elusive, corticosterone should be assessed as a potential confounder.
METHODS
Animals
Male GK rats, and male Wistar Kyoto rats, a rodent control model, were obtained from Taconic at approximately 14- to 16-weeks of age. Rats were fed ad libitum the standard commercial diet (NIH #31M Rodent Diet, Taconic) along with ad libitum access to water. They were housed in 12 hours of light/12 hours of dark cycles and acclimated for 5–7 days prior to the placement of jugular venous and carotid catheters. All studies were approved by the International Animal Care and Use Committee (IACUC) at the Veterans Affairs Medical Center, West Haven, CT.
KTZ treatment
GK rats received either a dose of water or KTZ suspension (175 mg/kg body weight) via oral gavage technique for 3 consecutive days prior to the experiment. Rats were studied after a 6-hour fast.
Measurement of basal rates of glucose production
Endogenous glucose production was measured in catheterized rats that received unprimed, continuous infusions of 6,6-2H glucose for 240 minutes at a rate of 0.025 ml/(kg-minute). In studies measuring alanine turnover, 3-13C alanine was infused at 0.5 mg/(kg-minute). Plasma blood samples were obtained at 10-minute intervals between 210 and 240 minutes. At the end of the infusion, rats were euthanized and liver tissues were harvested in situ with tongs that had been pre-cooled in liquid nitrogen.
Metabolites and hormones
Blood was collected from surgically placed catheters, as described previously (Samuel et al., 2004), after 120 minutes and immediately centrifuged in aprotinized Beckman P100 tubes, and plasma supernatants were removed and stored at 4°C. Plasma glucose was measured by the glucose oxidase method on a Beckman Glucose Analyzer II. Plasma insulin, glucagon and corticosterone were measured by RIA (Millipore). Urine was collected in metabolic cages after allowing for a 24-hour acclimation period. Plasma ACTH was measured by EIA (Phoenix Pharmaceuticals).
Analysis of plasma glucose and alanine by GC/MS
To determine the enrichment of 6,6-2H glucose or alanine in plasma, samples were deproteinized with 5 volumes of 100% methanol, dried, and derivatized with 1:1 acetic anhydride/pyridine to produce the pentacetate derivative of glucose, or with 1:8 trifluoroacetic anhydride/methylene chloride to produce the trifluoroacetyl n-butyl ester of alanine. The atom percent of enrichment of glucoseM+2 and alanineM+1 was measured by gas-chromatography–mass-spectrometry (GC/MS) analysis using a Hewlett-Packard 5890 gas chromatograph interfaced to a Hewlett-Packard 5971A mass-selective detector operating in the electron-ionization mode (Petersen et al., 2005). GlucoseM+2 enrichments were determined from the ratio of m/z 202 to 200. AlanineM+1 enrichments were determined from the ratio of m/z 243 to 242. Endogenous glucose and alanine production was calculated using Steele’s equation in steady state (Wolfe and Chinkes, 2005).
TRANSLATIONAL IMPACT.
Clinical issue
A key finding in humans with type 2 diabetes (T2D) is fasting hyperglycemia attributed to increased hepatic gluconeogenesis. Many different rodent models are used to explore the potential mechanism for this clinical phenotype, but the pathogenesis of fasting hyperglycemia in certain models might not be relevant to the human situation. For example, many rodent strains have increased levels of corticosterone, which increases the expression of gluconeogenic enzymes; however, T2D in humans is not associated with increased levels of corticosterone. Although data concerning corticosterone levels were available for several other rodent models, published data were not available for the Goto-Kakizaki (GK) rat, a non-obese rat strain that develops T2D early in life and is an established model of the human disease.
Results
These results show that GK rats have increased levels of corticosterone compared with Wistar-Kyoto (WK) control rats. Decreasing plasma corticosterone in GK rats using ketoconazole normalized plasma glucose, decreased endogenous glucose production and seemed to improve insulin sensitivity. This could be attributed to decreased expression of phosphoenolpyruvate carboxykinase (PEPCK; a key gluconeogenic enzyme) and/or decreased Cori cycling.
Implications and future directions
These results show that hypercorticosteronemia is associated with hyperglycemia in the GK rat. Given that hypercorticosteronemia is an important confounder in rodent models of T2D, studies involving this model should take this into consideration when investigating mechanisms of T2D and testing responses to therapeutic agents.
Total RNA preparation and real-time quantitative RT-PCR analysis
Total RNA was extracted from liver samples stored in RNAlater solution by using the RNeasy kit (Qiagen). RNA was reverse-transcribed into cDNA by using Stratascript Reverse Transcriptase (Stratagene). The abundance of transcripts for PEPCK1 (cytosolic), G6Pc and PC were assessed by real-time PCR using a SYBR Green detection system (Stratagene). For each run, samples were run in duplicate for both the gene of interest and actin. The expression data for each gene of interest and actin were normalized for the efficiency of amplification, as determined by a standard curve included on each run (Pfaffl, 2001). All mRNA expression values are expressed as relative abundance (RA).
Assessment of protein content
Liver proteins were extracted in homogenization buffer (50 mM HEPES, 150 mM NaCl, 1 mM EDTA, 2 mM Na3VO4, 20 mM Na4P2O7, 100 mM NaF, 1% Triton X-100, 2 mM PMSF, 20 μg/ml aprotinin, 1 mg/ml leupeptin and pepstatin) and separated into cytosolic and nuclear/mitochondrial fractions via ultracentrifugation. Protein concentrations were determined by the Bradford method (Bio-Rad). Equal amounts of protein were resolved by SDS-PAGE and electroblotted onto a polyvinylidene difluoride membrane (DuPont) by using a semidry transfer cell (Bio-Rad). After blocking for 2 hours at room temperature in TBST containing 5% (wt/vol) non-fat dried milk, and then incubated overnight with polyclonal rabbit anti-PEPCK antibody (SantaCruz). After further washings, membranes were incubated with horseradish-peroxidase-conjugated secondary antibody and visualized by ECL (Amersham). These blots were stripped and reblotted with both HSP90 and VDAC antibody to ensure proper fractionation had occurred.
Statistical analysis
Statistical analysis of the data was performed using GraphPad Prism 5.0. All data are expressed as mean ± s.e.m. For comparisons of two groups, Student’s t-test was used.
Acknowledgments
We graciously acknowledge the technical assistance of Yanna Kosover and Aida Grossman.
Footnotes
COMPETING INTERESTS
The authors declare that they do not have any competing or financial interests.
AUTHOR CONTRIBUTIONS
Both authors designed and performed experiments, analyzed data, and wrote and edited the manuscript.
FUNDING
This project was supported by a VA Merit Review Award (to V.T.S.).
REFERENCES
- Bates H. E., Sirek A. S., Kiraly M. A., Yue J. T., Goche Montes D., Matthews S. G., Vranic M. (2008). Adaptation to mild, intermittent stress delays development of hyperglycemia in the Zucker diabetic Fatty rat independent of food intake: role of habituation of the hypothalamic-pituitary-adrenal axis. Endocrinology 149, 2990–3001 [DOI] [PubMed] [Google Scholar]
- Burgess S. C., He T., Yan Z., Lindner J., Sherry A. D., Malloy C. R., Browning J. D., Magnuson M. A. (2007). Cytosolic phosphoenolpyruvate carboxykinase does not solely control the rate of hepatic gluconeogenesis in the intact mouse liver. Cell Metab. 5, 313–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farese R. V., Standaert M. L., Yamada K., Huang L. C., Zhang C., Cooper D. R., Wang Z., Yang Y., Suzuki S., Toyota T. (1994). Insulin-induced activation of glycerol-3-phosphate acyltransferase by a chiro-inositol-containing insulin mediator is defective in adipocytes of insulin-resistant, type II diabetic, Goto-Kakizaki rats. Proc. Natl. Acad. Sci. USA 91, 11040–11044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galli J., Li L. S., Glaser A., Ostenson C. G., Jiao H., Fakhrai-Rad H., Jacob H. J., Lander E. S., Luthman H. (1996). Genetic analysis of non-insulin dependent diabetes mellitus in the GK rat. Nat. Genet. 12, 31–37 [DOI] [PubMed] [Google Scholar]
- Gauguier D., Froguel P., Parent V., Bernard C., Bihoreau M. T., Portha B., James M. R., Penicaud L., Lathrop M., Ktorza A. (1996). Chromosomal mapping of genetic loci associated with non-insulin dependent diabetes in the GK rat. Nat. Genet. 12, 38–43 [DOI] [PubMed] [Google Scholar]
- Goto Y., Kakizaki M. (1981). The spontaneous-diabetes rat-A model of non-insulin dependent diabetes-mellitus. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 57, 381–384 [Google Scholar]
- Goto Y., Kakizaki M., Masaki N. (1975). Spontaneous diabetes produced by selective breeding of normal wistar rats. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 51, 80–85 [Google Scholar]
- Hall R. K., Sladek F. M., Granner D. K. (1995). The orphan receptors COUP-TF and HNF-4 serve as accessory factors required for induction of phosphoenolpyruvate carboxykinase gene transcription by glucocorticoids. Proc. Natl. Acad. Sci. USA 92, 412–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai E., Stromstedt P. E., Quinn P. G., Carlstedt-Duke J., Gustafsson J. A., Granner D. K. (1990). Characterization of a complex glucocorticoid response unit in the phosphoenolpyruvate carboxykinase gene. Mol. Cell. Biol. 10, 4712–4719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen U., Vassiliadou A., Riley S. G., Phillips A. O., Floege J. (2004). The quest for a model of type II diabetes with nephropathy: the Goto Kakizaki rat. J. Nephrol. 17, 769–773 [PubMed] [Google Scholar]
- Kaisaki P. J., Woon P. Y., Wallis R. H., Monaco A. P., Lathrop M., Gauguier D. (1998). Localization of tub and uncoupling proteins (Ucp) 2 and 3 to a region of rat chromosome 1 linked to glucose intolerance and adiposity in the Goto-Kakizaki (GK) type 2 diabetic rat. Mamm. Genome 9, 910–912 [DOI] [PubMed] [Google Scholar]
- Loose D. S., Kan P. B., Hirst M. A., Marcus R. A., Feldman D. (1983). Ketoconazole blocks adrenal steroidogenesis by inhibiting cytochrome P450-dependent enzymes. J. Clin. Invest. 71, 1495–1499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maekawa F., Fujiwara K., Kohno D., Kuramochi M., Kurita H., Yada T. (2006). Young adult-specific hyperphagia in diabetic Goto-kakizaki rats is associated with leptin resistance and elevation of neuropeptide Y mRNA in the arcuate nucleus. J. Neuroendocrinol. 18, 748–756 [DOI] [PubMed] [Google Scholar]
- Miyamoto K., Ogura Y., Nishiwaki H., Matsuda N., Honda Y., Kato S., Ishida H., Seino Y. (1996). Evaluation of retinal microcirculatory alterations in the Goto-Kakizaki rat. A spontaneous model of non-insulin-dependent diabetes. Invest. Ophthalmol. Vis. Sci. 37, 898–905 [PubMed] [Google Scholar]
- Murakawa Y., Zhang W., Pierson C. R., Brismar T., Ostenson C. G., Efendic S., Sima A. A. (2002). Impaired glucose tolerance and insulinopenia in the GK-rat causes peripheral neuropathy. Diabetes Metab. Res. Rev. 18, 473–483 [DOI] [PubMed] [Google Scholar]
- O’Rourke C. M., Davis J. A., Saltiel A. R., Cornicelli J. A. (1997). Metabolic effects of troglitazone in the Goto-Kakizaki rat, a non-obese and normolipidemic rodent model of non-insulin-dependent diabetes mellitus. Metabolism 46, 192–198 [DOI] [PubMed] [Google Scholar]
- Petersen K. F., Dufour S., Befroy D., Lehrke M., Hendler R. E., Shulman G. I. (2005). Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes 54, 603–608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaffl M. W. (2001). A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 29, e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson S. W., Dinulescu D. M., Cone R. D. (2000). Genetic Models of obesity and energy balance in the mouse. Annu. Rev. Genet. 34, 687–745 [DOI] [PubMed] [Google Scholar]
- Saito M., Bray G. A. (1984). Adrenalectomy and food restriction in the genetically obese (ob/ob) mouse. Am. J. Physiol. 246, R20–R25 [DOI] [PubMed] [Google Scholar]
- Samuel V. T., Liu Z. X., Qu X., Elder B. D., Bilz S., Befroy D., Romanelli A. J., Shulman G. I. (2004). Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J. Biol. Chem. 279, 32345–32353 [DOI] [PubMed] [Google Scholar]
- Samuel V. T., Beddow S. A., Iwasaki T., Zhang X. M., Chu X., Still C. D., Gerhard G. S., Shulman G. I. (2009). Fasting hyperglycemia is not associated with increased expression of PEPCK or G6Pc in patients with Type 2 Diabetes. Proc. Natl. Acad. Sci. USA 106, 12121–12126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sena C. M., Barosa C., Nunes E., Seica R., Jones J. G. (2007). Sources of endogenous glucose production in the Goto-Kakizaki diabetic rat. Diabetes Metab. 33, 296–302 [DOI] [PubMed] [Google Scholar]
- Shimomura Y., Bray G. A., Lee M. (1987). Adrenalectomy and steroid treatment in obese (ob/ob) and diabetic (db/db) mice. Horm. Metab. Res. 19, 295–299 [DOI] [PubMed] [Google Scholar]
- Takeshita N., Yoshino T., Mutoh S. (2000). Possible involvement of corticosterone in bone loss of genetically diabetic db/db mice. Horm Metab. Res. 32, 147–151 [DOI] [PubMed] [Google Scholar]
- Tomlinson J. W., Stewart P. M. (2005). Mechanisms of disease: Selective inhibition of 11beta-hydroxysteroid dehydrogenase type 1 as a novel treatment for the metabolic syndrome. Nat. Clin. Pract. Endocrinol. Metab. 1, 92–99 [DOI] [PubMed] [Google Scholar]
- Vander Kooi B. T., Onuma H., Oeser J. K., Svitek C. A., Allen S. R., Vander Kooi C. W., Chazin W. J., O’Brien R. M. (2005). The glucose-6-phosphatase catalytic subunit gene promoter contains both positive and negative glucocorticoid response elements. Mol. Endocrinol. 19, 3001–3022 [DOI] [PubMed] [Google Scholar]
- Veneziale C. M., Donofrio J. C., Nishimura H. (1983). The concentration of P-enolpyruvate carboxykinase protein in murine tissues in diabetes of chemical and genetic origin. J. Biol. Chem. 258, 14257–14262 [PubMed] [Google Scholar]
- Vesely D. L., Gower W. R., Jr, Dietz J. R., Overton R. M., Clark L. C., Antwi E. K., Farese R. V. (1999). Elevated atrial natriuretic peptides and early renal failure in type 2 diabetic Goto-Kakizaki rats. Metabolism 48, 771–778 [DOI] [PubMed] [Google Scholar]
- Watts L. M., Manchem V. P., Leedom T. A., Rivard A. L., McKay R. A., Bao D., Neroladakis T., Monia B. P., Bodenmiller D. M., Cao J. X., et al. (2005). Reduction of hepatic and adipose tissue glucocorticoid receptor expression with antisense oligonucleotides improves hyperglycemia and hyperlipidemia in diabetic rodents without causing systemic glucocorticoid antagonism. Diabetes 54, 1846–1853 [DOI] [PubMed] [Google Scholar]
- Wolfe R. R., Chinkes D. L. (2005). Isotope Tracers in Metabolic Research: Principles and Practice of Kinetic Analysis, pp. vii, 474 Hoboken, N.J.: Wiley-Liss [Google Scholar]